Abstract
Purpose
Approximately 25% of breast cancer patients experience treatment delays or discontinuation due to paclitaxel-induced peripheral neuropathy (PN). Currently, there are no predictive biomarkers of PN. Pharmacometabolomics is an informative tool for biomarker discovery of drug toxicity. We conducted a secondary whole blood pharmacometabolomics analysis to assess the association between pretreatment metabolome, early treatment-induced metabolic changes, and the development of PN.
Methods
Whole blood samples were collected pre-treatment (BL), just before the end of the first paclitaxel infusion (EOI), and 24 h after the first infusion (24H) from sixty patients with breast cancer receiving (80 mg/m2) weekly treatment. Neuropathy was assessed at BL and prior to each infusion using the sensory subscale (CIPN8) of the EORTC CIPN20 questionnaire. Blood metabolites were quantified from 1-D-1H-nuclear magnetic resonance spectra using Chenomx® software. Metabolite concentrations were normalized in preparation for Pearson correlation and one-way repeated measures ANOVA with multiple comparisons corrected by false discovery rate (FDR).
Results
Pretreatment histidine, phenylalanine, and threonine concentrations were inversely associated with maximum change in CIPN8 (ΔCIPN8) (p < 0.02; FDR ≤ 25%). Paclitaxel caused a significant change in concentrations of 2-hydroxybutyrate, 3-hydroxybutyrate, pyruvate, o-acetylcarnitine, and several amino acids from BL to EOI and/or 24H (p < 0.05; FDR ≤ 25%), although these changes were not associated with ΔCIPN8.
Conclusions
Whole blood metabolomics is a feasible approach to identify potential biomarker candidates of paclitaxel-induced PN. The findings suggest that pretreatment concentrations of histidine, phenylalanine, and threonine may be predictive of the severity of future PN and paclitaxel-induced metabolic changes may be related to disruption of energy homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paclitaxel is routinely used for breast cancer treatment; however, approximately 25% of patients experience treatment delays or discontinuation due to the development and progression of paclitaxel-induced peripheral neuropathy (PN) [1]. Paclitaxel-induced PN substantially diminishes patients’ quality of life, and up to 80% of affected patients still experience symptoms of neuropathy up to 2 years after treatment discontinuation [2]. Currently, there is no effective strategy to prevent or treat paclitaxel-induced PN, partially due to a lack of a clear definition of PN phenotype and understanding of its underlying pathophysiology [3, 4]. As a result, clinicians do not have reliable tools to predict PN prior to symptoms becoming clinically apparent. This has created a significant unmet need to discover predictive biomarkers of paclitaxel-induced PN that clinicians can use proactively to identify patients at risk of developing severe PN [5], which may also permit the tailoring of paclitaxel dosing regimens to maximize efficacy and minimize toxicity [6].
Previous clinical studies have evaluated the role of antioxidants, amino acids, and vitamins in prevention and/or treatment of chemotherapy-induced PN (acetyl-l-carnitine [7, 8]; glutathione [9,10,11]; glutamine [12,13,14]; multivitamin [15]). There is also evidence suggesting that alcohol-induced neuropathy may be related to low vitamin and nutrient levels [16]. Together, these studies imply that PN may result from a complex, multifactorial interaction of small molecules related to vitamin and amino acid metabolism. As such, it is plausible that there is a metabolic basis for the risk of paclitaxel-induced PN, which could be revealed by metabolomics profiling. Metabolomics simultaneously identifies small molecules in a single biological sample. It captures signals from multiple factors (e.g., genetic, environment, microbiome) in aggregate. Pharmacometabolomics, the clinical application of metabolomics, utilizes unbiased profiling to identify metabolic features prior to and during treatment that are related to treatment outcomes [17]. Proof-of-concept studies have demonstrated the potential of pharmacometabolomics to enhance understanding and/or prediction of chemotherapy-induced toxicities [18,19,20].
Given this scientific rationale and the need to discover predictive biomarkers of paclitaxel-induced PN, we conducted a secondary, proof-of-concept, pharmacometabolomics analysis using whole blood samples collected prior to paclitaxel treatment and after the first treatment dose from patients enrolled on an observational clinical registry (NCT02338115) to identify metabolic profiles associated with the future development of PN.
Methods
Selection and description of participants
The detailed study design and enrolled patients have been previously described [21]. Briefly, sixty female adult patients (> 18 years old) with the diagnosis of stage I–III or oligometastatic breast cancer planning to receive paclitaxel 80 mg/m2 1-h infusions weekly for 12 weeks were prospectively enrolled to an observational clinical registry (NCT02338115). The secondary analysis was approved by the University of Michigan IRBMed (HUM 00086253) and signed informed consent was obtained from each participant. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Neuropathy assessment
PN was assessed at pre-treatment (BL), just before the end of the first paclitaxel infusion (EOI), 24 h after the first infusion (24H), and prior to each of the subsequent paclitaxel infusion using paper copies of the validated European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Chemotherapy-Induced Peripheral Neuropathy (CIPN20). The CIPN20 is a patient-reported outcome (PRO) questionnaire that includes 20 questions about symptoms of sensory, motor, and autonomic neuropathy [22]. Items are scored from 1 to 4 with 1 representing “not at all” and 4 representing “very much.” The treating clinicians did not have access to the CIPN20 data at any point during treatment. Paclitaxel is known to cause a primarily sensory neuropathy; therefore, the primary endpoint for this analysis was the 8-item sensory subscale (CIPN8) that quantifies numbness, tingling, and burning/shooting pain in the upper and lower extremities, difficulty walking due to diminished plantar sensation, and temperature sensation [23]. CIPN8 scores were linearly converted to a 0–100 scale with higher scores implying worse neuropathy [24].
Whole blood 1-D-1H-NMR metabolomics
Whole blood sample collection and processing
Whole blood (WB) samples were collected at BL, EOI, and 24H into Vacutainer® tubes containing sodium heparin as previously described [25]. Following collection, the tubes were placed in an ice water bath and 600 µL of WB was aliquoted into cryovials and promptly stored at (− 80 °C). Following the completion of the study, cryovials were transferred to liquid nitrogen for long-term storage.
1-D-1H-NMR workflow
Prior to assay, samples were randomly assigned into batches to avoid potential batch effects. At the time of assay, the samples were thawed in an ice water bath and subjected to a 1:1:1 sample/methanol/chloroform precipitation to remove macromolecules [26]. The resulting upper aqueous methanol layers of each sample were dried by lyophilization (Labconco #7382021 at − 105 °C and 0.014mBar) and resuspended in 50 mM sodium phosphate buffer in D2O (500 µL) with DSS-d6 internal standard Chenomx IS-2 (Chenomx Inc., Edmonton, Alberta, Canada; chenomx.com) of known concentration. The 1-D-1H-NMR spectrum of each WB sample was acquired at the University of Michigan’s Biochemical NMR Core Laboratory on a Varian (now Agilent, Inc., Santa Clara, CA) 11.74 T (500 MHz) NMR spectrometer with a VNMRS console operated by host software VNMRJ4.0 and equipped with a 5-mm Agilent “One Probe” [27]. The resulting NMR spectra were analyzed using Chenomx NMR Suite 8.3 (Chenomx, Inc.) [28]. Spectral processing, compound identification, and quantification of metabolites were completed and reconciled by three users who were blinded to the samples’ identities.
Data and statistical analysis
WB samples from six out of the sixty patients were selected for initial methodology optimization and were excluded from this analysis. Of the remaining fifty-four patients, forty-eight were included in this secondary pharmacometabolomics analysis based on the availability and the quality of the acquired NMR spectra.
Pretreatment metabolome association with PN
The entire pretreatment NMR metabolite dataset (µM) was log transformed and mean centered to achieve a normal distribution using MetaboAnalyst 3.0 (http://www.metaboanalyst.ca) [29]. Pearson correlation was performed to examine the association between each pretreatment normalized metabolite concentration value and maximum change in CIPN8 (ΔCIPN8). ΔCIPN8 was calculated as the difference between the highest value of CIPN8 score during treatment and the baseline. Each resulting p value was corrected for multiple comparisons by calculating the false discovery rate (FDR) using the method of Storey [30]. WB metabolites were ranked by ascending FDR and those with an FDR ≤ 25% were considered as potentially discriminating [31] and were used in the subsequent bioinformatics analysis.
Treatment-induced metabolic changes and their association with PN
The combined pretreatment and first cycle treatment NMR metabolite dataset (µM) was cube root transformed and auto scaled to achieve a normal distribution using MetaboAnalyst 3.0 (http://www.metaboanalyst.ca) [29]. The normalized BL value of each metabolite was compared to that at EOI and 24H using a one-way repeated measures ANOVA followed by the Dunnett’s multiple comparison test [32]. Each resulting p value was FDR corrected; those with an FDR ≤ 25% were used in the subsequent bioinformatics analysis. A heatmap of median fold-change was generated to visualize the magnitude of changes in metabolite concentrations. To assess the association between the metabolic change from BL to EOI and ΔCIPN8, Pearson correlation was performed as described above. Statistical analyses were performed, and figures were generated using Prism 7® (GraphPad software), R Studio (version 1.1.423) with ggplot2 package and PathVisio (version 3.3.0) (https://www.pathvisio.org).
Bioinformatics analysis
To assess the metabolic relationship between the metabolites that may be important in the development of PN, WB metabolites with associated Kyoto Encyclopedia of Genes and Genomes (KEGG) ID and FDR ≤ 25% were used to generate compound–gene–reaction networks in MetScape, a plugin for Cytoscape (http://www.cytoscape.org/). MetScape is a free online bioinformatics tool for visualizing and interpreting metabolomics data in the context of human metabolic networks [33].
Results
Patient demographics
Metabolomics data were acquired from 48 patients enrolled in the clinical study (Supplemental Fig. 1). Table 1 shows the demographic and clinical characteristics of these patients. Prior to treatment, the mean (± SD) CIPN8 was 0.87 (± 2.57). The mean value (± SD) of the maximum CIPN8 scores, reported by all patients during 12 weeks of treatment, was 26.91 (± 22.36).
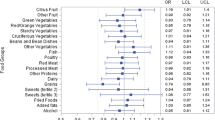
Pretreatment metabolome association with PN
Thirty-four metabolites were identified and quantified in all samples. The entire data set can be found at http://www.metabolomicsworkbench.org/. Pretreatment histidine, phenylalanine, and threonine concentrations were inversely correlated with ΔCIPN8 (p < 0.02; FDR ≤ 25%) (Fig. 1) (Supplemental Table 1). A MetScape-generated network shows the metabolic relatedness between histidine, phenylalanine, and threonine (Fig. 2).
Pretreatment metabolite concentrations are informative of the development of paclitaxel-induced peripheral neuropathy (PN). Pretreatment concentrations of a histidine, b phenylalanine, and c threonine are inversely correlated with the maximum change in CIPN8 score by Pearson correlation (p < 0.02; FDR ≤ 25%). The Pearson correlation coefficient (r), r2, p value, and FDR for each metabolite are shown in each panel (a–c). The blue line represents the fitted line and gray shade represents the 95% confidence interval
Metabolic networks of histidine, phenylalanine, and threonine generated by MetScape. Networks illustrate the relationship between uploaded metabolites (input, dark red hexagons): histidine (KEGG ID C00135), phenylalanine (KEGG ID C00079), and threonine (KEGG ID C00188). a Both phenylalanine and histidine undergo decarboxylation reactions (R00699 and R01167, respectively), catalyzed by aromatic-l-amino-acid decarboxylase encoded by the DDC gene, to form phenylethylamine and histamine, respectively (yellow shading). b The threonine network is distinct and its primary reaction (R00751) is catalyzed by threonine aldolase to form glycine (blue shading); glycine was not found to be a differentiating metabolite of the development of PN (p = 0.67; FDR = 99.3%). Pink hexagons represent metabolites, green squares represent enzymes, blue circle represent genes, and gray diamond represent reactions
Treatment-induced metabolic changes and their association with PN
Paclitaxel induced statistically significant changes in concentrations of 14 metabolites from BL to EOI, from BL to 24H, or both (FDR ≤ 25%) (Fig. 3). The metabolites 3-hydroxybutyrate and 2-hydroxybutyrate (Fig. 3a, b) increased from BL to EOI and then declined from BL to 24H. Pyruvate, alanine, and threonine (Fig. 3c–e) initially decreased from BL to EOI, but were higher than BL at 24H. Phenylalanine, tyrosine, asparagine, lysine, o-acetylcarnitine, proline, lactate, glutamine, and leucine (Fig. 3f–n) did not change from BL to EOI, but increased from BL to 24H. p values and FDR of each metabolite (BL vs. EOI and BL vs. 24H) are listed in Supplemental Table 2. There was no statistically significant association between the change in concentration of any metabolite from BL to EOI and ΔCIPN8 (data not shown).
Impact of the first dose of paclitaxel on individual metabolite concentrations at the end of infusion (EOI) and after 24 h (24H). The concentrations of 14 metabolites, a 3-hydroxybutyrate, b 2-hydroxybutyrate, c pyruvate, d alanine, e threonine, f phenylalanine, g tyrosine, h asparagine, i lysine, j o-acetylcarnitine, k proline, l lactate, m glutamine, and n leucine changed significantly from BL to EOI, from BL to 24H, or both (FDR ≤ 25%). Data are represented by individual concentration measurements in a box and whisker plot in which the box represents interquartile. None of the metabolic changes from BL to EOI is significantly correlated with maximum change in CIPN8 score by Pearson correlation corrected by FDR (FDR ≤ 25%). KEGG IDs of metabolites can be found in Supplemental Table 3
A heatmap of the median fold-change (Fig. 4a) shows the magnitude of concentration changes of all metabolites. A MetScape network revealed that paclitaxel impacts multiple pathways (Supplemental Table 3). The primary metabolic pathways that incorporate the differentiating metabolites are glycolysis and the tricarboxylic acid (TCA) cycle; these are depicted in Fig. 4b, c.
First dose of paclitaxel disrupts energy homeostasis. A heatmap a scaled by median fold-change of each metabolite concentration from BL to EOI (first column) and from BL to 24H (second column). Red represents the increase in concentration (fold-change > 1) and blue represents the decrease in concentration (fold-change < 1) from BL. The metabolic pattern at EOI and 24H is illustrated in a biological context through MetScape mapping. Metabolites with FDR ≤ 25% are uploaded into MetScape and the resulting metabolic networks represented by these metabolites were simplified in panel (b) and panel (c). The primary metabolic pathways disrupted by first-dose paclitaxel are glycolysis and tricarboxylic acid cycle (TCA). In both panels, the concentrations of metabolites in red are increased and those in blue are decreased. In aggregate, these findings suggest that there is a series of sequential energy metabolic responses induced by paclitaxel
Discussion
Paclitaxel-induced PN is a debilitating toxicity that substantially affects patient’s quality of life. To the best of our knowledge, this is the first pharmacometabolomics study of paclitaxel-induced PN, and it demonstrates that whole blood metabolomics is a viable approach for PN biomarker discovery. Furthermore, we employed a PRO tool to assess patients’ PN symptoms, which has been shown to be more reliable compared to clinician-graded NCI CTCAE [34,35,36]. This innovative analytic approach in conjunction with PRO data provides new insights into the understanding and prediction of paclitaxel-induced PN. Specifically, they implicate an inverse correlation between pretreatment histidine, phenylalanine, and threonine concentrations and ΔCIPN8, suggesting that the initial concentrations of these three metabolites may have predictive value for the severity of future PN. In addition, the early-treatment results suggest that paclitaxel-induced metabolic changes may be related to the disruption of energy homeostasis, in particular glycolysis and the TCA cycle. However, early metabolic changes induced by paclitaxel treatment do not appear to be informative of the severity of future PN.
Importantly, our findings have plausible neurobiological explanations. Histidine is an essential amino acid and a precursor of histamine, a neuromodulator implicated in the pathogenesis and inflammatory process of neuropathic pain [37,38,39]. Phenylalanine is also an essential amino acid and a precursor of phenylethylamine and dopamine, both of which are neuromodulators implicated in the pathogenesis of certain psychiatric and neurological diseases [40, 41]. Interestingly, phenylalanine is metabolically related to glutamine, which has been evaluated as a neuroprotective agent, but our findings do not suggest any association between glutamine and PN (Supplemental Table 1). Threonine, another essential amino acid, has not been shown to directly play a role in PN; however, elevated plasma threonine concentration can lead to the accumulation of glycine in the brain which has been shown to affect neurotransmitter balance during early postnatal life [42].
Although our analysis did not show that paclitaxel-induced changes in metabolite concentrations were associated with the future development of PN, the elevation in 2-and 3-hydroxybutyrate concentrations concurrent with lower pyruvate, alanine, and threonine concentrations at EOI (Fig. 4b) are suggestive of mitochondrial dysfunction and/or oxidative stress [43]. In animal tissue studies, paclitaxel induces mitochondrial structural changes due to inflammation [44,45,46] and causes mitochondrial dysfunction manifested as a persistent energy deficiency [47]. Both features were related to painful PN in these studies. Collectively, the distinct metabolic pattern at EOI (Fig. 4b) and 24H (Fig. 4c) provides some evidence for a series of sequential metabolic responses important in energy homeostasis.
The clinical implications of our findings could lead to improvement in paclitaxel-induced PN prevention. Genomics- [48,49,50] and proteomics-based PN [51] studies have not yielded clinically useful biomarkers, but the trend of utilizing systems biology to better understand and predict PN has gained traction. Our preliminary results support continued work in the pharmacometabolomics field that will require further testing and validation using existing blood samples from completed clinical trials [52] as well as prospective verification in future clinical trials to accurately define metabolite concentration thresholds associated with the development of PN. By identifying the subset of patients at risk for PN, more frequent PN monitoring can be implemented and paclitaxel dosing regimens can be tailored to maximize efficacy and minimize toxicity [6, 25]. In addition, the metabolite concentration thresholds can be used to identify patients susceptible to PN for enrollment in clinical studies evaluating novel techniques or agents for PN prevention and treatment.
Although our results are provocative, there are a few limitations that warrant consideration. First, this is a feasibility study with a small sample size. We elected to use a liberal FDR of 25% to identify differentiating metabolites and capture important metabolic patterns that may be associated with the development of PN. This liberal FDR cut-off has been used in a previous proteomics study [51]. Second, NMR metabolomics only captures a small fraction of the entire metabolome. Given the inconclusive findings of previous clinical PN prevention and treatment studies about the role of certain antioxidants, vitamins, and amino acids [7,8,9,10,11,12,13,14,15], and the preliminary nature of our study, we selected to employ quantitative NMR platform because of its advantages of reproducibility, quick turn-around time, and its utility for WB metabolomics [53]. Lastly, dietary and supplement information was not collected from enrolled patients. The range of pretreatment histidine, phenylalanine, and threonine concentrations was broad. Since these differentiating metabolites are essential amino acids, we could not rule out the possibility that differences in diet may contribute to our findings.
In conclusion, this study demonstrates the feasibility of whole blood metabolomics, together with PRO data, to discover potential clinical biomarker of paclitaxel-induced PN. Pretreatment histidine, phenylalanine, and threonine concentrations may have predictive value for the severity of treatment-emergent PN. Confirmatory studies are needed to validate these candidate biomarkers and extend the scope of our findings by employing a more detailed metabolomics approach [e.g., liquid chromatography (LC)–mass spectroscopy (MS)] [54, 55]. We envision that a predictive model, incorporating the PN biomarkers from metabolomics validation studies, could be transformed into a decision-making algorithm that can help tailor PN monitoring and/or guide paclitaxel dosing to enhance efficacy and prevent unnecessary PN in patients with breast cancer.
References
Speck RM, Sammel MD, Farrar JT, Hennessy S, Mao JJ, Stineman MG, DeMichele A (2013) Impact of chemotherapy-induced peripheral neuropathy on treatment delivery in nonmetastatic breast cancer. J Oncol Pract 9:e234–e240. https://doi.org/10.1200/JOP.2012.000863
Hershman DL, Weimer LH, Wang A, Kranwinkel G, Brafman L, Fuentes D, Awad D, Crew KD (2011) Association between patient reported outcomes and quantitative sensory tests for measuring long-term neurotoxicity in breast cancer survivors treated with adjuvant paclitaxel chemotherapy. Breast Cancer Res Treat 125:767–774. https://doi.org/10.1007/s10549-010-1278-0
Han Y, Smith MT (2013) Pathobiology of cancer chemotherapy-induced peripheral neuropathy (CIPN). Front Pharmacol 4 DEC:1–16. https://doi.org/10.3389/fphar.2013.00156
Hershman DL, Lacchetti C, Dworkin RH, Lavoie Smith EM, Bleeker J, Cavaletti G, Chauhan C, Gavin P, Lavino A, Lustberg MB, Paice J, Schneider B, Smith M, Lou Smith T, Terstriep S, Wagner-Johnston N, Bak K, Loprinzi CL (2014) Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American society of clinical oncology clinical practice guideline. J Clin Oncol 32:1941–1967. https://doi.org/10.1200/JCO.2013.54.0914
Travis LB, Fossa SD, Sesso HD, Frisina RD, Herrmann DN, Beard CJ, Feldman DR, Pagliaro LC, Miller RC, Vaughn DJ, Einhorn LH, Cox NJ, Dolan ME (2014) Chemotherapy-induced peripheral neurotoxicity and ototoxicity: new paradigms for translational genomics. J Natl Cancer Inst https://doi.org/10.1093/jnci/dju044
Joerger M, von Pawel J, Kraff S, Fischer JR, Eberhardt W, Gauler TC, Mueller L, Reinmuth N, Reck M, Kimmich M, Mayer F, Kopp HG, Behringer DM, Ko YD, Hilger RA, Roessler M, Kloft C, Henrich A, Moritz B, Miller MC, Salamone SJ, Jaehde U (2016) Open-label, randomized study of individualized, pharmacokinetically (PK)-guided dosing of paclitaxel combined with carboplatin or cisplatin in patients with advanced non-small-cell lung cancer (NSCLC). Ann Oncol 27:1895–1902. https://doi.org/10.1093/annonc/mdw290
Bianchi G, Vitali G, Caraceni A, Ravaglia S, Capri G, Cundari S, Zanna C, Gianni L (2005) Symptomatic and neurophysiological responses of paclitaxel- or cisplatin-induced neuropathy to oral acetyl-l-carnitine. Eur J Cancer 41:1746–1750. https://doi.org/10.1016/j.ejca.2005.04.028
Hershman DL, Unger JM, Crew KD, Minasian LM, Awad D, Moinpour CM, Hansen L, Lew DL, Greenlee H, Fehrenbacher L, Wade JL, Wong SF, Hortobagyi GN, Meyskens FL, Albain KS (2013) Randomized double-blind placebo-controlled trial of acetyl-l-carnitine for the prevention of taxane-induced neuropathy in women undergoing adjuvant breast cancer therapy. J Clin Oncol 31:2627–2633. https://doi.org/10.1200/JCO.2012.44.8738
Smyth JF, Bowman A, Perren T, Wilkinson P, Prescott RJ, Quinn KJ, Tedeschi M (1997) Glutathione reduces the toxicity and improves quality of life of women diagnosed with ovarian cancer treated with cisplatin: results of a double-blind, randomised trial. Ann Oncol 8:569–573
Colombo N, Bini S, Miceli D, Bogliun G, Marzorati L, Cavaletti G, Parmigiani F, Venturino P, Tedeschi M, Frattola L, Buratti C, Mangioni C (1995) Weekly cisplatin ± glutathione in relapsed ovarian carcinoma. Int J Gynecol Cancer 5:81–86. https://doi.org/10.1046/j.1525-1438.1995.05020081.x
Cascinu S, Catalano V, Cordella L, Labianca R, Giordani P, Baldelli AM, Beretta GD, Ubiali E, Catalano G (2002) neuroprotective effect of reduced glutathione on oxaliplatin-based chemotherapy in advanced colorectal cancer: a randomized, double-blind, placebo-controlled trial. J Clin Oncol 20:3478–3483. https://doi.org/10.1200/JCO.2002.07.061
Wang W-S, Lin J-K, Lin T-C, Chen W-S, Jiang J-K, Wang H-S, Chiou T-J, Liu J-H, Yen C-C, Chen P-M (2007) Oral glutamine is effective for preventing oxaliplatin-induced neuropathy in colorectal cancer patients. Oncologist 12:312–319. https://doi.org/10.1634/theoncologist.12-3-312
Vahdat L, Papadopoulos K, Lange D, Leuin S, Kaufman E, Donovan D, Frederick D, Bagiella E, Tiersten A, Nichols G, Garrett T, Savage D, Antman K, Hesdorffer CS, Balmaceda C (2001) Reduction of paclitaxel-induced peripheral neuropathy with glutamine. Clin Cancer Res 7:1192–1197
Subblefield MD, Vahdat LT, Balmaceda CM, Troxel AB, Hesdorffer CS, Gooch CL (2005) Glutamine as a neuroprotective agent in high-dose paclitaxel-induced peripheral neuropathy: a clinical and electrophysiologic study. Clin Oncol 17:271–276. https://doi.org/10.1016/j.clon.2004.11.014
Zirpoli GR, McCann SE, Sucheston-Campbell LE, Hershman DL, Ciupak G, Davis W, Unger JM, Moore HCF, Stewart JA, Isaacs C, Hobday TJ, Salim M, Hortobagyi GN, Gralow JR, Budd GT, Albain KS, Ambrosone CB (2017) Supplement use and chemotherapy-induced peripheral neuropathy in a cooperative group trial (S0221): the DELCaP study. JNCI 109:1–8. https://doi.org/10.1093/jnci/djx098
Chopra K, Tiwari V (2012) Alcoholic neuropathy: possible mechanisms and future treatment possibilities. Br J Clin Pharmacol 73:348–362. https://doi.org/10.1111/j.1365-2125.2011.04111.x
Kaddurah-Daouk R, Weinshilboum RM (2014) Pharmacometabolomics: implications for clinical pharmacology and systems pharmacology. Clin Pharmacol Ther 95:154–167. https://doi.org/10.1038/clpt.2013.217
Kwon HN, Kim M, Wen H, Kang S, Yang H, Choi M-J, Lee HS, Choi D, Park IS, Suh YJ, Hong S, Park S (2011) Predicting idiopathic toxicity of cisplatin by a pharmacometabonomic approach. Kidney Int 79:529–537. https://doi.org/10.1038/ki.2010.440
Keun HC, Sidhu J, Pchejetski D, Lewis JS, Marconell H, Patterson M, Bloom SR, Amber V, Coombes RC, Stebbing J (2009) Serum molecular signatures of weight change during early breast cancer chemotherapy. Clin Cancer Res 15:6716–6723. https://doi.org/10.1158/1078-0432.CCR-09-1452
Backshall A, Sharma R, Clarke SJ, Keun HC (2011) Pharmacometabonomic profiling as a predictor of toxicity in patients with inoperable colorectal cancer treated with capecitabine. Clin Cancer Res 17:3019–3028. https://doi.org/10.1158/1078-0432.CCR-10-2474
Hertz DL, Kidwell KM, Vangipuram K, Li F, Pai MP, Burness M, Griggs JJ, Schott AF, Poznak C, Van Hayes DF, Smith EML, Henry NL (2018) Paclitaxel plasma concentration after the first infusion predicts treatment-limiting peripheral neuropathy. Clin Cancer Res https://doi.org/10.1158/1078-0432.CCR-18-0656
Smith EML, Barton DL, Qin R, Steen PD, Aaronson NK, Loprinzi CL (2013) Assessing patient-reported peripheral neuropathy: the reliability and validity of the European Organization for Research and Treatment of Cancer QLQ-CIPN20 Questionnaire. Qual Life Res 22:2787–2799. https://doi.org/10.1007/s11136-013-0379-8
Postma TJ, Aaronson NK, Heimans JJ, Muller MJ, Hildebrand JG, Delattre JY, Hoang-Xuan K, Lantéri-Minet M, Grant R, Huddart R, Moynihan C, Maher J, Lucey R (2005) The development of an EORTC quality of life questionnaire to assess chemotherapy-induced peripheral neuropathy: the QLQ-CIPN20. Eur J Cancer 41:1135–1139. https://doi.org/10.1016/j.ejca.2005.02.012
Fayers P, Aaronson NK, Bjordal KCD, Grønvold M (2001) EORTC QLQ-C30 scoring manual, 3rd edn, EORTC Quality of Life Group, Brussels
Hertz DL, Kidwell KM, Vangipuram K, Sun D, Henry NL (2018) Abstract P6-11-03: association of systemic paclitaxel concentrations with severity and progression of paclitaxel-induced peripheral neuropathy. Cancer Res https://doi.org/10.1158/1538-7445.SABCS17-P6-11-03
Nagana Gowda GA, Raftery D (2017) Whole blood metabolomics by1H NMR spectroscopy provides a new opportunity to evaluate coenzymes and antioxidants. Anal Chem 89:4620–4627. https://doi.org/10.1021/acs.analchem.7b00171
Lacy P, McKay RT, Finkel M, Karnovsky A, Woehler S, Lewis MJ, Chang D, Stringer KA (2014) Signal intensities derived from different NMR probes and parameters contribute to variations in quantification of metabolites. PLoS ONE 9:1–10. https://doi.org/10.1371/journal.pone.0085732
Trexel J, Yoon GS, Keswani RK, McHugh C, Yeomans L, Vitvitsky V, Banerjee R, Sud S, Sun Y, Rosania GR, Stringer KA (2017) Macrophage-mediated clofazimine sequestration is accompanied by a shift in host energy metabolism. J Pharm Sci 106:1162–1174. https://doi.org/10.1016/j.xphs.2016.12.009
Xia J, Sinelnikov IV, Han B, Wishart DS (2015) MetaboAnalyst 3.0-making metabolomics more meaningful. Nucleic Acids Res 43:W251–W257. https://doi.org/10.1093/nar/gkv380
Storey JD (2003) The positive false discovery rate: a Bayesian interpretation and the q-value. Ann Stat 31:2013–2035. https://doi.org/10.1214/aos/1074290335
Storey JD, Tibshirani R (2003) Statistical significance for genomewide studies. Proc Natl Acad Sci 100:9440–9445. https://doi.org/10.1073/pnas.1530509100
Dunnet C (1955) A multiple comparison procedure for comparing several treatments with a control. J Am Stat Assoc 50:1096–1121
Gao J, Tarcea VG, Karnovsky A, Mirel BR, Weymouth TE, Beecher CW, Cavalcoli JD, Athey BD, Omenn GS, Burant CF, Jagadish HV (2010) Metscape: a Cytoscape plug-in for visualizing and interpreting metabolomic data in the context of human metabolic networks. Bioinformatics 26:971–973. https://doi.org/10.1093/bioinformatics/btq048
Cirillo M, Venturini M, Ciccarelli L, Coati F, Bortolami O, Verlato G (2009) Clinician versus nurse symptom reporting using the National Cancer Institute—Common Terminology Criteria for Adverse Events during chemotherapy: results of a comparison based on patient’s self-reported questionnaire. Ann Oncol 20:1929–1935. https://doi.org/10.1093/annonc/mdp287
Le-Rademacher J, Kanwar R, Seisler D, Pachman DR, Qin R, Abyzov A, Ruddy KJ, Banck MS, Lavoie Smith EM, Dorsey SG, Aaronson NK, Sloan J, Loprinzi CL, Beutler AS (2017) Patient-reported (EORTC QLQ-CIPN20) versus physician-reported (CTCAE) quantification of oxaliplatin- and paclitaxel/carboplatin-induced peripheral neuropathy in NCCTG/Alliance clinical trials. Support Care Cancer 25:3537–3544. https://doi.org/10.1007/s00520-017-3780-y
Bennett BK, Park SB, Lin CSY, Friedlander ML, Kiernan MC, Goldstein D (2012) Impact of oxaliplatin-induced neuropathy: a patient perspective. Support Care Cancer 20:2959–2967. https://doi.org/10.1007/s00520-012-1428-5
Huang L, Adachi N, Nagaro T, Liu K, Arai T (2007) Histaminergic involvement in neuropathic pain produced by partial ligation of the sciatic nerve in rats. Reg Anesth Pain Med 32:124–129. https://doi.org/10.1016/j.rapm.2006.11.009
Farshid AA, Tamaddonfard E, Najafi S (2015) Effects of histidine and n-acetylcysteine on experimental lesions induced by doxorubicin in sciatic nerve of rats. Drug Chem Toxicol 38:436–441. https://doi.org/10.3109/01480545.2014.981753
Yu J, Lou GD, Yue JX, Tang YY, Hou WW, Shou WT, Ohtsu H, Zhang SH, Chen Z (2013) Effects of histamine on spontaneous neuropathic pain induced by peripheral axotomy. Neurosci Bull 29:261–269. https://doi.org/10.1007/s12264-013-1316-0
Zhou G, Shoji H, Yamada S, Matsuishi T (1997) Decreased beta-phenylethylamine in CSF in Parkinson’s disease. J Neurol Neurosurg Psychiatry 63:754–758
Moyle JJ, Fox AM, Arthur M, Bynevelt M, Burnett JR (2007) Meta-analysis of neuropsychological symptoms of adolescents and adults with PKU. Neuropsychol Rev 17:91–101. https://doi.org/10.1007/s11065-007-9021-2
Boehm G, Cervantes H, Georgi G, Jelinek J, Sawatzki G, Wermuth B, Colombo J-P (1998) Effect of increasing dietary threonine intakes on amino acid metabolism of the central nervous system and peripheral tissues in growing rats. Pediatr Res 44:900
Gall WE, Beebe K, Lawton KA, Adam KP, Mitchell MW, Nakhle PJ, Ryals JA, Milburn MV, Nannipieri M, Camastra S, Natali A, Ferrannini E (2010) Α-hydroxybutyrate is an early biomarker of insulin resistance and glucose intolerance in a nondiabetic population. PLoS ONE https://doi.org/10.1371/journal.pone.0010883
Xiao WH, Zheng H, Zheng FY, Nuydens R, Meert TF, Bennett GJ (2011) Mitochondrial abnormality in sensory, but not motor, axons in paclitaxel-evoked painful peripheral neuropathy in the rat. Neuroscience 199:461–469. https://doi.org/10.1016/j.neuroscience.2011.10.010
Flatters SJL, Bennett GJ (2006) Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: evidence for mitochondrial dysfunction. Pain 122:245–257. https://doi.org/10.1016/j.pain.2006.01.037
Zhang H, Li Y, De Carvalho-Barbosa M, Kavelaars A, Heijnen CJ, Albrecht PJ, Dougherty PM (2016) Dorsal root ganglion infiltration by macrophages contributes to paclitaxel chemotherapy induced peripheral neuropathy HHS Public Access. J Pain 17:775–786. https://doi.org/10.1016/j.jpain.2016.02.011
Duggett NA, Griffiths LA, Flatters SJL (2017) Paclitaxel-induced painful neuropathy is associated with changes in mitochondrial bioenergetics, glycolysis, and an energy deficit in dorsal root ganglia neurons. Pain 158:1499–1508. https://doi.org/10.1097/j.pain.0000000000000939
Sucheston-Campbell LE, Clay-Gilmour AI, Barlow WE, Budd GT, Stram DO, Haiman CA, Sheng X, Yan L, Zirpoli G, Yao S, Jiang C, Owzar K, Hershman D, Albain KS, Hayes DF, Moore HC, Hobday TJ, Stewart JA, Rizvi A, Isaacs C, Salim M, Gralow JR, Hortobagyi GN, Livingston RB, Kroetz DL, Ambrosone CB (2018) Genome-wide meta-analyses identifies novel taxane-induced peripheral neuropathy-associated loci. Pharmacogenet Genom 28: 49–55
Schneider BP, Li L, Radovich M, Shen F, Miller KD, Flockhart DA, Jiang G, Vance G, Gardner L, Vatta M, Bai S, Lai D, Koller D, Zhao F, O’Neill A, Smith M, Lou Railey E, White C, Partridge A, Sparano J, Davidson NE, Foroud T, Sledge GW (2015) Genome-wide association studies for taxane-induced peripheral neuropathy in ECOG-5103 and ECOG-1199. Clin Cancer Res 21:5082–5091. https://doi.org/10.1158/1078-0432.CCR-15-0586
Baldwin RM, Owzar K, Zembutsu H, Chhibber A, Kubo M, Jiang C, Watson D, Eclov RJ, Mefford J, McLeod HL, Friedman PN, Hudis CA, Winer EP, Jorgenson EM, Witte JS, Shulman LN, Nakamura Y, Ratain MJ, Kroetz DL (2012) A genome-wide association study identifies novel loci for paclitaxel-induced sensory peripheral neuropathy in CALGB 40101. Clin Cancer Res 18:5099–5109. https://doi.org/10.1158/1078-0432.CCR-12-1590
Chen EI, Crew KD, Trivedi M, Awad D, Maurer M, Kalinsky K, Koller A, Patel P, Kim Kim J, Hershman DL. Chen EI, Crew KD, Trivedi M et al (2015) Identifying predictors of taxane-induced P1. Identifying predictors of taxane-induced peripheral neuropathy using mass spectrometry-based proteomics technology. PLoS ONE 10(12):e0145816. https://doi.org/10.1371/journal.pone.0
Budd GT, Barlow WE, Moore HCF, Hobday TJ, Stewart JA, Isaacs C, Salim M, Cho JK, Rinn KJ, Albain KS, Chew HK, Burton GV, Moore TD, Srkalovic G, McGregor BA, Flaherty LE, Livingston RB, Lew DL, Gralow JR, Hortobagyi GN (2015) SWOG S0221: a phase III trial comparing chemotherapy schedules in high-risk early-stage breast cancer. J Clin Oncol 33:58–64. https://doi.org/10.1200/JCO.2014.56.3296
Lu W, Su X, Klein MS, Lewis IA, Fiehn O, Rabinowitz JD (2017) Metabolite measurement: pitfalls to avoid and practices to follow. Annu Rev Biochem 86:277–304. https://doi.org/10.1146/annurev-biochem-061516-044952
Koulman A, Lane GA, Harrison SJ, Volmer DA (2009) From differentiating metabolites to biomarkers. Anal Bioanal Chem 394:663–670. https://doi.org/10.1007/s00216-009-2690-3
Ioannidis JPA, Bossuyt PMM (2017) Waste, leaks, and failures in the biomarker pipeline. Clin Chem 63:963–972. https://doi.org/10.1373/clinchem.2016.254649
Acknowledgements
We would like to thank Cora McHugh and Zyad Smiley at the University of Michigan College of Pharmacy Biochemical NMR Core for their technical and analytic support.
Funding
This work was supported through a Michigan Institute for Clinical and Health Research (MICHR) KL2 award to Dr. Daniel L. Hertz. Dr. Kathleen Stringer’s effort was supported, in part, by a Grant from the National Institute of General Medical Sciences (NIGMS R01 GM111400). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIGMS or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Daniel F. Hayes reports financial interest with Oncimmune LLC and Inbiomotion, serves as a consultant for Cepheid (no compensation), receives research grants from Merrimack Pharmaceuticals, Inc, Eli Lilly Company, Menarini/Silicon BioSystems, Puma Biotechnology, Inc, Pfizer, and Astra Zeneca, receives royalties from licensed technology from Janssen R&D, LLC, and holds three patents. The rest of the authors declare no conflict of interest.
Research involving human participants
The study was approved by the University of Michigan IRBMed (HUM 00086253). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sun, Y., Kim, J.H., Vangipuram, K. et al. Pharmacometabolomics reveals a role for histidine, phenylalanine, and threonine in the development of paclitaxel-induced peripheral neuropathy. Breast Cancer Res Treat 171, 657–666 (2018). https://doi.org/10.1007/s10549-018-4862-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4862-3