Abstract
Purpose
Research suggests that physical activity may be a promising treatment for cancer-related cognitive impairment; however, evidence is limited by small samples and self-report measures and little is known about the underlying mechanisms. The purpose of this study was to examine the effects of physical activity on cognitive function in a national sample of breast cancer survivors (BCSs) using objective measures. We hypothesized that physical activity’s effects on cognition would be indirect through survivors’ self-reported fatigue.
Methods
Participants (N = 299; M = 57.51 ± 9.54 years) included BCSs with access to an iPad. Participants wore an accelerometer for seven consecutive days to measure their average daily minutes of moderate-to-vigorous physical activity (MVPA) and completed a battery of questionnaires and neuropsychological tests via an iPad application to measure fatigue and cognitive function. Cognitive function was modeled as two latent factors—executive function and working memory—comprising performance across seven cognitive tasks. A structural equation modeling framework was used to test the hypotheses.
Results
MVPA was associated with less fatigue (γ = 0.19), which, in turn, was associated with faster times on executive function tasks (γ = −0.18) and greater accuracy on working memory tasks (γ = 0.16). The indirect paths from MVPA to cognitive performance were also significant (executive function: β = −0.03, memory: β = 0.03).
Conclusions
Findings suggest that MVPA may be associated with greater executive function and working memory in BCSs. Further, this effect may be partially indirect through cancer-related symptoms (e.g., fatigue). Results emphasize the need for additional scientific investigation in the context of prospective and efficacy trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer-related cognitive impairment (CRCI) is increasingly receiving recognition as a priority in clinical research and practice [1, 2]. Among the cognitive functions most susceptible to cancer and its treatments are executive function and working memory [1, 3, 4], which involve top-down mental processes that control and regulate behaviors and actions and include the ability to temporarily store, translate, and apply information. Breast cancer survivors (BCS) have reported difficulties returning to work, concentrating, multi-tasking, and fulfilling social roles and have cited these side-effects as distressing and damaging to their self-confidence [5,6,7]. Unfortunately, these disruptions to daily functioning may be more extreme and common than in aging adults without cancer and may have lasting effects on survivors’ quality of life [8, 9]. Scientific investigation to develop evidence-based treatments of CRCI is needed.
The trajectory of cognitive impairment after cancer is thought to be parallel to that of aging, but may occur substantially earlier and at an accelerated rate when compared with healthy adults [8, 10, 11]. Therefore, aging models of cognition may have utility in BCS. The aging literature has provided strong evidence in support of aerobic physical activity for ameliorating age-related cognitive decline in older adults [12,13,14,15,16]. Recent studies in exercise oncology have extended these findings to cancer survivors [17,18,19,20,21]. Mackenzie et al. [19] found that more physically active BCS performed better on a working memory task regardless of treatment(s) received. Likewise, Hartman et al. [22] observed greater performance on tests of executive function and attention among BCS reporting the highest levels of physical activity. This nascent literature warrants further research, as findings to date are preliminary and limited by self-report measures and small samples. Few studies have investigated associations in larger samples, using objective measures of both physical activity and cognitive function [23], and in combination with self-report measures of physical, behavioral, and psychological correlates.
Fatigue has been identified as an important psychological correlate of both physical activity and CRCI. Specifically, physical activity is a well-documented, evidence-based treatment of cancer-related fatigue [2, 24, 25]. Fatigue has also been identified as a potential mechanism of cognitive impairment in cancer and non-cancer populations [4, 26,27,28]. As such, it is possible that increased physical activity may benefit fatigue symptoms, which, in turn, may improve cognitive functioning among survivors. However, to our knowledge, this path has not been investigated.
The purpose of this study was to examine relationships among physical activity, fatigue symptoms, and cognitive function (i.e., executive function and working memory) in a national sample of BCS using objective measures of physical activity (i.e., accelerometry) and cognitive functioning. We hypothesized that (1) average daily minutes of moderate-to-vigorous physical activity (MVPA) would be directly associated with self-reported fatigue, (2) fatigue would be directly associated with performance on cognitive tasks, and (3) MVPA would be indirectly associated with cognitive performance via fatigue symptoms. We hypothesized that these relationships would be evident independent of covariates of CRCI (e.g., age, treatment history) [24, 29].
Methods
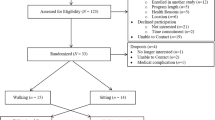
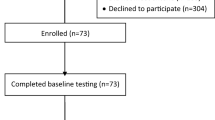
Participants and procedures
Participants included 299 women aged 21 years and older, diagnosed with breast cancer at any stage, and who had access to an iPad with iOS 6.1 or later. Women were recruited through the Army of Women©, social media, http://BreastCancerTrials.org, electronic fliers, and word of mouth. Interested individuals enrolled in the study by downloading an iPad app designed specifically for this study (powered by BrainBaseline©, Digital Artefacts, Iowa City, IA). Those who expressed interest were emailed links to a full description of the study. Upon logging into the app for the first time, participants confirmed their eligibility and electronically signed the institutional review board approved informed consent.
Participants were instructed to complete a battery of questionnaires and cognitive tasks via the app within 14 days of signing the consent form. The app provided participants with feedback on their progress through the assessments and on Day 10 of the data collection period automatically sent emails to remind participants to complete the assessments. Participants were also mailed an accelerometer to wear for seven consecutive days.
Measures
Demographic and clinical information
Demographics, breast cancer history, and general health history questionnaires were used to measure demographic and clinical information (Table 1). Covariates of CRCI and MVPA, including age, body mass index (BMI) category, menopausal status, comorbidities, treatment history, and hormonal therapies, were derived from these questionnaires. To measure comorbidities, participants were asked to respond yes/no to the following question: “Has your doctor diagnosed you with any of the following conditions?” This item was consistent with our previous research in BCS [30]. Comorbidities were summed across self-reported diagnosis of ten chronic diseases consistent with Goodman et al. [31]: arthritis, osteoporosis, asthma, chronic obstructive pulmonary disorder, congestive heart failure, heart attack, stroke, dementia, Type 2 diabetes, and depression. Participants were also asked to report if they ever received chemotherapy and/or radiation therapy. Treatment history was defined as receipt of chemotherapy + radiation, chemotherapy only, radiation only, or neither. Hormonal therapy history was derived from an item asking participants to choose which medication(s) they were currently taking and the number of months taking these medications. The list included aromatase inhibitors (e.g., anastrozole, exemestane, letrozole), tamoxifen, fulvestrant, toremifene, raloxifene, and none of these. Hormonal therapy history was modeled in months, and individuals reporting no medication were coded as 0 months.
Physical activity
Only participants who agreed via the consent form were mailed an accelerometer (Actigraph GT3X, Pensacola, FL). Participants were instructed to wear the device for seven consecutive days on a waistband on their non-dominant hip during their wake period, to move the device to their non-dominant wrist at bedtime, and return it to their waist upon wakening. Sleep time was filtered out before processing the accelerometer data for physical activity. When scored with an interruption period of 60 min, those with at least 10 h of wear time on at least 4 days were retained in analyses [32]. Devices were initialized to capture movement in 1-s epochs. Physical activity data were scored using Freedson cutpoints [33] and are represented as average daily minutes spent in MVPA (≥1952 counts/min).
Fatigue
The functional assessment of chronic illness therapy-fatigue scale (FACIT-F) [34] was used to measure fatigue. The FACIT-F is a 13-item questionnaire assessing self-reported fatigue and its impact upon daily function during the past 7 days. Higher scores signify less fatigue. Internal consistency in the present sample was high (α = 0.94).
Cognitive function
Cognitive function was measured as participants’ performance on tasks of executive function and working memory (detailed below) administered through the BrainBaseline© iPad platform. Raw data from each task were downloaded from BrainBaseline© and processed in MATLAB R2014b Version 8.4 (MathWorks, Inc., Natick, MA) to calculate summary scores for each variable included in data analyses. Extreme values were Winsorized at ±3.0 standard deviations from the mean for each variable. Reaction times on the flanker and task-switch tasks were coded as missing when corresponding accuracy was less than 50%.
Executive function
Flanker
During the flanker task [35], participants were presented with a central fixation cross for 500 ms. Next, a flanker display consisting of five arrows was presented for 2000 ms or until a response was made. On a random half of the trials, the flanking arrows (two on each side) pointed in the same direction as the target arrow (congruent), and on the other half they pointed in the opposite direction (incongruent). Participants were instructed to focus on the central arrow and report as quickly and accurately as possible whether the arrow pointed to the right or left. Task performance was defined as reaction time across incongruent trials.
Mazes
The mazes task required participants to use their finger to draw a line from the start of the maze to the finish. Task performance was measured as the total time spent drawing while completing the maze.
Task-switch
Task-switch [36] trials began with the presentation of a pink or blue square, inside of which was a number (1–4 or 6–9). Numbers were presented individually for 2500 ms. If the background was blue, participants were asked to report (by touching buttons on the screen with their left hand) whether the number was higher or lower than 5. If the background was pink, participants were asked to report whether the number was odd or even using the right hand. Participants completed 48 trials in which the task switched unpredictably from trial to trial. Task performance was defined as reaction time across switch trials.
Trails B
During trails B [37] participants used their finger to draw a line as quickly as possible between a series of alternating numbers and letters in ascending order (i.e., 1, A, 2, B, etc.). Task performance was defined as the total time to complete the trail.
Working memory
Spatial span
Spatial span required participants to identify a pattern of green dots. Individual dots momentarily turned green in a particular order. When prompted, the subject was asked to tap the dots in the reverse order in which the dots were highlighted. The patterns became progressively longer across each trial. Task performance was defined as the maximum number of dot locations correctly remembered in sequence.
Spatial working memory (SPWM)
Each SPWM trial began with presentation of a central fixation point for 1500 ms. Next, sets of two or three black dots appeared on the screen for 500 ms. The locations of the dots were randomly determined on each trial. Participants were instructed to remember the location of each dot in the array. After a 1000 ms delay, a single red probe dot appeared at one location on the screen, and participants were asked to determine if the location of the red dot matched one of the locations occupied by one of the black dots. The red probe dot remained on the screen for 2000 ms or until the participant responded. The probe dot matched the location of one of the black dots on half of the 60 trials. Task performance was defined as accuracy for the sets containing three dots.
Swap
Participants first observed the spatial positioning of three or five ordinary objects on the screen (e.g., table and chairs, banana, drum, teacup, and saucer). The viewing window then becomes blank and the objects are lined across the bottom of the screen. When prompted, the participant was asked to use their finger to drag the objects back to their original position in the window. Task performance for the present study was defined as the average number of distortions, or placement of objects in positions not used in the initial array, on sets including five objects.
Data analysis
The hypothesized pathways from MVPA to fatigue to executive function and working memory were tested using a structural equation modeling framework (MPlus v7.31; Muthén and Muthén, 1998–2015). This approach allowed us to test relationships while controlling for covariates. Preliminary analyses indicated that missing data were missing at random; therefore, the full information maximum likelihood estimation was used [38, 39]. Only individuals with valid accelerometer wear-time were included (N = 299/340 sent). Data were missing due to device malfunction (n = 1), participant decline to wear upon device receipt (n = 35), incomplete wear (≤4 days of valid wear; n = 2), and loss of device (n = 3). The extent of missing data on the app-based assessments ranged from 1.7% (fatigue) to 7.0% (spatial span).
Prior to hypothesis testing, a confirmatory factor analysis was conducted to model executive function and working memory as latent constructs. The executive function latent factor comprised flanker incongruent reaction time, mazes drawing time, task-switch reaction time on switch trials, and trails B overall time. Working memory comprised SPWM accuracy on three-probe trials, spatial span correct responses, and swap distortions. Flanker reaction time and SPWM accuracy were fixed to 1 to identify each scale, while other indicators were freely estimated. The hypothesized pathways were then tested as follows: (1) direct effect of MVPA on fatigue, (2) direct effect of fatigue on executive function and working memory, and (3) indirect effect of MVPA on executive function and working memory via fatigue. To further test that the effect of MVPA on cognitive performance was indirect, we tested the direct effect of MVPA on executive function and working memory. Age, BMI category, menopausal status, comorbidities, treatment(s) received, and months of hormonal therapy were included in all models to test the effects of MVPA and fatigue on cognitive performance independent of covariates. Significant effects are presented as standardized effects at a one-tailed alpha of p < 0.05. Model fit was assessed using standard, accepted indices: non-significant normal theory weighted χ 2, comparative fit index (CFI >0.90), root mean square error of approximation (RMSEA <0.05), and standardized root mean residual (SRMR <0.08) [40].
Results
Participant characteristics and descriptive statistics of primary outcome variables are reported in Tables 1 and 2, respectively. Briefly, participants ranged in age from 28 to 79 years (M = 57.51 ± 9.54 years) and were primarily white, educated, affluent, and married. Most were not currently taking any of the listed medications (n = 151). Among those taking medication, most reported an aromatase inhibitor (n = 84), followed by tamoxifen (n = 47). The measurement model for the executive function and working memory latent factors provided excellent fit to the data (χ 2 = 14.24 [13], p = 0.36, CFI = 0.99, RMSEA = 0.02 [90% CI = 0.00–0.06], SRMR = 0.03), and all factor loadings were significant (p < 0.001; Fig. 1). Next, a model was tested that specified the direct effects of MVPA on fatigue; direct effects of fatigue on executive function and working memory; and indirect effects of MVPA on executive function and working memory. The model including age, BMI category, menopausal status, comorbidities, treatment history, and hormonal therapy as covariates had excellent fit to the data (χ 2 = 53.82 [55], p = 0.52, CFI = 1.00, RMSEA = 0.00 [90% CI = 0.00–0.04], SRMR = 0.03).
As hypothesized, a direct path from MVPA to fatigue symptoms was observed (γ = 0.19, z = 3.44, p < 0.001) whereby greater daily MVPA was associated with fewer fatigue symptoms (Fig. 2). Additionally, direct paths from fatigue to executive function and working memory were observed whereby fewer fatigue symptoms were associated with faster times on executive function tasks (γ = −0.18, z = −2.50, p = 0.005) and higher accuracy on working memory tasks (γ = 0.16, z = 1.88, p = 0.03). The indirect paths from MVPA to cognitive performance, through fatigue, were also significant (executive function: β = −0.03, z = −2.01, p = 0.02, memory: β = 0.03, z = 1.65, p < 0.05). Finally, we did not find evidence of a direct path from MVPA to working memory (γ = 0.03, z = 0.31, p = 0.76). However, contrary to our hypothesis, a direct effect of MVPA on executive function was observed (γ = −0.13, z = −1.95, p = 0.03). Goodness of fit of the model including the latter path was similar to that of the hypothesized model (χ 2 = 50.08 [54], p = 0.63, CFI = 1.00, RMSEA = 0.00 [90% CI = 0.00–0.03], SRMR = 0.03).
Structural equation model of relationships among moderate-to-vigorous physical activity (MVPA), fatigue, and cognitive function. Note all coefficients represent standardized estimates from model output. Solid lines reflect statistical significance at p < 0.05, one-tailed. Covariate paths have been omitted for clarity, but are presented in the text. aNegative path indicates more daily minutes of MVPA were associated with faster reaction times on executive function tasks. bPositive path indicates more daily minutes of MVPA were associated with less fatigue. cNegative path indicates less fatigue was associated with faster reaction times on executive function tasks. dPositive path indicates less fatigue was associated with greater accuracy on working memory tasks
A number of associations between covariates and other model constructs were observed. Age emerged as the strongest correlate of fatigue, executive function, and working memory (γ = 0.35, z = 5.89, p < 0.001; γ = 0.53, z = 6.98, p < 0.001; γ = −0.38, z = −3.99, p < 0.001, respectively). Older women reported fewer fatigue symptoms, had slower performance on executive function tasks and lower accuracy on working memory tasks. Menopausal status and months of hormonal therapy were not associated with cognitive performance (p > 0.32), but were negatively associated with fatigue (menopause: γ = −0.13, z = −2.30, p = 0.01, hormonal: γ = 0.10, z = 1.81, p = 0.04). Post-menopausal women and those taking adjuvant hormonal therapies for fewer months reported greater fatigue. The number of self-reported comorbidities was significantly associated with fatigue and cognitive performance (fatigue: γ = −0.26, z = −4.71, p < 0.001, executive function: γ = 0.14, z = 1.89, p = 0.03, memory: γ = −0.18, z = −2.08, p = 0.02). Those with more comorbidities had more fatigue symptoms and worse performance on executive function and working memory tasks. BMI category was associated with executive function (γ = −0.13, z = −1.89, p = 0.03), but not with fatigue or working memory (p > 0.15). Overweight and obese women had faster reaction times on executive function tasks when compared with normal weight women. Treatment history was not associated with fatigue or cognitive performance (p > 0.17). The model including covariates explained 40 and 24% of the variance in executive function and working memory, respectively (Fig. 2).
Discussion
Findings of the present study support an emerging literature on exercise and CRCI. Notably, positive relationships between MVPA, executive function, and working memory were observed via objective measures of both physical activity and cognitive function, using multiple indicators of cognitive function, across a national sample of BCS, and independent of hypothesized covariates. Results extend previous research in suggesting the effects of MVPA on CRCI may be partially explained by MVPA’s influence on cancer-related symptoms such as fatigue. Additionally, in testing multiple cognitive domains together, the current study suggests that both executive function and working memory may be sensitive to the benefits of exercise. Taken together, findings contribute to our knowledge of the mechanisms of CRCI and indicate a need for experimental trials testing the effects of exercise on cognitive function in cancer survivors.
Results are consistent with the aging literature [12, 13, 16, 41] and corroborate previous cross-sectional work in cancer survivors. For instance, Hartman et al. [22] observed a positive association between BCS’s self-reported physical activity and performance on neuropsychological tests of executive function and attention. A number of studies have also observed a positive effect of MVPA on working memory [18, 19, 42]. The cancer literature suggests that cognitive processes may be differentially affected by cancer and its treatments [27], and the benefits of exercise to CRCI may also be specific to particular cognitive domains. Consistent with this, reviews and meta-analyses in older adults, while observing benefits of MVPA on multiple cognitive domains, indicate that the effects may be strongest for executive control processes [12, 41]. Our results also indicate that MVPA may differentially affect cognitive domains in BCS. Specifically, the data suggest a stronger effect of MVPA on executive function when compared with working memory, in addition to a direct effect of MVPA on executive function. However, additional studies testing the effects of exercise on multiple domains of cognitive function concomitantly are needed.
Mackenzie et al. [8] have noted that treatment of CRCI is limited due to a lack of understanding of the underlying mechanisms. As such, of further interest is the finding that MVPA’s effects on executive function and working memory were indirect through fatigue. This finding is consistent with a framework proposed by Janelsins et al. [27] in which fatigue and inflammation may be important mechanisms between cancer treatment(s) and CRCI. Specifically, fatigue has been associated with increased levels of pro-inflammatory cytokines (IL-6, IL-8, IL-10), which have been linked to CRCI [4, 24, 26, 43]. In non-cancer populations, inflammation has also been associated with aging and cognitive decline [28], and physical activity is known to protect against systemic inflammation [44]. Therefore, an important area of future research includes examination of fatigue and inflammation as mediators of the pathway between exercise and CRCI. If our preliminary findings are corroborated, exercise intervention studies targeting cancer-related fatigue may be useful in informing the design of exercise interventions addressing CRCI [45].
Further research examining the influence of exercise on brain structure and function, in addition to cognitive functions, is also warranted. The direct effect of MVPA on executive function suggests that mechanisms other than fatigue (e.g., brain structure, function) may also contribute to exercise’s influence on cognitive function in BCS. Most of the available literature on the effects of exercise on brain health in cancer patients and survivors has focused on the hippocampus and memory functions [17, 21, 46]. Our findings support this research and suggest that memory may be a strong candidate for modifiable lifestyle intervention among cancer survivors [14]. However, deficits in prefrontal cortex-dependent processes (e.g., executive function) are also frequently reported by cancer survivors [47], but rarely have been investigated in neurobiological studies of CRCI [21]. Our findings support further investigation of exercise’s influence on prefrontal cortex health and function, in addition to hippocampal health and function. Exercise studies combining neuropsychological testing with neurobiological assessments may be most informative.
Interestingly, being overweight or obese was associated with faster reaction times on executive function tasks. This finding is contrary to those of previous studies in which overweight and obese participants exhibited worse performance on cognitive tasks [22] and MVPA was associated with cognitive performance only in overweight and obese BCS [23]. Treatment(s) received and current hormonal therapy use were not associated with executive function or working memory in the present study. Similar to Mackenzie et al. [19], MVPA’s effects on cognitive performance were evident regardless of the treatments survivors received. As participants in our study were generally long-term survivors, studies examining interactions between MVPA and treatment-related factors during active treatment and the early survivorship period may uncover for whom and when physical activity may be most beneficial in mitigating CRCI.
Approximately two-thirds of our sample reported at least one chronic condition, and comorbidities were associated with fatigue and cognitive performance. BCS represent a population facing the intersection of cancer and aging [48] and, as a result, a number of other health conditions in addition to or following cancer. Physical activity represents a modifiable, non-pharmacologic treatment that benefits many health outcomes in addition to cognitive functioning, including reduced risk of cancer recurrence; decreased levels of fatigue, depression, and anxiety; improved physical fitness; and enhanced self-worth and quality of life [8, 30]. Unfortunately, surveillance data suggest that BCS may participate in as little as 3.7 min of MVPA/day [49]. While we observed a positive effect of MVPA on cognitive function independent of comorbidities, further research focusing on the effects of physical activity in survivors with multiple chronic conditions is warranted. These individuals may not only represent survivors with the greatest cognitive impairment, but they may also have the lowest physical activity levels [50].
Limitations
Despite the strengths of this study (e.g., national sample, app-based assessment), there are some notable limitations. As data were cross-sectional, causal links among MVPA, fatigue, and CRCI cannot be discerned. Efficacy trials are needed to confirm the preliminary findings of this study and others. Additionally, although we gathered data from a national sample, participants were generally well-educated, affluent, and white, thereby limiting the generalizability of the results. This may in part be due to the iPad inclusion criterion. Although we still observed effects in this homogeneous sample, testing platforms that are mobile-phone compatible (e.g., BrainBaseline© for the iPhone) and available in other languages (e.g., NIH toolbox) may broaden our understanding of CRCI in more diverse populations of BCS. Finally, the mechanisms of fatigue and CRCI are complex and may include a number of psychological, physiological, genetic, behavioral, and treatment-related determinants [4, 24]. Therefore, while the present study provides preliminary information on the role of fatigue along the pathway between MVPA and CRCI, studies examining other symptoms (e.g., anxiety, depression), biomarkers (e.g., inflammation, fitness, brain volume), and behaviors (e.g., sleep) may further contribute to our knowledge and treatment of CRCI.
Conclusions
Findings suggest that participation in daily MVPA may be associated with greater executive function and working memory in BCS. The effect of MVPA may be partially indirect through cancer-related symptoms such as fatigue. Results emphasize the need for additional scientific investigation of relationships between MVPA and CRCI, particularly prospective and efficacy trials that test effects temporally and against a comparison group. As BCS represent a rapidly growing population of women at the intersection of aging and cancer, the personal and public health burden of CRCI may be considerable. Identification of evidence-based treatments is critically needed.
References
Wefel JS, Vardy J, Ahles T, Schagen SB (2011) International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol 12(7):703–708. doi:10.1016/S1470-2045(10)70294-1
Runowicz CD, Leach CR, Henry NL et al (2016) American Cancer Society/American Society of Clinical Oncology breast cancer survivorship care guideline. CA Cancer J Clin 66(1):43–73. doi:10.3322/caac.21319
Argyriou AA, Assimakopoulos K, Iconomou G, Giannakopoulou F, Kalofonos HP (2011) Either called “chemobrain” or “chemofog,” the long-term chemotherapy-induced cognitive decline in cancer survivors is real. J Pain Symptom Manag 41(1):126–139. doi:10.1016/j.jpainsymman.2010.04.021
Janelsins MC, Kesler SR, Ahles TA, Morrow GR (2014) Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry 26(1):102–113. doi:10.3109/09540261.2013.864260
Ahles TA, Root JC, Ryan EL (2012) Cancer- and cancer treatment-associated cognitive change: an update on the state of the science. J Clin Oncol 30(30):3675–3686. doi:10.1200/JCO.2012.43.0116
Myers JS (2011) Chemotherapy-related cognitive impairment: the breast cancer experience. Oncol Nurs Forum 39(1):E31–E40. doi:10.1188/12.ONF.E31-E40
Von Ah D, Habermann B, Carpenter JS, Schneider BL (2013) Impact of perceived cognitive impairment in breast cancer survivors. Eur J Oncol Nurs 17(2):236–241. doi:10.1016/j.ejon.2012.06.002
Mackenzie M, Zuniga K, McAuley E (2006) Cognitive impairment in breast cancer: the protective role of physical activity, cardiorespiratory fitness, and exercise training. In: McMorris T (ed) Exercise-cognition interaction: neuroscience perspectives. Elsevier, Amsterdam
Wefel JS, Lenzi R, Theriault RL, Davis RN, Meyers CA (2004) The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer 100(11):2292–2299. doi:10.1002/cncr.20272
Maccormick RE (2006) Possible acceleration of aging by adjuvant chemotherapy: a cause of early onset frailty? Med Hypotheses 67(2):212–215. doi:10.1016/j.mehy.2006.01.045
Merriman JD, Von Ah D, Miaskowski C, Aouizerat BE (2013) Proposed mechanisms for cancer- and treatment-related cognitive changes. Semin Oncol Nurs 29(4):260–269. doi:10.1016/j.soncn.2013.08.006
Bherer L, Erickson KI, Liu-Ambrose T (2013) A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. J Aging Res. doi:10.1155/2013/657508
Colcombe SJ, Erickson KI, Scalf PE et al (2006) Aerobic exercise training increases brain volume in aging humans. J Gerontol A 61(11):1166–1170
Erickson KI, Voss MW, Prakash RS et al (2011) Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci USA 108(7):3017–3022. doi:10.1073/pnas.1015950108
Hillman CH, Erickson KI, Kramer AF (2008) Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci 9(1):58–65. doi:10.1038/nrn2298
Northey JM, Cherbuin N, Pumpa KL, Smee DJ, Rattray B, Northey JM (2017) Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis. (3):1–9. doi:10.1136/bjsports-2016-096587
Chaddock-Heyman L, Mackenzie MJ, Zuniga K et al (2015) Higher cardiorespiratory fitness levels are associated with greater hippocampal volume in breast cancer survivors. Front Hum Neurosci 9(August):465. doi:10.3389/fnhum.2015.00465
Cooke GE, Wetter NC, Banducci SE et al (2016) Moderate physical activity mediates the association between white matter lesion volume and memory recall in breast cancer survivors. PLoS ONE 11(2):e0149552. doi:10.1371/journal.pone.0149552
Mackenzie MJ, Zuniga KE, Raine LB et al (2016) Associations between physical fitness indices and working memory in breast cancer survivors and age-matched controls. J Womens Health (Larchmt) 25(1):99–108. doi:10.1089/jwh.2015.5246
Sprod LK, Mohile SG, Demark-Wahnefried W et al (2012) Exercise and cancer treatment symptoms in 408 newly diagnosed older cancer patients. J Geriatr Oncol 3(2):90–97. doi:10.1016/j.jgo.2012.01.002
Zimmer P, Baumann FT, Oberste M et al (2016) Effects of exercise interventions and physical activity behavior on cancer related cognitive impairments: a systematic review. Biomed Res Int. doi:10.1155/2016/1820954
Hartman SJ, Marinac CR, Natarajan L, Patterson RE (2014) Lifestyle factors associated with cognitive functioning in breast cancer survivors. Psychooncology. doi:10.1002/pon.3626
Marinac CR, Godbole S, Kerr J, Natarajan L, Patterson RE, Hartman SJ (2015) Objectively measured physical activity and cognitive functioning in breast cancer survivors. J Cancer Surviv 9(2):230–238. doi:10.1007/s11764-014-0404-0
Bower JE (2014) Cancer-related fatigue—mechanisms, risk factors, and treatments. Nat Rev Clin Oncol 11(10):597–609. doi:10.1038/nrclinonc.2014.127
Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O (2015) Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database Syst Rev (8). www.cochranelibrary.com
Ahles TA, Saykin AJ (2007) Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer 7(3):192–201. doi:10.1038/nrc2073
Janelsins MC, Kohli S, Mohile SG, Usuki K, Ahles TA, Morrow GR (2011) An update on cancer- and chemotherapy-related cognitive dysfunction: current status. Semin Oncol 38(3):431–438. doi:10.1053/j.seminoncol.2011.03.014
Sartori AC, Vance DE, Slater LZ, Crowe M (2012) The impact of inflammation on cognitive function in older adults: implications for healthcare practice and research. J Neurosci Nurs 44(4):206–217. doi:10.1097/JNN.0b013e3182527690
Asher A, Myers JS (2015) The effect of cancer treatment on cognitive function. Clin Adv Hematol Oncol 13(7):441–450
Phillips S, McAuley E (2015) Associations between self-reported post-diagnosis physical activity changes, body weight changes, and psychosocial well-being in breast cancer survivors. Support Care Cancer 23:159–167. doi:10.1007/s00520-014-2346-5
Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK (2013) Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. 10. doi:10.5888/pcd10.120239
Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M (2008) Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 40(1):181–188. doi:10.1249/mss.0b013e31815a51b3
Freedson P, Melanson E, Sirard J (1998) Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sport Exerc 30:777–781
Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E (1997) Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manag 13(2):63–74. doi:10.1016/S0885-3924(96)00274-6
Eriksen BA, Eriksen CW (1974) Effects of noise letters upon the identification of a target letter in a nonsearch task. Percept Psychophys 16(1):143–149. doi:10.3758/BF03203267
Monsell S (2003) Task switching. Trends Cogn Sci 7(3):134–140. doi:10.1016/S1364-6613(03)00028-7
Battery AIT (1994) Manual of directions and scoring. War Department, Adjutant General’s Office, Washington, DC
Muthén B, Kaplan D, Hollis M (1987) On structural equation modeling with data that are not missing completely at random. Psychometrika 52(3):431–462. doi:10.1007/BF02294365
Larsen R (2011) Missing data imputation versus full information maximum likelihood with second-level dependencies. Struct Equ Model Multidiscip J 18(4):649–662. doi:10.1080/10705511.2011.607721
Hu L, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J 6(1):1–55. doi:10.1080/10705519909540118
Colcombe S, Kramer AF (2003) Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci J Am Psychol Soc 14(2):125–130
Crowgey T, Peters KB, Hornsby WE et al (2013) Relationship between exercise behavior, cardiorespiratory fitness, and cognitive function in early breast cancer patients treated with doxorubicin-containing chemotherapy: a pilot study 1. Appl Physiol Nutr Metab 39(December):724–729
Cheung YT, Lim SR, Ho HK, Chan A (2013) Cytokines as mediators of chemotherapy-associated cognitive changes: current evidence, limitations and directions for future research. PLoS ONE. doi:10.1371/journal.pone.0081234
Woods JA, Wilund KR, Martin SA, Kistler BM (2012) Exercise, inflammation and aging. Aging Dis 3(1):130–140
Mustian KM, Sprod LK, Janelsins M, Peppone LJ, Mohile S (2012) Exercise recommendations for cancer-related fatigue, cognitive impairment, sleep problems, depression, pain, anxiety, and physical dysfunction: a review. Oncol Hematol Rev 8(2):81–88
Kesler S, Janelsins M, Koovakkattu D et al (2013) Reduced hippocampal volume and verbal memory performance associated with interleukin-6 and tumor necrosis factor-alpha levels in chemotherapy-treated breast cancer survivors. Brain Behav Immun 30(Suppl.):S109–S116. doi:10.1016/j.bbi.2012.05.017
Lindner OC, Phillips B, McCabe MG et al (2014) A meta-analysis of cognitive impairment following adult cancer chemotherapy. Neuropsychology 28(5):726–740. doi:10.1037/neu0000064
Desantis C, Ma J, Bryan L, Jemal A (2014) Breast cancer statistics, 2013. CA Cancer J Clin 64:52–62. doi:10.3322/caac.21203
Lynch BM, Dunstan DW, Healy GN, Winkler E, Eakin E, Owen N (2010) Objectively measured physical activity and sedentary time of breast cancer survivors, and associations with adiposity: findings from NHANES (2003–2006). Cancer Causes Control 21(2):283–288. doi:10.1007/s10552-009-9460-6
Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “Silver Tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomark Prev 25(7). doi:10.1158/1055-9965.EPI-16-0133
Acknowledgements
The authors would like to acknowledge Allen Best and the Team at Digital Artefacts for their development of the iPad application used for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
DKE is supported by an American Cancer Society Postdoctoral Fellowship (PF-16-021-01-CPPB).
Ethical approval
This study was approved by and carried out in accordance with the recommendations of the Institutional Review Board at the University of Illinois at Urbana-Champaign with signed informed consent from all participants. The study is registered with United States National Institutes of Health http://ClinicalTrials.gov (ID NCT02523677).
Rights and permissions
About this article
Cite this article
Ehlers, D.K., Aguiñaga, S., Cosman, J. et al. The effects of physical activity and fatigue on cognitive performance in breast cancer survivors. Breast Cancer Res Treat 165, 699–707 (2017). https://doi.org/10.1007/s10549-017-4363-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4363-9