Abstract
Objective
To test whether trends in breast cancer mortality varied by ethnicity and socio-economic position during the 1980s and ‘90s in New Zealand.
Methods
Four cohorts of the entire New Zealand population for 1981–84; 86–89; 91–94 and 96–99 allowed direct determination of socio-economic trends in breast cancer mortality. For ethnicity, unlinked routine census and mortality data were used with adjustment factors for undercounting of Māori and Pacific deaths.
Results
Māori and non-Māori non-Pacific mortality rates changed little until mid-1990s with Māori experiencing 25% higher mortality. In 1996–99, Māori rates increased notably to become 68% higher than non-Māori non-Pacific (SRR 1.68; 95% CI: 1.49–1.90). Pacific women experienced an approximate three-fold increase in breast cancer mortality over time.
There appeared to be reducing mortality among higher income and education groups but trends within socio-economic groups were not statistically significant. Nevertheless, by 1996–99, there was a significant 22% excess mortality (SRR 1.22; 95% CI: 1.01–1.49) for low compared with high-income groups.
Conclusions
Widening ethnic, and probably, socio-economic disparities in breast cancer mortality are likely due to both underlying incidence and differential survival trends. Disparities are likely to increase once the full differential mortality benefits of screening impact on the population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As in many other regions in the world, incidence rates of breast cancer have markedly increased in New Zealand, nearly doubling between 1956 and 1996. In contrast, over the same period, mortality rates have been relatively stable and probably declined since the mid-1980s [1–3] Increasing incidence is thought to be largely due to increasing lifetime exposure to oestrogens due to delayed childbearing, increases in post-menopausal obesity, younger age at menarche and older age at menopause, as well as the recent increase in access to screening [2, 3]. The stable or reducing mortality seen in New Zealand and in other countries is likely to be largely due to earlier detection of breast cancer and improvements in treatment [3].
A number of international studies have suggested that both breast cancer incidence and mortality are more common among women from higher socio-economic groups—in the past at least [4, 5]. However, time trend studies suggest that this pattern is becoming less marked and may be disappearing, particularly for mortality [6–9]. There are also a number of reports of ethnic minority groups experiencing increasing incidence and/or mortality from breast cancer particularly over the last two or three decades [10–13].
There is good reason to expect varying trends in breast cancer incidence and mortality by social groups within countries—in particular, by ethnicity and socio-economic position. For example, patterns in factors resulting in variations in ‘lifetime exposure to oestrogens’ varied between socio-economic and ethnic groups in New Zealand. In New Zealand fertility rates fell most notably among Europeans initially (total fertility rate 4.12 in 1962, falling to 1.97 in 1999), but have been followed by dramatic declines among Māori (the indigenous population; 6.18 in 1962 to 2.69 in 1999) [14]. Similarly for survival rates, the inverse care law [15] and, by extension, the inverse equity hypothesis [16] predicts that higher socio-economic groups (and more advantaged ethnic groups) will receive the benefits of new and improved treatments for breast cancer before lower socio-economic groups.
The aim of this paper is to test the hypothesis that trends in breast cancer mortality have varied by socio-economic position and ethnicity in New Zealand during the 1980s and 1990s, resulting in changing socio-economic and ethnic disparities over time. From an international perspective, this study contributes to a growing literature on ethnic and socio-economic disparities in cancer incidence and outcomes. In New Zealand, disparities in health experiences and status between Māori (the indigenous population), Pacific ethnic groups, and non-Māori non-Pacific (predominantly European) ethnic groups are well documented and long-standing. Both Māori and Pacific people are socio-economically disadvantaged compared to New Zealand Europeans, and despite a nominally universal health care system, have worse access to health services and health care [17]. Second, the linkage of census and mortality data in New Zealand allows a rigorous analysis of both socio-economic and ethnic trends in one country. From a New Zealand perspective, mortality (and incidence) rates have been calculated before [18–21], but differences in the collection of ethnicity on mortality data compared to census data make these results prone to error—especially for trend analyses. Socio-economic trends in breast cancer mortality have not been previously described in New Zealand.
Materials and methods
Linkage of census and mortality data
The anonymous and probabilistic record linkage in the New Zealand Census-Mortality Study (NZCMS) is described in detail elsewhere [22]. Briefly, four cohorts of the total New Zealand population aged 0–74 years on census night were created for 1981–84, 1986–89, 1991–94 and 1996–99. The percentage of eligible mortality records linked back to a census record ranged from 71% to 78%, and at least 96% of the links were estimated to be true links [23]. Deaths from breast cancer (ICD 174) were identified from the ICD code for underlying cause of death from the mortality data.
Determining ethnic and socio-economic trends
The NZCMS data was central to our calculation of both ethnic and socio-economic trends in cancer mortality. But we used different methods for ethnic and socio-economic analyses. There was no alternative other than to conduct analyses directly on the linked data (i.e. linked census and mortality records) to determine socio-economic trends. However, for ethnic analyses we actually used routinely collected national mortality data that includes data on ethnicity, but adjusted them for undercounting of Māori and Pacific deaths using adjustment ratios calculated from the NZCMS. This latter method had the advantage of being able to include 5 years of mortality data for each period (rather than just the 3 years linked back to each census), conferring an important improvement in precision and stability of mortality rate estimates for the relatively small Māori and Pacific populations. This meant there were slightly different time periods covered by the ethnicity and socio-economic analyses. These two methods are now described in more detail.
Ethnicity trends
Mortality data were provided by year of registration of death and grouped into four periods: 1980–84, 1985–89, 1990–1995, and 1996–99. Census data for 1981, 1986, 1991 and 1996 by strata of sex, age and ethnicity were used as denominator data in the calculation of mortality rates. We used a prioritised approach to the categorisation of ethnicity, by which the Māori population includes all those people with at least one of the (up to three) self-identified ethnicity responses on the 1986, 1991 or 1996 census being Māori or, in 1981, if any degree of Māori ethnic origin was recorded. Otherwise, ethnicity was assigned as Pacific if one of the self-identified ethnic groups was Pacific, or any degree of Pacific ethnic origin (in 1981) was noted. Pacific is an aggregate term that includes a number of specific ethnic groups. The remaining non-Māori non-Pacific group includes all other people, predominantly European New Zealanders.
To adjust for the undercounting of Māori and Pacific deaths on mortality data, we used adjustment factors calculated from the NZCMS described in detail elsewhere [24]. Briefly, by cross-classifying the mortality and census data coding of ethnic groups for the linked dataset we were able to calculate adjustment factors that, when applied back to routine mortality data (by strata of sex and age), gave the expected number of deaths for each ethnic group had the census definition of ethnicity applied. These corrected mortality counts and the census population counts were then used to calculate direct age-standardised mortality rates (and 95% confidence intervals [CI]), using the WHO standard population as the standard population.
Socio-economic trends
The census collects highest educational qualification and gross personal income. An intercensal classification of educational qualifications was used to harmonise educational categories across censuses. Educational qualification was missing for between 2% and 11% of census respondents. Educational groups were classified as no educational qualifications, school level qualifications only, and qualifications gained post school. Personal incomes were collated up to the household level, then equivalised for economies of scale based on the numbers of children and adults in the household using a New Zealand-specific index [25] and finally consumer price index adjusted to 1996 dollars. The household income variable was unable to be calculated for between 15% and 21% of individuals due to one or more adults in the household being absent on census night or declining to report an income. The equivalised household income variable was treated as a 3-level categorical variable (approximate tertiles) for the majority of analyses.
Analyses
Mortality rates (and 95% CI) by ethnicity were calculated with direct standardisation to the age structure of the 1991 cohort. Mortality rates by level of education and income (each three-levels) were calculated with direct standardisation both to the age and ethnic structure of the 1991 cohort. We standardised the socio-economic variables for ethnicity as well as age, because ethnicity, as a determinant of socio-economic position (see Table 1) and, independently, a determinant of health, is a potential confounder. We used weighted person-time data in these calculations, where the weighting adjusted for any linkage bias due to variation in the proportion of mortality records linked to a census record [26]. For example, if 20 out of 30 eligible mortality records for 45- to 64-year-old Māori females living in moderately deprived areas in the north of New Zealand were linked to a census record, then each of the 20 linked records were assigned a weight of 1.5 (i.e. 30/20). These weights were calculated for many strata. Sensitivity analyses published elsewhere suggest the weights are reliable at adjusting for any residual linkage bias [26].
To determine the socio-economic differences in breast cancer mortality by income and education, we calculated relative indices of inequality (RII) in addition to rate ratios [27]. The RII is equivalent to a relative risk measure for the poorest compared to the richest (or people with lowest compared to highest educational qualification), but utilises mortality rates across all levels of income (and education) using regression, that is the RII overcomes the problem of socioeconomic groups changing in size over time. Mortality rates by quintile of income, and five-levels of education, were used in the calculation of RIIs.
Results
Ethnicity
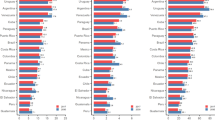
The numbers of breast cancer deaths in the period 1980–84 were 104 Māori women and 1,842 non-Māori non-Pacific women. The respective numbers of deaths among Māori and non-Māori non-Pacific women in the other time periods were 102 and 2,003 in 1985–89; 140 and 2,406 in 1990–95 and 217 and 1,474 deaths in 1996–99. In the 1980s and early 90s, both Māori and non-Māori non-Pacific mortality rates were stable (Fig. 1). However, in the most recent cohort Māori mortality rates increased, and non-Māori non-Pacific rates decreased slightly. As a result, Māori mortality rates were about 25% higher than non-Māori non-Pacific during the 1980s and 1990–1995, and 70% higher in 1996–99 (standardised rate ratios and 95% CI in Table 2). There was a similar pattern both for women aged under 45 years, and 45 years and older, with Māori women having excess mortality from breast cancer over all time periods compared with non-Māori non-Pacific women, particularly in the 1996–99 cohort (data not shown).
The number of deaths among Pacific women was small with 11 deaths in the 1980–84 period, increasing to 96 deaths by 1996–99. This meant that for Pacific women there was an approximate three-fold increase in breast cancer mortality over time, with non-overlapping confidence intervals for the 1981–84 and 1996–99 rates. However, probably because of small numbers combined with only four observation points, the test for trend is not significant (P = 0.19). In the first cohort period Pacific women appeared to experience considerably lower breast cancer mortality than the other two groups, but in the last cohort period they had the highest mortality rate.
Socio-economic position
The number of breast cancer deaths among women in the lowest income group ranged from 375 deaths in 1981–84 period to 528 in 1996–99. The numbers of deaths in the middle-income group ranged from 300 to 366, and in the high-income group from 273 to 312 deaths over the four cohort periods. Figure 2 shows that between 1981–84 and 1996–99 the breast cancer mortality rate among the high income group declined nearly 20% from 48 to 39 per 100,000 (P for trend 0.11), and to a lesser extent in the middle income group (52 to 46 per 100,000; P for trend 0.20). In contrast, there was no apparent trend among the low-income group. Accordingly, by 1996–99 there was a significant 22% excess mortality among the low income compared to high-income women (SRR 1.22; 95% CI: 1.01–1.49, Table 3). This was also reflected in the relative index of inequality of 1.4 (1.08–1.83) for 1996–99, which measures the relative difference comparing the expected mortality risk among the poorest person to the richest person.
The number of breast cancer deaths among women in the lowest education group ranged from 606 to 738 deaths over the four cohort periods. The number of deaths in the middle education group ranged from 138 to 357, and the highest education group from 183 to 378 deaths over the four periods. For education, there was little change in mortality rates over time for those in the lowest education group, whilst those in the middle and highest groups appeared to demonstrate a small and non-significant declining trend in breast cancer mortality during the 1980s and 90s (Fig. 2). This meant that what may have been an association of higher breast cancer mortality with higher education in the early 1980s (SRR 0.82; 95%CI: 0.66–1.03) disappeared over the remainder of the period studied (Table 3).
Discussion
This study shows a widening gap between the breast cancer mortality rates for Māori and non-Māori non-Pacific women in New Zealand, primarily due to increasing breast cancer mortality among Māori women. There was also a three-fold increase in Pacific breast cancer mortality, such that by the end of the 1990s Pacific rates were twice those of non-Māori non-Pacific women. There may also be a trend of reducing breast cancer mortality among those in the highest income and education groups compared with little or no change in the lower income and education groups, although these trends are of marginal statistical significance. By the late 1990s, there was a significant 22% excess in breast cancer mortality among the lower income groups compared with the highest.
Whilst the NZCMS presents a unique international opportunity to simultaneously examine socio-economic and ethnic trends in breast cancer mortality, and accounts for systematic differences in the way ethnicity data are collected in mortality and census datasets, the results are still prone to limitations. First, New Zealand is a relatively small country, rendering trends stratified by either ethnicity or socio-economic position to be somewhat imprecise statistically. Second, not all eligible mortality records are linked back to a census record. However, we adjust for any resultant linkage bias using weights that have been shown elsewhere in sensitivity analyses to be reliable [26].
Interpretation of ethnic trends
In New Zealand, there has been little difference in the pattern for breast cancer incidence between Māori, Pacific and non-Māori non-Pacific up to the 1990s, with the exception of younger Māori women who have been reported to have higher incidence rates [18–21]. More recent cross-sectional population-based research has suggested that while there may be a small excess risk among Māori women in terms of incidence, there is considerably higher breast cancer mortality among Māori compared with non-Māori women [1, 28]. Similar patterns can be seen elsewhere, for example, among African-American women compared with White women in the United States [10]. The pattern of similar incidence but higher mortality suggests a survival disadvantage for Māori women compared with non-Māori non-Pacific women in New Zealand. Such survival disparities among indigenous populations are also seen, for example, in the United States and Australia [13, 29, 30].
Less data is available about Pacific women, with studies suggesting they have lower or similar incidence to non-Māori non-Pacific women [21, 31]. The rapid increase in mortality among Pacific women during the 1980s and 90s may be due to under-ascertainment of cases early in that period, combined with increasing incidence due to declining fertility and increasing rates of obesity [14, 32]. It is also likely that survival disparities exist for Pacific women, but as yet there are no studies from New Zealand investigating this issue.
Three studies have directly examined differences in cancer survival between Māori and non-Māori non-Pacific people in New Zealand. Two concluded that, for breast cancer, most of the survival disparity was due to differences in stage at diagnosis [33, 34], while the third suggested that even after adjusting for differences in stage, significant disparities in survival persisted [35]. Internationally some, but not all, studies have found ethnic disparities in survival persist even after adjusting for stage [7, 29, 36]. Other suggested reasons for survival disparities between ethnic groups include delays in access to or incomplete treatment among some groups, differences in the presence of other co-morbidities, prevalence of smoking, obesity and other risk factors, and genetic factors resulting in more aggressive disease [29, 30, 37–39].
Stage at diagnosis is the single most important predictor of survival for breast cancer. There is evidence that both Māori and Pacific women are diagnosed at a later stage, with larger tumours, more lymphatic involvement and more distally metastatic disease [21, 33, 35]. Little research has examined why Māori and Pacific women are diagnosed later than non-Māori non-Pacific. The national mammographic screening programme in New Zealand was initiated in 1998, so whilst there are marked differences in screening coverage by ethnicity, the impact of this is unlikely to be seen in these mortality results. New Zealand has a partially subsidized, mostly fee-for-service primary health care system, which acts largely as a gatekeeper to universal secondary care and specialist services. Nevertheless, there is some evidence to suggest that Māori and Pacific people not only experience more barriers in accessing primary care than non-Māori non-Pacific people in New Zealand [40, 41], but also that their experience of the health system may differ from that of non-Māori non-Pacific people. For example, a recent national audit of women with cervical cancer found that there were longer delays between the identification of smear abnormalities and final diagnosis among Māori women compared with non-Māori non-Pacific women [42]. Also, despite their higher cardiovascular mortality, Māori and Pacific people receive fewer cardiac interventions than expected [43, 44]. This evidence is consistent with evidence from the United States which shows that there are ethnic differences in the receipt of optimal cancer diagnostic, treatment and palliative services [45].
In New Zealand, Māori and Pacific people experience higher rates of morbidity and mortality, are more likely to smoke and have higher levels of obesity than non-Māori. It is possible that these differences may account for some of the disadvantage in terms of cancer survival. These factors are thought to affect survival both directly and through their adverse effects on treatment adequacy [36, 46–48]. There are no studies in New Zealand that examine this issue, however, there is some evidence from the US that even after adjusting for differences in underlying co-morbidity, disparities in survival rates between African-Americans and Whites persist [49], suggesting that this is, at best, a partial explanation.
The potential role of genetic differences between ethnic groups has not been thoroughly explored in New Zealand. International evidence suggests that while some ethnic groups are at greater risk of carrying high-risk genes for breast cancer, no such evidence exists for Māori and Pacific Island women in New Zealand [38]. Furthermore, genetic susceptibility cannot adequately explain the increasing disparities in breast cancer mortality over this 20-year time frame.
Socio-economic status
Our study suggests the emergence of socio-economic disparities in breast cancer mortality, which are not as large as the ethnicity disparities described above. As such, our results are consistent with emerging international data on changing socio-economic disparities [6–9] which shows that while breast cancer mortality may have been more common among women from higher socio-economic position in the past, that association has disappeared and is now appearing to reverse. Interestingly, while there is undoubtedly a greater difference in mortality than incidence between ethnic groups in New Zealand, such a pattern is not evident for socio-economic groups. For example, recent work using an area-based measure of socio-economic position (NZDep) demonstrated a significant negative socio-economic gradient in breast cancer incidence but not mortality using data from 1996 to 97 [1]. The study presented here, which uses individual measures of socio-economic position over a 20-year time period, does suggest a negative gradient may be emerging for mortality also, and it would be interesting to do similar trend analyses for breast cancer incidence using New Zealand data. In general, the findings are consistent with the idea that changes in the socio-economic patterning of breast cancer mortality in New Zealand may be primarily due to changes in underlying risk factors such as changing patterns in childbearing, and increases in post-menopausal obesity, resulting first in changes in incidence, followed by mortality. However, it is likely that there are socio-economic survival differences within New Zealand such as those documented in other countries [4]. These differences can be explained using the inverse equity theory, which suggests that inequality will initially increase as individuals within higher socio-economic groups access new technologies such as improved breast cancer treatments, prior to those within lower groups [16].
Conclusion
This paper has highlighted the increasing ethnic and possibly socio-economic disparities in breast cancer mortality in New Zealand during the 1980s and 1990s. These findings are important because firstly, there are clearly disparities that exist now, and which are important in their own right; secondly, there is evidence that these disparities may be increasing, and thirdly once the full differential mortality benefits of screening impact on the population, it is likely that disparities will increase more rapidly, at least for older women.
References
Ministry of Health (2002) Cancer in New Zealand. Trends and projections. Ministry of Health, Wellington
Hermon C, Beral V (1996) Breast cancer mortality rates are levelling off or beginning to decline in many western countries: analysis of time trends, age-cohort and age-period models of breast cancer mortality in 20 countries. Br J Cancer 73:955–960
Althuis M, Dozier J, Anderson W, Deversa S, Brinton L (2005) Global trends in breast cancer incidence and mortality 1973–1997. Int J Epidemiol 34:405–412
van Loon AJ, Brug J, Goldbohm RA, van den Brandt PA, Burg J (1995) Differences in cancer incidence and mortality among socio-economic groups. Scand J Soc Med 23:110–120
Faggiano F, Partanen T, Kogevinas M, Boffetta P (1997) Socioeconomic differences in cancer incidence and mortality. IARC Scientific Publications, Lyon
Pukkala E, Weiderpass E (1999) Time trends in socio-economic differences in incidence rates of cancers of the breast and female genital organs (Finland, 1971–1995). Int J Cancer 81:56–61
Le Marchand L, Yoshizawa N, Kolonel LN, Nomura AM (1987) Time trends in characteristics at diagnosis and subsequent survival for Caucasian, Japanese and Hawaiian women with breast cancer in Hawaii. J Chronic Dis 40:1099–1110
Wagener DK, Schatzkin A (1994) Temporal trends in the socioeconomic gradient for breast cancer mortality among US women. Am J Public Health 84:1003–1006
Martikainen P, Valkonen T (2000) Diminishing educational differences in breast cancer mortality among Finnish women: a register-based 25-year follow-up. Am J Public Health 90:277–280
Krieger N, Quesenberry C Jr, Peng T et al. (1999) Social class, race/ethnicity, and incidence of breast, cervix, colon, lung, and prostate cancer among Asian, Black, Hispanic, and White residents of the San Francisco Bay Area, 1988–92 (United States). Cancer Causes Control 10:525–537
Weir HK, Thun MJ, Hankey BF et al. (2003) Annual report to the nation on the status of cancer, 1975–2000, featuring the uses of surveillance data for cancer prevention and control. J Natl Cancer Inst 95:1276–1299
Hunter CP (2000) Epidemiology, stage at diagnosis, and tumor biology of breast carcinoma in multiracial and multiethnic populations. Cancer 88:1193–1202
Frost F, Tollestrup K, Hunt WC et al. (1996) Breast cancer survival among New Mexico Hispanic, American Indian, and non-Hispanic white women (1973–1992). Cancer Epidemiol Biomarkers Prev 5:861–866
Ministry of Social Policy (2005) The social report: Indicators of social well-being in New Zealand. Ministry of Social Policy, Wellington
Hart J (1971) The inverse care law. Lancet 1:405–412
Victora C, Vaughan J, Barros F, Silva A, Tomasi E (2000) Explaining trends in inequities: evidence from Brazilian child health studies. Lancet 356:1093–1098
Blakely T, Tobias M, Robson B et al. (2005) Widening ethnic mortality disparities in New Zealand, 1981–99. Soc Sci Med 61: 2233–2251
Foster F (1977) Cancer registry in New Zealand. N Z Med J 47:41–44
Armstrong W, Borman B (1996) Breast cancer in New Zealand: trends, patterns, and data quality. N Z Med J 109:221–224
McCredie M, Paul C, Skegg DC, Williams S (1999) Breast cancer in Maori and non-Maori women. Int J Epidemiol 28:189–195
Lawes CM, Tukuitonga CF, Scragg RK (1999) The epidemiology of breast cancer in Pacific women in New Zealand. N Z Med J 112:354–357
Blakely T, Woodward A, Salmond C (2000) Anonymous linkage of New Zealand mortality and census data. Aust N Z J Public Health 24:92–95
Blakely T, Salmond C (2002) Probabilistic record linkage and a method to calculate the positive predictive value. Int J Epidemiol 31:1246–1252
Ajwani S, Blakely T, Robson B, Atkinson J, Kiro C (2003) Unlocking the numerator-denominator bias III: adjustment ratios by ethnicity for 1981–1999 mortality data. The New Zealand Census-Mortality Study. N Z Med J 116:U456
Jensen J (1988) Income equivalences and the estimation of family expenditure on children. Department of Social Welfare (unpublished)
Fawcett J, Blakely T, Atkinson J (2002) Weighting the 81, 86, 91 and 96 census-mortality cohorts to adjust for linkage bias. NZCMS technical report no. 5. Department of Public Health, Wellington School of Medicine and Health Sciences, Wellington
Mackenbach JP, Kunst AE (1997) Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med 44:757–771
Curtis E, Wright C, Wall M (2005) The epidemiology of breast cancer in Maori women in Aotearoa New Zealand: implications for screening and treatment. N Z Med J 118:U1297
Meng L, Maskarinec G, Wilkens L (1997) Ethnic differences and factors related to breast cancer survival in Hawaii. Int J Epidemiol 26:1151–1158
Condon JR, Armstrong BK, Barnes T, Zhao Y (2005) Cancer incidence and survival for indigenous Australians in the Northern Territory. Aust N Z J Public Health 29:123–128
Tukuitonga CF, Solomon N, Stewart A (1992) Incidence of cancer among Pacific Island people in New Zealand. N Z Med J 105:463–466
Ministry of Health (2004) Tracking the obesity epidemic: New Zealand 1977–2003. Ministry of Health, Wellington
Lethaby AE, Mason BH, Holdaway IM, Kay RG (1992) Age and ethnicity as prognostic factors influencing overall survival in breast cancer patients in the Auckland region Auckland Breast Cancer Study Group. N Z Med J 105:485–488
Jeffreys M, Stevanovic S, Tobias M et al. (2004) Ethnic differences in cancer survival in New Zealand: linkage study. Am J Public Health 95:834–837
Cormack D, Robson B, Purdie G, Ratima M, Brown R (2005) Access to cancer services for Maori. Ministry of Health, Wellington
Maskarinec G, Pagano IS, Yamashiro G, Issell BF (2003) Influences of ethnicity, treatment, and comorbidity on breast cancer survival in Hawaii. J Clin Epidemiol 56:678–685
Gwyn K, Bondy ML, Cohen DS et al. (2004) Racial differences in diagnosis, treatment, and clinical delays in a population-based study of patients with newly diagnosed breast carcinoma. Cancer 100:1595–1604
Neuhausen SL (1999) Ethnic differences in cancer risk resulting from genetic variation. Cancer 86:2575–2582
Perera NM, Gui GP (2003) Multi-ethnic differences in breast cancer: current concepts and future directions. Int J Cancer 106:463–467
Ministry of Health (2004) A portrait of health: key results of the 2002/03 New Zealand Health Survey. Ministry of Health, Wellington
Davis P, Lay-Yee R, Sinclair O, Gribben B (1997) Maori/non-Maori patterns of contact, expressed morbidity and resource use in general practice: data from the Waikato Medical Care Survey 1991–2. N Z Med J 110:390–392
Sadler L, Priest P, Peters J, Crengle S, Jackson R (2004) Cervical cancer audit report. Screening of women with cervical cancer, 2000–2002. Ministry of Health, Wellington
Westbrooke I, Baxter J, Hogan J (2001) Are Maori under-served for cardiac interventions? N Z Med J 114:484–487
Tukuitonga CF, Bindman AB (2002) Ethnic and gender differences in the use of coronary artery revascularisation procedures in New Zealand. N Z Med J 115:179–182
Smedley B, Stith A, Nelson A (eds) (2002) Unequal treatment: confronting racial and ethnic disparities in health care. National Academy Press, Washington DC
Louwman WJ, Janssen-Heijnen ML, Houterman S et al. (2005) Less extensive treatment and inferior prognosis for breast cancer patient with comorbidity: a population-based study. Eur J Cancer 41:779–785
Carmichael AR, Bates T (2004) Obesity and breast cancer: a review of the literature. Breast 13:85–92
Yancik R, Wesley MN, Ries LA et al. (2001) Effect of age and comorbidity in postmenopausal breast cancer patients aged 55 years and older. JAMA 285:885–892
Eley JW, Hill HA, Chen VW et al. (1994) Racial differences in survival from breast cancer. Results of the National Cancer Institute Black/White Cancer Survival Study. JAMA 272:947–954
Acknowledgements
The NZCMS is conducted in collaboration with Statistics New Zealand and within the confines of the Statistics Act 1975. The NZCMS was funded by the Health Research Council of New Zealand, and is now funded by the Ministry of Health.
Summary statistics New Zealand security statement
The New Zealand Census-Mortality Study (NZCMS) is a study of the relationship between socio-economic factors and mortality in New Zealand, based on the integration of anonymised population census data from Statistics New Zealand and mortality data from the New Zealand Health Information Service. The project was approved by Statistics New Zealand as a Data Laboratory project under the Microdata Access Protocols in 1997. The datasets created by the integration process are covered by the Statistics Act and can be used for statistical purposes only. Only approved researchers who have signed Statistics New Zealand’s declaration of secrecy can access the integrated data in the Data Laboratory (A full security statement is in a technical report at http://www.wnmeds.ac.nz/nzcms-info.html). For further information about confidentiality matters in regard to this study please contact Statistics New Zealand.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarfati, D., Blakely, T., Shaw, C. et al. Patterns of Disparity: Ethnic and Socio-economic Trends in Breast Cancer Mortality in New Zealand. Cancer Causes Control 17, 671–678 (2006). https://doi.org/10.1007/s10552-005-0583-0
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10552-005-0583-0