Abstract
Purpose
Weight gain in adulthood is a risk factor for breast cancer; however, the impact on age of onset is unknown. The objective of this study was to investigate whether weight gain from early- to mid-adulthood influenced the timing of breast cancer onset.
Methods
Increase in body mass index (BMI) from lowest adult BMI to BMI at diagnosis and age at which these events occurred were calculated from breast cancer survivors enrolled in a weight loss trial (n = 660). Quartiles (Q) of the average increase in BMI were determined and associations between weight gain and age at disease onset were analyzed using analysis of covariance and spline regression models.
Results
A significant linear trend was observed across the quartiles of BMI change for earlier age at diagnosis [Q1 52.3 (± 0.73), Q2 51.9 (± 0.70), Q3 49.6 (± 0.66), Q4 47.3 (± 0.67), p < 0.0001] after adjusting for potential confounders. In analyses that stratified by tumor subtype and menopausal status, significant linear trends continued to be observed for earlier age at diagnosis across quartiles of BMI for ER ± , PR ± , HER2 + , as well as pre- and postmenopausal status (p-values < 0.001).
Conclusions
Women who gain excess weight during adulthood are not only at risk for breast cancer, but also may experience earlier onset of disease and reduced cancer-free years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent global estimates indicate that two million women were diagnosed with breast cancer in 2018, and the incidence rate is expected to continue to climb to over three million cases per year by 2040 [1]. A key lifestyle factor driving the current and projected breast cancer rates is excess adiposity and obesity. Obesity is recognized as a significant risk factor for breast cancer and is not only associated with incidence, but also worse prognosis, increased morbidity, and reduced survival rates in breast cancer patients [2].
The linkage between breast cancer and obesity is a major public health issue given that, worldwide, 40% of women are classified as overweight status [body mass index (BMI 25–29.9)] and 15% are obese (BMI ≥ 30) [3]. The obesity pandemic is expected to increase globally with Westernization of developing countries. In the US, where obesity rates are among the highest in the world, 40% of women are obese and nearly 27% are classified as overweight [4]. These trends may be partly due to steady weight gain from early- to mid-adulthood resulting in a transition from normal weight to overweight or obesity [5]. Results from the CARDIA study, a longitudinal epidemiological study comprised four urban cities in the US, showed that BMI increased from 23.1 to 28.3 in non-Hispanic white women and 26.2 to 33.8 in black women over a 25 year period that corresponded with ages 26 to 51 years [6]. In the Nurses’ Health Study, a cohort of predominantly non-Hispanic white women, recent analyses showed steady weight gain throughout adulthood with women gaining an average 12.6 kg from age 18 to 55 years [7]. These current trends of weight gain in women and the growing global obesity pandemic are particularly concerning given that previous studies have consistently shown significant positive associations between risk for breast cancer and weight gain during adulthood in women [8,9,10,11].
In a recent review, Berger expanded on the relationship between adult weight gain and breast cancer and hypothesized that exposure to excessive weight gain (i.e., weight gain that results in overweight or obesity) throughout adulthood may not only be a risk factor for breast cancer but could also reduce the latency period of malignancy and thus expedite the onset of breast cancer [12]. Further, earlier exposure to an obesogenic host environment could drive cancer progression, thus influencing the timing of cancer onset. Indeed, the burden of cancer appears to be shifting to an earlier age. Sung et al. showed that in the US obesity-related cancers are being diagnosed at an earlier age than previous generations [13]. In support of this hypothesis, results from a previous case–control study showed that among pancreatic cancer patients, those who had onset of obesity between the ages of 20 and 49 years were diagnosed with pancreatic cancer 5 years earlier than those who were of normal weight during this same time period [14]. Whether the timing of adult weight gain is associated with earlier onset of breast cancer is unclear, but warrants investigation given the prevalence of excessive weight gain in women and its positive association with risk for breast cancer.
The purpose of this study was to investigate whether adult weight gain was associated with earlier onset of breast cancer. A secondary aim of this study was to explore whether the association between onset of breast cancer and adult weight gain was modified by tumor subtype or menopausal status at the time of breast cancer diagnosis.
Methods
Study population
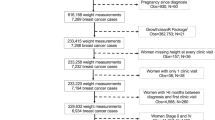
This study utilized data from the Exercise and Nutrition to Enhance Recovery and Good Health for You (ENERGY) Trial, a multi-site weight loss trial for breast cancer survivors [15]. Eligibility for the study included the following: 21 years of age or older; a history of breast cancer (stages I [≥ 1 cm], II, or III) diagnosed within the previous 5 years; completion of initial therapies; BMI between 25 and 45 kg/m2; and able to comply with all required study procedures and schedule. A full listing of exclusion criteria is available elsewhere [15]. Institutional Review Board approval from the participating institutions (University of Alabama at Birmingham, University of California, San Diego, University of Colorado, Denver, and Washington University in St. Louis) was obtained and all participants provided written informed consent.
At baseline, demographic information was collected via surveys in which participants self-reported race (White, Black, Asian, American Indian, Hawaiian/Pacific Islander, Mixed/Other), education level (less than high school graduate, some college, college graduate, post-college), and smoking status (ever smoker, never smoker). Participants completed a questionnaire and documented their menopausal status at diagnosis (premenopausal, perimenopausal, postmenopausal), lowest adult weight, weight at breast cancer diagnosis, and age at each of these time points. Height was directly measured at enrollment and was used to calculate BMI. Medical records were obtained to confirm breast cancer diagnosis and disease characteristics including tumor receptor status (estrogen receptor [ER], progesterone receptor [PR], Her2/neu, triple negative) stage (I [≥ 1 cm], II or III) and grade (I, II or III). A full description of the parent study and CONSORT diagram have been previously published [15].
Analytical methods
Because this study was designed to assess the influence of increased BMI during adulthood on age at breast cancer onset, data from 33 women were excluded for the following reasons: incomplete data on lowest adult weight, age at lowest adult weight or weight at breast cancer diagnosis (n = 19), lowest body weight occurring after breast cancer diagnosis (n = 11), or lowest adult weight was greater than their breast cancer diagnosis weight (n = 2). One participant was excluded due to a diagnosis of in situ rather than invasive disease.
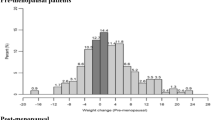
In this study population, the mean lowest adult BMI [21.5 (21.2, 21.7)] occurred at 27.2 (26.5, 27.8) years of age and was considered indicative of body weight during early adulthood. Breast cancer diagnosis occurred at 53.7 (53.0, 54.4) years of age and BMI at this time point [30.4 (29.9, 30.8)] was considered indicative of mid-adulthood body weight. Lowest adult BMI was subtracted from BMI at the time of breast cancer diagnosis and divided by the numbers of years between these time points to calculate the increase in BMI from early- to mid-adulthood. Quartiles of increase in BMI were then determined. Descriptive characteristics of participants were determined according to quartiles of increase in BMI using ANOVA. Data are presented as mean (95% confidence interval) for continuous variables and frequency (percentage) for categorical variables. Self-reported race was categorized as White, Black, and Other. Analysis of covariance (ANCOVA) with age at breast cancer diagnosis as the dependent variable was used to determine the least squares means and standard error for each quartile of in BMI adjusting for race, study site, and menopausal status at diagnosis. To evaluate the dose–response between increase in BMI (independent variable) and age at breast cancer diagnosis (dependent variable), we used restricted cubic spline regression models adjusting for race, study site, and menopausal status at diagnosis [16]. To prevent estimation bias in the models, we excluded individuals in the top 5th percentile of increase in BMI. In premenopausal women, the best fitting model included spline knots at the 5th, 25th, and 75th percentiles, corresponding to 0.12, 0.24, and 0.49 kg/m2/year. In postmenopausal women, the best model included spline knots at the 40th, 60th, 80th, and 95th percentiles, corresponding to 0.25, 0.33, 0.44 and 0.62 kg/m2/year. Difference in age at diagnosis was calculated for specific values of change in BMI (0.2, 0.4, and 0.6) compared to Q1 (0.15/kg/m2/year change in BMI).
Results
Data from 660 breast cancer survivors were included in this study. The overall characteristics of the participants are presented in Table 1. Most participants were non-Hispanic white (85%), high school graduates (86%), and never smoked (65%). Lowest adult BMI was 21.5 kg/m2 (95% CI 21.2–21.7) and occurred at 27.2 (95% CI 26.5–27.8) years of age. At the time of breast cancer diagnosis, most women were postmenopausal (58%), average age of 53.7 (95% CI 53.0–54.4) years and BMI of 30.4 kg/m2 (95% CI 29.9–30.8). The majority of participants had stage II disease (52%), tumors that were ER or PR positive (75%) and Her2 negative (78%). Fourteen percent of tumors were triple negative. Overall, increase in BMI was 0.42 (0.38–0.46) kg/m2/year.
The differences in characteristics of study participants according to quartiles of increase in BMI are presented in Table 2. Differences across the quartiles were observed for race and menopausal status at diagnosis. There was a significant trend for lowest adult BMI to increase across the quartiles suggesting that women with higher increases in BMI were heavier, even at their lowest weight. Differences across quartiles were observed for BMI at diagnosis and age at diagnosis indicating that women with higher increase in BMI were significantly heavier and younger at the time of breast cancer diagnosis. No differences in stage, grade, or receptor status were observed.
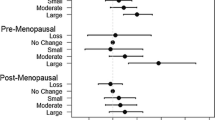
Based on these data, associations between quartiles of increase in BMI and age at breast cancer diagnosis were examined further (Table 3). Overall, significant linear trends were observed for earlier age at breast cancer diagnosis across quartiles of increase in BMI after adjusting for race, recruitment site, and menopausal status. Women in quartile 4, i.e., those who had the greatest increase in BMI, were diagnosed with breast cancer at 47.1 ± 0.67 years of age, whereas women who had the lowest gain in BMI (quartile 1) at 52.2 ± 0.73 years of age. In analyses that stratified by tumor characteristics and menopausal status, significant linear trends were observed for ER ± , PR ± , Her2/neu as well as pre- and postmenopausal status. Similar linear trends were observed for triple-negative tumors and for women who were perimenopausal at time of diagnosis but these associations did not reach statistical significance.
Spline regression analyses confirmed a highly significant association between increase in BMI and earlier age at diagnosis for both premenopausal (p = 0.01) and postmenopausal (p < 0.0001) women (Fig. 1a, b, respectively). In premenopausal women, there was a gradual, monotonic decrease in age at diagnosis with increase in BMI (test for non-linear association p = 0.73); however, only rates of BMI change of 0.55 kg/m2/year and above were associated with a significant decrease in the age at diagnosis. In postmenopausal women, the rate of decrease in age at diagnosis was gradual up to 0.3 kg/m2/year, steeper up to 0.5 kg/m2/year, and then leveled off (p for non-linear association = 0.06). Estimated differences (95% CI) in age at diagnosis for postmenopausal women with increased rate in BMI of 0.2, 0.4, or 0.6 kg/m2/year were − 0.4 (− 1.0 to 0.2), − 4.0 (− 5.8 to − 2.2), and − 6.6 (− 8.7 to − 4.5) years earlier compared with a woman with 0.15 kg/m2/year change in BMI.
Adjusted dose–response association between the annual change in BMI kg/m2/year (from lowest adult weight to weight at diagnosis) and age at invasive breast cancer diagnosis for premenopausal women (a) and postmenopausal women (b). The Y-axis represents the difference in age at diagnosis between women with varying rates of BMI change with the default value of 0.15 kg/m2/year (mean value of first quartile)
Discussion
The results of this study suggest that adult weight gain is associated with earlier onset of breast cancer. Overall, women with the highest adult weight gain [0.87 (0.75, 0.99) kg/m2/year] were diagnosed with breast cancer 5 years earlier than women with the lowest adult weight gain [0.15 ± (0.14, 0.16) kg/m2/year]. This trend was observed in all breast cancer subtypes and in both pre- and postmenopausal women, although the effect was stronger in postmenopausal women. Our findings provide evidence that not only obesity is a risk factor for breast cancer, but also that excessive weight gain throughout adulthood significantly reduces the latency period for breast cancer onset.
Previous studies have shown that chronic diseases, once considered diseases associated with aging, are being diagnosed earlier in life as a result of the obesity pandemic. In particular, type 2 diabetes [17], gout [18], kidney disease [19], and indicators of heart disease [20] are among some of the most common obesity-related conditions with earlier onset as a result of excessive adult weight gain. A recent large epidemiological study investigated the loss of disease-free years attributed to obesity-related diseases including type 2 diabetes, heart disease, stroke, and cancer [21]. Women classified as having severe obesity (BMI ≥ 35 kg/m2) had an overall reduction in disease-free living of approximately 7 years and women with mild obesity (BMI 30–34.9 kg/m2) had a reduction of nearly 3 years compared to normal weight women of similar age. Similar to these previous reports, we observed significant reduction in cancer-free years attributed to adult weight gain. Collectively, our results and those of others [14] indicate that progressive weight gain throughout adulthood drives progression of chronic disease to manifest at an earlier age.
There are several potential mechanisms that may be involved in breast cancer progression associated with obesity. Excessive adiposity stimulates low-grade inflammation, oxidative stress, and proinflammatory cytokines; increases circulating insulin concentrations; alters adipocytokine proteins, sex steroid hormones, and binding proteins; and may alter intestinal microbiota [12]. These changes are believed to play major roles in driving cancer progression by increasing tumor growth, angiogenesis, and metastasis [22]. We hypothesize that higher rates of weight gain from early- to mid-adulthood result in chronic exposure to adiposity-driven factors at an earlier age thus providing a host environment that accelerates malignant growth and earlier onset of cancer. Of note, we observed an association between adult weight gain and earlier onset of breast cancer for all tumor subtypes. While breast cancer cells from different tumor subtypes share similar characteristics such as the ability to evade the body’s immune system, inhibition of apoptosis, and increased proliferation, they express different molecular profiles; thus, breast cancer is considered a heterogeneous disease [23]. How the metabolic, inflammatory, and hormonal disturbances brought on by obesity independently or synergistically interact with different tumor receptor subtypes and underlying molecular profiles is unclear, but warrants further investigation.
Our findings have several implications. Our data underscore a critical public health need for weight maintenance and obesity prevention awareness in young adults [24]. Obesity is recognized as a preventable lifestyle risk factor for cancer and as such healthy diet and regular physical activity should be promoted across the lifespan [25]. We postulate that although fat tissue accumulates as part of the normal aging process, slowing the rate of fat mass accumulation through healthy diet and physical activity could extend cancer-free living. In support of this premise, we noted that women who gained the least amount of weight were diagnosed significantly later in life. This may be important for breast cancer prognosis considering that younger women diagnosed with breast cancer tend to have more aggressive disease and poorer prognosis [26]. Further, women who gain excess weight during early- to mid-adulthood may require earlier and/or more aggressive breast cancer screening. Identifying women who may benefit from earlier screening could lead to expedited diagnosis and treatment thus improving breast cancer outcomes.
This study has some limitations which should be noted. First, we were unable to assess the influence of hormone replacement therapy, parity, family history, and history of physical activity on the association between adult weight gain and age at onset of breast cancer diagnosis; therefore, the influence of these factors on our findings is unknown. However, it should be noted that while these factors have been associated with overall risk for breast cancer, to our knowledge no previous study has observed that they are associated with earlier onset of breast cancer. Second, although our results showed a strong dose–response between adult weight gain and age of breast cancer onset, we cannot rule-out the potential for recall bias given the retrospective collection of weight history. However, a recent study from the Women’s Health Initiative found strong concordance between self-reported and measured weight (r = 0.97) suggesting that self-reported weight is a reliable measure in epidemiological studies [27]. A key strength of this study was that it leveraged data from a large clinical trial that included a heterogenous sample of women with invasive breast cancer who were recruited across the U.S. Further, where previous studies have used weight at 18 or 20 years of age to investigate an association between weight gain and breast cancer incidence [8, 9, 11], these ages may not represent the lowest adult body weight [28]. A unique strength of this study was that we were able to capture adult weight gain starting with a baseline time point which reflects the lowest adult weight which occurred at approximately 27, and not 18 or 20 years of age. Although we could not account for the effects of exposure to childhood or lifelong obesity or possible fluctuations in body weight during adulthood, our data represent the net weight gain from the lowest weight during adulthood until breast cancer diagnosis and its influence on the timing of disease onset.
In conclusion, we provide evidence that increased body weight from early- to mid-adulthood not only portends risk, but also appears to accelerate the onset of breast cancer resulting in earlier onset and reduced cancer-free years. Women who gain large amounts of weight during early- to mid-adulthood may be at risk for developing breast cancer at a younger age. Such data point to the need of promoting lifestyle modification consonant with weight management and control and the potential need for more vigilant screening among women who manifest excessive weight gain. Additional studies, that investigate the timing of weight gain and onset of breast cancer, are needed to confirm these findings.
References
Ferlay J, Colombet M, Soerjomataram I et al (2018) Global and regional estimates of the incidence and mortality for 38 cancers: GLOBOCAN 2018. International Agency for Research on Cancer/World Health Organization, Lyon
Chan DS, Norat T (2015) Obesity and breast cancer: not only a risk factor of the disease. Curr Treat Options Oncol 16:22. https://doi.org/10.1007/s11864-015-0341-9
World Health Organization. Obesity and overweight. [Web page]. http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 26 Oct 2018
U.S. Department of Health and Human Services. Overweight and obesity statistics. [Web page]. https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity. Accessed 8 Nov 2018
Sheehan TJ, DuBrava S, DeChello LM, Fang Z (2003) Rates of weight change for black and white Americans over a twenty year period. Int J Obes Relat Metab Disord 27:498–504
Dutton GR, Kim Y, Jacobs DR Jr et al (2016) 25-Year weight gain in a racially balanced sample of U.S. adults: the CARDIA study. Obesity 24:1962–1968. https://doi.org/10.1002/oby.21573
Zheng Y, Manson JE, Yuan C et al (2017) Associations of weight gain from early to middle adulthood with major health outcomes later in life. JAMA 318:255–269
Feigelson HS, Jonas CR, Teras LR, Thun MJ, Calle EE (2004) Weight gain, body mass index, hormone replacement therapy, and postmenopausal breast cancer in a large prospective study. Cancer Epidemiol Biomark Prev 13:220–224
Ahn J, Schatzkin A, Lacey JV Jr, Albanes D, Ballard-Barbash R, Adams KF et al (2007) Adiposity, adult weight change, and postmenopausal breast cancer risk. Arch Intern Med 167:2091–2102
Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE (2006) Adult weight change and risk of postmenopausal breast cancer. JAMA 296:193–201
Harvie M, Howell A, Vierkant RA, Kumar N, Cerhan JR, Kelemen LE et al (2005) Association of gain and loss of weight before and after menopause with risk of postmenopausal breast cancer in the Iowa women’s health study. Cancer Epidemiol Biomark Prev 14:656–661
Berger NA (2018) Young adult cancer: influence of the obesity pandemic. Obesity. 26:641–650. https://doi.org/10.1002/oby.22137
Sung H, Siegel RL, Rosenberg PS, Jemal A (2019) Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health S2468–2667(18):30267–30276. https://doi.org/10.1016/S2468-2667(18)30267-6
Li D, Morris JS, Liu J, Hassan MM, Day RS, Bondy ML, Abbruzzese JL (2009) Body mass index and risk, age of onset, and survival in patients with pancreatic cancer. JAMA 301:2553–2562
Rock CL, Byers TE, Colditz GA, Demark-Wahnefried W, Ganz PA, Wolin KY et al (2013) Reducing breast cancer recurrence with weight loss, a vanguard trial: the exercise and nutrition to enhance recovery and good health for you (ENERGY) trial. Contemp Clin Trials 34:282–295
Desquilbet L, Mariotti F (2010) Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 29:1037–1057
Stokes A, Collins JM, Grant BF, Scamuffa RF, Hsiao CW, Johnston SS et al (2018) Obesity progression between young adulthood and midlife and incident diabetes: a retrospective cohort study of US adults. Diabetes Care 41:1025–1031
DeMarco MA, Maynard JW, Huizinga MM et al (2011) Obesity and younger age at gout onset in a community-based cohort. Arthr Care Res 63:1108–1114
Grubbs V, Lin F, Vittinghoff E et al (2014) Body mass index and early kidney function decline in young adults: a longitudinal analysis of the CARDIA (coronary artery risk development in young adults) study. Am J Kidney Dis 63:590–597
Reis JP, Loria CM, Lewis CE et al (2013) Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA 310:280–288
Nyberg ST, Batty GD, Pentti J et al (2018) Obesity and loss of disease-free years owing to major non-communicable diseases: a multicohort study. Lancet Public Health 3:e490–e497. https://doi.org/10.1016/s2468-2667(18)30139-30147
Hursting SD, Digiovanni J, Dannenberg AJ et al (2012) Obesity, energy balance, and cancer: new opportunities for prevention. Cancer Prev Res 5:1260–1272
Feng Y, Spezia M, Huang S et al (2018) Breast cancer development and progression: risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis. Genes Dis 5:77–106
Lemmens VE, Oenema A, Klepp KI, Henriksen HB, Brug J (2008) A systematic review of the evidence regarding efficacy of obesity prevention interventions among adults. Obes Rev 9:446–455
World Cancer Research Fund/American Institute for Cancer Research. Diet, nutrition, physical activity and cancer: a global perspective. Continuous update project expert report 2018. http://dietandcancerreport.org/
Han W, Kim SW, Park IA et al (2004) Young age: an independent risk factor for disease-free survival in women with operable breast cancer. BMC Cancer 4:82
Luo J, Thomson C, Hendryx M et al (2018) Accuracy of self-reported weight in the Women’s Health Initiative. Public Health Nutr 19:1–10. https://doi.org/10.1017/s1368980018003002
Sawyer S, Azzopardi PS, Wickremarathne D et al (2018) The age of adolescence. Lancet Child Adolesc Health 2:223–228
Funding
Supported by grants from the Breast Cancer Research Foundation, National Cancer Institute Grants CA148791, CA047888 and NIH/NCATS Colorado CTSI Grant Number UL1 TR001082 at the University of Colorado Denver.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors have no disclosures to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Azrad, M., Blair, C.K., Rock, C.L. et al. Adult weight gain accelerates the onset of breast cancer. Breast Cancer Res Treat 176, 649–656 (2019). https://doi.org/10.1007/s10549-019-05268-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05268-y