Abstract
Purpose
This study aims to examine the burden of breast cancer in 185 countries in 2018.
Methods
The estimates of incidence, mortality, and prevalence of breast cancer were drawn from GLOBOCAN 2018. The overall burden of breast cancer was gauged using breast cancer burden index (BRCBI)—a novel index comprising age-standardized incidence rate (ASIR), age-standardized mortality rate (ASMR), mortality-to-incidence ratio (MIR), prevalence-to-incidence ratio (PIR), and prevalence-to-mortality ratio (PMR). The socioeconomic status of countries was measured using human development index (HDI)
Results
Globally, breast cancer was responsible for an estimated 626,679 deaths at age-standardized rate of 13/100,000; there were 2.1 million cases diagnosed in 2018 at age-standardized rate of 46.3/100,000. The ASIR varied 22-fold from 5/100,000 (Bhutan) to 113.2/100,000 (Belgium). The ASMR varied 13-fold from 2.7/100,000 (Bhutan) to 36.9/100,000 (Fiji). The HDI exhibited a positive gradient with ASIR (r = 0.73), PIR (r = 0.98), and PMR (r = 0.85); with MIR, however, it exhibited a negative association (r = − 0.83). The BRCBI spanned from 0.70 in Somalia to 78.92 in South Korea and exhibited a positive association with HDI (r = 0.76). An additional 46,823 female lives in 2018 and a cumulative total of 333,304 lives could have been saved over 2013–2018, had countries performed as per their HDI.
Conclusions
The substantial burden of breast cancer in developing and low-resource economies calls for a holistic approach to cancer management and control that includes oncologic infrastructure to provide cost-effective screening, diagnostic, therapeutic, and palliative services, greater breast cancer awareness, and mitigation of risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the leading malignancy in females worldwide, and its burden has grown in the last three decades, with higher incidence and survival rates in developed countries than the developing ones [1,2,3]. The improved treatment modalities and early detection in developed countries have improved the mortality and survival rates; in developing countries, however, survival rates are lower due to late-disease presentation, lack of oncologic infrastructure, and lack of cost-effective treatment regimens [2]. Breast cancer is linked with a multitude of modifiable risk factors (e.g., alcohol, tobacco consumption, and obesity) that relate to lifestyle [4, 5] and non-modifiable risk factors such as inherited gene mutation (e.g., BRCA 1/2), age, and familial risks [6,7,8].
For informed policy formulation and decision-making against breast cancer in global, regional, and national context, it is pertinent to understand the epidemiology of breast cancer burden in a cross-country context. This study investigates breast cancer's burden in 185 countries drawing upon estimates from GLOBOCAN 2018 [9, 10]. We studied the breast cancer burden in three dimensions. First, we examined the all-age, age-group-wise, and age-standardized incidence, mortality, and 5-year prevalence and made a comparative analysis between countries as per their socioeconomic development measured by human development index (HDI) [11]. Second, we constructed a novel index of breast cancer burden, namely breast cancer burden index (BRCBI), which is a composite of five epidemiological metrics: age-standardized incidence rate (ASIR), age-standardized mortality rate (ASMR), mortality-to-incidence ratio (MIR), prevalence-to-incidence ratio (PIR), and prevalence-to-mortality ratio (PMR). In the absence of actual survival data from low-resource economies, MIR has previously been demonstrated as a useful proxy of 5-year survival rate in a cross-country context [3, 12,13,14]. The new epidemiological constructs PIR and PMR, coupled with MIR, can gauge health system quality and oncologic care in different countries. Third, we identified few exemplar countries in each HDI groupings, which performed better than expected based on their HDI alone through observed-to-expected ratio (OER); based on OER, we quantified number of lives that could have been saved worldwide in 2018 and cumulatively in 2013–18.
Materials and methods
Estimates of breast cancer
We procured estimates of breast cancer burden in females for 185 countries from GLOBOCAN 2018 [9, 10, 15]. The estimates were available for three metrics: incidence, mortality, and prevalence (1-year, 3-year, and 5-year). GLOBOCAN produced age-standardized rates using World Population Reference standard. All-age and age-specific incidence and death counts are reported along with 95% uncertainty intervals (UIs) and are displayed inside square brackets; these UIs reflect uncertainties associated with cancer registry coverage and death registration, data quality, and timeliness of data reporting [9, 10, 15].
BRCBI and its components
BRCBI is an index used to compare breast cancer burden across countries; it comprises ASIR, ASMR, MIR, PIR, and PMR. We constructed an index for each of these metrics with 0 being assigned to worst-performing country and 100 being assigned to best-performing country by following formula.
In the above formula, \({ASIRI}_{i}\) denotes value of \(ASIR\) index for ith country; \({ASIR}_{99}\) and \({ASIR}_{1}\) are 99th percentile and first percentile values of \(ASIR\); \({ASIR}_{i}\) is value of \(ASIR\) of ith country. For ASIR, ASMR, and MIR, high values implied worst performance and hence resulted in low value of the index; in the case of PIR and PMR, high values implied better performance; therefore, the index construction for these two indices was modified as per the following formula.
We also assigned threshold values for countries at lowest and highest levels: countries with values lower than first percentile were assigned a minimum value of 0.1, and countries with values higher than 99th percentile were assigned a threshold value of 100Footnote 1 The BRCBI was constructed by taking geometric meanFootnote 2 of individual indices by the following formula.
The choice of these five epidemiological constructs was governed by availability of metrics and breast cancer burden characterized by the metrics. The MIR (high MIR means low value on MIR index), for instance, has been shown to reflect 5-year survival rates in the previous literature [3, 12,13,14]. Similarly, higher PIR (i.e., high PIR index) in a country implies that a patient diagnosed with breast cancer lives greater number of years so that 5-year prevalence is high in relation to incidence. The PIR of breast cancer in a country would be lower than diseases such as diabetes, but the inter-country differences in PIR in diseases such as breast cancer reflect the survival rates and quality of oncologic care. Lastly, high age-standardized rates (e.g., high ASIR and ASMR and low value on respective indices) imply that countries need to improve oncologic care involving early detection, prevention, and timely, cost-effective therapeutics.
Human Development Index
Countries' comparative performance and progress against breast cancer were gauged against a country’s development status measured by its HDI [11, 16]. HDI is a summary measure of three indicators: natural logarithm of gross national income per capita, education (composite construct of mean years of schooling and expected years of schooling), and life span (life expectancy at birth). A country’s value was rated on a 0 (worst) to 1 (best) scale for each of these three indicators; the geometric mean of three indicators provided HDI's final value.
Bivariate association between breast cancer metrics and HDI
The association between various breast cancer metrics and HDI was examined using bivariate regression as per the following equation.
In above equation, \({y}_{i}\) denotes breast cancer metrics, \({x}_{i}\) denotes HDI for ith country. The expected value of breast cancer metrics is generated as follows.
The OER was calculated as \(OER= \frac{{y}_{i}}{{\widehat{y}}_{i}}\). For MIR, OER lesser than one reflected better than the expected performance, whereas for PMR, an OER greater than one denoted better performance than was expected based on HDI alone.
We also tested for non-linear effects of HDI on breast cancer metrics by including a quadratic term in (5) as per the following regression.
The quadratic term was added if quadratic term and linear term were found to be statistically significant as per Eq. 6. The fitted model, fitted values (\({\widehat{y}}_{i})\) , and OER were thence modified accordingly.
Results
Incidence, mortality, and prevalence
Globally, breast cancer was responsible for 626,679 deaths [95% UI, 606,077–647,981] at an age-adjusted rate of 13/100,000; there were an estimated 2.1 million cases [2.0–2.2 million] in 2018 at an age-standardized rate of 46.3/100,000. East Asia was the leading region in terms of incidence with 476,509 [474,656–478,370] cases; in terms of death counts, however, South-central Asia was ranked first with 123,060 [119,256–126,986] breast cancer deaths in 2018 (Table 1). The ASIR was highest in Australia/New Zealand at 94.2/100,000, followed by Western Europe (92.6/100,000), and it was the lowest in South-central Asia (25.9/100,000). The 5-year prevalence was highest in East Asia, with 1.5 million females living with breast cancer; however, the 5-year prevalence rate was highest in developed regions led by Northern Europe (653.9/100,000) and lowest in middle Africa (30.1/100,000).
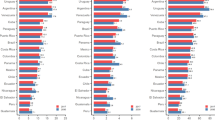
China was the leading country with 367,900 [346,754–390,335] cases and 97,972 [93,309–102,868] deaths (Supplementary Table S1). India was ranked second in terms of death counts (87,090 [84,651–89,599]) and was ranked third in terms of incidence (162,468 [158,245–166,804]) after China and United States (234,087 [232,580–235,604]). The ASIR varied more than 22-fold between countries, spanning from 5/100,000 in Bhutan to 113.2/100,000 in Belgium; the ASMR varied 13-fold between countries, ranging from 2.7/100,000 (Bhutan) to 36.9/100,000 (Fiji) (Fig. 1a, b).
Geographical distribution of Breast Cancer Statistics in 2018 1a. ASIR 1b. ASMR 1c. MIR. ASIR: Age-standardized incidence rate (cases per 100 000); ASMR: Age-standardized mortality rate (deaths per 100 000); MIR: Mortality-to-incidence ratio. The estimates of breast cancer burden were drawn from GLOBOCAN 2018
Global MIR stood at 0.30, varying five-fold worldwide from 0.12 in South Korea to 0.68 in Central African Republic (Fig. 1c; Supplementary Table S1) and exhibited a negative association with HDI (r = -0.8260; Supplementary Table S2). Globally, PIR stood at 3.29, varying threefold between countries spanning from 1.29 in Niger to 4.29 in Norway (Supplementary Table S1). The PMR exhibited a positive association with HDI (r = 0.8543; Supplementary Table S2); it was comparatively higher in high/very high HDI countries led by South Korea (28.53), followed by Norway (25.72) and was lower in low/medium HDI countries (e.g., Central African Republic 1.90 and Somalia 1.93).
Age-group-wise burden
Figure 2a–d illustrates that the age-wise distribution of breast cancer incidence and mortality varied substantially across HDI groupings. In low/medium HDI countries, the incidence and mortality of breast cancer peaked in the 45–54 age group, whereas developed countries faced a substantial portion of breast cancer burden in 55-plus age groups. In low HDI countries, 55% of cases were diagnosed before the age of 50 years, claiming 50% breast cancer deaths (Supplementary Fig S1); in very high HDI countries, however, the burden of breast cancer was lowest in the young age groups (~ 21% cases and ~ 10% of deaths in under-50 age groups).
Age-group-wise distribution of incidence and mortality of Breast Cancer a. Low HDI b. Medium HDI c. High HDI d. Very High HDI e. Global. Incidence: new cases; Deaths: deaths due to breast cancer; HDI: human development index. The estimates of breast cancer burden were drawn from GLOBOCAN 2018. The data of the human development index were taken from the United Nations Development Program. The countries were categorized as low (HDI < 0.550), medium (0.550−0.669), high (0.700−0.799), and very high (> 0.800)
Breast cancer burden index and components
The developed countries performed poorly in terms of ASIR index (or high ASIR), whereas populous countries such as China (ASIR index:71.26), India (81.8), and low/medium HDI countries (e.g., Bhutan 100, Mongolia 99.3, and Mozambique 95.9) scored high on this index (Fig. 3; Supplementary Table S3). In contrast, the ASMR index had mixed values as per the country's development status, with majority of least developed countries and few developed countries recording best performance (i.e., low values) on the ASMR index (e.g., Gambia 100, South Korea 92.23). Notably, few developed countries scored intermediate values on this index (e.g., Luxembourg 51.3 and United Kingdom 59.6).
Country-wise distribution of Breast Cancer Burden Index and Components. ASIR: Age-standardized incidence rate (cases per 100 000); ASMR: Age-standardized mortality rate (deaths per 100 000); MIR: Mortality-to-incidence ratio; HDI: Human development index; PIR: Prevalence-to-incidence ratio; PMR: Prevalence-to-incidence ratio; BRCBI: Breast cancer burden index. The MIR was calculated as the ratio of all-age death counts and all-age cases of breast cancer. The PIR was calculated as the ratio of all-age 5-year prevalence and all-age incidence count. The PMR was calculated as the ratio of 5-year prevalence and all-age death counts. The BRCBI was calculated as the geometric mean of ASIR index, ASMR index, MIR index, PIR index, and PMR index. The estimates of breast cancer burden were drawn from GLOBOCAN 2018
MIR index had a clear positive association with HDI, with a majority of developed countries recording high values on this index (e.g., Australia 100, Finland 99.9) and low/medium HDI countries recorded low values on this index (e.g., Somalia and Niger 0.1, Equatorial Guinea 3.8). PIR and PMR indices followed similar patterns as that of MIR, with developed countries recording high values and low/medium HDI countries lagging with low values. Those developed countries which performed relatively high on BRCBI also generally performed high on individual indices except for ASIR index (Fig. 3). The BRCBI varied from 0.70 in Somalia to 78.92 in South Korea and exhibited a positive correlation (r = 0.76) with HDI (Supplementary Table S2-S3).
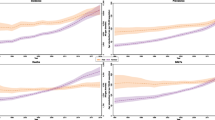
Bivariate regression
The association between breast cancer burden and HDI was examined using bivariate regression with HDI as explanatory variable (Fig. 4a–f; Supplementary Table S4). The ASIR was positively and significantly associated with HDI (\({R}^{2}=0.5277)\) with the inclusion of quadratic term significantly improving the model fit (\({R}^{2}=0.6448)\). There was no statistically significant relationship between ASMR and HDI, neither linear nor in quadratic form (Supplementary Table S4). The MIR had an inverse relationship with HDI (\({R}^{2}=0.6822)\), whereas PIR was positively linked with HDI (\({R}^{2}=0.9623)\). In case of PMR, there was a statistically significant positive association with HDI, and inclusion of quadratic term significantly improved the model fit (from \({R}^{2}=0.7298\ to\ {R}^{2}=0.8235).\) The HDI had a positive and statistically significant relationship with BRCBI and could explain 57% of variation in BRCBI, and the inclusion of quadratic term marginally improved the model fit (\({R}^{2}=0.6029)\). The relationship became slightly inverted U in shape, implying that after reaching a certain HDI level, HDI's influence on BRCBI tapers off (Fig. 4f).
Bivariate Association Between Childhood Cancer Burden and HDI a. ASIR vs. HDI b. ASMR vs. HDI c. MIR vs. HDI d. PIR vs. HDI e. PMR vs HDI f. BRCBI vs HDI. ASIR: Age-standardized incidence rate (cases per 100 000); ASMR: Age-standardized mortality rate (deaths per 100 000); MIR: Mortality-to-incidence ratio; PIR: Prevalence-to-incidence ratio; BRCBI: Breast cancer burden index; HDI: Human development index. The MIR was calculated as the ratio of all-age death counts and all-age cases of breast cancer. The PIR was calculated as the ratio of all-age 5-year prevalence and all-age incidence count. The PMR was calculated as the ratio of 5-year prevalence and all-age death counts. The BRCBI was calculated as the geometric mean of ASIR index, ASMR index, MIR index, PIR index, and PMR index. The estimates of breast cancer burden were procured from GLOBOCAN 2018. The data of human development index were taken from United Nations Development Program. The countries were categorized as low (HDI < 0.550), medium (0.550–0.669), high (0.700–0.799), and very high (> 0.800)
A comparative analysis of OERs as per HDI
The country-wise OERs were produced as per linear regression in MIR and quadratic regression in the case of PMR (Supplementary Table S5). In terms of MIR, Syria in low HDI (OER 0.81); Guatemala in medium HDI (OER 0.65); Brazil in high HDI (OER 0.63); South Korea in very high HDI (OER 0.47) were the best performers. Notably, a heavily burdened country such as India performed relatively poor in terms of its HDI (OER 1.27); it could have saved an estimated 18,915 lives in 2018 had it performed as per its HDI.Footnote 3 In terms of PMR, Syria in low HDI (OER 1.44); Guatemala in medium HDI (OER 1.66); Libya in high HDI (OER 1.56); South Korea in very high HDI (OER 1.62) were the best performers. Notably, due to its better performance as per HDI, Brazil (OER 1.49) could save 86,593 lives over five years (2013–2018); India, in contrast, could have saved 75,420 lives had it performed as per its HDI. In very high HDI category, United States and South Korea saved 208,468 and 29,952 lives, respectively, due to their better than expected performance as per HDI.Footnote 4
Discussion
Breast cancer was responsible for more than half a million deaths, and 2 million cases were estimated to be diagnosed worldwide in 2018. The ASIR exhibited positive association with HDI (r = 0.7264) and was the highest in developed countries (e.g., Belgium 113.2/100,000 and Luxembourg 109.2/100,000) and lowest in low/medium HDI countries (e.g., Bhutan 5/100,000 and Mozambique 14.5/100,000). Although incidence rates were the highest in developed regions, the developing countries in Asia and Africa shared a substantial portion of deaths and cases (~ 52% cases; ~ 61% deaths) in 2018. The 5-year survival rates proxied by MIR were the worst in sub-Saharan Africa (SSA) led by Central African Republic (0.68) and Equatorial Guinea (0.64). As with the previous studies [12], if we treat 1-MIR as the equivalent of 5-year survival rate, it varied from 32% in the Central African Republic to 88% in South Korea (MIR 0.12).
Consistent with previous studies [17, 18], breast cancer patients were comparatively younger in low and medium HDI countries; importantly, the proportion of younger patients diminishes with rising HDI. The developed countries had a substantial portion of breast cancer burden in 50-plus age groups (81% of cases and 89% of deaths), with low HDI countries had half the deaths and cases diagnosed before the age of 50 [19]. The age profile of breast cancer patients as per development status likely reflects higher life expectancy in developed countries, reproductive patterns, and etiologic differences [20]. In addition to younger age profile of breast cancer patients, the risk profile of breast cancer patients is also different in developing countries with a substantial portion of high-risk cancers such as triple-negative breast cancer, which has a poor prognosis [17, 21, 22].
The high incidence rates and high survival rates in developed countries (low MIR and high PIR) reflect an early detection, better cancer infrastructure, and cancer treatment in these countries [23]. The population-wide screening through breast mammograms has shown success in lowering mortality rates in developed countries [24, 25]. However, there are recent concerns over mammographic screening harms such as overdiagnosis/overtreatment, risk of secondary tumors due to ionizing radiation, and adverse psychological effects [26, 27]. Therefore, population-based mammographic screening cannot be emulated in low-resource economies due to large population sizes; younger breast cancer patients; financial, sociocultural, and logistical constraints; and competing population health problems [28, 29]. Moreover, population-based screening's success depends crucially on strength of health system to provide high-quality mammography, ensure high coverage and follow-up of screened patients, manage symptomatic patients, and provide timely access to diagnostic and therapeutic services [30]. Low-cost screening solutions such as clinical breast examination may be considered, which have shown some success in clinical downstaging in low and medium-income countries [31,32,33,34].
The HDI exhibited a positive association with PIR (r = 0.98), PMR (r = 0.85), and negative association with MIR (r = -0.83). As these metrics reflect relative survival rates, this implies that higher HDI countries provide better cancer care and ensures greater survival. Previous studies have also found marked disparities in 5-year survival rates, ranging from 12% and 46% in Gambia and Uganda [35] to over 90% in developed countries such as Australia and United States [2]. Late-disease presentation is one of the primary reasons for low survival rates in developing and low-resource economies, which leads to poor prognoses and fatal outcomes [35, 36]. About 50–75% of African women presented with advanced disease [37]; in United States, however, only 11% of females were diagnosed with an advanced tumor (stage III/IV) [38]. In SSA, lack of awareness, sociocultural factors, fatalism (i.e., cancer is not curable and always results in death), and fear of mastectomy are few of the patient-specific factors resulting in delayed diagnosis [17, 39, 40].
Due to resource constraints and low awareness levels in low-resource countries, previous studies have shown that focus must be on downstaging and raising cancer awareness rather than screening asymptomatic women in low-resource countries [28, 30, 41]. Even in upper-middle-income countries such as Brazil, there is limited evidence of improved cancer mortality rates after the Ministry of Health's introduction of screening guidelines in 2004 [30]. The African Breast Cancer-Disparities in Outcomes (ABC-DO) study found that stage at diagnosis was the most potent prognostic factor and concluded that earlier stage at diagnosis and improved therapy can avert one-third of breast cancer deaths over 2020–2029 in SSA [42]. In few low-resource countries, such programs have shown some success. For instance, in a pilot study conducted in Malaysia, a program focused on training health workers and raising cancer awareness reduced advanced breast cancer detection (stage III/IV) from 60 to 35% between 1994 and 1998 [43]. Similarly, increased cancer awareness and breast examination program among trained, non-medical volunteers in rural Sudan led to greater detection of benign, early-stage, and potentially curable tumors [33].
Low HDI countries' performance was worst in terms of BRCBI (e.g., Somalia 0.70; Central African Republic 1.11) and high/very high HDI countries showed the best performance (South Korea 78.92; Brunei 74.36). Notably, apart from incidence and mortality rates, which are the most commonly considered variables of breast cancer burden, BRCBI also encompasses the burden measured by metrics such as MIR and PIR. Therefore, improvements in BRCBI can be attained through improvements in individual components (i.e., reduction of ASIR, ASMR, MIR or increases in PIR, PMR), which is linked with all facets of oncologic care from disease prevention, availability of facilities (e.g., hospitals, oncologist, drugs, imaging techniques), early detection, cost-effective diagnostic and therapeutic services, and coverage of treatment expenses.
The poor performance of low/medium HDI countries on most epidemiological metrics and BRCBI is reminiscent of other public health systems' weaknesses in these countries. First, the treatment expenses and travel and accommodation cost from pocket discourages patients from reaching healthcare providers even after noticing cancer symptoms [17, 40]. For instance, in the ABC-DO study, the treatment completion and survival rates were the highest in Namibia because of free treatment [42, 44]. Second, the treatment options are also limited in LMICs so that surgery is sometimes the only treatment option due to limited availability of chemotherapy, radiotherapy, and hormonal treatments such as Tamoxifen [17, 40, 45, 46]. Third, under-staging of breast cancer is also possible in low-income countries due to inadequate imaging techniques resulting in inappropriate treatment decisions, high costs, and side effects [42].
Limitations
This study suffers from three limitations. First, data coverage and quality from cancer registries, which have a marked effect on GLOBOCAN estimates, are far from complete in many low-resource economies. This implies that breast cancer estimates in these countries are expected to be biased, and the country-specific values of different metrics and BRCBI would be adjusted accordingly. Second, we used MIR, PIR, and PMR as the proxy measures of survival rates and quality of health care system. These are not the actual survival rates and should not be substituted with actual survival rates. In the absence of actual data, however, these three indicators can serve the dual purpose of proxy for relative survival rates and quality of health services in a country. Third, although GLOBOCAN estimates provided a snapshot of breast cancer burden in 2018, lack of consistent time series prevented us from examining the improvement/worsening of breast cancer burden in cross-country context.
Conclusion
Low incidence and low survival rates in resource-poor countries and high incidence and high survival rates in developed countries mark the dichotomy of breast cancer burden as per HDI status of countries. The BRCBI, a novel index capturing the relative intensity of breast cancer burden on a 0 to 100 scale, is positively correlated with HDI. The burden characterized by different metrics in BRCBI shows that breast cancer poses different challenges across the development continuum, which is reflected in different incidence, mortality and survival rates, different age profiles of breast cancer patients, etiology, and prevalence of risk factors. The developed countries need to address the risk factors that result in disease onset (e.g., obesity, alcohol consumption), ensure elongated survival, and quality of life for breast cancer patients across the socioeconomic strata. In low- and medium-income countries, the breast cancer burden is expected to escalate further in future due to the westernization of lifestyles [47] (e.g., delayed marriages, low parity, low age at menarche, lack of physical activity, and poor diet), better cancer registration and cancer detection. The developing and low-resource economies, therefore, have to adopt a holistic approach to cancer management and control that requires oncologic infrastructure, cost-effective and equitable access to diagnostic, therapeutic, and palliative services, increase breast cancer awareness, and mitigate potentially modifiable risk factors that can aggravate incidence and death rates in these populations.
Notes
Choosing minimum values as 1st percentile also helped in not assigning 0 value to BRCBI.
An alternate index using arithmetic mean was generated; it has a pairwise correlation of r = 0.9230 with BRCBI (Supplementary Table S3).
Number of deaths that could be prevented in 2018 was calculated as per the following.
$$({\text{Extra}}\; {\text{Deaths}})_{2018} = ({\text{Incidence}})_{2018}({\text{Observed}}\; {\text{MIR}}-{\text{Expected}}\; {\text{MIR}})$$Number of lives saved as per PMR was calculated as per the following.
$$\left( {{\text{Extra}}\; {\text{Deaths}}} \right)_{2013{-}18} = \left( {{\text{Observed}} \;{\text{Deaths}}} \right)_{2018} \left( {{\text{Observed}}\; {\text{PMR }}- {\text{Expected}}\; {\text{PMR}}} \right)$$
References
Global Burden of Disease Cancer Collaboration (2019) Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: a systematic analysis for the global burden of disease study. JAMA Oncol 5(12):1749–1768. https://doi.org/10.1001/jamaoncol.2019.2996
Allemani C, Matsuda T, Di Carlo V et al (2018) Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391(10125):1023–1075
Sharma R (2019) Breast cancer incidence, mortality and mortality-to-incidence ratio (MIR) are associated with human development, 1990–2016: evidence from Global Burden of Disease Study 2016. Breast Cancer 26(4):428–445
Pérez-Solis MA, Maya-Nuñez G, Casas-González P et al (2016) Effects of the lifestyle habits in breast cancer transcriptional regulation. Cancer Cell Int 16(1):7
Yung RL, Ligibel JA (2016) Obesity and breast cancer: risk, outcomes, and future considerations. Clin Adv Hematol Oncol 14(10):790–797
Bradbury AR, Olopade OI (2007) Genetic susceptibility to breast cancer. Rev Endocr Metab Disord 8(3):255–267
Kim H, Choi DH (2013) Distribution of BRCA1 and BRCA2 mutations in Asian patients with breast cancer. J Breast Cancer 16(4):357–365
Skol AD, Sasaki MM, Onel K (2016) The genetics of breast cancer risk in the post-genome era: thoughts on study design to move past BRCA and towards clinical relevance. Breast Cancer Res 18(1):99
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Ferlay J, Colombet M, Soerjomataram I et al (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144(8):1941–1953
UNDP. Human Development Statistical Update 2018. (United nations Development Programme,2016) http://hdr.undp.org/sites/default/files/2018_human_development_statistical_update.pdf. Accessed 24 June2019
Vostakolaei F, Karim-Kos HE, Janssen-Heijnen ML et al (2010) The validity of the mortality to incidence ratio as a proxy for site-specific cancer survival. Eur J Public Health 21(5):573–577
Choi E, Lee S, Nhung BC et al (2017) Cancer mortality-to-incidence ratio as an indicator of cancer management outcomes in Organization for Economic Cooperation and Development countries. Epidemiol Health 39:e2017006
Sharma R (2019) The burden of prostate cancer is associated with human development index: evidence from 87 countries, 1990–2016. EPMA J 10(2):137–152
Ferlay J, Ervik M, Lam F et al Global Cancer Observatory. Lyon, France: International Agency for Research on Cancer. https://gco.iarc.fr/. Accessed Dec 2019 - Jan 2020
Human Development Database. http://hdr.undp.org/en/data#. Accessed Dec 2019
Brinton LA, Figueroa JD, Awuah B et al (2014) Breast cancer in Sub-Saharan Africa: opportunities for prevention. Breast Cancer Res Treat 144(3):467–478
Sharma R (2020) Breast cancer burden in Africa: evidence from GLOBOCAN 2018. J Public Health. https://doi.org/10.1093/pubmed/fdaa099
DeSantis CE, Ma J, Goding Sauer A et al (2017) Breast cancer statistics, racial disparity in mortality by state. CA Cancer J Clin 67(6):439–448
Gabriel CA, Domchek SM (2010) Breast cancer in young women. Breast Cancer Res 12(5):212
Corbex M, Bouzbid S, Boffetta P (2014) Features of breast cancer in developing countries, examples from North-Africa. Eur J Cancer 50(10):1808–1818
Youlden DR, Cramb SM, Yip CH, Baade PD (2014) Incidence and mortality of female breast cancer in the Asia-Pacific region. Cancer Boil Med 11(2):101
Youlden DR, Cramb SM, Dunn NA et al (2012) The descriptive epidemiology of female breast cancer: an international comparison of screening, incidence, survival and mortality. Cancer Epidemiol 36(3):237–248
Shapiro S (1997) Periodic screening for breast cancer: the HIP randomized controlled trial. JNCI Monogr 1997(22):27–30
Tabár L, Yen AM, Wu WY et al (2015) Insights from the breast cancer screening trials: how screening affects the natural history of breast cancer and implications for evaluating service screening programs. Breast J 21(1):13–20
Bleyer A, Welch HG (2012) Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med 367(21):1998–2005
Marmot MG, Altman DG, Cameron DA et al (2013) The benefits and harms of breast cancer screening: an independent review. Br J Cancer 108(11):2205–2240
Harford JB (2011) Breast-cancer early detection in low-income and middle-income countries: do what you can versus one size fits all. Lancet Oncol 12(3):306–312
Black E, Richmond R (2019) Improving early detection of breast cancer in sub-Saharan Africa: why mammography may not be the way forward. Glob Health 15(1):3
dos-Santos-Silva I, de Stavola BL, Junior NL, Nogueira MC, Aquino EM, Bustamante-Teixeira MT, Silva GA (2019) Ethnoracial and social trends in breast cancer staging at diagnosis in Brazil, 2001–14: a case only analysis. Lancet Glob Health 7(6):e784–e797
Mittra I, Mishra GA, Singh S et al (2010) A cluster randomized, controlled trial of breast and cervix cancer screening in Mumbai, India: methodology and interim results after three rounds of screening. Int J Cancer 126(4):976–984
Sankaranarayanan R, Ramadas K, Thara S et al (2011) Clinical breast examination: Preliminary results from a cluster randomized controlled trial in India. J Natl Cancer Inst 103(19):1476–1480
Abuidris DO, Elsheikh A, Ali M et al (2013) Breast-cancer screening with trained volunteers in a rural area of Sudan: a pilot study. Lancet Oncol 14(4):363–370
Song QK, Wang XL, Zhou XN et al (2015) Breast cancer challenges and screening in China: Lessons from current registry data and population screening studies. Oncologist 20(7):773–779
Sankaranarayanan R, Swaminathan R, Brenner H et al (2010) Cancer survival in Africa, Asia, and Central America: a population-based study. Lancet Oncol 11(2):165–173
Jedy-Agba E, McCormack V, Adebamowo C et al (2016) Stage at diagnosis of breast cancer in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health 4(12):e923–e935
Abdulrahman GO, Rahman GA (2012) Epidemiology of breast cancer in Europe and Africa. J Cancer Epidemiol 2012:915610
Sariego J (2009) Patterns of breast cancer presentation in the United States: does geography matter? Am Surg 75(7):545–550
Akuoko CP, Armah E, Sarpong T, Quansah DY, Amankwaa I, Boateng D (2017) Barriers to early presentation and diagnosis of breast cancer among African women living in sub-Saharan Africa. PLoS ONE 12(2):e0171024
Tetteh DA, Faulkner SL (2016) Sociocultural factors and breast cancer in sub-Saharan Africa: implications for diagnosis and management. Women’s Health 12(1):147–156
Yip CH (2019) Downstaging is more important than screening for asymptomatic breast cancer. Lancet Glob Health 7(6):e690–e691
McCormack V, McKenzie F, Foerster M, Zietsman A, Galukande M, Adisa C, Anele A, Parham G, Pinder LF, Cubasch H, Joffe M (2020) Breast cancer survival and survival gap apportionment in sub-Saharan Africa (ABC-DO): a prospective cohort study. Lancet Glob Health 8(9):e1203–e1212
Devi BC, Tang TS, Corbex M (2007) Reducing by half the percentage of late-stage presentation for breast and cervix cancer over 4 years: a pilot study of clinical downstaging in Sarawak. Malays Ann Oncol 18(7):1172–1176
Foerster M, Anderson BO, McKenzie F, Galukande M, Anele A, Adisa C, Zietsman A, Schuz J, dos Santos SI, McCormack V (2019) Inequities in breast cancer treatment in sub-Saharan Africa: findings from a prospective multi-country observational study. Breast Cancer Res 21(1):93
Clegg-Lamptey J, Dakubo J, Attobra YN (2009) Why do breast cancer patients report late or abscond during treatment in ghana? A pilot study. Ghana Med J 43(3):127–131
Sullivan R, Alatise OI, Anderson BO (2015) Global cancer surgery: delivering safe, affordable, and timely cancer surgery. Lancet Oncol 16(11):1193–1224
Porter P (2008) ‘Westernising’ women’s risks? Breast cancer in lower income countries. N Engl J Med 358(3):213–216
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Informed consent
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
The research was conducted using data available in the public domain and did not include any human participants or animals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sharma, R. Global, regional, national burden of breast cancer in 185 countries: evidence from GLOBOCAN 2018. Breast Cancer Res Treat 187, 557–567 (2021). https://doi.org/10.1007/s10549-020-06083-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06083-6