Abstract
Introduction
Many eligible women with invasive breast cancer do not receive recommended adjuvant radiation (RT), despite its role in local control and overall survival. We examined trends in RT use over 10 years, and the impact of sociodemographic factors on the receipt of standard-of-care RT, using the National Cancer Database (NCDB).
Materials/methods
Women under age 70 with invasive breast cancer who underwent BCS from 2004 to 2014 were analyzed. Receipt of RT was evaluated in the whole cohort and by time period to identify temporal trends. Multiple logistic regression models were used to assess associations between factors such as race, insurance status, ethnicity, and receipt of RT.
Results
A total of 501,733 patients met eligibility criteria. The percentage of patients undergoing adjuvant RT increased from 86.7% in 2004 to 92.4% in 2012, and then decreased in 2013 and 2014 to 88.9%. On univariate analysis, patients of white race were significantly more likely to receive RT compared with patients of black race (90.4% vs 86.9%, p < 0.0001), as were non-Hispanic women compared to Hispanic patients (90.2% vs. 85.3%, p < 0.0001). On multivariate analysis, race, ethnicity, insurance status, education level, and age remained significantly associated with receipt of RT. On temporal analysis, gaps remained stable, with no significant improvements over time.
Conclusions
This analysis suggests a recent decline in guideline-concordant receipt of RT in women under 70, and persistent disparities in the use of RT after BCS by race, ethnicity, and socioeconomic factors. These findings raise concern for a recent detrimental change in patterns of care delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adjuvant radiation therapy (RT) after breast-conserving surgery (BCS) is a standard element of breast-conserving therapy for women with invasive breast cancer who are younger than 70 years of age, contributing to improvements both in locoregional control and overall survival [1, 2]. Historically, the standard for adjuvant radiation as a component of breast conservation applied to all women with invasive breast cancer, based on the landmark NSABP B06 study, which established the equivalence of breast conservation to the historical “gold standard” of mastectomy [3]. Over time, as the literature has culled out groups of patients at higher and lower risk of recurrence, there has been an increasing interest in research designed to identify low-risk subgroups in whom the benefit of radiation is small and a survival advantage is unlikely [4,5,6]. To this end, the Cancer and Leukemia Group (CALGB) 9343 study (first published in 2004 and subsequently updated with 10-year follow-up in 2013) demonstrated a relatively small reduction in local recurrence from 10 to 2% with the addition of radiation in women over 70 with stage T1N0, hormone-receptor-positive breast cancer who received endocrine therapy, with no improvement in metastasis-free survival or mastectomy-free survival. This study led to the adoption of RT omission as a guideline-concordant treatment option for women over 70 who meet the CALGB eligibility criteria [7]. While a great deal of ongoing work seeks to further expand this low-risk cohort, at this time no other population of women with invasive breast cancer who undergo breast-conserving surgery has been identified who can safely avoid RT outside the context of a research study [4, 8, 9].
Despite strong data and clear national guidelines supporting the use of adjuvant RT after BCS in women with invasive breast cancer < 70 years of age, it has been known for some time that many eligible women do not receive the recommended RT.4 Previous studies have demonstrated disparities in the appropriate receipt of adjuvant RT in certain demographic groups with overall rates of RT use varying from 65 to 95% [10, 11]. Factors identified as associated with inadequate receipt of RT have included race, ethnicity, age, and geographic location. In a recent analysis of the Surveillance, Epidemiology and End Results registry database (SEER) from 2004 to 2009, it was shown that African American women ages 40–85 were nearly 20% less likely to receive post-lumpectomy radiation [12]. In a similar analysis of the SEER database looking specifically at patients with locally advanced breast cancer requiring RT, both African Americans and Hispanics were significantly less likely than white females to receive appropriate RT [13]. These disparities in receipt of appropriate RT have been found to extend to patients of lower socioeconomic status as well [14]. Most concerning is the finding that these inadequacies in care translate to inferior outcomes and even survival in these groups [15, 16].
The National Cancer Database (NCDB) is an oncology database that is jointly sponsored by the American College of Surgeons and the American Cancer Society. It includes over 1500 accredited facilities and represents over 70% of newly diagnosed cancer cases in the U.S. nationwide. Data are available going back to 2004, and the NCDB is well suited to examine trends in the use of RT in this population, as it includes comprehensive details on radiation treatment course as well as socioeconomic characteristics such as race, income, and education. While disparities in the utilization of radiation are well established, temporal trends in both RT utilization after BCS and specifically in disparities have not been examined since the establishment of the NCDB. We sought to evaluate trends in patterns of RT use over a 10-year period, as well as the impact of race, ethnicity, and socioeconomic factors on the receipt of standard-of-care RT in women under 70 with invasive breast cancer who undergo breast-conserving surgery.
Materials/methods
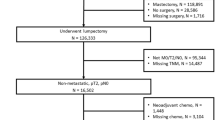
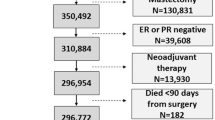
Using the NCDB, we identified women under age 70 who were diagnosed with invasive breast cancer and underwent BCS from 2004 to 2014. Any patient with stage IV disease or incomplete demographic data was excluded from the analysis, as were patients in whom radiation data were incomplete. We examined the rate of utilization of RT in this population over each year of the study period.
The association between patient characteristics and the receipt of radiation therapy over the entire time period was evaluated using univariate analysis, (χ2 tests for categorical variables). All the variables with a significance level of p < 0.05 in the univariate analysis were included in the logistic regression model to assess the multivariate relationship between patient characteristics and the probability of a woman receiving radiation therapy. Least absolute shrinkage and selection operator (LASSO) regression with cross-validation was performed. Lambda that gives minimum mean cross-validated errors was used to select variables in the final model.
Annual rates of radiation therapy use by facility type, facility location, age, insurance status, travel distance from the treatment facility, annual median income, race, ethnicity, proportion of population without high school diploma, and comorbidity were calculated, with adjustment of all other factors in the multivariate logistic model.
To evaluate change in effects of factors over time, multivariate logistic regression models on subset data were performed. Specifically, the multivariate logistic regression model was used on data from patients included in the study diagnosed only during the first and last years of the analysis, 2004 and 2014. We included interaction terms between each factor with year of diagnosis (e.g., 2004 vs 2014) to assess statistically significant differences in the effect of each factor between the 2 years. To verify downward trends observed, results were checked using various inclusion criteria. This included limiting the study cohort to only those with invasive ductal carcinoma, including patients with missing demographic data, as well as further stratifying patients by age for analysis. Additionally, the distribution of covariates was assessed between years to ensure comparability.
All analyses were performed in R 3.4.3 (glmnet package was used for cross-validation and emmeans package for comparing estimated marginal means).
Results
A total of 501,733 patients met inclusion criteria for this study. Table 1 shows the percent of patients who did or did not receive radiation by socioeconomic and demographic characteristics, and by year. The percentage of patients undergoing adjuvant RT increased from 86.7% in 2004 to a peak of 92.4% in 2012, and then decreased in 2013 and 2014 to 88.9%.
On univariate analysis taking into account the full time period, patients of white race were significantly more likely to receive RT compared with patients of black race (90.4% vs 86.9%, p < 0.0001). This difference was also seen between those of non-Hispanic and Hispanic ethnicity (90.2% vs. 85.3%, p < 0.0001). Both insurance status and median income were significantly associated with receipt of RT: patients with private insurance were most likely to undergo RT (90.9%) compared to patients with Medicare (88.3%), Medicaid (86.8%), and those without insurance (84.7%) (p < 0.0001). Those in the highest income group of $63,000 or more had the highest rates of RT at 90.6%, compared with the lowest rates (87.9%) in those making less than $38,000 per year (87.9%) (p < 0.0001) (Table 1).
Differences were also observed based on treating facility characteristics. The rate of RT utilization decreased with increasing distance from treatment facility, with those living more than 27.8 miles from treating facility being least likely to receive RT (p < 0.0001). The highest rates of RT were seen at integrated network cancer programs (INCP) (90.6%) and the lowest rates in community cancer programs (CCP) (88%). Patients living in the South had the lowest RT rates (85.9%), while the highest rates were seen among those patients living in the North (93%) (p < 0.0001). Patients were also analyzed by Charlson Comorbidity Score (CDCC), with 0 indicating no comorbid conditions, and 2 indicating two or more comorbidities (such as myocardial infarction, diabetes, and renal disease). Those patients with CDCC of 0 were most likely to receive radiation (90.2%) compared to those with CDCC of 2 or more, of whom only 85.9% received necessary RT (p < 0.0001).
On multivariate analysis, race, ethnicity, insurance status, education level, CDCC, and age remained significantly associated with receipt of RT (Table 1, far right column). For facility characteristics, distance from treating facility, geographic location, and facility type remained significant as well.
We also evaluated trends over time in receipt of radiation, specifically comparing the first and last year from available data (Table 2; Fig. 1). Overall rates of radiation receipt increased steadily between 2004 and 2012 when it peaked at 92.4%. A decline in overall rates was then seen from 2013 to 2014 when rate was 88.9%. As seen in Fig. 1, this trend was observed across all subgroups analyzed, and was not isolated to any specific patient characteristic.
Also notable was that gaps remained stable over time despite the overall trends seen before and after 2012. This is highlighted with both race and insurance status. In Fig. 1e, it is seen that the largest disparity in receipt of radiation by race is between black and white patients, and this was seen across all time points. Although OR for radiation receipt increased from 0.67 (2004) to 0.74 (2014), interaction term remained non-significant (Table 2) suggesting no meaningful improvements over time.
Similarly, as seen in Fig. 1b, those patients with private insurance consistently received RT at the highest rates, with the greatest gap between those with private insurance vs those uninsured. These trends were also seen when analyzed by facility location, with those patients diagnosed in the South consistently exhibiting the lowest rates of radiation receipt over time (Fig. 1a). When considering distance to treatment facility, however, there was a significant narrowing of differences seen for those patients living > 27.8 miles, as seen by the narrowing of curves in Fig. 1c between 2004 and 2014. Specifically, compared to those living > 27.8 miles from treatment facility, there was a narrowing in the difference in receipt of treatment compared to those living within 6.3 miles (odds ratio [OR] 1.65; 95% CI 1.5–1.81 in 2004 vs 1.29; 1.19–1.4 in 2014). Figure 1f demonstrates that the decrease in rates of RT use in recent years was seen in both younger and older women.
Discussion
Our analysis demonstrates persistent disparities in appropriate receipt of adjuvant RT after lumpectomy that spans socioeconomic, ethnic, and racial groups and appears persistent over the last decade. In addition, the rate of utilization of RT in this population has a consistent pattern of increase from 2004 to 2012 (86.7–92.4%) followed by a decrease from 2012 to 2014 (92.4–88.9%), which is not readily explained.
The literature and guidelines supporting the use of RT in the population we have analyzed are clear [3, 4, 17]. A great deal of work is ongoing to identify patients at a particularly low risk of recurrence, including those under 70 years of age with low-risk features, from the perspective that tumor biology, rather than age, is the most important determinant of risk. Current studies are evaluating the omission of RT in younger post-menopausal women, using markers of tumor biology such as the 21-gene recurrence score (Individualized Decisions for Endocrine Therapy Alone, IDEA) and the Prediction Analysis of Microarray-50, or PAM-50 (Profiling Early Breast Cancer for Radiotherapy Omission, PRECISION) [8, 9]. The PRIME II study, which closely mirrors the CALGB study but includes women 65 and over, published 5-year follow-up in 2015, and similarly to CALGB shows a very small reduction in the risk of local recurrence with the addition of RT [5, 6]. Based on PRIME II, some practices may have adopted age 65 as a reasonable cut-off for RT omission, though based on the short follow-up, NCCN guidelines still reflect an age of 70 or older as appropriate for RT omission. Importantly, in 2014, the last year of our analysis, PRIME II had not been published, and the IDEA and PRECISION studies were not yet open. Thus, while there is a growing interest in RT omission in younger patients, during the time period we studied, there were no published data and no national studies to explain the decrease in RT use from 2012 to 2014. In addition, the decrease in RT utilization was seen in all age groups under 70, as shown in Fig. 1f and Table 2.
In addition to age, another possible cause for the observed reduction in RT utilization could be in the increased attention given to secondary risks of radiation, including the risk of ischemic heart disease that garnered increased attention after the publication of the paper by Darby et al. [18]. This study linked increased rates of major coronary events to radiation dose to the heart, with events starting within 5 years of treatment. Again, the timing of this publication does not fully explain the observed findings.
Since the observed decline is not explained by changes in literature or guidelines during this period, we ran additional analyses to ensure that this was not reflective of an error in our study method. Our analysis was repeated on a broader cohort of patients inclusive of those with missing demographic data, to ascertain whether omission of these patients translated to a systematic underrepresentation of certain patients. The same trend, with decline in rates of RT after 2012, was observed. This same downward trend in RT rates was also seen in each individual cohort when analyzed by racial and socioeconomic group as well as all age groups, suggesting a more systemic cause for omission.
Albeit unexplained, this downward trend across all groups is a concerning finding in our study that warrants close attention in coming years to establish if there is persistent decline. During the period of analysis, the use of adjuvant RT in breast-conserving therapy represents a standard in women included in the study, and omission of RT in this population thus represents a deviation from optimal breast cancer management.
Our analysis also identifies significant disparities in RT receipt based on multiple socioeconomic and demographic factors including treating facility type, distance to facility, race, ethnicity, and education level. Most concerning, perhaps, is that little improvement in these gaps was observed over a 10-year period. These findings have been reported in previous studies as well, noted at both the state and national level. In another large database analysis, Yeboa et al. performed a SEER analysis of disparities in the receipt of RT in Stage I breast cancer from 2004 to 2009. Similar to our results, not only were African American women significantly less likely than white women to receive adjuvant RT, but disparities persisted across the 6-year study period [12]. Although the authors comment that perhaps the economic recession at the time could contribute to persistent disparities through 2009, our results continue to reflect their findings over 5 years later. Data also exist to suggest that these gaps in breast cancer care stretch beyond receipt of radiation alone. In a study by Dosch et al. of minority populations in Florida, both black and Hispanic patients were more likely to present with regional and distant disease than localized disease at the time of diagnosis compared to white women, as were women of lower socioeconomic status [19]. In another analysis of the NCDB, black (vs. white) women were less likely to receive definitive locoregional therapy, hormonal therapy, as well as chemotherapy [20].
The reasons for the above-mentioned gaps in breast cancer care between groups is likely multifactorial. As seen in our multivariate analysis, distance from treating facility was an independent predictor of receipt of radiation and highlights the basic lack of access to care as an impediment to optimal cancer treatment. Other studies have also demonstrated that minority groups such as African Americans are more likely to rely on public transportation to reach RT facilities, taking 7 times longer than private transportation thus representing a significant barrier [21]. Our results also demonstrated that those patients with higher CDCC and thus more medical comorbidities were less likely to receive RT. This may represent both a reluctance on the part of some providers to offer RT to those with many competing medical issues, or also reflect the difficulty experienced by patients in making daily RT appointments if quality of life is already effected by other active comorbidities.
It should be noted that our analysis has several limitations. We analyzed receipt of RT after BCS as reported in the NCDB; to be captured in the database, patients must be treated at a Commission on Cancer (CoC) accredited hospital. While this includes approximately 70% of newly diagnosed cancer cases each year, this represents only 30% of US hospitals. Thus, it is possible that there is systematic underrepresentation of certain populations in this study cohort, true of any analysis done using the NCDB. In addition, this analysis should be repeated in other cancer databases as this is the first analysis we are aware of to show a decline in RT utilization in recent years.
This analysis identifies a concerning downtrend in appropriate use of RT after breast conservation surgery in women under age 70 across all groups, and highlights persistent disparities in receipt of RT among certain racial, ethnic, and socioeconomic groups. These findings are concerning for shifting patterns of care that stray from current accepted guidelines. Further research into causes of this observation, as well as additional analyses of other large cancer databases, are warranted.
References
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Darby S, McGale P et al (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378(9804):1707–1716
Clarke M, Collins R, Darby S et al (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366(9503):2087–2106
Fisher B, Anderson S, Bryant J et al (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347(16):1233–1241
Fyles AW, McCready DR, Manchul LA et al (2004) Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast cancer. N Engl J Med 351(10):963–970
Hughes KS, Schnaper LA, Bellon JR et al (2013) Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J Clin Oncol 31(19):2382–2387
Kunkler IH, Williams LJ, Jack WJ, Cameron DA, Dixon JM (2015) PRIME II investigators. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. Lancet Oncol 16(3):266–273
National comprehensive cancer network breast cancer. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
The IDEA Study (Individualized Decisions for Endocrine Therapy Alone) (2015) Retrieved from https://Clinicaltrials.gov/ct2 (identification no. NCT02400190)
The PRECISION Trial (Profiling Early Breast Cancer for Radiotherapy Omission). (2016). A phase II study of breast-conserving surgery without adjuvant radiotherapy for favorable-risk breast cancer. Retrieved from https://Clinicaltrials.gov/ct2 (identification no. NCT02653755)
Du Xianglin L, Gor BJ (2007) Racial disparities and trends in radiation therapy after breast-conserving surgery for early-stage breast cancer in women, 1992 to 2002. Ethn Dis 17(1):122–128
Jagsi R, Abrahamse P, Morrow M et al (2010) Patterns and correlates of adjuvant radiotherapy receipt after lumpectomy and after mastectomy for breast cancer. J Clin Oncol 28(14):2396–2403
Yeboa DN, Xu X, Jones BA, Soulos P, Gross C, Yu JB (2016) Trend in age and racial disparities in the receipt of postlumpectomy radiation therapy for stage I breast cancer: 2004–2009. Am J Clin Oncol 39(6):568–574
Martinez SR, Tseng WH, Shah DR, Canter RJ, Bold RJ (2012) Urban and non-urban disparities in the use of post-mastectomy radiation for breast cancer. Med Oncol 29(3):1523–1528
Parise CA, Bauer KR, Caggiano V (2012) Disparities in receipt of adjuvant radiation therapy after breast-conserving surgery among the cancer-reporting regions of california. Cancer 118(9):2516–2524
Dragun AE, Huang B, Tucker TC, Spanos WJ (2011) Disparities in the application of adjuvant radiotherapy after breast-conserving surgery for early stage breast cancer: impact on overall survival. Cancer 117(12):2590–2598
McClelland S 3rd, Page BR, Jaboin JJ, Chapman CH, Deville C Jr, Thomas CR (2017) Jr. The pervasive crisis of diminishing radiation therapy access for vulnerable populations in the united states, part 1: African-american patients. Adv Radiat Oncol 2(4):523–531
National Comprehensive Cancer Network Breast Cancer (2018) https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 4 Jan 2018.
Darby SC, Ewertz M, Hall P (2013) Ischemic heart disease after breast cancer radiotherapy. N Engl J Med 368(26):2527
Dosch AR, Koru-Sengul T, Miao F, Tannenbaum SL, Byrne MM, Wright JL (2014) Racial and ethnic disparities in the diagnosis of breast cancer: changes in presenting stage in minority populations in florida during 1981–2009. Breast Cancer Res Treat 148(2):379–387
Freedman RA, Virgo KS, He Y et al (2011) The association of race/ethnicity, insurance status, and socioeconomic factors with breast cancer care. Cancer 117(1):180–189
Peipins LA, Graham S, Young R, Lewis B, Flanagan B (2013) Racial disparities in travel time to radiotherapy facilities in the atlanta metropolitan area. Soc Sci Med 89:32–38
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Parekh, A., Fu, W., Hu, C. et al. Impact of race, ethnicity, and socioeconomic factors on receipt of radiation after breast conservation surgery: analysis of the national cancer database. Breast Cancer Res Treat 172, 201–208 (2018). https://doi.org/10.1007/s10549-018-4881-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4881-0