Abstract
Purpose
Screening mammography aims to improve breast cancer (BC) prognosis by increasing the incidence of early-stage tumours in order to decrease the incidence of late-stage cancer, but no reports have investigated these potential effects in an Australian population. Therefore we aimed to identify temporal trends in stage-specific BC in New South Wales (NSW), Australia, between 1972 and 2012.
Methods
An observational study of women who received a diagnosis of BC from 1972–2012 as recorded in the NSW Cancer Registry, a population-based registry with almost complete coverage and high rates of histological verification. We analysed trends in stage-specific incidence before screening and compared them to periods after screening began. Our primary group of interest was women in the target age range of 50–69 years, though trends in women outside the target age were also assessed.
Results
Screening was not associated with lower incidence of late-stage BC at diagnosis. Incidence for all stages remained higher than prescreening levels. In women aged 50–69 years, the incidence of carcinoma in situ (CIS), localised and regional BC has more than doubled compared to the prescreening era, with incidence rate ratios ranging from 2.0 for regional (95% CI 1.95–2.13) to 121.8 for CIS (95% CI 82.58–179.72). Before the introduction of screening, there was a downward trend in distant metastatic BC incidence, and after the introduction of screening there was an increase (IRR 1.8; 95% CI 1.62–2.00). In women too young to screen the incidence of late-stage BC at diagnosis also increased, whereas localised disease was stable.
Conclusions
The incidence of all stages of BC has increased over the past 40 years, with the greatest rise seen during the established screening period for women aged 50–69 years. Our findings suggest that some of the expected benefits of screening may not have been realised and are consistent with overdiagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For a cancer screening programme to be effective, it must detect disease at an early stage so that treatment might alter the natural history and reduce the risk of metastases [1]. In turn, this should decrease cancer mortality [2]. Therefore effective screening should result in an increased incidence of early-stage cancer and decreased incidence of late-stage cancer.
Staging information is essential in determining cancer prognosis [3, 4], treatment options and the effectiveness of screening programmes. Thus an analysis of stage-specific incidence is important when considering the benefits and harms of early detection. Trends in the stage distribution of BC before, during and after the introduction of the Australian national screening programme, BreastScreen, have not been evaluated. While several international studies have considered the stage distribution of BC incidence [5,6,7,8,9,10,11,12], few included CIS [5, 6, 8, 11], or assessed long-term effects of established screening [5, 7, 10].
Over the past three decades, the lifetime risk of an Australian woman being diagnosed with invasive BC has increased, from 1 in 12 to 1 in 8 [13]. The state of NSW in Australia provides a unique opportunity to examine the association of screening and incidence of advanced cancer as it is the only jurisdiction with historical records of BC stage at diagnosis. Since 1988, BreastScreen has offered free biennial screening to NSW women over age 40 using two-view mammography with double-reading. From 1991–2012, women aged 50-69 years were targeted via letters of invitation. Biennial participation rates for NSW women in the target age group have ranged from 51 to 56%. Participation for eligible women outside 50–69 years has been more variable, with higher rates in the early years of the programme at around 22%, dropping sharply in 2005 to around 7%. While the overall clinical burden of BC has increased, we do not know if this has translated into a decrease in more advanced cancers. Our aim was to examine the trends in stage-specific incidence of BC in women within and outside the target age group for BreastScreen, before and after the introduction of screening.
Methods
Study design and setting
Descriptive study set in NSW where around one-third of Australia’s female population reside.
Data sources and population
Incidence
We obtained de-identified individual data for all cases of female BC from the NSW Cancer Registry (NSWCR) diagnosed from 1972–2012. The NSWCR contains records of all new diagnoses of cancer in residents of NSW. The Registry has been collecting cancer data since 1972 with mandatory pathology reporting from 1986 and almost 100% coverage. BC is histologically verified for over 99% of CIS cases and approximately 95% of invasive lesions. The NSWCR is the only cancer registry in Australia that contains information on degree of spread from 1972 onwards. CIS of the breast has been notifiable since 1992 and completeness of CIS data before this time was estimated to be around 90% [14]. Female population estimates were obtained from the Australian Bureau of Statistics [15]. Our research protocol was approved by the NSW Population & Health Services Research Ethics Committee.
BC stage is assigned from the highest degree of spread within 4 months of the diagnosis. The NSW summary stage indicator is equivalent to the US Surveillance and Epidemiology End Results historic stage A (SEER SS2000) [16]. It classifies degree of BC spread as: CIS (a neoplasm that remains in the position of origin and has not invaded the basement membrane); localised (node-negative cancer confined to the breast); regional (spread to adjacent tissues or regional lymph nodes); distant metastases (spread beyond the breast, adjacent tissues and regional lymph nodes); and unknown (invasive BC with an unknown stage at diagnosis).
Inclusion and exclusion criteria
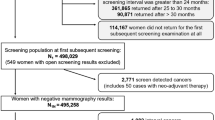
We identified 133,658 women with BC, diagnosed from 1972–2012: 12,218 CIS; 59,149 localised; 41,109 regional; 7309 distant metastases; and 13,873 unknown. We excluded cases that were not histologically verified (n = 6949), the majority of whom had an unknown stage (n = 3660), leaving 126,709 eligible women.
Screening mammography attendance
Screening mammography has been established in NSW for over 25 years. Data on annual numbers of mammographic examination for women aged 40 years and older were obtained from BreastScreen NSW for 1988–2012 (Fig. 1a). These data did not include private screening, and an additional 6.9% of NSW women aged 50–69 years have a bilateral mammogram annually through the Medicare Benefits Schedule (MBS), many of whom are likely to be asymptomatic and the mammography performed for screening purposes [17]. To capture publically funded screening outside of the programme, we obtained data on the number of bilateral mammograms in NSW reimbursed by the MBS from the Department of Human Services since 1984 (MBS item number 2734 for 1984–1991 and 59300 for 30 November 1991 onwards). The rate of MBS screening peaked around 1991, declined until 1996 and has been relatively stable since (Fig. 1b). The proportion of MBS-funded bilateral mammograms in women aged 50–69 years performed for screening purposes has been estimated to be around 53% [17], but is likely to be higher.
Statistical analysis
We divided the study into five time periods, which represent important periods concerning screening mammography in NSW. 1972–1983 was the period where there was no government-funded mammography and women were unexposed to mass screening. 1984–1987 saw the implementation of government-funded diagnostic mammography through the MBS and opportunistic screening. From 1988–1995, population-based screening was gradually introduced via BreastScreen NSW. 1996–2005 was the period where BreastScreen had full geographical coverage and reached a steady state. 2006–2012 saw the gradual replacement of film with digital mammography [18]. In each period, and for individual years over the entire study period from 1972–2012, we calculated the stage-specific incidence rates, standardised to the Australian 2001 population [19]. We used Poisson regression to analyse trends in incidence by period for relevant age groups. We compared incidence rates (IR), incidence rate ratios (IRR) and incidence rate differences (IRD) across the different periods for each age group.
We conducted two sensitivity analyses around unknown stage and method of diagnosis. Firstly, we recategorised unknown stage as localised, regional or distant metastatic BC. Secondly, we included women who did not have histologic verification and diagnosis was by any method, including cytology, imaging, post-mortem, death certificate as well as histology.
We used SAS software for statistical analyses [20]. We assumed that the number of cases for a specific period would follow a Poisson distribution from which 95% CIs were estimated [21]. For scatter plots, we used penalised B-splines to fit a smooth curve through trend points using the PBSPLINE statement in the SGPLOT procedure.
Results
A total of 126,709 women diagnosed with BC between 1972 and 2012 were eligible for the study. Figure 2 shows trends in the age-standardised incidence of stage-specific BC over time for women of all-ages, and Fig. 3 for women younger than 40 (Fig. 3a), women aged 40–49 (Fig. 3b), women aged 50–69 (Fig. 3c), and those aged 70 and older (Fig. 3d).


Note Rates were standardised by 5-year age intervals within broad age groups, using the Australian 2001 population
Age-standardised incidence of stage-specific breast cancer in NSW women, all ages, 1972–2012. a younger than 40 years of age, b 40–49 years of age, c 50–69 years of age, d 70 years of age and older.
There was a gradual increasing temporal trend in the age-standardised rates of CIS, localised and regional BC incidence for all-ages that accelerated from the late 1980s, coinciding with the introduction of screening mammography; rates for these stages have remained elevated since (Fig. 2). In contrast, the incidence of distant metastatic BC was relatively stable before screening, with rates for the most recent period of 2006–2012 higher compared to the prescreening period. The incidence of unknown BC fluctuated and was at its lowest level during 2006–2012. In women younger than age 40, there was a proportional increase in regional breast cancer, though the absolute change was small (Fig. 3a); the incidence of all other stages remained stable.
Early-stage breast cancer trends
The increased incidence of CIS and localised BC rates in NSW was greatest in women aged 50–69 years (Table 1; Fig. 3c). The average annual incidence of CIS among women aged 50–69 increased from 0.5 per 100,000 before screening to 58.8 per 100,000 during 2006–2012, corresponding to an IRD of 58.3 per 100,000 (95% CI 56.3–60.4) and IRR of 121.8 (95% CI 82.58–179.72) (Table 1). The incidence of localised BC more than doubled, from 63.3 before screening to 162.6 per 100,000 women during 2006–2012, with an IRD of 99.3 per 100,000 (95% CI 95.3–103.2) and an IRR of 2.6 (95% CI 2.47–2.67). In contrast, rates of CIS and localised BC in women younger and older than the screened group were either stable or had much smaller increases in IRRs compared to those aged 50–69 (Table 1; Fig. 3a, b, d).
Late-stage breast cancer trends
Changes in rates of late-stage BCs were similar for women aged 50–69 and those outside of the screening target age group (Table 1; Fig. 3). Regional BC in women aged 50–69 doubled from 53 per 100,000 before screening to 107 per 100,000 during 2006–2012, with an IRD of 54.4 per 100,000 (95% CI 51.1–57.7) and an IRR of 2.0 (95% CI 1.95–2.13). Over the same period, distant metastases increased from 9 to 17 per 100,000 with an IRD of 7.5 per 100,000 (95% CI 6.2–8.9) and an IRR of 1.8 (95% CI 1.6–2.0).
Sensitivity analysis
Incorporating cases that were not histologically verified made little difference to estimates for women younger than 50 years and did not affect early-stage BC. For regional BC, it decreased the IRR for women aged 70 and older from 2.1 to 1.7. For distant metastases, it decreased estimates for older women, though IRs remained equal to or higher than prescreening levels. For 2006–2012, the IRR in women aged 50–69 changed from 1.8 for histologically verified cancer to 1.3 for any method of diagnosis. The largest change in the IRR for distant metastases was in those older than 70 years with the IRR decreasing from 1.8 to 1.0.
When we recategorised all invasive cancers of unknown stage as localised and regional BC, it had a minimal effect on our estimates and the incidence trends persisted. Due to the relatively small number of cases of distant metastases, the IRs and IRRs were influenced by the addition of unknown stage, with the IRRs decreasing after 1996 for all age-groups. Younger women diagnosed with distant metastases were most sensitive to this recategorisation, with IRs for 2006–2012 less than prescreening levels. When we recategorised unknown stage as distant metastases in women older than 50 years, IRs remained higher in 2006–2012 compared to prescreening levels.
Screening participation
The increase in early-stage BC incidence in women aged 50–69 during the late 1980s coincided with increasing rates of MBS-funded bilateral mammograms, which rose by approximately 40% per year from 1985–1991 (Fig. 1b). BreastScreen NSW started in 1988 and screening rates increased dramatically from 1991–1993 (Fig. 1a) following a policy decision to actively recruit women via letters of invitation and advertising. Although women aged 50–69 years were officially targeted, local jurisdictions were able to recruit eligible women outside of the target age range using advertisements. From 2005 onwards, recruitment was limited to women aged 50–69, reflected in the large fall in screening mammography rates for women outside of the target age range at this time.
Discussion
Key results
We present the first temporal analysis of stage-specific incidence of BC in Australia. The data suggest that screening mammography involved a substantial rise in the detection of early-stage cancers that was not matched by a reduction in late-stage cancers. In fact, IRs for both early- and late-stage disease increased after the introduction of screening and incidence has not returned to prescreening levels. Before BreastScreen, CIS of the breast was rare and never above 1 per 100,000 in any age group. While still uncommon in women younger than 40, the incidence of CIS is now 59 per 100,000 for women aged 50–69 years. The incidence of localised BC among women invited to screening is currently double that in the prescreening era. Although the incidence of regional and distant metastases have also increased, this has been at similar rates for women outside and inside the screening targeted age range. Taken together, these data suggest that while the background rate across all stages has increased, screening has resulted in the detection of many more early-stage cancers.
Strengths and limitations
The NSWCR is a large, population-based dataset spanning over 40 years, has almost 100% coverage and high rates of histological confirmation. Notification of cancer to the registry has been mandatory since 1972 ensuring high coverage of population incidence. Screening mammography should have an immediate effect by increasing incidence directly after introduction (especially with early-stage cancers), and a delayed effect of reducing incidence in women who have left the screening programme (especially late-stage cancers, if there is a beneficial effect of early detection). We utilised 40 years of data which allows for these immediate and delayed effects. It is one of the few international registries that have collected data on stage, including CIS, from the outset. These factors make the NSWCR a unique dataset for studies of cancer epidemiology.
Our study, however, has several limitations. Histological verification for early-stage and regional BCs was high (98.8% of early-stage cancer and 97.6% of regional), but less complete for distant metastases (80.7%) and unknown cancers (73.6%). This is likely due to several factors including the availability of histopathology services in rural and remote areas of NSW, as well as clinical variation. Historically, clinical diagnosis (including imaging) was more common and histologic verification was deemed unnecessary as there were limited treatment options for advanced disease [22, 23]. Biopsy confirmation of distant metastases was rarely performed [24], with elderly and frail patients undergoing less testing and treatment [25]. In recent decades, however, histological confirmation has increased for distant metastases (91%) and unknown (75%) cancers, likely reflecting changes in clinical practice and better distribution of services throughout regional NSW. We conducted a sensitivity analysis around this by including any method of diagnosis for all stages and IRs remained equal to or higher than prescreening levels.
Although the rarity of CIS of the breast during the prescreening era may reflect some underreporting (CIS, unlike invasive cancer, was not legally notifiable in NSW until 1992) [14], estimates of the ratio of CIS to invasive BC were similar to other states where CIS was legally notifiable [14]. Further, prescreening incidence before 1983 was similar to other countries [26], suggesting capture was good. Regardless, almost 30 years of diagnostic and screening mammography in NSW have contributed to a substantial increase in the incidence of CIS. The detection of additional CIS is beneficial only when there is a corresponding decrease in the presentation of invasive disease which we did not observe.
Our results may be influenced slightly by the small proportion of cancers for which stage at diagnosis was unknown. Unknown stage accounts for 8.1% (n = 10,213) of all histologically verified cancers in our dataset and 10.4% (n = 13873) of all BC cases. Unknown stage has decreased over time, and the proportion of BC of unknown stage has fallen from 15% to 5%. Along with some of the changes in clinical practice outlined above, this decrease may be due to improving and more frequent cancer staging techniques. As unknown stage was more common in the prescreening period, the migration from unknown to known stages in more recent periods may have inflated the IRRs for invasive BCs (but not CIS). When we recategorised unknown stage as localised and regional, however, the incidence trends persisted. For distant metastases, the IRs and IRRs decreased as the small numbers in this category meant they were strongly influenced by the addition of unknown stage.
We provide estimates of the incidence rates for women outside of the target age range, where the IRRs have progressively increased compared to the prescreening period, though to a lesser extent than among women aged 50–69. The fall in localised disease during 2005 in women aged 70 and older coincided with a decrease in screening participation (Fig. 1a and Fig. 3d). Thus it is unlikely to be due to a compensatory drop in incidence following earlier detection of BC among the target age group [27]. There are, however, other factors that may explain some of the observed increasing incidence of BC in older women. Hormone replacement therapy (HRT) use is a known risk factor for BC [28]. HRT prescriptions in women older than 50 increased from 1996–2001 [29], but decreased by 55% between 2001 and 2005 [30,31,32] following the publication of the Women’s Health Initiative trial in 2002 [33]. Although some of the increase in BC incidence observed during 1996–2001 would be explained by HRT, BC risk returns to the population risk within two years after stopping HRT [34], thus HRT is unlikely to explain the increased rates during 2006–2012. While the decrease in HRT use after the publication of the Women’s Health Initiative trial has been linked to falls in the rates of BC for women in the target screening age of 50–69 years [29], current incidence remains higher than 2001, the estimated prevalence peak of HRT use in NSW.
Although the definitions of stage in the NSWCR have remained consistent over time, there may be differences in how cancer stage is determined due to increasing use of diagnostic tests. The adoption of sentinel lymph node biopsy (SNB) in NSW in the late 1990s [35, 36] for example, may have caused stage migration of localised to regional BC. The impact of this ‘upstaging’ is evident from 1998 (prior to SNB) through 2008, where the incidence of regional BC for all-ages increased by 28%, from 33.5 to 43.0 per 100,000 (Fig. 2), with 83% of NSW women diagnosed with BC in 2008 undergoing SNB [37]. SNB brought more meticulous examination of specimens, including a greater number of sections of tissue and enhanced staining [38] and the detection of micrometastases in lymph nodes [39]. Advances in pathological specimen processing and development of standards for axillary surgery in women may also have shifted some cancers to regional that would have otherwise been classified as localised. Likewise, the introduction of new technologies that are more sensitive than conventional imaging may have increased the detection of distant metastases [40] and moved some localised, regional or unknown BC into the distant category; however, we could find no direct evidence for this from population datasets. Stage migration, however, may not fully explain the rise of late-stage tumours. Other possible contributors to the ongoing increase in the incidence of regional BC include changes in the prevalence of risk factors for BC such as postmenopausal obesity [41], reproductive factors [42, 43], and increased awareness of BC and use of other early detection methods.
Comparison with other studies
International estimates from Denmark [44], the Netherlands [45], the USA [46] and the UK [12], found no decrease in advanced BC incidence with screening, along with large increases in early-stage disease. A review of incidence trends in Australia, Europe and the USA showed that in areas where screening mammography had been implemented there was no decrease in late-stage BC [47]. Two studies from the USA found a large increase in early-stage BC and a slight decrease in advanced BC [5, 7]. A similar pattern has also been observed in older women in the Netherlands [48]. A linked data analysis of BC incidence from Norway reported that screening attendance was associated with increased rates of early-stage and decreased rates of late-stage BC compared to non-attendees [8]. These results, however, are prone to selection bias due to the comparison groups, and in contrast to three other studies from Norway that found an increase in early-stage cancers with no decrease in more advanced cancers [9,10,11].
Interpretation
After a steady state of screening is reached, we would expect to see the incidence of early-stage BC stabilise and a fall in the incidence of late-stage disease. We found no evidence of a decrease in regional or metastatic BC. That distant metastases do not appear to be affected by screening mammography is a concern given prevention of advanced disease is a key aim of screening, along with a reduction in BC mortality. Further, with steady-state screening and relatively stable participation rates up to 2005, we would expect the incidence of CIS to stabilise. During 2006–2012, however, the absolute increase in the incidence of CIS relative to the period 1996 through 2005 for all age groups was 3 per 100,000. Reasons why the incidence continued to rise, especially when screening participation decreased in women outside of the target age range (Fig. 1a), may include changes in risk factors and more sensitive technology with the transition from film to digital mammography [49,50,51].
BC mortality rates in NSW have decreased considerably over the past 30 years. Among women aged 50–69 years, deaths from BC declined by 30%, from 68 to 48 deaths per 100,000 [52]. This reduction is probably due to both the effects of screening mammography and improved management [53,54,55]. Although we do not observe a decrease in distant metastases, we do not know what the trends would have been in the absence of screening. It is possible that screening may have resulted in relatively fewer metastases. These unexpected findings in relation to advanced cancer rates should prompt further exploration around their causes.
Further, our results indicate that our understanding of the natural history of BC is incomplete. They suggest that mammography may have limited ability to detect aggressive cancers at an earlier stage to prevent advancement to metastatic disease. The relatively stable incidence of distant metastases in NSW, despite widespread early detection and treatment, is consistent with the idea that BC may be a systemic disease [56] rather than one that progressively spreads [57, 58]. This theory is supported by the absence of any long-term adverse effects on distant metastatic rates or survival, following the clinical practice shift away from radical mastectomies to breast conserving surgery [59]. Our findings lend support to trials evaluating de-escalation of therapy for certain types of early-stage BC, such as DCIS [60].
Finally, our results are consistent with previous reports of overdiagnosis of invasive BC in NSW [61]. Due to the observational nature of our study, however, they require corroborating evidence as benefits and harms—including overdiagnosis—are best estimated by randomised controlled trials with long-term follow-up [55].
Conclusion
After 25 years of screening mammography, we found no evidence that detection of early-stage BC has reduced the incidence of late-stage disease. Combined with the expected increase in the incidence of early-stage cancers evident in this analysis, the overall result suggests substantial overdiagnosis, with a net increase in the clinical burden of BC and cost to the health system. Our findings indicate that some of the expected benefits of screening may not have been realised.
Abbreviations
- BC:
-
Breast cancer
- CIS:
-
Carcinoma in situ
- HRT:
-
Hormone replacement therapy
- IR:
-
Incidence rates
- IRR:
-
Incidence rate ratios
- IRD:
-
Incidence rate differences
- MBS:
-
Medicare benefits schedule
- NSW:
-
New South Wales
- NSWCR:
-
New South Wales Cancer Registry
- SNB:
-
Sentinel node biopsy
References
Cole P, Morrison AS (1980) Basic issues in population screening for cancer. J Natl Cancer Inst 64(5):1263–1272
Morrison AS (1992) Screening in chronic disease. Monographs in epidemiology and biostatistics (Book 19), 2nd edn. Oxford University Press, New York
Haybittle J, Blamey R, Elston C, Johnson J, Doyle P, Campbell F, Nicholson R, Griffiths K (1982) A prognostic index in primary breast cancer. Br J Cancer 45(3):361
Fitzgibbons PL, Page DL, Weaver D, Thor AD, Allred DC, Clark GM, Ruby SG, O’Malley F, Simpson JF, Connolly JL (2000) Prognostic factors in breast cancer: College of American Pathologists consensus statement 1999. Arch Pathol Lab Med 124(7):966–978
Bleyer A, Welch HG (2012) Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med 367(21):1998–2005
Buiatti E, Barchielli A, Bartolacci S, Federico M, De Lisi V, Bucchi L, Ferretti S, Paci E, Segnan N, Tumino R (2003) The impact of organised screening programmes on the stage-specific incidence of breast cancer in some Italian areas. Eur J Cancer 39(12):1776–1782
Esserman L, Shieh Y, Thompson I (2009) Rethinking screening for breast cancer and prostate cancer. JAMA 302(15):1685–1692
Hofvind S, Lee CI, Elmore JG (2012) Stage-specific breast cancer incidence rates among participants and non-participants of a population-based mammographic screening program. Breast Cancer Res Treat 135(1):291–299
Kalager M, Adami H-O, Bretthauer M, Tamimi RM (2012) Overdiagnosis of invasive breast cancer due to mammography screening: results from the Norwegian screening program. Ann Intern Med 156(7):491–499
Lousdal ML, Kristiansen IS, Møller B, Støvring H (2014) Trends in breast cancer stage distribution before, during and after introduction of a screening programme in Norway. Eur J Public Health 24(6):1017–1022
Lousdal ML, Kristiansen IS, Møller B, Støvring H (2016) Effect of organised mammography screening on stage-specific incidence in Norway: population study. Br J Cancer 114(5):590–596
McCann J, Stockton D, Day N (1998) Breast cancer in East Anglia: the impact of the breast screening programme on stage at diagnosis. J Med Screen 5(1):42–48
Australian Institute of Health and Welfare (2017) Australian Cancer Incidence and Mortality (ACIM) books: Breast cancer. Available from: AIHW. www.aihw.gov.au/acim-books. Accessed 7 June 2017
Osborn M, Armstrong B, Kricker A, Coates M (1999) Current recording and registration practices for carcinoma in situ (CIS) of the breast in Australasian State and Territory cancer registries. NHMRC National Breast Cancer Centre, Sydney
Australian Bureau of Statistics (2014) Australian Historical Population Statistics, 2014. Population Age-Sex Structure. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/0/632CDC28637CF57ECA256F1F0080EBCC?Opendocument. Accessed 9 Feb 2017
Young JL Jr, Roffers SD, Ries LAG, Fritz AG, Hurlbut AA (eds) (2001) SEER summary staging manual—2000: codes and coding instructions. National Cancer Institute, Bethesda
Department of Health and Ageing (2009) BreastScreen Australia evaluation. Screening Monograph No.1/2009. Evaluation final report. Canberra, Australia
Cancer Institute NSW (2006) Annual report 2005–2006. Cancer Institute NSW, Sydney
Australian Bureau of Statistics (2013) Which population to use for age standardisation? Australian Bureau of Statistics. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/products/42479A8EF04E40EBCA257C430016EA3B?OpenDocument. Accessed 31 May 2017
SAS Institute Inc (2011) SAS version 9.4 of the SAS System for Windows. SAS Institute Inc, Cary
Esteve J, Benhamou E, Raymond L (1994) Statistical methods in cancer research. Volume IV. Descriptive epidemiology. IARC Sci Publ 1(128):302
Baum M, Houghton J (1999) Contribution of randomised controlled trials to understanding and management of early breast cancer. BMJ 319(7209):568
Verghese A, Brady E, Kapur CC, Horwitz RI (2011) The bedside evaluation: ritual and reason. Ann Intern Med 155(8):550–553
Amir E, Clemons M (2009) Should a biopsy be recommended to confirm metastatic disease in women with breast cancer? Lancet Oncol 10(10):933–935
Bouchardy C, Rapiti E, Blagojevic S, Vlastos A-T, Vlastos G (2007) Older female cancer patients: importance, causes, and consequences of undertreatment. J Clin Oncol 25(14):1858–1869
Levi F, Te V-C, Randimbison L, La Vecchia C (1997) Trends of in situ carcinoma of the breast in Vaud, Switzerland. Eur J Cancer 33(6):903–906
Zahl P, Jørgensen KJ, Gøtzsche P (2013) Overestimated lead times in cancer screening has led to substantial underestimation of overdiagnosis. Br J Cancer 109(7):2014–2019
Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, Rodabough RJ, Gilligan MA, Cyr MG, Thomson CA (2003) Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative Randomized Trial. JAMA 289(24):3243–3253
Canfell K, Banks E, Moa AM, Beral V (2008) Decrease in breast cancer incidence following a rapid fall in use of hormone replacement therapy in Australia. Med J Aust 188(11):641–644
Canfell K, Banks E, Clements M, Kang YJ, Moa A, Armstrong B, Beral V (2009) Sustained lower rates of HRT prescribing and breast cancer incidence in Australia since 2003. Breast Cancer Res Treat 117(3):671–673
Australian Bureau of Statistics (1996) 1995 National Nutrition Survey. Basic Confidentialised Unit Record File (CURF), CD-ROM. Findings based on use of ABS Microdata. Canberra, Australia
Australian Bureau of Statistics (2002) 2001 National Health Survey. Expanded Confidentialised Unit Record File (CURF), Remote Access Data Laboratory (RADL). Findings based on use of ABS Microdata. Canberra, Australia
Writing Group for the Women’s Health Initiative Investigators (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA 288(3):321–333
Ravdin PM, Cronin KA, Howlader N, Berg CD, Chlebowski RT, Feuer EJ, Edwards BK, Berry DA (2007) The decrease in breast-cancer incidence in 2003 in the United States. N Engl J Med 356(16):1670–1674
Chua B, Ung O, Taylor R, Bilous M, Salisbury E, Boyages J (2001) Treatment implications of a positive sentinel lymph node biopsy for patients with early-stage breast carcinoma. Cancer 92(7):1769–1774
Ung OA (2004) Australasian experience and trials in sentinel lymph node biopsy: the RACS SNAC trial. Asian J Surg 27(4):284–290
Morris T, Wetzig N, Sinclair S, Kollias J, Zorbas H (2012) Evaluation of implementation of sentinel node biopsy in Australia. ANZ J Surg 82(7–8):541–547
Bilous M, Morey A, Armes J, Cummings M, Francis G (2006) Chromogenic in situ hybridisation testing for HER2 gene amplification in breast cancer produces highly reproducible results concordant with fluorescence in situ hybridisation and immunohistochemistry. Pathology (Phila) 38(2):120–124
Giuliano AE, Dale PS, Turner RR, Morton DL, Evans SW, Krasne DL (1995) Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg 222(3):394
Brennan M, Houssami N (2012) Evaluation of the evidence on staging imaging for detection of asymptomatic distant metastases in newly diagnosed breast cancer. Breast 21(2):112–123
Munsell MF, Sprague BL, Berry DA, Chisholm G, Trentham-Dietz A (2014) Body mass index and breast cancer risk according to postmenopausal estrogen-progestin use and hormone receptor status. Epidemiol Rev 36(1):114–136
Hunter DJ, Spiegelman D, Adami H-O, van den Brandt PA, Folsom AR, Goldbohm RA, Graham S, Howe GR, Kushi LH, Marshall JR, Miller AB, Speizer FE, Willett W, Wolk A, Yaun S-S (1997) Non-dietary factors as risk factors for breast cancer, and as effect modifiers of the association of fat intake and risk of breast cancer. Cancer Causes Control 8(1):49–56
Ewertz M, Duffy SW, Adami HO, Kvåle G, Lund E, Meirik O, Mellemgaard A, Soini I, Tulinius H (1990) Age at first birth, parity and risk of breast cancer: a meta-analysis of 8 studies from the nordic countries. Int J Cancer 46(4):597–603
Jørgensen K, Gøtzsche PC, Kalager M, Zahl P (2017) Breast cancer screening in Denmark: a cohort study of tumor size and overdiagnosis. Ann Intern Med 166(5):313–323
Autier P (2016) Mammography screening effectiveness and overdiagnosis in the Netherlands. In: Paper presented at the 4th international conference on Preventing Overdiagnosis, Barcelona, Spain, 20–22 Sept
Harding C, Pompei F, Burmistrov D, Welch HG, Abebe R, Wilson R (2015) Breast cancer screening, incidence, and mortality across US counties. JAMA Intern Med 175(9):1483–1489
Autier P, Boniol M, Middleton R, Doré J-F, Héry C, Zheng T, Gavin A (2011) Advanced breast cancer incidence following population-based mammographic screening. Ann Oncol 22(8):1726–1735
de Glas NA, de Craen AJ, Bastiaannet E, Op’t Land EG, Kiderlen M, van de Water W, Siesling S, Portielje JE, Schuttevaer HM, de Bock GTH (2014) Effect of implementation of the mass breast cancer screening programme in older women in the Netherlands: population based study. BMJ 349:g5410
Hofvind S, Skaane P, Elmore JG, Sebuødegård S, Hoff SR, Lee CI (2014) Mammographic performance in a population-based screening program: before, during, and after the transition from screen-film to full-field digital mammography. Radiology 272(1):52–62
Karssemeijer N, Bluekens AM, Beijerinck D, Deurenberg JJ, Beekman M, Visser R, Rv Engen, Bartels-Kortland A, Broeders MJ (2009) Breast cancer screening results 5 years after introduction of digital mammography in a population-based screening program. Radiology 253(2):353–358
Weber RJ, Nederend J, Voogd AC, Strobbe LJ, Duijm LE (2015) Screening outcome and surgical treatment during and after the transition from screen-film to digital screening mammography in the south of The Netherlands. Int J Cancer 137(1):135–143
Cancer Institute NSW (2016) Annual NSW cancer incidence and mortality data set, 2012. Cancer Registry NSW. Available at: http://www.statistics.cancerinstitute.org.au/trends_agegroup/trends_agegroup_mort_C50_NSW_extall_2.htm. Accessed 1 Aug 2017
Morrell S, Taylor R, Roder D, Dobson A (2012) Mammography screening and breast cancer mortality in Australia: an aggregate cohort study. J Med Screen 19(1):26–34
Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, Mandelblatt JS, Yakovlev AY, Habbema JDF, Feuer EJ (2005) Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 353(17):1784–1792
Independent UK Panel on Breast Cancer Screening (2012) The benefits and harms of breast cancer screening: an independent review. Lancet 380(9855):1778–1786
Fisher B (1980) Laboratory and clinical research in breast cancer—a personal adventure: the David A. Karnofsky memorial lecture. Cancer Res 40(11):3863–3874
Halsted WS (1907) I. The results of radical operations for the cure of carcinoma of the breast. Ann Surg 46(1):1
Welch HG, Gorski DH, Albertsen PC (2015) Trends in metastatic breast and prostate cancer—lessons in cancer dynamics. N Engl J Med 373:1685–1687
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong J-H, Wolmark N (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347(16):1233–1241
Identifier NCT02926911, Comparison of operative to monitoring and endocrine therapy (COMET) trial for low risk DCIS (COMET), 2016 Sept 19 (2000) National Library of Medicine (US). Available at: https://clinicaltrials.gov/ct2/show/NCT02926911. Accessed 4 June 2017
Morrell S, Barratt A, Irwig L, Howard K, Biesheuvel C, Armstrong B (2010) Estimates of overdiagnosis of invasive breast cancer associated with screening mammography. Cancer Causes Control 21(2):275–282
Acknowledgements
This work was supported by grants from the National Health and Medical Research Centre, Australia. A postgraduate scholarship (Grant No 1074626) was awarded to GJ and a Centre for Research Excellence award (Grant No 1104136) was awarded to AB. Incidence data were supplied by the NSW Central Cancer Registry, which is managed and operated by The Cancer Council NSW under contract to the NSW Health Department.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they do not have any conflicts of interest to report.
Ethical approval
Our research protocol was approved by the research ethics board of the NSW Population & Health Services Research Ethics Committee (Cancer Institute NSW reference number: LNR 2014/07/032).
Rights and permissions
About this article
Cite this article
Jacklyn, G., McGeechan, K., Irwig, L. et al. Trends in stage-specific breast cancer incidence in New South Wales, Australia: insights into the effects of 25 years of screening mammography. Breast Cancer Res Treat 166, 843–854 (2017). https://doi.org/10.1007/s10549-017-4443-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4443-x