Abstract
Background
Endocrine resistant metastatic disease develops in ~ 20–25% of hormone-receptor-positive (HR+) breast cancer (BC) patients despite endocrine therapy (ET) use. Upregulation of HER family receptor tyrosine kinases (RTKs) represent escape mechanisms in response to ET in some HR+ tumors. Short-term neoadjuvant ET (NET) offers the opportunity to identify early endocrine escape mechanisms initiated in individual tumors.
Methods
This was a single arm, interventional phase II clinical trial evaluating 4 weeks (± 1 week) of NET in patients with early-stage HR+/HER2-negative (HER2-) BC. The primary objective was to assess NET-induced changes in HER1-4 proteins by immunohistochemistry (IHC) score. Protein upregulation was defined as an increase of ≥ 1 in IHC score following NET.
Results
Thirty-seven patients with cT1-T3, cN0, HR+/HER2- BC were enrolled. In 35 patients with evaluable tumor HER protein after NET, HER2 was upregulated in 48.6% (17/35; p = 0.025), with HER2-positive status (IHC 3+ or FISH-amplified) detected in three patients at surgery, who were recommended adjuvant trastuzumab-based therapy. Downregulation of HER3 and/or HER4 protein was detected in 54.2% of tumors, whereas HER1 protein remained low and unchanged in all cases. While no significant volumetric reduction was detected radiographically after short-term NET, significant reduction in tumor proliferation rates were observed. No significant associations were identified between any clinicopathologic covariates and changes in HER1-4 protein expression on multivariable analysis.
Conclusion
Short-term NET frequently and preferentially upregulates HER2 over other HER family RTKs in early-stage HR+/HER2- BC and may be a promising strategy to identify tumors that utilize HER2 as an early endocrine escape pathway.
Clinical trial registry
Trial registration number: NCT03219476.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adjuvant endocrine therapy (ET) provides significant recurrence-risk reduction as well as survival benefit to patients with hormone-receptor-positive (HR+) breast cancer (BC). However, metastatic recurrences of endocrine resistant disease occur in about 20–25% of patients and remain a major cause of breast cancer mortality [1, 2]. There is a continuum from early to late mechanisms of endocrine resistance in HR+ BC, with some tumors exhibiting de novo resistance to endocrine treatments, while other tumors acquire resistance after an initial response [3, 4]. Early escape and survival mechanisms of HR+ BC in response to ET involve adaptive upregulation of growth factor receptor tyrosine kinases (RTKs), which promotes ligand-independent activation of estrogen receptors (ER) through MAP kinase signaling and phosphorylation of Ser11 of ER [5,6,7]. RTKs commonly upregulated in response to ET are members of the human epidermal growth factor receptor (HER) family, especially HER2 and epidermal growth factor receptor (EGFR)/HER1, but also HER3 and HER4, as well as FGFR1 [4,5,6,7,8]. In a study of 240 metastatic HR+ /HER2- BC patients on first-line ET, 25% converted to HER2-positive status at progression and had significantly shorter overall survival [9]. In another study, HER2 status switching, i.e. ERBB2 gene amplification and/or overexpression, was observed in 12% (3/26) of HR+/HER2- tumors that became tamoxifen-resistant [10]. Intrinsic subtype switching with acquired HER2-positive status has also been reported in ~ 20% of metastatic recurrences of HER2- primary tumors [11].
Neoadjuvant endocrine therapy (NET) can be used to downstage HR+ tumors to potentially de-escalate surgery (increase rates of breast-conserving surgery; decrease rates of axillary node dissection in node-positive disease) [12,13,14,15] in patients not felt to be ideal candidates for upfront chemotherapy. However, NET has more recently emerged as a strategy to assess changes in the tumor microenvironment and emerging resistance pathways as well as to determine tumor responses to additive targeted therapies in the neoadjuvant setting [16,17,18]. Most NET studies have included at least 3 months of treatment for tumor response assessments, however, changes in tumor proliferation have been reported as early as 2 weeks post-NET [19].
Understanding and characterizing the underlying molecular features of endocrine resistance for more accurate response prediction and optimal clinical management to improve patient outcomes is of the utmost importance. Major clinical challenges to overcome late resistance include broad cancer cell heterogeneity and genetic diversity in advanced metastatic setting. Tailored targeting of early endocrine escape mechanisms used by individual HR+ tumors, when metastatic burden is clinically undetectable and with lower genetic heterogeneity, will likely be more effective than later treatment directed at recurrent clinically overt metastases.
DESTINY Breast04 [20], a recent landmark study showed significant improvement in long term outcomes with HER2-directed therapy in patients with metastatic ‘HER2-low’ BC, which has traditionally been treated as HER2- BC. Given these findings, it is imperative to identify patients who may benefit from HER2-directed therapies. To identify targetable early endocrine escape mechanisms and potential candidates for HER2-directed therapies, we performed an interventional phase II clinical trial to assess molecular changes and tumor responses in early-stage HR+/HER2- BC patients treated with short-term NET, with the primary objective of measuring changes in HER1-4 protein levels with NET.
Methods
Study design and patients
A phase II single arm, interventional clinical trial was completed to evaluate changes in molecular biology and tumor responses in patients treated with short-term NET. The primary objective of the study was to assess NET-induced changes in HER1-4 protein expression levels in tumors, and their association with post-NET cancer cell proliferation rate dichotomized Ki-67 positivity as low (< 10%) or high (≥ 10%). Secondary objectives included assessment of radiographic responses and other molecular markers. We enrolled women aged 18 years or older with HR+/HER2- BC with histologically confirmed operable and clinically or radiographically measurable lesions (cT1-T3, cN0, cM0). Estrogen and/or progesterone receptor positivity was defined as ≥ 1% nuclear staining by immunohistochemistry (IHC) and HER2/neu-negative by IHC or fluorescence in situ hybridization (FISH) according to the current ASCO/CAP guidelines [21, 22]. Patients had to have an ECOG performance status of ≤ 2. Patients with bilateral BC and those with multifocal or multicentric disease were eligible. Patients were excluded if they had lymph node-positive or distant metastatic BC, purely noninvasive BC (i.e., ductal carcinoma in situ, lobular carcinoma in situ), HER2-positive BC, history of any malignancy except non-melanomatous skin cancer or carcinoma in situ of the cervix within 2 years, or were pregnant or actively breast feeding. All patients provided written informed consent. This study was performed in line with the principles of the Declaration of Helsinki. The Institutional Review Board and the Protocol Review and Monitoring Committee of the Medical College of Wisconsin approved the study.
Procedures
Patients were treated with NET for 4 weeks (± 1 week) prior to surgery, with dosing continuing until the day of surgery (± 2 days). Choice of NET regimen [tamoxifen or aromatase inhibitors (AIs)], based on menopausal status, medical conditions and patient preference, was at the discretion of the treating physicians. Standard daily dosing was used without any dose reductions or modifications (tamoxifen 20 mg, anastrozole 1 mg, letrozole 2.5 mg, exemestane 25 mg). Ovarian suppression with gonadotropin-releasing hormone (GnRH) analogues was allowed for premenopausal women. Cytochrome P450 2D6 (CYP2D6) inhibitors were prohibited with tamoxifen use. Initial diagnostic core biopsies were used for pre-treatment biomarker assessments and surgical tumor specimens were used for post-treatment assessments. Study Schema is shown in Fig. 1. Patients were followed for 30 days after surgery to record any adverse events from treatment. Adverse events were assessed according to Common Terminology Criteria for Adverse Events version 5.0. After tumor resection, patients were treated with radiation and/or chemotherapy according to standard-of-care treatment guidelines. Pre-NET biopsy specimens were used for OncotypeDx testing to aid in adjuvant chemotherapy decision making when indicated. ET will continue in the adjuvant setting for a period of at least 5 years. Patients will be followed for at least five years from completion of study to assess patient outcomes, i.e., ipsilateral, contralateral or distant recurrences.
Clinical assessments
Patients underwent diagnostic breast mammography and ultrasonography at the time of diagnosis and again within 5 days prior to surgery. For clinical radiographic tumor measurements, the largest bi-dimensional measurements and when possible, three-dimensional measurements were recorded. Radiographic tumor responses were assessed using World Health Organization Response Evaluation Criteria in Solid Tumors (WHO) [23, 24]: Complete response (disappearance of tumor), Partial response (≥ 50% decrease in the product of the bi-dimensional measurements of the tumor), No change (50% decrease in total tumor size cannot be established nor has a 25% increase in the size of the lesion been demonstrated), or Progressive disease (≥ 25% or greater increase in the total tumor size). Given our study included cT1a and cT1b tumors, we elected to use WHO criteria for radiographic response assessment. WHO criteria have been used in multiple prior neoadjuvant endocrine therapy clinical trials to capture responses in smaller tumors [25,26,27].
Pathology assessments
Among the 37 patients, one patient had pathological complete response (pCR) and a second patient had too few residual cancer cells post-NET to measure HER proteins. Analyses of paired molecular tumor data on pre- and post-NET specimens were therefore limited to 35 patients. Standardized immunohistochemistry (IHC) protocols for estrogen receptor (ER) (6F11, Leica Biosystems, Buffalo Grove, IL), progesterone receptor (PR) (16, Leica Biosystems, Buffalo Grove, IL), HER1 (EGFR H11, Agilent, Santa Clara, CA), HER2 (4B5, Ventana, Roche Diagnostics, Indianapolis, IN), HER3 (HER3, Cell signaling, Danvers, MA) and HER4 (erbB4/HER4, MilliporeSigma, Burlington, MA) as well as HER2 dual probe FISH (PathVysion, Abbott, Abbott Park, IL) testing if HER2 IHC score was equivocal (2+), were performed in a College of American Pathologists (CAP)-accredited laboratory and all stains were visually evaluated by a board certified breast pathologist (JMJ) to assess biomarker status in the pre- and post-treatment tumor specimens. IHC for HER1 (EGFR), HER3 and HER4 was interpreted visually, with HER1 IHC interpreted as positive if there was membranous staining and HER3 and HER4 interpreted as positive if there was cytoplasmic and/or membranous staining, with 0 being negative (< 1%) and 1+ , 2+ or 3+ scores matching the intensity and cutoffs (10% tumor staining) used by the current HER2 guidelines [22]. HER1-4 protein upregulation was defined as an increase of ≥ 1 in IHC score (ordinal 0, 1, 2, 3), whereas downregulation conversely was defined as a decrease of ≥ 1 in IHC score.
Histopathological responses were assessed by change in tumor proliferation and cellularity. Tumor proliferation protein Ki-67 (MIB-1, Agilent, Santa Clara, CA) on pre- and post-treatment specimens was assessed by quantitative IHC. For Ki-67 quantification image analysis, QuPath (version 0.3.0, build 2021) software (Queen’s University Belfast, Belfast, Northern Ireland; https://qupath.github.io) was used for the cell detection, segmentation, objective classification (cancer and stroma) and determination of the percent of Ki-67-positive cancer cells. Tumor cellularity and tumor infiltrating lymphocytes (TILs) in pre- and post-treatment tumor specimens were assessed visually by pathologist according to Residual Cancer Burden guidelines [28] and the International TILs Working Group guidelines [29], respectively.
Statistical analyses
We planned a sample size of 37 patients to achieve at least 80% power at significance level of 0.05, when testing the one-sided one sample hypothesis that the proportion of tumors with NET-associated upregulation of one or more HER proteins (HER1-4) is at least 50% versus the null hypothesis that the proportion is no larger than 30%. One patient had two ipsilateral HR+ tumors with distinct histologies. Since two tumors in one patient cannot be regarded as independent, biostatistician blinded to marker data determined that the tumor with highest post vs. pre-NET HER1-4 protein change should be included in the analyses, with larger tumor size serving as a second selection criterion in case of a tie. Chi-square, Wilcoxon rank-sum tests and t-tests were performed where appropriate. Linear regression multivariable analysis was performed to evaluate the association of covariates (age, BMI, menstrual status, tumor grade, histology, pre- and post-NET changes in tumor size, Ki67, ER%, PR%, cellularity and TILs) with the primary outcome of changes in HER1-4 protein levels. All analyses were performed using SAS version 9.4 (Cary, NC).
Results
Patient characteristics
Between March 2018 and February 2020, 37 women diagnosed with localized invasive HR+/HER2- BC were enrolled. Patient and pretreatment tumor characteristics are summarized in Table 1. Most patients were post-menopausal (83.8%). Median age at diagnosis was 64 years (range 42–81) and median BMI was 28.3 kg/m2 (19.3–55.1). Overall, the majority of tumors were grade 1 (42.1%) or grade 2 (47.4%) and had ductal histology (70%). Median tumor size clinically at diagnosis was 1.3 cm (0.5–7.7). Median pathological tumor size at surgery was 1.2 cm (0.0–4.0). One patient had a complete pathologic response (pCR) at surgery with no residual tumor tissue available while another patient had pT1mi disease resulting in material insufficient for repeat HER1-4 testing, resulting in paired pre- and post-NET tumor HER1-4 tumor assessments for 35 patients. One patient had two ipsilateral HR+ tumors with distinct histology (invasive ductal carcinoma and invasive lobular carcinoma; see Statistical Methods section). Seven patients had pN1 disease at surgery (six with 1 lymph node involved, one with pN1mi). OncotypeDx® Recurrence Score (RS) was performed on diagnostic core biopsies in 27 patients with low RS (≤ 15) in 10 patients, intermediate RS (16–25) in 8 patients and high RS (≥ 26) in 9 patients.
NET-associated upregulation of HER1-4 protein expression
IHC scoring was used to identify patients with tumors displaying upregulation of HER1-4 protein levels in cancer cells from pre-NET biopsies to post-NET surgical resections. Collectively, upregulation of one or more of the HER proteins in tumors after ~ 4 weeks of NET were detected in 17 of the 35 patients with evaluable tumors (48.6%; p = 0.025; exact binomial 95% CI of 31.4–66.0%; Figs. 2, 3, Supplementary Table 1). Intriguingly, HER2 was upregulated in all 17 cases that had upregulation of any HER protein, with dual upregulation of HER3 in one case, dual upregulation of HER4 in another case, while HER1 protein levels were low and remained unchanged in all 35 cases. In contrast, HER2 protein downregulation was observed in only two cases (2/35; 5.7%), while HER3 and HER4 proteins were each downregulated in 19 cases (54.2%). Bivariate Spearman rank correlation revealed no significant associations between changes in HER1-4 protein scores after short-term NET. In addition to upregulation of HER2 protein in 17 cases, one additional tumor with equivocal HER2 IHC score of 2+ both pre- and post-NET showed ERBB2 gene amplification post-NET. In total, three of the 35 patients (8.6%) with evaluable HER2 scores pre- and post-NET converted from HER2-negative to HER2-positive status (IHC 3+ or FISH-amplified) at surgery and were recommended adjuvant trastuzumab-based treatment. Of the 14 cases with HER2 IHC score of 0 at baseline, post-NET 10 cases upregulated to IHC 1+ or 2+ , qualifying as “HER2-low”. No significant associations were identified between any clinicopathologic covariates and changes in HER1-4 protein expression on multivariable analysis.
Examples of upregulation of HER family of proteins by immunohistochemistry in early-stage HR+/HER2- breast cancer before and after short-term neoadjuvant endocrine therapy. A, B - HER1/EGFR, C, D - HER2, E, F - HER3, and G, H - HER4. Note: although minor emergence of HER1/EGFR expression was observed, in no case was HER1- positive cells >1%
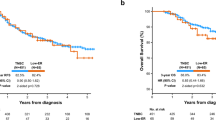
NET-associated changes in Ki-67 and PR
Significant reductions in cancer cell proliferation rates were induced by short-term NET, with median Ki-67-positivity of 9.7% before treatment and 4.5% after treatment (p < 0.001; Fig. 4A). NET led to a decrease in tumor Ki-67-positivity in 74.3% of cases [median decrease of 3.14 percentage points (range 0.22–37.8)] and an increase in 25.7% of tumors [median increase of 1.29 percentage points (range 0.37–5.32)]. High cancer cell Ki-67-positivity ≥ 10% was only detected in 3 cases (8.6%) post-NET and was not associated with changes in HER protein levels. Intermediate tumor Ki-67-positivity between 2.7 and 10% was observed in 21 cases (60.0%) post-NET, whereas Ki-67-positivity was ≤ 2.7% in 11 cases (31.4%), consistent with complete cell cycle arrest [19]. While median ER-positivity remained unchanged at 98% between pre- and post-treatment specimens, median PR-positivity was reduced from 80.0 to 40.0% after short-term NET (p < 0.001, Fig. 4B), consistent with functional ER pathway disruption.
Radiographic responses
Median tumor size change was − 7.6% (range − 60.3–44.3) by ultrasonography and − 5.8% (range – 49–59) by mammography with short-term NET, however, these changes were not statistically nor clinically significant (p = 0.83 and p = 0.85, respectively). Pre-treatment low tumor grade and PR-positivity were significantly associated with tumor volume reduction radiographically (p = 0.006 and p = 0.02 respectively), while higher OncotypeDx RS was a negative predictor of radiographic response (p = 0.02). No significant correlation of radiographic response was detected with changes in HER1-4 scores. When assessed by WHO criteria, most patients had no change on radiographic response assessment, one had a partial response and 3 patients had disease progression.
Adverse events
NET was associated with a favorable toxicity profile. No adverse events (AEs) ≥ grade 3 were seen in this study. Incidence of grade 1 and 2 AEs were low (2.7% and 5.5%, respectively) and included arthralgias, insomnia, fatigue, hot flashes, nausea, constipation, and headaches. No discontinuation due to AEs or complications were seen.
Discussion
In this study, we treated 37 women with early-stage HR+/HER2- BC with short-term NET. Paired specimens for pre- and post-NET tumor HER1-4 assessments were available for 35 tumors and we identified upregulation of HER2 protein in 17 tumors (48.5%), including two that converted to HER2 IHC3+ status at surgery. In addition, one additional tumor with equivocal HER2 IHC score of 2+ both pre- and post-NET showed ERBB2 gene amplification post-NET. The ERBB2 gene amplification uncovered after short-term NET in this tumor is assumed to represent tumor heterogeneity with pre-existing HER2 gene amplification that was likely not captured in the smaller biopsy sample. Regardless, HER2 analyses after short-term NET identified a total of three patients (8.6%) that were recommended adjuvant trastuzumab-based chemotherapy. In contrast to the observed frequent upregulation of HER2 protein, short-term NET was associated with frequent downregulation of protein levels of HER3 and/or HER4 in more than half of the cases, while upregulation of either HER3 or HER4 protein was rare. HER1/EGFR protein levels were low and generally remained unchanged in these early-stage HR+ tumors.
Significant and selective upregulation of HER2 protein, in response to short-term NET is suggestive of compensatory activation of HER2-signaling in nearly half of the HR+/HER2- tumors. This finding is important because signaling via HER2 alone or with its dimerization partners HER1 or HER3 represents a well-established endocrine resistance mechanism based on experimental studies of HR+ breast cancer cell lines [30], in vivo tumor studies [31], and most importantly by frequent HER2-upregulation in recurrent metastases after anti-estrogen therapy [10, 32,33,34,35]. The ExteNET trial showed that 1 year of treatment with neratinib, an irreversible pan-HER tyrosine kinase inhibitor (TKI), significantly improved invasive disease-free survival (iDFS) after trastuzumab-based adjuvant therapy primarily in women with HR+ HER2-positive breast cancer [36,37,38]. The observed efficacy of neratinib in the HR+/HER2-positive cohort (most of whom were receiving concurrent ET) may be attributed to the effective inhibition of cross-talk between HER2 and estrogen receptors, a known mechanism of resistance in HR+/HER2-positive tumors [39]. Our study provides further insight into interactions between ER and HER2 pathways. Whether HER2-directed therapies, including TKIs would reduce metastatic recurrences in HR+ tumors that gain intermediate HER2 expression levels post-NET, remains to be determined, however, further investigation is warranted. Likewise, HR+/HER2-positive tumors have poor prognosis compared to HR+/HER2- tumors and frequently display inherent or rapidly acquired endocrine resistance [40, 41]. While HR+/HER2-positive tumors clinically respond at least as well to NET as HR+/HER2- tumors in terms of volumetric reduction [42, 43], data from two clinical trials of standard NET of 4–6 month duration showed that cancer cell proliferation rates (Ki-67-positivity) after NET remained significantly higher in ER+ /HER2-positive tumors [44].
The tumor proliferation marker Ki-67 is a useful and reliable measure of early response or resistance to treatment and is being used in NET trials to guide developmental therapeutics. Reduction in Ki-67 as early as 2 weeks post-NET has been reported in endocrine sensitive tumors while endocrine resistant tumors had a less impressive reduction highlighting the sensitivity of Ki-67 measurements in NET response assessments [19, 45, 46]. The IMPACT trial [26] showed a statistically significant 85% reduction of mean cancer cell Ki-67 positivity rate in the HER2-negative group compared to a 45% reduction in the HER2-positive group despite good clinical responses seen in the HER2-positive group, which suggests rapid emergence of HER2-mediated resistance. While short-term NET was associated with significant reductions in Ki-67 in our study, no statistically significant associations between post-NET Ki-67 and levels of HER2 or other HER family protein levels were seen. Based on the observations of frequent upregulation of HER2 in HR+/HER2- BC, short-term NET while patients are awaiting surgery may therefore identify HR+/HER2- tumors that engage HER2-signaling to overcome ET.
In this study, downregulation in both HER3 and/or HER4 was seen in 54.2% of tumors in response to short-term NET. HER3 overexpression has been associated with HER2-mediated tamoxifen resistance in preclinical and clinical studies and downregulation of HER3 has been shown to inhibit HER2-associated proliferation and tumorigenesis [34]. Nuclear HER4 intracellular domain (ICD) functions as a potent ER co-activator and promotes the proliferation of ER+ breast tumor cells [47] whereas cytosolic HER4 ICD has antiproliferative and pro-apoptotic activity including tamoxifen-induced apoptosis [48]. Pre-clinical studies have shown that the presence of HER4 in HER2-positive BC cells results in reduced proliferation and increased apoptosis, possibly indicating that HER4 antagonizes HER2-signaling activity [49, 50]. Consequently, loss of HER4 may be associated with tamoxifen resistance in patients with BC. The significance of HER3 and HER4 downregulation will require further study.
Limitations of our study include small sample size and the possibility of tumor heterogeneity, clonality, and tissue biopsy sampling impacting the histological results. It is conceivable that in select cases there was pre-existing focal HER2-positive disease that was not detected by biopsy sampling. However, upregulation of HER2 protein in almost half of the cohort is unlikely to be secondary to tumor heterogeneity or tissue biopsy sampling differences.
In conclusion, this pilot study demonstrates the possibility of identifying early endocrine resistance mechanisms using a cost-effective, well-tolerated and practical strategy of short-term NET. This finding creates an opportunity for in vivo analysis of the tumor microenvironment and exploration of biomarker development to provide personalized care by tailoring adjuvant treatments and improving patient outcomes.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jemal A, Bray F, Center MM et al (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Youlden DR, Cramb SM, Dunn NA et al (2012) The descriptive epidemiology of female breast cancer: an international comparison of screening, incidence, survival and mortality. Cancer Epidemiol 36:237–248
Razavi P, Chang MT, Xu G et al (2018) The genomic landscape of endocrine-resistant advanced breast cancers. Cancer Cell 34:427-438 e6
Osborne CK, Schiff R (2011) Mechanisms of endocrine resistance in breast cancer. Annu Rev Med 62:233–247
Clarke R, Tyson JJ, Dixon JM (2015) Endocrine resistance in breast cancer—An overview and update. Mol Cell Endocrinol 418(Pt 3):220–234
Ma CX, Reinert T, Chmielewska I et al (2015) Mechanisms of aromatase inhibitor resistance. Nat Rev Cancer 15:261–275
Zilli M, Grassadonia A, Tinari N et al (2009) Molecular mechanisms of endocrine resistance and their implication in the therapy of breast cancer. Biochim Biophys Acta 1795:62–81
Girault I, Bieche I, Lidereau R (2006) Role of estrogen receptor alpha transcriptional coregulators in tamoxifen resistance in breast cancer. Maturitas 54:342–351
Lipton A, Leitzel K, Ali SM et al (2005) Serum HER-2/neu conversion to positive at the time of disease progression in patients with breast carcinoma on hormone therapy. Cancer 104:257–263
Gutierrez MC, Detre S, Johnston S et al (2005) Molecular changes in tamoxifen-resistant breast cancer: relationship between estrogen receptor, HER-2, and p38 mitogen-activated protein kinase. J Clin Oncol 23:2469–2476
Priedigkeit N, Hartmaier RJ, Chen Y et al (2017) Intrinsic subtype switching and acquired ERBB2/HER2 amplifications and mutations in breast cancer brain metastases. JAMA Oncol 3:666–671
Banys-Paluchowski M, Gasparri ML, de Boniface J et al (2021) Surgical management of the axilla in clinically node-positive breast cancer patients converting to clinical node negativity through neoadjuvant chemotherapy: current status, knowledge gaps, and rationale for the EUBREAST-03 AXSANA Study. Cancers. https://doi.org/10.3390/cancers13071565
Kantor O, Wakeman M, Weiss A et al (2021) Axillary management after neoadjuvant endocrine therapy for hormone receptor-positive breast cancer. Ann Surg Oncol 28:1358–1367
Montagna G, Sevilimedu V, Fornier M et al (2020) How effective is neoadjuvant endocrine therapy (NET) in downstaging the axilla and achieving breast-conserving surgery? Ann Surg Oncol 27:4702–4710
Murphy BM, Hoskin TL, Degnim AC et al (2021) Surgical management of axilla following neoadjuvant endocrine therapy. Ann Surg Oncol 28:8729–8739
Ellis MJ, Tao Y, Luo J et al (2008) Outcome prediction for estrogen receptor-positive breast cancer based on postneoadjuvant endocrine therapy tumor characteristics. J Natl Cancer Inst 100:1380–1388
Ellis MJ, Suman VJ, Hoog J et al (2017) Ki67 proliferation index as a tool for chemotherapy decisions during and after neoadjuvant aromatase inhibitor treatment of breast cancer: results from the american college of surgeons oncology group Z1031 trial (Alliance). J Clin Oncol. https://doi.org/10.1200/JCO.2016.69.4406
Guerrero-Zotano AL, Arteaga CL (2017) Neoadjuvant trials in ER+ breast cancer: a tool for acceleration of drug development and discovery. Cancer Discov 7:561–574
Johnston S, Puhalla S, Wheatley D et al (2019) Randomized phase II study evaluating palbociclib in addition to letrozole as neoadjuvant therapy in estrogen receptor-positive early breast cancer: PALLET Trial. J Clin Oncol 37:178–189
Modi S, Jacot W, Yamashita T et al (2022) Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med 387:9–20
Allison KH, Hammond MEH, Dowsett M et al (2020) Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol 38:1346–1366
Wolff AC, Hammond MEH, Allison KH et al (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American Society of clinical oncology/college of american pathologists clinical practice guideline focused update. J Clin Oncol 36:2105–2122
World Health Organization (1979) WHO handbook for reporting results of cancer treatment. WHO offset publication 48, Geneva
Miller AB, Hoogstraten B, Staquet M et al (1981) Reporting results of cancer treatment. Cancer 47:207–214
Eiermann W, Paepke S, Appfelstaedt J et al (2001) Preoperative treatment of postmenopausal breast cancer patients with letrozole: a randomized double-blind multicenter study. Ann Oncol 12:1527–1532
Smith IE, Dowsett M, Ebbs SR et al (2005) Neoadjuvant treatment of postmenopausal breast cancer with anastrozole, tamoxifen, or both in combination: the Immediate Preoperative Anastrozole, Tamoxifen, or Combined with Tamoxifen (IMPACT) multicenter double-blind randomized trial. J Clin Oncol 23:5108–5116
Ellis MJ, Suman VJ, Hoog J et al (2011) Randomized phase II neoadjuvant comparison between letrozole, anastrozole, and exemestane for postmenopausal women with estrogen receptor-rich stage 2 to 3 breast cancer: clinical and biomarker outcomes and predictive value of the baseline PAM50-based intrinsic subtype–ACOSOG Z1031. J Clin Oncol 29:2342–2349
Dieci MV, Radosevic-Robin N, Fineberg S, van den Eynden G, Ternes N, Penault-Llorca F, Pruneri G, D'Alfonso TM, Demaria S, Castaneda C, Sanchez J, Badve S, Michiels S, Bossuyt V, Rojo F, Singh B, Nielsen T, Viale G, Kim SR, Hewitt S, Wienert S, Loibl S, Rimm D, Symmans F, Denkert C, Adams S, Loi S, Salgado R, International Immuno-Oncology Biomarker Working Group on Breast Cancer (2018) Update on tumor-infiltrating lymphocytes (TILs) in breast cancer, including recommendations to assess TILs in residual disease after neoadjuvant therapy and in carcinoma in situ: a report of the International Immuno-Oncology Biomarker Working Group on Breast Cancer. Semin Cancer Biol 52(Pt 2):16–25. https://doi.org/10.1016/j.semcancer.2017.10.003
Salgado R, Denkert C, Demaria S et al (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 26:259–271
Shou J, Massarweh S, Osborne CK et al (2004) Mechanisms of tamoxifen resistance: increased estrogen receptor-HER2/neu cross-talk in ER/HER2-positive breast cancer. J Natl Cancer Inst 96:926–935
Sun Y, Yang N, Utama FE et al (2021) NSG-Pro mouse model for uncovering resistance mechanisms and unique vulnerabilities in human luminal breast cancers. Sci Adv 7:eabc8145
Dowsett M (2001) Overexpression of HER-2 as a resistance mechanism to hormonal therapy for breast cancer. Endocr Relat Cancer 8:191–195
Nicholson RI, Hutcheson IR, Harper ME et al (2001) Modulation of epidermal growth factor receptor in endocrine-resistant, oestrogen receptor-positive breast cancer. Endocr Relat Cancer 8:175–182
Liu B, Ordonez-Ercan D, Fan Z et al (2007) Downregulation of erbB3 abrogates erbB2-mediated tamoxifen resistance in breast cancer cells. Int J Cancer 120:1874–1882
Selli C, Turnbull AK, Pearce DA et al (2019) Molecular changes during extended neoadjuvant letrozole treatment of breast cancer: distinguishing acquired resistance from dormant tumours. Breast Cancer Res 21:2
Chan A, Delaloge S, Holmes FA et al (2016) Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 17:367–377
Martin M, Holmes FA, Ejlertsen B et al (2017) Neratinib after trastuzumab-based adjuvant therapy in HER2-positive breast cancer (ExteNET): 5-year analysis of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 18:1688–1700
Chan A, Moy B, Mansi J et al (2021) Final efficacy results of neratinib in HER2-positive hormone receptor-positive early-stage breast cancer from the phase III ExteNET trial. Clin Breast Cancer 21:80-91 e7
Johnston SR (2010) New strategies in estrogen receptor-positive breast cancer. Clin Cancer Res 16:1979–1987
Brinkman JA, El-Ashry D (2009) ER re-expression and re-sensitization to endocrine therapies in ER-negative breast cancers. J Mammary Gland Biol Neoplasia 14:67–78
Lopez-Tarruella S, Schiff R (2007) The dynamics of estrogen receptor status in breast cancer: re-shaping the paradigm. Clin Cancer Res 13:6921–6925
Ellis MJ, Coop A, Singh B et al (2001) Letrozole is more effective neoadjuvant endocrine therapy than tamoxifen for ErbB-1- and/or ErbB-2-positive, estrogen receptor-positive primary breast cancer: evidence from a phase III randomized trial. J Clin Oncol 19:3808–3816
Zhu L, Chow LW, Loo WT et al (2004) Her2/neu expression predicts the response to antiaromatase neoadjuvant therapy in primary breast cancer: subgroup analysis from celecoxib antiaromatase neoadjuvant trial. Clin Cancer Res 10:4639–4644
Ellis MJ, Tao Y, Young O et al (2006) Estrogen-independent proliferation is present in estrogen-receptor HER2-positive primary breast cancer after neoadjuvant letrozole. J Clin Oncol 24:3019–3025
Dowsett M, Kilburn L, Rimawi MF et al (2022) Biomarkers of response and resistance to palbociclib plus letrozole in patients with ER(+)/HER2(-) breast cancer. Clin Cancer Res 28:163–174
Smith I, Robertson J, Kilburn L et al (2020) Long-term outcome and prognostic value of Ki67 after perioperative endocrine therapy in postmenopausal women with hormone-sensitive early breast cancer (POETIC): an open-label, multicentre, parallel-group, randomised, phase 3 trial. Lancet Oncol 21:1443–1454
Zhu Y, Sullivan LL, Nair SS et al (2006) Coregulation of estrogen receptor by ERBB4/HER4 establishes a growth-promoting autocrine signal in breast tumor cells. Cancer Res 66:7991–7998
Naresh A, Long W, Vidal GA et al (2006) The ERBB4/HER4 intracellular domain 4ICD is a BH3-only protein promoting apoptosis of breast cancer cells. Cancer Res 66:6412–6420
Barnes NL, Khavari S, Boland GP et al (2005) Absence of HER4 expression predicts recurrence of ductal carcinoma in situ of the breast. Clin Cancer Res 11:2163–2168
Sartor CI, Zhou H, Kozlowska E et al (2001) Her4 mediates ligand-dependent antiproliferative and differentiation responses in human breast cancer cells. Mol Cell Biol 21:4265–4275
Funding
Investigator Initiated clinical trial (NCT03219476) supported by Rock River Foundation and the Medical College of Wisconsin Cancer Center. Effort for this project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health Awards KL2TR001438, R03 CA259594 I, and R01 CA267549 (HR).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by LNC, JMJ, YS and HR. Pathology protein analyses were performed by JMJ and HR. Biostatistical analyses were performed by AB and IC. The first draft of the manuscript was written by LNC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Lubna N, Chaudhary has received consultant and advisory boards honoraria Puma Biotechnology, Seattle Genetics, Gilead Oncology, AstraZeneca, and Novartis Advisory as well as grant from Regeneron Pharmaceuticals outside the submitted work. Other authors have no financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presentations: Preliminary analysis of HER2 data in the first 14 patients was presented at San Antonio Breast Cancer Symposium (SABCS) 2019 as ‘Poster Presentation’.
Preliminary analysis of HER2 data for all patients was presented at SABCS 2020 as ‘Spotlight Poster Presentation’.
Preliminary analysis of HER1-4 upregulation for all patients was presented at SABCS 2021 as ‘Poster Presentation’.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chaudhary, L.N., Jorns, J.M., Sun, Y. et al. Frequent upregulation of HER2 protein in hormone-receptor-positive HER2-negative breast cancer after short-term neoadjuvant endocrine therapy. Breast Cancer Res Treat 201, 387–396 (2023). https://doi.org/10.1007/s10549-023-07038-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07038-3