Abstract
Purpose
To examine the association between obesity measured by body mass index (BMI) and waist circumference (WC) according to menopausal status in Korean women.
Methods
We identified 6,467,388 women, using the Korean National Health Insurance System Cohort. Cox-proportional hazard models were used to generate adjusted hazard ratios (aHRs) and 95% confidence intervals (CIs) for breast cancer risk in relation to BMI and WC.
Results
In postmenopausal women, the risk of breast cancer increased with BMI. Compared to women with a BMI of 18.5–23 kg/m two, the risk of invasive breast cancer was lower in patients with BMI < 18.5 (aHR 0.82, 95% CI 0.75–0.89), while it increased linearly in those with BMI 23–25 (1.11, 1.08–1.14), BMI 25–30 (1.28, 1.25–1.32), and BMI ≥ 30 (1.54,1.47–1.62). In contrast, the risk of breast cancer decreased with BMI in premenopausal women. Compared to women with a BMI of 18.5–23, the risk of IBC was similar in those with a BMI < 18.5 (1.02, 0.94–1.11) and BMI 23–25 (1.01, 0.97–1.05), but was significantly lower in those with a BMI 25–30 (0.95, 0.91–0.98) and BMI ≥ 30 (0.90, 0.82–0.98). A relative increase with BMI was less profound for carcinoma in situ in postmenopausal women, and a relative decrease was more profound in premenopausal women. An analysis using WC showed almost identical results.
Conclusions
There was a positive relationship between obesity and breast cancer in postmenopausal women, and an inverse association in premenopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is one of the most prevalent cancers and a leading cause of cancer mortality in females worldwide. As of 2018, 2.09 million new breast cancer cases were diagnosed worldwide, and 0.62 million women died from breast cancer, contributing to 24.2% of cancer incidence and 15.0% of cancer mortality in the female population [1].
The association between obesity and the risk of breast cancer has been investigated in many studies. Breast cancer was found to be associated with obesity and this association was related to the estrogenic effect of obesity [2]. Therefore, it can be hypothesized that the association between obesity and breast cancer risk is modified by menopausal status [3].
Most studies consistently found a positive association between body mass index (BMI) [4,5,6,7,8] and waist circumference (WC) [9, 10] with breast cancer incidence, and recent meta-analyses confirming such overall positive associations [11, 12] in postmenopausal women. However, for premenopausal women, results are inconsistent. Many studies performed in the Western population showed a negative association [13,14,15]. Asian studies showed null associations between BMI and breast cancer [7, 16, 17]. However, a recent pooled analysis showed a negative association [18] and several meta-analyses showed a positive association in Asian women [11, 19]. This discrepancy suggests that there may be ethnic or racial differences in the correlation between obesity and breast cancer. However, previous studies in Asia had relatively small sample sizes and so, had insufficient statistical power to draw definite conclusions [18], which suggested the need for an additional study to be carried out in an Asian population.
In addition, previous studies had the following limitations. First, they generally used a single obesity parameter. Most studies used only BMI as the obesity indicator to assess obesity’s association with breast cancer risk [4, 8, 9, 11, 12, 15, 17], while others only used WC [20, 21] which has the advantage of reflecting abdominal obesity and metabolic syndrome [22]. Only a few studies have used both parameters [6, 23, 24]. Second, some studies included only invasive breast cancer (IBC) cases, and did not include carcinoma in situ (CIS) [25, 26]. Although it is unclear whether CIS develops into invasive breast cancer or not [27], both types of breast cancer (IBC and CIS), should be considered at the same time in studies done to investigate the risk of breast cancer.
Therefore, we sought to examine the association between obesity and breast cancer risk according to menopausal status in Korean women. We evaluated obesity using both BMI and WC, and considered IBC and CIS as separate outcomes.
Methods
Study setting and data source
We used data from the Korean National Health Insurance Service (NHIS). As the single government insurer, the NHIS provides comprehensive medical insurance to most of the Korean population (over 97%) and provides the administration of medical aid assistance to 3% of the vulnerable population. The NHIS database contains data on the characteristics of the enrollees (age, sex, income status, place of residence, etc.), diagnosis code by the International Classification of Disease 10th revision (ICD-10), and information about medical treatment based on medical expenditure claims and prescription data [28].
The NHIS provides biennial general health screening programs for people ≥ 40 years [29], including anthropometric measurements (BMI, WC, etc.), lifestyle questionnaires (smoking, alcohol consumption, physical activities, etc.), and laboratory testing (blood glucose, lipid levels, etc.). In addition, the NHIS runs breast cancer Screening Programs for all Korean women ≥ 40 years every two years. Before breast cancer screening examination, women are required to answer a questionnaire, which includes menopausal status and reproductive history [30]. This data is also registered on the NHIS database. The NHIS database offers useful and relevant data as a massive epidemiological study pool to medical researchers. More details of the NHIS database are described elsewhere [31].
Study population
We included women ≥ 40 years who had undergone both the general health screening and breast cancer screening at the same time from January 1, 2009 to December 31, 2014 (Fig. 1). Even though there were individuals who were screened two or more times during the enrollment period, the measurement of the first screening was considered as baseline. Data were collected at the study enrollment, which was the first health screening participation during the study period Table1.
Among 6,467,388 eligible subjects, we excluded participants who had previously undergone a hysterectomy (n = 14,926), were diagnosed with any previous malignancy (n = 167,585) and those with missing data for a key variable (n = 12,510). As a result, a total of 6,272,367 women (1,418,180 premenopausal and 4,854,187 postmenopausal women) were included in this study. Our study was approved by the Institutional Review Board of Samsung Medical Center (IRB File No. SMC 2019–01-050), and individual informed consent was waived because this study used only de-identified data.
Data collection
All data collection, including anthropometric measurement and questionnaires, were made at the date of health screening. BMI was calculated using weight (kg) divided by the square of the height (m2), and classified into five levels as low (< 18.5 kg/m2), normal (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), obese (25–29.9 kg/m2), or severely obese (≥ 30 kg/m2) according to the World Health Organization/International Association for the Study of Obesity/International Obesity Task Force obesity guidelines [32]. WC was measured at the midpoint between the lower margin of the last palpable rib and the top of the iliac crest. WC was divided into 5 levels as low (< 65 cm), normal (65–74.9 cm), overweight (75–84.9 cm), obese (85–94.9 cm), and severely obese (≥ 90 cm) according to the Korean Society for the Study of Obesity guidelines [33].
Information about health-related behaviors and menstrual and reproductive histories were obtained using a self-administered questionnaire. Before the general health examination, women were asked about their smoking history (classified as never, former and current smoker), alcohol consumption (divided into three levels: none, < 30 g/day, and ≥ 30 g/day), regularity of exercise (defined as moderate physical activity for more than 30 min daily and more than 5 days per week over the past week), and comorbidities. Before taking the breast cancer screening examination, women were asked about their age at menarche, age at menopause, parity (0, 1, or ≥ 2 children), breast feeding history (never, < 6, 6–12, and ≥ 12 total months), use of hormone replacement therapy (HRT; never, < 2, 2–5, ≥ 5 years) and oral contraceptive use (never, < 1, ≥ 1 year, and unknown).
Study outcomes and follow-up
The primary endpoint of this study was newly diagnosed IBC cases, defined as new claims for inpatient or outpatient care with the diagnosis code of C50 (malignant neoplasm of the breast) with registration in the special co-payment reduction program for critical illnesses. CIS (D05, carcinoma in situ of the breast) was defined in the same manner. All breast cancer was defined as either being IBC or CIS. The patients were followed up from their health check-up date to the date of incident breast cancer, death, or until the end of the study period (December 31, 2016), whichever came first.
Statistical analysis
The incidence rates for breast cancer were calculated by dividing the number of incident cases by the total follow-up period. Hazard ratios (HRs) and 95% confidence interval (CI) according to BMI and WC categories were analyzed using Cox proportional hazards models. Covariates for adjustment were selected based on their previous association with breast cancer incidence in the literature [34,35,36,37], and were added serially into the models: (1) Model 1 was non-adjusted; (2) Model two was adjusted for age, income, smoking [34], alcohol drinking [35], and physical activity [36]; (3) Model three was further adjusted for age at menarche, parity, breast feeding, oral contraceptive use in premenopausal women, and additionally for age at menopause and HRT in postmenopausal women [37]. Statistical analyses were performed using the Statistical Analysis System (SAS) version 9.4 (SAS Institute Inc., Cary, NC, USA), and a p value < 0.05 was considered statistically significant.
Results
Baseline characteristics
The mean age of the participants was 43.7 years in the premenopausal women and 59.9 years in the postmenopausal women. The mean BMI and WC was 23.1 kg/m2 and 75.0 cm, respectively in the premenopausal women and 24.1 kg/m2 and 79.6 cm, respectively in the postmenopausal women. Reproductive factors differed by menopausal status: postmenopausal women had later menarche (16.3 vs. 14.8 years), more parity (90.1 vs. 78.6%), longer breast-feeding history (91.8% vs. 78.4% for any, 65.8 vs. 27.8 for ≥ 1 year), and more oral contraceptive use (19.2% vs 16.0%) (Table 1).
Association between BMI and the risk of breast cancer by menopausal status
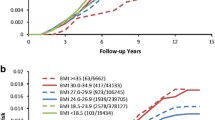
During a mean follow-up of 6.2 years, 18,141 premenopausal women and 39,485 postmenopausal women were diagnosed with breast cancer. In postmenopausal women, the risk of breast cancer increased with BMI (Table 2, Fig. 2). Compared with the BMI reference group (BMI 18.5–23), the risk of invasive breast cancer (IBC) was lower in the underweight group (aHR 0.82, 95% CI 0.75–0.89), while it increased linearly in the overweight (1.11, 1.08–1.14), obese (1.28,1.25–1.32), and severely obese groups (1.54,1.47–1.62). In contrast, IBC decreased with BMI in premenopausal women. Compared with the BMI reference group (BMI 18.5–23), the risk of IBC was similar in the underweight (1.02, 0.94–1.11) and overweight groups (1.01, 0.97–1.05), but was significantly lower in the obese (0.95, 0.91–0.98), and severely obese groups (0.90, 0.82–0.98) (Fig. 2a). But the relative risk increased less with BMI in the postmenopausal women with CIS [e.g., aHR, 95% CI for the severely obese group was 1.26 (1.14–1.40) in CIS compared to 1.54 (1.47–1.62) for IBC] and it decreased more in the premenopausal women with CIS [e.g., aHR, 95% CI for the severely obese group was 0.68 (0.56–0.82) in CIS compared to 0.82 (0.75–0.89) for IBC] (Fig. 2b).
Association between WC and the risk of breast cancer by menopausal status
In postmenopausal women, the risk of breast cancer increased with WC (Table 3, Fig. 2). Compared with the reference group (WC: 65–75), the relative risk (aHR, 95% CI) for IBC was lower in the underweight group (0.92, 0.85–0.98), while it increased linearly in the overweight (1.15, 1.12–1.18), obese (1.32, 1.28–1.37), and severely obese groups (1.49, 1.42–1.57). In contrast, the risk of breast cancer decreased with WC in premenopausal women. Compared with the WC reference group (WC 65–75), the relative risk of IBC was similar in the underweight (1.01, 0.95–1.08) and overweight groups (1.00, 0.97–1.04), but was significantly lower in the obese (0.94, 0.89–0.99), and severely obese groups (0.93, 0.83–1.05) (Fig. 2d). The relative risk increased less with WC in postmenopausal women with CIS women [e.g., aHR and 95% CI for the severely obese group was 1.22 (1.09–1.36) in CIS compared to 1.49 (1.42–1.67) for IBC], and decreased more with WC in premenopausal women with CIS [e.g., aHR, 95% CI for the severely obese group was 0.70 (0.55–0.89) in CIS compared to 0.93 (0.83–1.05) for IBC] (Fig. 2e).
Discussion
In this large-scale prospective cohort of Korean women, we found a significant positive association between obesity and IBC in postmenopausal women, but a significant inverse association in premenopausal women. CIS showed a less positive association in postmenopausal women, and an inverse association with obesity in premenopausal women. The patterns were not different, whether they were measured by BMI or WC. The strengths of our study are as follows; it was a single ethnic Asian cohort which is representative of the entire Korean population, had a large sample size with a sufficient number of breast cancer events, a simultaneous evaluation of BMI and WC in a single study, and a low number of lost to follow-up cases.
In postmenopausal women, we confirmed a positive association between obesity and IBC, which was consistent with numerous previous studies [10, 38,39,40,41]. Obesity induces oncogenic environments by multiple biological pathways including endogenous sex hormone synthesis, inflammation, and insulin resistance [2, 42] An obese woman has large amounts of adipose cells, which act as primary sources of estrogen production after menopause; for example, androgens originating from the adrenal glands are converted to estrogen by aromatization in adipose cells [2]. Therefore, women with higher amounts of body fat tend to have higher levels of circulating estrogen, and this stimulates more estrogen-sensitive breast tissues that may already have a propensity for hyperstimulation, ultimately promoting the formation and development of tumors [43]. In addition, adipose tissue produces various cytokines, growth factors, and inflammatory factors, which may in turn trigger sex hormone aromatization. Moreover, insulin resistance, adipocytokines, and leptin, are also important factors for the formation and development of breast cancer stimulated in the obese state [43,44,45,46].
In contrast, we found an inverse association between obesity and breast cancer in premenopausal women. In premenopausal women unlike postmenopausal women, estrogen is mainly produced in the ovaries. Estrogen production in premenopausal women is less affected by obesity. Estrogen levels are lower in obese premenopausal women, which is explained by the substantial uptake of estradiol into fat and the higher liver clearance rate of estrogen [47].
In comparison with other studies, while obesity and breast cancer had an inverse association in premenopausal women in most Western studies [14, 48], several Asian studies showed inconsistent results. Several Japanese studies showed a null association between obesity and breast cancer [7, 16, 17]. A Pooled analysis of eight Japanese studies by Wada et al. (the number for premenopausal breast cancer patients in the meta-analyses was only about 300) found a positive association between BMI and breast cancer [49]. Ethnic and/or racial difference can explain this, as the epidemiology of breast cancer is much different between Asian and Western countries (e.g., much leaner body composition in Asian countries, earlier age of breast cancer diagnosis [50, 51] and smaller proportion of estrogen receptor-positive (ER +) cancer cases [52]). However, our large-scale study (n for premenopausal breast cancer = 18,141) showed an inverse association which is rather similar to that of the Western population.
Our study shows that CIS has a somewhat different association with obesity compared to IBC. The positive association in postmenopausal women was weaker, and the inverse association in premenopausal women was stronger than those observed for IBC. This is consistent with previous studies which showed a different direction of association for obesity between CIS and IBC [53]. This suggests that CIS may have a distinct pathophysiology from IBC. Though its etiology is still not clear, there is some evidence suggesting that CIS has a different pathogenesis. First, though CIS is suggested as a precursor of IBC, its progression to IBC is not absolute [27]. Second, in relation to HRT especially in estrogen and breast cancer patients, several studies showed that CIS has no relationship with HRT use [54, 55], while IBC has a positive relationship [56, 57]. This suggests that CIS has a weak association with estrogen in terms of etiology. So, obesity has been shown to be less influential in the development of CIS than in IBC, regardless of menopausal status [58]. An alternative explanation to differences in tumor biology could be the effect of screening, as CIS is mostly detected by breast cancer screening. It is possible that the attenuation of effect estimates can occur as a result of misclassification in CIS-specific analysis, but the stronger association observed for CIS in premenopausal women cannot be explained in this way. In addition, a previous study that investigated CIS and IBC did not expect differential misclassification of mode of detection by CIS or IBC [53]. Overall, we think our results are more suggestive of a different tumor biology between IBC and CIS, rather than a difference in screening pattern.
WC is a simple and convenient way to measure obesity, and it reflects abdominal and central obesity more exactly than BMI [22]. Many studies showed that WC is better for predicting type 2 diabetes [59], myocardial infarction [60], and all causes of mortality [61] than BMI but the results between WC and BMI did not show any significant difference in the risk of breast cancer incidence.
Although menopause does not directly increase BMI, the decrease in ovary-related hormones promotes an increase in adipose tissue mass especially in the early postmenopausal period [62]. Our findings suggest that obesity in postmenopausal women results in an increased breast cancer incidence; so, controlling obesity in postmenopausal women is important for the prevention of breast cancer.
This study had several limitations. First, we did not have information on the hormonal receptor status of the breast cancer cases. As ER + breast cancers in Asians is a growing trend [52], future studies will need to investigate whether ER receptors are expressed in Korean women in order to correlate ER + status with obesity and menopausal status. Analyses according to receptor status would have been helpful to better elucidate their relationship with obesity, estrogen, and breast cancer. Second, obesity measurement was only done once at the time of enrollment, so, it did not reflect changes in obesity patterns. There could be a bias in evaluating dose-dependent effects. Third, menopausal status was evaluated at baseline only. However, premenopausal women at baseline can become menopausal during follow up. Breast cancer in premenopausal women may not necessarily be premenopausal breast cancer. Finally, our study findings cannot be generalized as it was carried out only in the Korean population. However, our data is supplementary to current knowledge on the risk factors for breast cancer in the Asian population.
In conclusion, we demonstrated that the association between obesity and breast cancer risk is modified by menopausal status. There was a positive relationship between obesity and breast cancer in postmenopausal women, and an inverse association in premenopausal women. Our study suggests the need to manage obesity in breast cancer prevention especially in postmenopausal women.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Clemons M, Goss P (2001) Estrogen and the risk of breast cancer. J N Eng J Med. 344(4):276–285
Rose DP, Vona-Davis L (2010) Interaction between menopausal status and obesity in affecting breast cancer risk. Maturitas 66(1):33–38. https://doi.org/10.1016/j.maturitas.2010.01.019
Song YM, Sung J, Ha M (2008) Obesity and risk of cancer in postmenopausal Korean women. J Clin Oncol 26(20):3395–3402. https://doi.org/10.1200/jco.2007.15.7867
Cecchini RS, Costantino JP, Cauley JA, Cronin WM, Wickerham DL, Land SR, Weissfeld JL, Wolmark N (2012) Body mass index and the risk for developing invasive breast cancer among high-risk women in NSABP P-1 and STAR breast cancer prevention trials. Cancer prevention research (Philadelphia, Pa) 5(4):583–592. https://doi.org/10.1158/1940-6207.Capr-11-0482
Gaudet MM, Carter BD, Patel AV, Teras LR, Jacobs EJ, Gapstur SM (2014) Waist circumference, body mass index, and postmenopausal breast cancer incidence in the cancer prevention study-II nutrition cohort. Cancer Causes Control 25(6):737–745. https://doi.org/10.1007/s10552-014-0376-4
Suzuki S, Kojima M, Tokudome S, Mori M, Sakauchi F, Wakai K, Fujino Y, Lin Y, Kikuchi S, Tamakoshi K, Tamakoshi A (2013) Obesity/weight gain and breast cancer risk: findings from the Japan collaborative cohort study for the evaluation of cancer risk. J Epidemiol 23(2):139–145. https://doi.org/10.2188/jea.je20120102
Canchola AJ, Anton-Culver H, Bernstein L, Clarke CA, Henderson K, Ma H, Ursin G, Horn-Ross PL (2012) Body size and the risk of postmenopausal breast cancer subtypes in the California Teachers Study cohort. Cancer Causes Control 23(3):473–485
Ahn J, Schatzkin A, Lacey JV Jr, Albanes D, Ballard-Barbash R, Adams KF, Kipnis V, Mouw T, Hollenbeck AR, Leitzmann MF (2007) Adiposity, adult weight change, and postmenopausal breast cancer risk. Arch Intern Med 167(19):2091–2102. https://doi.org/10.1001/archinte.167.19.2091
Lahmann PH, Hoffmann K, Allen N, van Gils CH, Khaw KT, Tehard B, Berrino F, Tjonneland A, Bigaard J, Olsen A, Overvad K, Clavel-Chapelon F, Nagel G, Boeing H, Trichopoulos D, Economou G, Bellos G, Palli D, Tumino R, Panico S, Sacerdote C, Krogh V, Peeters PH, Bueno-de-Mesquita HB, Lund E, Ardanaz E, Amiano P, Pera G, Quiros JR, Martinez C, Tormo MJ, Wirfalt E, Berglund G, Hallmans G, Key TJ, Reeves G, Bingham S, Norat T, Biessy C, Kaaks R, Riboli E (2004) Body size and breast cancer risk: findings from the European prospective Investigation into cancer and nutrition (EPIC). Int J Cancer 111(5):762–771. https://doi.org/10.1002/ijc.20315
Chen Y, Liu L, Zhou Q, Imam MU, Cai J, Wang Y, Qi M, Sun P, Ping Z, Fu X (2017) Body mass index had different effects on premenopausal and postmenopausal breast cancer risks: a dose-response meta-analysis with 3,318,796 subjects from 31 cohort studies. BMC Public Health 17(1):936. https://doi.org/10.1186/s12889-017-4953-9
Chen GC, Chen SJ, Zhang R, Hidayat K, Qin JB, Zhang YS, Qin LQ (2016) Central obesity and risks of pre- and postmenopausal breast cancer: a dose-response meta-analysis of prospective studies. Obes Rev 17(11):1167–1177. https://doi.org/10.1111/obr.12443
Weiderpass E, Braaten T, Magnusson C, Kumle M, Vainio H, Lund E, Adami HO (2004) A prospective study of body size in different periods of life and risk of premenopausal breast cancer. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 13(7):1121–1127
Palmer JR, Adams-Campbell LL, Boggs DA, Wise LA, Rosenberg L (2007) A prospective study of body size and breast cancer in black women. Cancer Epidemiology Prevention Biomarkers 16(9):1795–1802
Reeves GK, Pirie K, Beral V, Green J, Spencer E, Bull D (2007) Cancer incidence and mortality in relation to body mass index in the million women study: cohort study. BMJ 335(7630):1134. https://doi.org/10.1136/bmj.39367.495995.AE
Iwasaki M, Otani T, Inoue M, Sasazuki S, Tsugane S (2007) Body size and risk for breast cancer in relation to estrogen and progesterone receptor status in Japan. Ann Epidemiol 17(4):304–312. https://doi.org/10.1016/j.annepidem.2006.09.003
Kuriyama S, Tsubono Y, Hozawa A, Shimazu T, Suzuki Y, Koizumi Y, Suzuki Y, Ohmori K, Nishino Y, Tsuji I (2005) Obesity and risk of cancer in Japan. Int J Cancer 113(1):148–157. https://doi.org/10.1002/ijc.20529
Schoemaker MJ, Nichols HB, Wright LB, Brook MN, Jones ME, O’Brien KM, Adami H-O, Baglietto L, Bernstein L, Bertrand KA (2018) Association of body mass index and age with subsequent breast cancer risk in premenopausal women. JAMA oncology 4(11):e181771–e181771
Nindrea RD, Aryandono T, Lazuardi L, Dwiprahasto I (2019) Association of overweight and obesity with breast cancer during premenopausal period in Asia: A meta-analysis. Int J Prev Med 10(1):192
MacInnis RJ, English DR, Gertig DM, Hopper JL, Giles GG (2004) Body size and composition and risk of postmenopausal breast cancer. Cancer Epidemiol Prev Biomarkers 13(12):2117–2125
Krebs EE, Taylor BC, Cauley JA, Stone KL, Bowman PJ, Ensrud KE (2006) Measures of adiposity and risk of breast cancer in older postmenopausal women. J Am Geriatr Soc 54(1):63–69
Pouliot M-C, Després J-P, Lemieux S, Moorjani S, Bouchard C, Tremblay A, Nadeau A, Lupien PJ (1994) Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am j cardiol 73(7):460–468
Lee KR, Hwang IC, Han KD, Jung J, Seo MH (2018) Waist circumference and risk of breast cancer in Korean women: A nationwide cohort study. Int J Cancer 142(8):1554–1559. https://doi.org/10.1002/ijc.31180
Wang X, Li L, Gao J, Liu J, Guo M, Liu L, Wang W, Wang J, Xing Z, Yu Z, Wang X (2016) The association between body size and breast cancer in han women in Northern and Eastern China. Oncologist 21(11):1362–1368. https://doi.org/10.1634/theoncologist.2016-0147
Neuhouser ML, Aragaki AK, Prentice RL, Manson JE, Chlebowski R, Carty CL, Ochs-Balcom HM, Thomson CA, Caan BJ, Tinker LF, Urrutia RP, Knudtson J, Anderson GL (2015) Overweight, obesity, and postmenopausal invasive breast cancer risk: A secondary analysis of the women's health initiative randomized clinical trials. JAMA oncology 1(5):611–621. https://doi.org/10.1001/jamaoncol.2015.1546
Anderson GL, Neuhouser ML (2012) Obesity and the risk for premenopausal and postmenopausal breast cancer. Cancer prev res 5(4):515–521
Cowell CF, Weigelt B, Sakr RA, Ng CK, Hicks J, King TA, Reis-Filho JS (2013) Progression from ductal carcinoma in situ to invasive breast cancer: revisited. Mol oncol. 7(5):859–869
Song SO, Jung CH, Song YD, Park C-Y, Kwon H-S, Cha BS, Park J-Y, Lee K-U, Ko KS, Lee B-W (2014) Background and data configuration process of a nationwide population-based study using the korean national health insurance system. Diabetes meta J 38(5):395–403
Lee H, Cho J, Shin DW, Lee S-P, Hwang S-S, Oh J, Yang H-K, Hwang S-H, Son KY, Chun SH (2015) Association of cardiovascular health screening with mortality, clinical outcomes, and health care cost: a nationwide cohort study. Prev Med 70:19–25
Choi KS, Yoon M, Song SH, Suh M, Park B, Jung KW, Jun JK (2018) Effect of mammography screening on stage at breast cancer diagnosis: results from the Korea National cancer screening program. Sci rep 8(1):1–8
Lee J, Lee JS, Park S-H, Shin SA, Kim K (2017) Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC). South Korea Int j epidemiol 46(2):e15–e15
Organization WH (2000) The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia, Sydney
Seo MH, Lee WY, Kim SS, Kang JH, Kang JH, Kim KK, Kim BY, Kim YH, Kim WJ, Kim EM, Kim HS, Shin YA, Shin HJ, Lee KR, Lee KY, Lee SY, Lee SK, Lee JH, Lee CB, Chung S, Cho YH, Choi KM, Han JS, Yoo SJ (2019) 2018 Korean Society for the study of obesity guideline for the management of obesity in Korea. J Obes Metab Syndr 28(1):40–45. https://doi.org/10.7570/jomes.2019.28.1.40
Catsburg C, Miller AB, Rohan TE (2015) Active cigarette smoking and risk of breast cancer. Int J Cancer 136(9):2204–2209
Jung S, Wang M, Anderson K, Baglietto L, Bergkvist L, Bernstein L, van den Brandt PA, Brinton L, Buring JE, Heather Eliassen A (2016) Alcohol consumption and breast cancer risk by estrogen receptor status: in a pooled analysis of 20 studies. Int J Epidemiol 45(3):916–928
Monninkhof EM, Elias SG, Vlems FA, van der Tweel I, Schuit AJ, Voskuil DW, van Leeuwen FE (2007) Physical activity and breast cancer: a systematic review. Epidemiology. 1:137–157
Bethea TN, Rosenberg L, Hong C-C, Troester MA, Lunetta KL, Bandera EV, Schedin P, Kolonel LN, Olshan AF, Ambrosone CB (2015) A case–control analysis of oral contraceptive use and breast cancer subtypes in the African American breast cancer epidemiology and risk consortium. Breast Cancer Res 17(1):22
Cheraghi Z, Poorolajal J, Hashem T, Esmailnasab N, Doosti Irani A (2012) Effect of body mass index on breast cancer during premenopausal and postmenopausal periods: a meta-analysis. PLoS ONE 7(12):e51446. https://doi.org/10.1371/journal.pone.0051446
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371(9612):569–578. https://doi.org/10.1016/s0140-6736(08)60269-x
Kawai M, Minami Y, Kuriyama S, Kakizaki M, Kakugawa Y, Nishino Y, Ishida T, Fukao A, Tsuji I, Ohuchi N (2010) Adiposity, adult weight change and breast cancer risk in postmenopausal Japanese women: the miyagi cohort study. Br J Cancer 103(9):1443–1447. https://doi.org/10.1038/sj.bjc.6605885
Tehard B, Lahmann PH, Riboli E, Clavel-Chapelon F (2004) Anthropometry, breast cancer and menopausal status: use of repeated measurements over 10 years of follow-up-results of the French E3N women's cohort study. Int J Cancer 111(2):264–269. https://doi.org/10.1002/ijc.20213
Healy L, Ryan A, Carroll P, Ennis D, Crowley V, Boyle T, Kennedy M, Connolly E, Reynolds J (2010) Metabolic syndrome, central obesity and insulin resistance are associated with adverse pathological features in postmenopausal breast cancer. Clin Oncol 22(4):281–288
Dal Maso L, Zucchetto A, Talamini R, Serraino D, Stocco CF, Vercelli M, Falcini F, Franceschi S (2008) Effect of obesity and other lifestyle factors on mortality in women with breast cancer. Int J Cancer 123(9):2188–2194. https://doi.org/10.1002/ijc.23747
Dizdar Ö, Alyamaç E (2004) Obesity: an endocrine tumor? Med Hypotheses 63(5):790–792
Maccio A, Madeddu C, Gramignano G, Mulas C, Floris C, Massa D, Astara G, Chessa P, Mantovani G (2010) Correlation of body mass index and leptin with tumor size and stage of disease in hormone-dependent postmenopausal breast cancer: preliminary results and therapeutic implications. J Mol Med (Berl) 88(7):677–686. https://doi.org/10.1007/s00109-010-0611-8
Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, Bandera EV, Hamilton KK, Grant B, McCullough M, Byers T, Gansler T (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 62(4):243–274. https://doi.org/10.3322/caac.21142
Potischman N, Swanson CA, Siiteri P, Hoover RN (1996) Reversal of relation between body mass and endogenous estrogen concentrations with menopausal status. J Natl Cancer Inst 88(11):756–758
Catsburg C, Kirsh VA, Soskolne CL, Kreiger N, Bruce E, Ho T, Leatherdale ST, Rohan TE (2014) Associations between anthropometric characteristics, physical activity, and breast cancer risk in a Canadian cohort. Breast Cancer Res Treat 145(2):545–552. https://doi.org/10.1007/s10549-014-2973-z
Wada K, Nagata C, Tamakoshi A, Matsuo K, Oze I, Wakai K, Tsuji I, Sugawara Y, Mizoue T, Tanaka K, Iwasaki M, Inoue M, Tsugane S, Sasazuki S (2014) Body mass index and breast cancer risk in Japan: a pooled analysis of eight population-based cohort studies. Ann Oncol 25(2):519–524. https://doi.org/10.1093/annonc/mdt542
Leong SP, Shen Z-Z, Liu T-J, Agarwal G, Tajima T, Paik N-S, Sandelin K, Derossis A, Cody H, Foulkes WD (2010) Is breast cancer the same disease in Asian and Western countries? World J Surg 34(10):2308–2324
Amadou A, Hainaut P, Romieu I (2013) Role of obesity in the risk of breast cancer: lessons from anthropometry. J oncol. https://doi.org/10.1155/2013/906495
De Santis CE, Ma J, Goding Sauer A, Newman LA, Jemal A (2017) Breast cancer statistics, 2017, racial disparity in mortality by state. A Cancer J Clini 67(6):439–448
Williams LA, Casbas-Hernandez P, Nichols HB, Tse CK, Allott EH, Carey LA, Olshan AF, Troester MA (2019) Risk factors for luminal a ductal carcinoma in situ (DCIS) and invasive breast cancer in the Carolina breast cancer study. PLoS ONE 14(1):e0211488
Calvocoressi L, Stowe MH, Carter D, Claus EB (2012) Postmenopausal hormone therapy and ductal carcinoma in situ: A population-based case–control study. Cancer Epidemiol 36(2):161–168
Phillips LS, Millikan RC, Schroeder JC, Barnholtz-Sloan JS, Levine BJ (2009) Reproductive and hormonal risk factors for ductal carcinoma in situ of the breast. Cancer Epidemiol Prev Biomarkers 18(5):1507–1514
Kumle M (2008) Declining breast cancer incidence and decreased HRT use. Lancet 372(9639):608–610. https://doi.org/10.1016/s0140-6736(08)61255-6
Lancet MWSCJT (2003) Breast cancer and hormone-replacement therapy in the Million Women Study. 362 (9382):419-427
Kuerer HM, Lari SA, Arun BK, Hu CY, Brewster A, Mittendorf EA, Albarracin CT, Babiera GV, Caudle AS, Wagner JL, Litton JK, Bedrosian I, Meric-Bernstam F, Lucci A, Hunt KK (2012) Biologic features and prognosis of ductal carcinoma in situ are not adversely impacted by initial large body mass. Breast Cancer Res Treat 133(3):1131–1141. https://doi.org/10.1007/s10549-012-1999-3
Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB (2005) Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am j clin nutr 81(3):555–563
Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, Lang CC, Rumboldt Z, Onen CL, Lisheng L (2005) Obesity and the risk of myocardial infarction in 27 000 participants from 52 countries: a case-control study. The Lancet 366(9497):1640–1649
Cerhan JR, Moore SC, Jacobs EJ, Kitahara CM, Rosenberg PS, Adami H-O, Ebbert JO, English DR, Gapstur SM, Giles GG 2014 A pooled analysis of waist circumference and mortality in 650,000 adults. In: Mayo Clinic Proceedings, Elsevier, pp 335–345
Toth M, Tchernof A, Sites C, Poehlman E (2000) Effect of menopausal status on body composition and abdominal fat distribution. Int J obesity 24(2):226–231
Acknowledgements
None.
Funding
No funding to declare.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest.
Ethical approval
All procedures performed in this study which involved human participants were in accordance with the ethical standards of institutional and/or national research committees and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participats included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, J.W., Han, K., Shin, D.W. et al. Obesity and breast cancer risk for pre- and postmenopausal women among over 6 million Korean women. Breast Cancer Res Treat 185, 495–506 (2021). https://doi.org/10.1007/s10549-020-05952-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05952-4