Abstract
Background
To examine time trends in cervical cancer incidence and mortality in NSW women aged ¥20 years in relation to important health service initiatives and programs.
Methods
Data on cervical cancer incidence and mortality were obtained from the NSW Central Cancer Registry for 1972–2001, and corresponding annual populations obtained from the Australian Bureau of Statistics. Direct age-standardised rates in the ¥20 year population were calculated using the 2001 NSW census population as standard. Proportional reductions in incidence and mortality since 1972–1974 were also calculated and related to key health service factors and to published NSW 5-year cervical cancer relative survival for similar periods.
Results
Declines in cervical cancer incidence (−10%) and mortality (−20%), and increased degree-of-spread specific survival following the introduction of universal health care in 1975 suggest effects of greater access to Pap screening, earlier access to diagnosis and treatment services, and improved effectiveness of treatment. Incidence plateaued during the 1980s, but mortality fell further (−7%) due to an increased proportion of localised cancers (without change to degree-of-spread specific survival). The 1980s mortality reduction was a consequence of earlier diagnosis and/or secondary prevention, not improved treatment effectiveness or reduced incidence. A marked and sustained incidence decline to 2001 (−35%) occurred after the introduction of the NSW Cervical Screening Program in 1992. This was followed 3 years later by a sustained mortality decline (−20%). During the 1990s survival across all degrees of spread remained unchanged and the mortality reduction was due entirely to reduction in incidence.
Conclusions
The substantial reduction of cervical cancer incidence and mortality in NSW over the last 3 decades is associated with important health service interventions that relate to control of cervical cancer, particularly the implementation of a population-based organised cervical screening program.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is a significant gynaecological cancer in women in most populations, and is preventable by regular screening by exfoliative cytology using the Papanicolaou technique. Screening identifies potentially pre-cancerous lesions (cervical intra-epithelial neoplasia or CIN) which convey a risk of development into invasive carcinoma. These lesions can then be removed or ablated which reduces population incidence of invasive cervical carcinoma (primary prevention). Lowered incidence eventually will translate directly into reduced mortality from the disease. Screening can also detect early asymptomatic invasive carcinoma (secondary prevention) and produce lower mortality and improved survival from earlier and thus more effective treatment [1, 2]. Lowered mortality can also result from earlier diagnosis of symptomatic disease, and to improved degree-of-spread specific treatment. In whole populations, declines in cervical cancer mortality over time can be a consequence of earlier incidence decline, and improved treatment outcomes for diagnosed cases, either through improvement in degree-of-spread specific treatment or increasing proportions of cases detected at earlier stages.
The evidence of effectiveness of population screening for cervical cancer relies on the results of observational studies of individuals and populations. A meta-analysis of published case–control and cohort studies has documented the effectiveness of regular cervical screening in preventing cancer of the cervix [3]. Evidence for effectiveness of screening in populations relies on studies of time trends in cervical cancer incidence and/or mortality in relation to the introduction and intensity of cervical screening, mainly from Nordic countries (Iceland [1, 4–6], Scandinavia [7], Finland [8]), Britain [9–13] and Canada [14]; and from studies of differentials in cervical cancer incidence or mortality between populations with different dates of introduction or intensities of cervical screening [15–17]. Two of these latter studies [4, 5] contributed to the meta-analytic evidence [3], and the remainder are later confirmation of the benefits of cervical screening.
Reduction in cervical cancer incidence and mortality, and improvements in survival, have been recorded in New South Wales (NSW) and Australia for some time [18–26]. In Australia, cervical cancer screening moved to an organised approach in the early 1990s, which included: state-wide recruitment activities; improvements in Pap smear taking and laboratory quality control; improvements in notification of results; standardised management guidelines for abnormal results; and monitoring and research. In NSW this included a population-based Pap Test Register (PTR), which commenced operation in mid-1996 in order to: send reminders to women for regular Pap test screening; ensure follow-up of abnormalities; supply previous Pap test results to service providers; and provide data for program surveillance and management. The first reminder letters for biennial screening were sent by the PTR in 1999, to women on the register who had not screened in 27 months.
To date, trends in cervical cancer outcomes in Australia have not been examined in relation to major health initiatives, particularly the implementation of organised population-based cervical screening. Moreover, in the absence of randomised controlled trials of cervical screening, it is important that service studies be conducted to assess the effectiveness of cervical screening at a population level. Accordingly, this article assesses the changes that have occurred in cervical cancer incidence, survival and mortality in NSW in relation to the introduction of population-based prevention and control activities.
Materials and methods
Data
Annual numbers of new cases and deaths from cervical cancer in NSW female residents by 5-year age group and year of diagnosis or death for 1972–2001 were obtained for this analysis from the NSW Central Cancer Registry (CCR), using the CCR cause of death attribution. Primary site of cancer is coded by the CCR according to the International Classification of Diseases, 9th revision (ICD-9). Cancer death data on the NSW CCR come from two sources: (1) deaths reported to the NSW CCR from reporting institutions, especially hospitals; and (2) the vital registration death data. The NSW CCR amalgamates both sources with information on incidence to derive fact of death and cause of death. Hence this is more accurate than just using cause of death data recorded by vital registration or just cancer deaths reported to the NSW CCR.
Since 1972, notification of malignant neoplasms to the NSW CCR has been a statutory requirement for all NSW public and private hospitals, radiotherapy departments and nursing homes, and for pathology and outpatients departments since 1985. The histological verification rate for all cancers in NSW increased from 68% in 1972 to 89% by 1985, and since has varied between 85% and 90% in females (including cytology which was not distinguished from histology prior to 1991) [25]. The histological verification rate for cervical cancer in 2001 was 96 percent. The proportion of death certificate only (DCO) notifications of cancer in NSW has varied between under 1% and 2% over 1972–2001, except for the period 1983–1990 where the DCO rate varied between 2% and over 3% due to limited CCR resources reducing active follow-up of cases first notified by death certificate. In 2001 the DCO rate for cervical cancer was 0.4% [25]. NSW CCR data meet quality guidelines and are published in cancer incidence in five continents by IARC [27].
Annual population estimates for 1972–2001 by sex and 5-year age group were obtained from the Australian Bureau of Statistics (ABS).
Analysis
Directly age-standardised incidence and mortality rates in the ¥20 year population were calculated using the 1996 NSW census population as standard, along with 95% confidence intervals [28]. The proportional reduction in incidence and mortality since 1972–1974, using aggregated 1972–1974 incidence and mortality as the baseline (100%), was computed as a percentage with accompanying 95% confidence intervals, and plotted by period against milestone health service factors on the same graph. Comparison was made with published NSW 5-year relative cervical cancer survival data for similar periods [21, 29]. Quoted relative 5-year survival figures were computed originally from the absolute survival of women up to 5 years after being diagnosed with cervical cancer regardless of their underlying cause of death, as a percent proportion of age- and period-matched survival for all NSW or Australian women [21, 29]. Microsoft Excel spreadsheet software was used for the calculation of rates, confidence intervals (using formulae from [28]) and for graphing.
Results
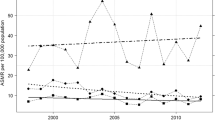
In the baseline comparison period (1972–1974) an average of 338 new cases of cervical cancer were diagnosed annually in NSW (as reported to the NSW CCR). Cervical cancer mortality during this period averaged 138 deaths per year. In 2001, the end of the study period, the total number of new cervical cancer cases diagnosed was 252, and mortality from cervical cancer was 82 deaths. Correspondingly, cervical cancer incidence and mortality rates have declined over the 30 years since 1972, by almost 50% and 60%, respectively (Figures 1, 2, 4), and 5-year survival has increased correspondingly (Tables 1 and 2, Figure 3).
The approximate 10% decline in incidence, most of which occurred in the 4 years after the introduction of universal health care in 1975, persisted more or less as a plateau thereafter through to 1992 (Figures 1 and 4). The approximate 20% reduction in mortality following introduction of universal health care was followed by a smaller reduction (≈7%) until the late 1980s. (Figures 2 and 4). Degree-of-spread specific 5-year survival also improved in the 1970s, particularly from regional spread (Tables 1 and 2, Figure 3 [21, 29]).
While the incidence trend of cervical cancer remained relatively static up to 1992, mortality fell by another 20% during 1989–1992. (Figures 1, 2, 4). The improved survival during the 1980s (Figure 3) was documented as a shift to a higher proportion of localised cancer as degree-of-spread specific 5-year survival remained unchanged (Table 1, [21, 29]).
A substantial and continued fall in cervical cancer incidence occurred following the introduction of the NSW Cervical Screening Program in 1992 (35% fall over 9 years), and this was followed 3 years later by a continued decline in mortality of approximately 20% over 6 years (Table 2, Figures 1, 2, 4). There was no significant further improvement in 5-year survival during this period (Table 1, Figure 3).
Incidence rates for the years 1995–2001 were significantly lower than for earlier years, as is evident from the non-overlapping 95% confidence intervals (Figure 1). Similarly, mortality rates for the years 1999–2001 were significantly lower than for any year during 1972–1997 (Figure 2).
Discussion
Reduction in population mortality from cervical cancer can be explained on the basis of reduced incidence, earlier detection and/or improved treatment. Reduced incidence of cervical cancer (primary prevention) can be a consequence of reduction in risk factors for the condition (including HPV infection), or detection and treatment of pre-cancerous cervical abnormalities/biological risk factors for cervical cancer. Organised population screening may also detect cancer in asymptomatic women at earlier stages of development than might be the case without screening and, in the absence of improvement in stage-specific treatment effectiveness, lead to better prognosis and survival (secondary prevention). Reduced mortality can be a consequence of diagnosis of cancer at a less advanced stage which can result from screening asymptomatic women (secondary prevention), and/or earlier diagnosis of symptomatic women from earlier clinical presentation, diagnostic evaluation and referral. Mortality reduction or increased survival can also be a consequence of improved effectiveness of treatment of cervical cancer for particular or all stages of the disease.
The approximate 10% decline in cervical cancer incidence following the introduction of universal health insurance (1975), which thereafter was stable through to 1992, suggests greater Pap test screening through improved access to general practitioners and laboratory cytology services because of improved accessibility from fee rebates. Population secular trends in Pap tests were not available from this period for comparison, however, nor are pre-cancer abnormality detection rates. However, following the introduction of universal health insurance there was an improvement in 5-year relative survival of cervical cancer from 64% to 70 % due to degree-of-spread specific improvement in survival, especially in cases with regional spread (37%–48%), with no significant shift in proportion of cases diagnosed at different degrees of spread [21] (Table 1). The 20% reduction in mortality following the introduction of universal health insurance, which became less pronounced through to the late 1980s, would, in part, reflect the decline in incidence from primary prevention through increased Pap screening. The decline in mortality in this period also reflects the better survival due to improved degree-of-spread specific survival, and this suggests improved effectiveness of stage-specific treatment (Table 1, Figure 3). Although there was little evidence of shift across the broad categories of localised, regional or distant spread during the 1970s, there could also have been earlier diagnosis and more prompt treatment within the degree-of-spread categories from secondary prevention by Pap tests (screening asymptomatic women) and earlier diagnosis in (minimally) symptomatic women. The hospital component of Medibank (and later Medicare) introduced in 1975 provided tertiary treatment without direct charge for the entire population, and this would have facilitated prompt referral and intensive treatment. Besides the improvement in degree-of-spread specific survival, the near simultaneous proportional declines in incidence and mortality (Figure 4) suggest that improved treatment or earlier referral (within stages or degrees of spread) must have played a role in the mortality decline in the 1970s, especially earlier on, since declines in mortality from reduced incidence alone would be expected to be delayed for some years, and this did occur following the introduction of organised cervical screening in NSW.
There was no significant reduction in incidence in the 1980s, and thus there was no effect of primary prevention on the mortality decline (≈7%) which occurred over the same part of this decade. Neither was there evidence of improvement in 5-year degree-of-spread specific relative survival in this period. However, overall survival did improve (from 68% to 73%) due to a shift in diagnosed cancers to an increase in the proportion of localised cancer from 67% to 73% (excluding 15% unknown spread) (Table 1, [21]). Thus the mortality reduction, especially in the late 1980s, is likely to be due to earlier diagnosis of cancer through higher participation in ad hoc screening by asymptomatic women (secondary prevention) and earlier cancer detection in (minimally) symptomatic women.
The most impressive changes in cervical cancer incidence in NSW occurred following the introduction of the NSW Cervical Screening Program in 1992, with a substantial and continuing decline in incidence of 35% over 9 years – following a period of relatively stable rates for over a decade. This incidence decline was followed 3 years later by a significant and continued decline in mortality of approximately 20% over the 6 years to 2001. Although the NSW Pap Test Register commenced operations in August 1996, it could not have had an immediate effect because the recommended biennial screening interval meant that the first reminder letters were not scheduled to be sent until January 1999, and then only to those women who became more than 3 months overdue for a Pap test. The effect of reminder letters routinely sent from the PTR since 1999 on incidence will require a longer monitoring period for assessment. During the 1990s there was minimal change in 5-year cervical cancer relative survival from 72% (1987–1991) [21] to 73% (1994–2000) [29]. It is clear that the decline of cervical cancer incidence in the decade since 1992, and the subsequent decline in cervical cancer mortality, is associated with the organised approach to cervical screening implemented by the NSW Cervical Screening Program.
Cervical screening programs detect a range of lesions of varying severity and closeness to cervical cancer. Lack of information on cervical pre-cancer abnormality detection rates prior to organised or sudden increased access to screening in NSW precludes exploration of the relationship between the advent of organised or increased access to screening and the subsequent rapid decline in cancer incidence. However, if one considers an already partly screened population that becomes more fully screened in a relatively short period, then a substantial fraction of the pool of women with undetected high grade lesions (CIN2/3, which on average would be expected to progress to invasive cancer within 1–3 years) would be picked up by organised or increased access to screening. The subsequent incidence reduction from prompt treatment of these high grade lesions would more than outbalance the additional number of undetected cancers picked up in newly screened women. This is because the incidence and/or background prevalence of high grade lesions is probably about 15–20 times higher than that of cervical cancer [30], although this is difficult to estimate because the recording of these lesions has only occurred in the context of organised screening when they are systematically recorded, followed up and treated. The most recent observed mortality reduction in NSW occurred 3 years following the introduction of organised cervical screening and was not associated with increased access to treatment or its improvement, significant shift to lesser degree of spread or to increased relative survival stemming from either.
Population data on Pap test screening in NSW became available with the advent of the NSW Pap Test Register in 1996. Currently there are relatively high rates of cervical screening participation in NSW women. While biennial (2-year) screening rates were around 60% during 1999–2003, triennial (3-year) screening rates were 74%, and the quinquennial (5-year) screening rate for 1998–2002 was 93% (based on NSW PTR data) [30]. Despite the protective effect of screening declining with increased screening interval, since most cervical screening is directed towards detecting pre-cancerous abnormalities, almost any screening interval has some effectiveness. Meta-analysis of observational research studies indicates that annual and 2-year screening are 93% effective in prevention of cervical cancer, 3-year screening 91% effective, 5-year screening 84% effective, and 10-year screening 64% effective [3].
The lack of randomised population trials of Pap test screening for prevention of cervical cancer has meant that evidence of effectiveness necessarily has come from meta-analyses of observational epidemiological studies (especially case–control studies), as mentioned above, and from aggregate comparative studies of cervical cancer incidence and mortality within and between populations, in relation to the introduction and implementation of population-level cervical screening programs. Time trend analyses of cervical cancer incidence and/or mortality in relation to the introduction and intensity of cervical screening in Nordic countries such as Iceland [1, 4–6], Scandinavia [7], Finland [8], and in Britain [9–13], have indicated the success of organised cervical screening at a population level.
In the late 1970's, Johannesson et al. [4] found a more than two-fold reduction in mortality from cervical cancer in Icelandic women aged 25–59 years. The authors concluded that the only tenable explanation for the reduction in cervical cancer mortality was that it was a consequence of the introduction of a comprehensive screening program, as it specifically targeted women aged 25–59 years. Subsequently Johannesson et al. [5] noted that since the introduction of mass cervical screening in Iceland in 1964 there had been a 60% decline in cervical cancer mortality by 1980. The same authors also observed that mortality resulting from cervical cancer in non-screened women was 10 times that in screened women. A Finnish study found a reduction in cervical cancer incidence of about 60–70% to be associated with organised cervical screening, and that the reduction was most pronounced in women aged 35–50 years who also were the most intensively screened [8].
Evidence for a dose-response relationship across different populations and program coverage has been noted by Laara et al. [15], who found lower cervical cancer mortality associated with higher screening coverage in Nordic countries. Thus, Iceland's mortality reduction for 1962–1981 was greatest (80%), as the screening program was nationwide and targeted the widest age range (25–69 years); mortality reductions in Finland and Sweden were lower (50% and 34%, respectively) as their screening programs targeted narrower age ranges (30–55 and 30–49 years, respectively); while in Denmark, with 40% population coverage, the mortality reduction was 25%. In Norway, with only 5% population screening coverage, the mortality reduction was 10%. All comparison countries had screening participation rates of 70–80% in their screening target populations.
Health service arrangements relevant to control of cervical cancer in other Australian states are similar to NSW. In particular, universal health insurance was a national program begun in 1975, and individual state cervical screening programs were spawned from a national program in the early 1990s. A pertinent finding of the present study is that despite universal health insurance with minimal financial barriers for patients to attend medical doctors (both general practitioners and specialists) because of fee rebates, with preservation of fee-for-service for both general practitioners and pathology laboratories, there was a minimal effect on cervical cancer incidence over more than 15 years. There was an approximate 10% reduction in incidence early on after the introduction of universal health insurance, but this was followed by a sustained plateau lasting until 1992. In contrast, the introduction of the organised approach to cervical screening was immediately followed by a substantial and continuing decline in cervical cancer incidence (35% over 9 years). The present before-and-after population assessment of the introduction of an organised approach to cervical screening includes sufficient time points before and after the introduction of the program to observe that the reduction in incidence is not random fluctuation but has been sustained which is evident from non-overlapping 95% confidence intervals; and that the mortality reduction is also likely to continue. It is improbable that explanations for these sudden and sustained changes in cervical cancer incidence are tenable other than as programmatic effects, especially since 5-year relative survival has not significantly altered over the same period.
We conclude that the decline in cervical cancer incidence and consequent mortality reduction in NSW women is a real public health success story of primary prevention of cancer, and that Pap test screening has also probably contributed to lower cervical cancer mortality through secondary prevention and earlier diagnosis. This is an example of a population-level intervention producing measurable improvement in population health. The decline in cervical cancer incidence and mortality in NSW can be associated with important health service interventions that relate to control of cervical cancer, particularly the implementation of the organised approach to cervical screening.
References
K Sigurdsson J Hrafnkelsson G Geirsson et al. (1991) ArticleTitleScreening as a prognostic factor in cervical cancer: analysis of survival and prognostic factors based on Icelandic population data, 1964–1988 Gynecol Oncol 43 64–70 Occurrence Handle10.1016/0090-8258(91)90011-S Occurrence Handle1:STN:280:By2D2s%2FnsVE%3D Occurrence Handle1959790
HO Adami J Ponten P Sparen et al. (1994) ArticleTitleSurvival trend after invasive cervical cancer diagnosis in Sweden before and after cytologic screening. 1960–1984 Cancer 73 140–147 Occurrence Handle1:STN:280:ByuC3c7lsVA%3D Occurrence Handle8275416
InstitutionalAuthorNameInternational Agency for Research on Cancer [IARC] (1986) ArticleTitleScreening for squamous cervical cancer: duration of low risk after negative results of cervical cytology and its implications for screening policies BMJ 293 659–664
G Johannesson G Geirsson N Day (1978) ArticleTitleThe effect of mass screening in Iceland, 1965–74, on the incidence and mortality of cervical carcinoma Int J Cancer 21 418–425 Occurrence Handle1:STN:280:CSeB3Mjkt1c%3D Occurrence Handle669847
G Johannesson G Geirsson N Day et al. (1982) ArticleTitleScreening for cancer of the uterine cervix in Iceland 1965–1978 Acta Obstet Gynecol Scand 61 199–203 Occurrence Handle1:STN:280:BiyD3Mfps1Y%3D Occurrence Handle7124352
K Sigurdsson (1993) ArticleTitleEffect of organized screening on the risk of cervical cancer: evaluation of screening activity in Iceland, 1964–1991 Int J Cancer 54 563–570 Occurrence Handle1:STN:280:ByyB1MzjslY%3D Occurrence Handle8514448
N Day (1984) ArticleTitleEffect of cervical cancer screening in Scandinavia Obstet Gynecol 63 714–718 Occurrence Handle1:STN:280:BiuC1M3jtlE%3D Occurrence Handle6717876
M Hakama K Louhivuori (1988) ArticleTitleA screening programme for cervical cancer that worked Cancer Surv 7 403–416 Occurrence Handle1:STN:280:BiaB3cflvVU%3D Occurrence Handle3242792
DM Parkin X Nguyen-Dinh NE Day (1985) ArticleTitleThe impact of screening on the incidence of cervical cancer in England and Wales Br J Obstet Gynaecol 92 150–157 Occurrence Handle1:STN:280:BiqC383mtVY%3D Occurrence Handle3970894
JE Macgregor KM Campbell EMF Mann KY Swanson (1994) ArticleTitleScreening for cervical intraepithelial neoplasia in north east Scotland shows fall in incidence and mortality from invasive cancer with concomitant rise in preinvasive disease BMJ 308 1407–1411 Occurrence Handle1:STN:280:ByuB1M%2FhtlY%3D Occurrence Handle8019250
L Gibson DJ Spiegelhalter C Camilleri-Ferrante et al. (1997) ArticleTitleTrends in invasive cervical cancer incidence in East Anglia from 1971 to 1993 J Med Screen 4 44–48 Occurrence Handle1:STN:280:ByiA2czltVM%3D Occurrence Handle9200063
M Quinn P Babb J Jones A Allen (1999) ArticleTitleEffect of screening on incidence of and mortality from cancer of the cervix in England: evaluation based on routinely collected statistic BMJ 318 IssueID7188 904–908 Occurrence Handle1:STN:280:DyaK1M3jtVCqsw%3D%3D Occurrence Handle10102852
J Peto C Gilham O Fletcher FE Matthews (2004) ArticleTitleThe cervical cancer epidemic that screening has prevented in the UK Lancet 364 IssueID9430 249–256 Occurrence Handle10.1016/S0140-6736(04)16674-9 Occurrence Handle15262102
S Liu R Semenciw A Probert Y Mao (2001) ArticleTitleCervical cancer in Canada: changing patterns in incidence and mortality Int J Gynecol Cancer 11 IssueID1 24–31 Occurrence Handle10.1046/j.1525-1438.2001.011001024.x Occurrence Handle1:STN:280:DC%2BD3M3gtVSjuw%3D%3D Occurrence Handle11285030
E Laara NE Day M Hakama (1987) ArticleTitleTrends in mortality from cervical cancer in the Nordic countries: association with organised screening programmes Lancet 1 IssueID8544 1247–1249 Occurrence Handle1:STN:280:BiiB38jmslA%3D Occurrence Handle2884378
T Aareleid E Pukkala H Thomson et al. (1993) ArticleTitleCervical cancer incidence and mortality trends in Finland and Estonia: a screened vs. an unscreened population Eur J Cancer 29 745–749 Occurrence Handle10.1016/S0959-8049(05)80359-4
K Sigurdsson (1999) ArticleTitleThe Icelandic and Nordic cervical screening programs: trends in incidence and mortality rates through 1995 Acta Obstet Gynecol Scand 78 478–485 Occurrence Handle1:STN:280:DyaK1Mzgtlenuw%3D%3D Occurrence Handle10376856
M McCredie MS Coates JM Ford (1989) ArticleTitleTrends in invasive cancer of the cervix uteri in New South Wales, 1973–1982 Aust NZ J Obstet Gynaecol 29 335–339 Occurrence Handle1:STN:280:By%2BC2cjktFI%3D
M McCredie M Coates T Churches (1990) Cancer of the Cervix Uteri: New South Wales, Australian Capital Territory 1972–1987 Cancer Epidemiology Research Unit and NSW Central Cancer Registry, NSW Cancer Council Sydney
A Kricker J Bell M Coates R Taylor B Armstrong (1996) Cancer of the Cervix in NSW 1972 to 1992 Cancer Epidemiology Research Unit and NSW Central Cancer Registry, NSW Cancer Council Sydney
R Taylor J Bell M Coates T Churches G Wain (1996) ArticleTitleCervical cancer in New South Wales women: five-year survival, 1972 to 1991 ANZ J Pub Health 20 IssueID4 413–420 Occurrence Handle1:STN:280:ByiD28ritF0%3D
Australian Institute of Health and Welfare [AIHW] (1998) Breast and cervical cancer screening in Australia 1996–1997. AIHW Cat. No. CAN 3 (Cancer Series Number 8). AIHW Canberra
New South Wales Cervical Screening Program and NSW Pap Test Register [NSW CSP/PTR] (1999) Cervical cancer screening in New South Wales: First Annual Statistical report 1997. NSW Health Department, Sydney. http://www.csp.nsw.gov.au
Coates M, et al. (1992–1998) Cancer in NSW, Incidence and Mortality [1990–1995, annual reports]. NSW Central Cancer Registry and Cancer Control Information Centre, NSW Cancer Council and NSW Health Department
Tracey E, et al. (2003) Cancer in NSW, Incidence and Mortality 2001 [2001 annual report]. NSW Central Cancer Registry, Cancer Research and Registers Division; NSW Cancer Council; and NSW Health Department
R Taylor S Morrell H Mamoon G Wain (2001) ArticleTitleThe effect of screening on cervical cancer incidence and mortality in New South Wales implied by influences of period of diagnosis and birth cohort J Epi Com Hlth 55 782–788 Occurrence Handle1:STN:280:DC%2BD3MrlvVWmtA%3D%3D
C Muir J Waterhouse T Mack et al. (1987) Cancer Incidence in Five Continents NumberInSeriesVol. V International Agency for Research on Cancer Lyon 45
P Armitage G Berry (1994) Statistical Methods in Medical Research EditionNumber3 Blackwell Scientific Publications Oxford
XQ Yu DL O'Connell RW Gibberd DP Smith BK Armstrong (2003) Cancer Survival, Incidence and Mortality by Area Health Service in NSW 1994–2000 NSW Cancer Council Sydney
New South Wales Cervical Screening Program and NSW Pap Test Register [NSW CSP/PTR] (2003) Cervical cancer screening in New South Wales: Annual Statistical report 2002. NSW Health Department, Sydney. http://www.csp.nsw.gov.au
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taylor, R., Morrell, S., Mamoon, H. et al. Decline in Cervical Cancer Incidence and Mortality in New South Wales in Relation to Control Activities (Australia). Cancer Causes Control 17, 299–306 (2006). https://doi.org/10.1007/s10552-005-0515-z
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10552-005-0515-z