Abstract
Purpose
In a screened population, breast cancer-specific mortality is lower for screen-detected versus symptom-detected breast cancers; however, it is unclear whether this association varies by follow-up time and/or tumor characteristics. To further understand the prognostic utility of mode of detection, we examined its association with breast cancer-specific mortality, overall and by follow-up time, estrogen receptor status, tumor size, and grade.
Methods
In the Cancer Prevention Study-II Nutrition Cohort, 3975 routinely screened women were diagnosed with invasive breast cancer (1992–2015). Among 2686 screen-detected and 1289 symptom-detected breast cancers, 206 and 209 breast cancer deaths, respectively, occurred up to 24 years post diagnosis. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated from Cox proportional hazard regression models.
Results
Controlling for prognostic factors, symptom detection was associated with higher risk of breast cancer-specific death up to 5 years after diagnosis (HR≤5years = 1.88, 95% CI 1.21–2.91) this association was attenuated in subsequent follow-up (HR>5years = 1.26, 95% CI 0.98–1.63). Within tumor characteristic strata, there was a 1.3–2.7-fold higher risk of breast cancer death associated with symptom-detected cancers ≤ 5 years of follow-up, although associations were only significant for women with tumors < 2 cm (HR≤5years = 2.42, 95% CI 1.19–4.93) and for women with grade 1 or 2 tumors (HR≤5years = 2.72, 95% CI 1.33–5.57). In subsequent follow-up, associations were closer to the null.
Conclusions
Screen detection is a powerful prognostic factor for short-term survival. Among women who survived at least 5 years after breast cancer diagnosis, other clinical factors may be more predictive of breast cancer survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
It is well established that mammographic screening reduces breast cancer-specific mortality [1, 2]. However, mammography does not detect all breast cancers; 15% of women with breast cancer who attend screening are diagnosed within 1 year of a negative screening mammogram [3]. Some of these symptom-detected breast cancers were missed due to technical/interpretive errors. Others include aggressive tumors that exhibit characteristics of rapid proliferation as well as tumors with unique tumor characteristics (e.g., lobular histology, absence of in situ component) that are harder to detect by screening mammography. These cancers are of concern, in part, because they have poorer prognosis compared to screen-detected breast cancers [4, 5].
The benefit of screen detection may vary by tumor characteristics and/or follow-up time. Most prior studies have had relatively short follow-up time (up to10 years) [6,7,8,9,10,11,12,13,14,15,16,17] and/or have not stratified by tumor characteristics [18]. For example, a study including 2006 cases found variation in the survival benefit attributed to screen detection over follow-up time (up to 20 years) [18]. Only three studies have had > 9 years of follow-up time and stratified on tumor characteristics, one stratifying on stage and estrogen receptor (ER) status [7], one on stage, tumor size, and lymph node status [19], and the other on tumor size and lymph node status [20]. Furthermore, statistical methods were not used to formally test differences in associations by tumor characteristics or follow-up time.
To overcome some of the limitations of previous studies, we examined the association between mode of detection and breast cancer-specific mortality, independent of known prognostic factors, among breast cancer survivors in the American Cancer Society’s Cancer Prevention Study (CPS)-II who have been followed for up to 24 years. We rigorously tested associations by follow-up time and tumor characteristics. We hypothesized that symptom-detected, compared to screen-detected, cancers would have higher risk of death during both short- and long-term follow-ups, and that the magnitude of these associations would be stronger among women with breast cancers that have more aggressive tumor characteristics (i.e., ER-, larger (≥ 2 cm), and higher grade). Furthermore, analyses were limited to women who received routine screening mammography 2 years prior to diagnosis to minimize confounding by differences in interindividual screening patterns and ensure that symptom-detected breast cancers did not include unscreened tumors, therefore limiting potential issues with lead and length time biases.
Materials and methods
Cancer prevention study-II
The study population was drawn from the 97,783 women free of cancer when they enrolled in the CPS-II Nutrition Cohort, a prospective longitudinal study of cancer incidence and mortality that began in 1992–1993 and enrolled participants from 21 US states [21]. The Nutrition Cohort is a subset of the approximately 1.2 million US men and women enrolled in the CPS-II Mortality Cohort in 1982 [22] who lived in one of the 21 US states with a population-based state cancer registry. CPS-II Nutrition Cohort participants completed a baseline questionnaire at baseline in 1992/1993 and were sent follow-up questionnaires biennially starting in 1997. The CPS-II Nutrition Cohort is approved by the Emory University Institutional Review Board.
Study population
After enrollment, 6499 women were diagnosed with invasive breast cancer (ICD code: C50) through June 30, 2015. State cancer registry or medical records were used to confirm self-reports of breast cancer and were abstracted for tumor characteristics. For this analysis, exclusions included women who had missing self-reported mode of detection data (N = 1411), missing diagnosis date (N = 9), breast cancer diagnosis prior to enrollment in CPS-II (N = 338), distant stage breast cancer (N = 46), and those who never reported any mammography use (N = 68) or had an unknown screening history (N = 652). The final cohort included 3975 women, who were aged 41–78 years at baseline interview.
Mammographic screening status
All mammography data used in this study were self-reported. Participants completed a baseline survey in 1992, followed by biennial surveys from 1997 to 2015. All surveys queried about mammography use. In 1992, women were asked about the timing and main reason for the mammographic exam; those who responded, “part of a routine physical exam” or “had it for screening purposes” were considered to have had a screening mammogram. In 1997, women were asked about mammography use for each year over the previous 5 years (1992–1997) but were not asked about the reason for mammography; all mammograms were assumed to be for routine screening (in other years, only 3–5% of women had mammograms for diagnostic purposes). From 1999 onwards, women were asked: (1) whether they had a mammogram in the past 2 years; and (2) whether it was “for routine exams” or “for symptoms.” Women were asked to mark all that apply, and those women who reported a routine mammogram were considered to be screened.
Self-reported mammography in conjunction with date of breast cancer diagnosis was used to define screening status within approximately 2-year intervals that included a breast cancer diagnosis. For example, a woman diagnosed on August 1, 2002 was considered screened if she reported screening mammography on her 2003 survey, which covers mammography use from 2001 to 2003. A woman with the same date of diagnosis who did not report any mammogram or reported a mammogram for reasons other than screening was not considered an eligible case.
Women who were missing screening information for the survey interval that included time of diagnosis were classified as having unknown screening history (N = 652). Because we were interested in studying survival among a screened population, women with unknown screening history were excluded from all survival analyses. Women were classified as “regular routine” mammography users if they reported screening mammography on every survey up until breast cancer diagnosis. All other screened women were classified as “irregular routine” mammography users.
Mode of detection
Women diagnosed with breast cancer were sent a supplemental survey that asked about initial treatment and mode of detection. In response to the question “How was your cancer found?”, women with invasive diagnoses who responded “routine (screening) mammography” were classified as screen-detected (N = 2686) and women who responded, “by a health professional,” “husband/non-health professional,” or “self” were classified as symptom-detected (N = 1289). A validation study in a subset of 100 breast cancer cases where medical records were used to verify self-reported mode of detection showed high concordance between self-report and medical records. Twenty-five cases in each of four groups defined by mode of detection and age (< 70, 70 + years) were randomly selected. Among cases with adequate documentation of the mode of detection in the medical record, there was strong concordance (88–100%) of self-report and medical record in each of the four groups.
Outcome ascertainment
Death and cause of death were ascertained through linkage with the National Death Index. Survival time was calculated from date of breast cancer diagnosis until date of death (breast cancer-related or death from other causes), loss to follow-up, or end of follow-up (December 31, 2016), whichever came first. Median follow-up time was 12.4 years overall: 12.2 years for screen-detected cancers and 12.5 years for symptom-detected cancers.
Statistical analysis
Age-adjusted and multivariable-adjusted Cox proportional hazards regression models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CI). Screen-detected cancers were used as the referent group and breast cancer deaths were the outcome of interest. We tested for violations of the proportional hazards assumption, by using time-dependent models and visual inspection of the hazard curves. After identifying a violation of this assumption for the full follow-up period, we further tested two different time cutoffs post diagnosis: 5 years (≤ 5 & > 5) and 10 years (≤ 10 & > 10). The proportional hazards assumption was upheld within both time periods for both cutoffs. As the slope of the survival curve among the symptom-detected cases changed around 5 years post diagnosis, the 5-year cutoff was used for analyses. Age-adjusted mortality rates (per 1000 person-years) were calculated overall, and for each tumor characteristic strata and follow-up time period.
Potential covariates included clinical characteristics from the medical record or cancer registry [age at diagnosis, year of diagnosis, tumor size, SEER stage, grade, nodal status, histology, and ER, progesterone receptor (PR), and human epidermal growth factor receptor-2 (HER2) status], self-reported treatment variables [breast surgery type (mastectomy, breast conservation surgery, none), chemotherapy, radiation therapy, and hormonal/targeted therapy use], and epidemiologic factors self-reported at baseline (age at menarche, race, education, weight change from age 18 to baseline), on the survey just prior to diagnosis [menopausal status, hormone replacement therapy (HRT) use, smoking status, alcohol use, body mass index (BMI), history of benign breast disease, family history of breast cancer, and routine mammography use], or based on survey responses through end of follow-up [number of comorbidities (diabetes, hypertension, heart disease, stroke, chronic obstructive pulmonary disease)]. For each variable, missing values were assigned to a “missing” category that was used in analysis. Covariates were selected for inclusion in multivariable models using backwards elimination; covariates that made < 10% change in the estimate after removal were excluded from final models. Although ER status should have been excluded based on these criteria, this variable was retained as a variable of interest. The final adjusted model included age at diagnosis, tumor size, ER status, PR status, stage, grade, surgery, chemotherapy, weight change, and number of comorbidities.
Differences in associations between mode of detection and risk of breast cancer-specific mortality by tumor characteristics [ER status (ER+/ER-; N = 3335), tumor size (< 2 cm/≥ 2 cm; N = 3700), and grade (grade 1 & 2/grade 3 & 4; N = 3386)] and time periods were assessed by computing P-values. P-values were calculated from models that allowed for different underlying hazards for strata; these models include covariates chosen for the final model in addition to interaction terms between these variables and the stratification variable, whether that be tumor subtype or time. All stratified models excluded women who were missing data for the stratification variable of interest.
To account for residual confounding by regularity of mammography use, we conducted a sensitivity analysis restricted to women who were regular routine mammography users. All analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC).
Results
Study population
Among the 3975 breast cancer survivors who reported a screening mammogram within the 2-year survey interval when breast cancer was diagnosed, 2686 (68%) reported a screen-detected cancer and 1289 (32%) reported a symptom-detected cancer (Table 1). The average age at breast cancer diagnosis (screen-detected: 70.9 years; symptom-detected: 69.9 years) was similar in both groups. The proportion of breast cancer deaths was greater for women with symptom-detected (N = 209, 16.2%) compared to screen-detected breast cancers (N = 206, 7.7%). The mean time to breast cancer death was longer for screen-detected (9.6 years) compared to symptom-detected (8.4 years) cancers.
Overall, screen-detected cancers displayed clinical features with better prognostic characteristics compared to symptom-detected cancers. A greater proportion of screen-detected cancers were < 2 cm, localized stage, either grade 1 or 2, had no lymph node involvement and were ER+ or PR+ compared with symptom-detected cancers (Table 1). Mastectomy and chemotherapy were more frequent among women with symptom-detected cancer, while radiation therapy was more frequent among women with screen-detected breast cancer.
Mode of detection and breast cancer-specific mortality overall and by follow-up time
Over the full follow-up period, age-adjusted mortality rates were higher for symptom-detected cancers compared to screen-detected cancers (14.6 vs. 6.6 per 1000 person-years). After adjusting for known prognostic factors, symptom-detected breast cancer was associated with a 40% higher risk of breast cancer death compared to screen-detected cancers (Table 2).
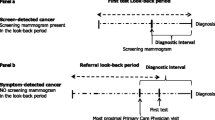
Over the follow-up time, the association between mode of detection and breast cancer-specific survival varied, as shown by visual inspection of the survival curve (Fig. 1) and statistical significance of the exposure*time interaction variable (P = 0.007), violating the proportional hazards assumption. Based on visual inspection of the survival curves (Fig. 1), the slope of the survival curve among the symptom-detected cases changes around 5 years post diagnosis. Age-adjusted mortality rates were still higher for symptom-detected cancers compared to screen-detected cancers, but their relative proportions were 3.68-fold different (12.8 vs. 3.2, respectively) in the first 5 years of follow-up after diagnosis, whereas the relative proportion was far less in the subsequent follow-up (1.60-fold, 15.5 vs. 9.7, respectively). In analyses dividing follow-up time into two periods, mode of detection was associated with higher risk of death from breast cancer during the first 5-year period post diagnosis (HR≤5 = 1.88, 95% CI 1.21–2.91), though the association was slightly attenuated afterwards (HR>5 = 1.26, 95% CI 0.98–1.63; P for difference between time periods = 0.13).
Mode of detection and breast cancer-specific mortality stratified on tumor characteristics
In analyses stratified by tumor characteristics, the age-adjusted mortality rates were consistently higher in women diagnosed with symptom-detected, compared to screen-detected, cancers (Table 3). In multivariable-adjusted models, HRs ranged from 1.24 to 1.56 over the full follow-up period. Statistically significant associations were observed only among women with tumors that were ≥ 2 cm (HR = 1.56, 95% CI 1.07–2.26) or grade 1 or 2 (HR = 1.48, 95% CI 1.07–2.04) (Table 3); however, differences by tumor characteristics were not statistically significant (P for tumor heterogeneity ≥ 0.48).
Hazard ratios for symptom detection were elevated during ≤ 5 years of follow-up (HR range: 1.30–2.72) but were only significant for women with tumors < 2 cm (HR = 2.42, 95% CI 1.19–4.93) and for women with grade 1 or 2 tumors (HR = 2.72, 95% CI 1.33–5.57; Table 3). Though HRs were slightly elevated (HR range>5: 1.10–1.89), symptom detection was not statistically significantly associated with breast cancer-specific mortality in the later follow-up period within any tumor characteristic stratum. There were no differences in effect measures observed by follow-up time period (P for period heterogeneity ≥ 0.06) or tumor characteristics (P for tumor heterogeneity ≥ 0.25).
As a sensitivity analysis (Supplemental Table 1), we restricted women who reported screening during every survey period (N = 2481) and found associations of similar magnitude and direction to those presented for the main analysis (Tables 2 and 3), although precision of the estimates was reduced.
Discussion
In our analysis of screened breast cancer survivors in the CPS-II Nutrition Cohort, we found that women diagnosed with symptom-detected cancers had an increased risk of breast cancer death within the first 5 years of diagnosis, although this association was attenuated after 5 years of follow-up. While we did not observe statistically significant differences by tumor characteristics, this pattern of higher breast cancer mortality in the first 5 years of follow-up but not the subsequent follow-up was limited to the tumors with more favorable prognostic factors.
Our reported association of mode of detection with breast cancer mortality for up to 24 years of follow-up time falls within the range of those reported in prior studies (HR range: 1.31–2.00), which had median follow-up time ranging from 3.2 to 16 years [7, 8, 12, 14, 19, 20, 23]. The range of HRs from prior studies might be due, in part, to possible attenuation of the association years after diagnosis. Our results suggest that other clinical factors may be more important when predicting breast cancer survival 5 years post diagnosis. Although we did not find significant differences in the prognostic ability of mode of detection by time period, a better understanding of prognostic factors for short- and long-term survivals is important given the increasing number of breast cancer survivors who might potentially benefit from a more personalized follow-up regimen [24].
We did not observe significant heterogeneity by tumor characteristics, which is consistent with three studies that showed that the higher risk of death from breast cancer associated with non-screen-detected cancer was similar for ER+ and ER- tumors [7], lymph node-positive and lymph node-negative cancers [20], as well as small and large tumors [19, 20]. Unfortunately, these three previous studies [7, 19, 20] did not rigorously test difference by tumor characteristics, and only two of these studies presented stratified multivariable-adjusted results [7, 20]. Additional research in screened, well-characterized populations is needed to better understand the independent contribution of mode of detection in association with mortality by known prognostic factors.
Most studies have found a survival benefit for screen-detected cancers even after adjusting for clinical prognostic features, such as tumor size and stage [19, 20, 25, 26], and/or treatment [13,14,15, 20], suggesting mode of detection may be an independent prognostic factor or a surrogate for unmeasured tumor characteristics. In our study, controlling for established prognostic factors attenuated our findings, particularly for the association with mode of detection in the first 5 years after diagnosis, although the association remained statistically significant. Further, most previous studies that compared mortality of symptom-detected and screen-detected breast cancers are limited by sparse lifestyle data [6,7,8,9,10,11,12,13,14,15,16,17, 19, 20, 23, 25] which may confound associations. The CPS-II Nutrition Cohort allowed us to examine several potential confounders, although the majority were not included in the final model. While our study was not conducted within a screening trial, sensitivity of mammography-history reporting is high, [27] and we had detailed self-reported biennial information on screening history. With these data, we limited bias in our main analysis by restricting the analytic sample to women who reported screening during the interval in which they were diagnosed with cancer. This approach allowed us to define a target population of screened women, and maximize “true” interval cancers in our symptom-detected category. The proportion of symptom-detected cancers in our study (32%), based on the roughly biennial screening routine captured by surveys, is comparable to the interval cancer rate from a large screening cohort [3] as it is roughly double the rate (15%) calculated from populations that screened annually. We had further assurance that screening patterns had little to no influence on our observed results based on our sensitivity analysis restricted to women who indicated screen adherence at all surveys prior to diagnosis [28]. We found associations with survival were slightly stronger than those observed in the full data set, supporting our main results.
Our study population included older women (average age was 70 years at diagnosis), older birth cohorts (1914–1951), and mostly higher socio-economic (SES) status and self-described white women [21], which might limit the generalizability of our results. Approximately 25% of breast cancer cases did not complete the follow-up survey sent to women with self-reported breast cancer and were therefore excluded due to missing mode of detection data. These women had a higher breast cancer mortality rate compared to women in the analytic set (28% vs. 10%), suggesting that our analytic set was enriched for cancers with a better prognosis. Furthermore, associations between mode of detection and breast cancer-specific mortality may differ by age and race. Indeed, higher risk of interval/symptom-detected breast cancers are associated with both younger age (age < 50 years) [15, 29,30,31,32,33,34], in part to increased mammographic screening sensitivity with age [35, 36], and non-white racial and low SES groups [37, 38]. We were unable to account for mammographic density in our study, yet high mammographic density is associated with both false-negative screens [39] and increased breast cancer risk [40], but not survival [41]. Moreover, the relevance of mammographic density data to our analysis is unclear as studies evaluating the relationship between mammographic density, mode of detection, and breast cancer death show conflicting associations [42, 43]. We addressed lead time and length time by limiting our study population to women who reported screening mammography before diagnosis, adjusting for stage, and stratifying by ER status and tumor size, although other factors might have biased our results. Nevertheless, our results represent the lower bound of the range of possible associations between mode of detection and breast cancer-specific mortality in regularly screened women.
Our research shows that screen detection is a powerful prognostic factor for short-term survival even for routinely screened women and cases with good-prognosis tumors in the first 5 years after diagnosis. Building upon this research, future studies should confirm these findings using better characterized breast cancer subtypes such as intrinsic subtypes or the new American Joint Committee on Cancer (AJCC) prognostic stage groups [44]. However, as new screening modalities with improved sensitivity become more widely available, mode of detection may contribute less to survival differences. Regardless, our results suggest the utility of incorporating mode of detection in the development and implementation of risk-stratified survivorship care [45].
References
Marmot MG, Altman DG, Cameron DA, Dewar JA, Thompson SG, Wilcox M (2013) The benefits and harms of breast cancer screening: an independent review. Br J Cancer 108(11):2205–2240. https://doi.org/10.1038/bjc.2013.177
Lauby-Secretan B, Scoccianti C, Loomis D, Benbrahim-Tallaa L, Bouvard V, Bianchini F, Straif K (2015) Breast-cancer screening–viewpoint of the IARC Working Group. N Engl J Med 372(24):2353–2358. https://doi.org/10.1056/NEJMsr1504363
Kerlikowske K (1997) Efficacy of screening mammography among women aged 40 to 49 years and 50 to 69 years: comparison of relative and absolute benefit. JNCI 22:79–86
Porter PL, El-Bastawissi AY, Mandelson MT, Lin MG, Khalid N, Watney EA, Cousens L, White D, Taplin S, White E (1999) Breast tumor characteristics as predictors of mammographic detection: comparison of interval- and screen-detected cancers. JNCI 91(23):2020–2028
Domingo L, Salas D, Zubizarreta R, Bare M, Sarriugarte G, Barata T, Ibanez J, Blanch J, Puig-Vives M, Fernandez A, Castells X, Sala M (2014) Tumor phenotype and breast density in distinct categories of interval cancer: results of population-based mammography screening in Spain. Breast Cancer Res 16(1):R3. https://doi.org/10.1186/bcr3595
Anttinen J, Kautiainen H, Kuopio T (2006) Role of mammography screening as a predictor of survival in postmenopausal breast cancer patients. Br J Cancer 94(1):147–151. https://doi.org/10.1038/sj.bjc.6602895
Dong W, Berry DA, Bevers TB, Kau SW, Hsu L, Theriault RL, Shen Y (2008) Prognostic role of detection method and its relationship with tumor biomarkers in breast cancer: the University of Texas M.D. Anderson Cancer Center experience. Cancer Epidemiol Prev Biomark 17(5):1096–1103. https://doi.org/10.1158/1055-9965.epi-08-0201
Gill PG, Farshid G, Luke CG, Roder DM (2004) Detection by screening mammography is a powerful independent predictor of survival in women diagnosed with breast cancer. Breast (Edinburgh, Scotland) 13(1):15–22. https://doi.org/10.1016/s0960-9776(03)00169-3
Crispo A, Barba M, D’Aiuto G, De Laurentiis M, Grimaldi M, Rinaldo M, Caolo G, D’Aiuto M, Capasso I, Esposito E, Amore A, Di Bonito M, Botti G, Montella M (2013) Molecular profiles of screen detected vs. symptomatic breast cancer and their impact on survival: results from a clinical series. BMC Cancer 13:15. https://doi.org/10.1186/1471-2407-13-15
Redondo M, Funez R, Medina-Cano F, Rodrigo I, Acebal M, Tellez T, Roldan MJ, Hortas ML, Bellinvia A, Pereda T, Domingo L, Morales-Suarez Varela M, Sala M, Rueda A (2012) Detection methods predict differences in biology and survival in breast cancer patients. BMC Cancer 12:604. https://doi.org/10.1186/1471-2407-12-604
Wishart GC, Greenberg DC, Britton PD, Chou P, Brown CH, Purushotham AD, Duffy SW (2008) Screen-detected vs symptomatic breast cancer: is improved survival due to stage migration alone? Br J Cancer 98(11):1741–1744. https://doi.org/10.1038/sj.bjc.6604368
Falck AK, Rome A, Ferno M, Olsson H, Chebil G, Bendahl PO, Ryden L (2016) St Gallen molecular subtypes in screening-detected and symptomatic breast cancer in a prospective cohort with long-term follow-up. Br J Surg 103(5):513–523. https://doi.org/10.1002/bjs.10070
Sihto H, Lundin J, Lehtimaki T, Sarlomo-Rikala M, Butzow R, Holli K, Sailas L, Kataja V, Lundin M, Turpeenniemi-Hujanen T, Isola J, Heikkila P, Joensuu H (2008) Molecular subtypes of breast cancers detected in mammography screening and outside of screening. Clin Cancer Res 14(13):4103–4110. https://doi.org/10.1158/1078-0432.ccr-07-5003
Olsson A, Borgquist S, Butt S, Zackrisson S, Landberg G, Manjer J (2012) Tumour-related factors and prognosis in breast cancer detected by screening. Br J Surg 99(1):78–87. https://doi.org/10.1002/bjs.7757
Domingo L, Blanch J, Servitja S, Corominas JM, Murta-Nascimento C, Rueda A, Redondo M, Castells X, Sala M (2013) Aggressiveness features and outcomes of true interval cancers: comparison between screen-detected and symptom-detected cancers. Eur J Cancer Prev 22(1):21–28. https://doi.org/10.1097/CEJ.0b013e328354d324
Allgood PC, Duffy SW, Kearins O, O’Sullivan E, Tappenden N, Wallis MG, Lawrence G (2011) Explaining the difference in prognosis between screen-detected and symptomatic breast cancers. Br J Cancer 104(11):1680–1685. https://doi.org/10.1038/bjc.2011.144
Fong Y, Evans J, Brook D, Kenkre J, Jarvis P, Gower Thomas K (2014) The incidence and 10-year survival of interval breast cancers in Wales. Clin Radiol 69(4):e168–172. https://doi.org/10.1016/j.crad.2013.11.018
Tabar L, Dean PB, Chen TH, Yen AM, Chen SL, Fann JC, Chiu SY, Ku MM, Wu WY, Hsu CY, Chen YC, Beckmann K, Smith RA, Duffy SW (2019) The incidence of fatal breast cancer measures the increased effectiveness of therapy in women participating in mammography screening. Cancer 125(4):515–523. https://doi.org/10.1002/cncr.31840
Shen Y, Yang Y, Inoue LYT, Munsell MF, Miller AB, Berry DA (2005) Role of detection method in predicting breast cancer survival: analysis of randomized screening trials. JNCI 97(16):1195–1203. https://doi.org/10.1093/jnci/dji239
Mook S, Van’t Veer LJ, Rutgers EJ, Ravdin PM, van de Velde AO, van Leeuwen FE, Visser O, Schmidt MK (2011) Independent prognostic value of screen detection in invasive breast cancer. JNCI 103(7):585–597. https://doi.org/10.1093/jnci/djr043
Calle EE, Rodriguez C, Jacobs EJ, Almon ML, Chao A, McCullough ML, Feigelson HS, Thun MJ (2002) The American cancer society cancer prevention study II nutrition cohort: rationale, study design, and baseline characteristics. Cancer 94(9):2490–2501. https://doi.org/10.1002/cncr.101970
Garfinkel L (1985) Selection, follow-up, and analysis in the American cancer society prospective studies. Natl Cancer Inst Monogr 67:49–52
Lehtimaki T, Lundin M, Linder N, Sihto H, Holli K, Turpeenniemi-Hujanen T, Kataja V, Isola J, Joensuu H, Lundin J (2011) Long-term prognosis of breast cancer detected by mammography screening or other methods. Breast Cancer Res 13(6):R134. https://doi.org/10.1186/bcr3080
Bluethmann SM, Mariotto AB, Rowland JH (2016) Anticipating the “Silver Tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Prev Biomark 25(7):1029–1036. https://doi.org/10.1158/1055-9965.Epi-16-0133
Dawson SJ, Duffy SW, Blows FM, Driver KE, Provenzano E, LeQuesne J, Greenberg DC, Pharoah P, Caldas C, Wishart GC (2009) Molecular characteristics of screen-detected vs symptomatic breast cancers and their impact on survival. Br J Cancer 101(8):1338–1344
Joensuu H, Lehtimäki T, Holli K et al (2004) RIsk for distant recurrence of breast cancer detected by mammography screening or other methods. JAMA 292(9):1064–1073. https://doi.org/10.1001/jama.292.9.1064
Rauscher GH, Johnson TP, Cho YI, Walk JA (2008) Accuracy of self-reported cancer-screening histories: a meta-analysis. Cancer Epidemiol Prev Biomark 17(4):748–757. https://doi.org/10.1158/1055-9965.Epi-07-2629
Gierisch JM, Earp JA, Brewer NT, Rimer BK (2010) Longitudinal predictors of nonadherence to maintenance of mammography. Cancer Epidemiol Prev Biomark 19(4):1103–1111. https://doi.org/10.1158/1055-9965.Epi-09-1120
Porter PL, El-Bastawissi AY, Mandelson MT, Lin MG, Khalid N, Watney EA, Cousens L, White D, Taplin S, White E (1999) Breast tumor characteristics as predictors of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst 91(23):2020–2028. https://doi.org/10.1093/jnci/91.23.2020
Tabar L, Fagerberg G, Chen HH, Duffy SW, Gad A (1995) Screening for breast cancer in women aged under 50: mode of detection, incidence, fatality, and histology. J Med Screen 2(2):94–98
Lowery JT, Byers T, Hokanson JE, Kittelson J, Lewin J, Risendal B, Singh M, Mouchawar J (2011) Complementary approaches to assessing risk factors for interval breast cancer. Cancer Causes Control 22(1):23–31. https://doi.org/10.1007/s10552-010-9663-x
Caldarella A, Puliti D, Crocetti E, Bianchi S, Vezzosi V, Apicella P, Biancalani M, Giannini A, Urso C, Zolfanelli F, Paci E (2013) Biological characteristics of interval cancers: a role for biomarkers in the breast cancer screening. J Cancer Res Clin Oncol 139(2):181–185. https://doi.org/10.1007/s00432-012-1304-1
Klemi PJ, Toikkanen S, Rasanen O, Parvinen I, Joensuu H (1997) Mammography screening interval and the frequency of interval cancers in a population-based screening. Br J Cancer 75(5):762–766
Ikeda DM, Andersson I, Wattsgard C, Janzon L, Linell F (1992) Interval carcinomas in the Malmo Mammographic Screening Trial: radiographic appearance and prognostic considerations. Am J Roentgenol 159(2):287–294. https://doi.org/10.2214/ajr.159.2.1632342
May DS, Lee NC, Nadel MR, Henson RM, Miller DS (1998) The national breast and cervical cancer early detection program: report on the first 4 years of mammography provided to medically underserved women. Am J Roentgenol 170(1):97–104. https://doi.org/10.2214/ajr.170.1.9423608
Kerlikowske K, Carney PA, Geller B, Mandelson MT, Taplin SH, Malvin K, Ernster V, Urban N, Cutter G, Rosenberg R, Ballard-Barbash R (2000) Performance of screening mammography among women with and without a first-degree relative with breast cancer. Ann Intern Med 133(11):855–863
Rauscher GH, Allgood KL, Whitman S, Conant E (2012) Disparities in screening mammography services by race/ethnicity and health insurance. J Womens Health 21(2):154–160. https://doi.org/10.1089/jwh.2010.2415
Mortel M, Rauscher GH, Murphy AM, Hoskins K, Warnecke RB (2015) Racial and ethnic disparity in symptomatic breast cancer awareness despite a recent screen: the role of tumor biology and mammography facility characteristics. Cancer Epidemiol Prev Biomark 24(10):1599–1606. https://doi.org/10.1158/1055-9965.Epi-15-0305
Mandelson MT, Oestreicher N, Porter PL, White D, Finder CA, Taplin SH, White E (2000) Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. JNCI 92(13):1081–1087
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Prev Biomark 15(6):1159–1169. https://doi.org/10.1158/1055-9965.Epi-06-0034
Gierach GL, Ichikawa L, Kerlikowske K, Brinton LA, Farhat GN, Vacek PM, Weaver DL, Schairer C, Taplin SH, Sherman ME (2012) Relationship between mammographic density and breast cancer death in the breast cancer surveillance consortium. JNCI 104(16):1218–1227. https://doi.org/10.1093/jnci/djs327
van der Waal D, Verbeek ALM, Broeders MJM (2018) Breast density and breast cancer-specific survival by detection mode. BMC Cancer 18:386. https://doi.org/10.1186/s12885-018-4316-7
Eriksson L, Czene K, Rosenberg LU, Törnberg S, Humphreys K, Hall P (2013) Mammographic density and survival in interval breast cancers. Breast Cancer Res 15(3):R48. https://doi.org/10.1186/bcr3440
Hortobagyi NGCJ, D’Orsi CJ et al (2017) AJCC Cancer Staging Manual, 8th edn. Springer, New York
Nekhlyudov L, O’Malley DM, Hudson SV (2017) Integrating primary care providers in the care of cancer survivors: gaps in evidence and future opportunities. Lancet Oncol 18(1):e30–e38. https://doi.org/10.1016/s1470-2045(16)30570-8
Acknowledgements
The authors express sincere appreciation to all Cancer Prevention Study participants, and to each member of the study and biospecimen management group. The authors would like to acknowledge the contribution to this study from central cancer registries supported through the Centers for Disease Control and Prevention’s National Program of Cancer Registries and cancer registries supported by the National Cancer Institute’s Surveillance Epidemiology and End Results Program.
Disclaimer
The views expressed here are those of the authors and do not necessarily represent the American Cancer Society or the American Cancer Society–Cancer Action Network.
Funding
Dr. Puvanesarajah was supported by the American Cancer Society’s Cancer Prevention Studies Post-Doctoral Fellowship Program. The American Cancer Society funds the creation, maintenance, and updating of the Cancer Prevention Study-II cohort.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Puvanesarajah, S., Gapstur, S.M., Patel, A.V. et al. Mode of detection and breast cancer mortality by follow-up time and tumor characteristics among screened women in Cancer Prevention Study-II. Breast Cancer Res Treat 177, 679–689 (2019). https://doi.org/10.1007/s10549-019-05322-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05322-9