Abstract
Purpose
Atypical ductal hyperplasia (ADH) identified on percutaneous breast biopsy represents a high-risk lesion, upgrading to cancer with surgical excision in ~7–45.8% of cases. Routine excision is questioned due to potential overtreatment and cost. This study evaluates clinical, imaging, and histologic features to predict the risk of upgrade.
Methods
With IRB approval, a single-institution retrospective review was performed of patients who underwent surgical excision of ADH diagnosed by core biopsy from June 2005 to June 2013. We reviewed electronic medical records, breast imaging, and biopsy slides. Multiple imputation was used for missing data. Association of various features with cancer upgrade was assessed using logistic regression.
Results
Among 399 cases, the upgrade rate to cancer was 16.0%, (95% CI: 12.8–20.0%), with nine invasive cancers and 55 ductal carcinoma in situ (DCIS) only. Via a logistic regression approach, we defined a subgroup with low risk for upgrade: women whose biopsies showed no individual cell necrosis, and either a) 1 focus of ADH with ≥50% removal, or b) 2–3 foci with ≥90% removal. Cases meeting these criteria had an upgrade rate of 4.9% (95% CI: 1.0–8.9%), compared to 21.4% (16.4–26.3%) in cases that did not meet this low-risk definition.
Conclusions
ADH on core biopsy with low risk of upgrade to cancer is defined by lack of individual cell necrosis, number of foci of ADH, and percent of imaging lesion removed. If these findings are validated, women whose biopsies meet low-risk criteria might be considered for prevention therapy and surveillance without surgical excision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With increased utilization of mammographic screening and percutaneous needle biopsy of screen-detected lesions, the diagnosis of high-risk breast lesions has increased [1,2,3,4]. Atypical ductal hyperplasia (ADH) is identified in approximately 8–17% of all core needle breast biopsies [1, 5]. ADH is considered a high-risk breast lesion due to both a long-term increase in breast cancer risk [6,7,8,9,10] and also risk of “upgrade” to cancer at surgical excision in 7–45.8% of cases [2, 11,12,13,14,15,16,17].
Therefore, the standard of care is surgical excision when a core needle biopsy site demonstrates ADH. However, given that the majority of ADH cases diagnosed percutaneously are not upgraded to cancer, routine excision may represent overtreatment. Therefore, recent research efforts have attempted to identify factors associated with a low risk of cancer upgrade, in order to select women who may avoid surgical excision with minimal risk of missed cancer [18]. The goal of this study was to identify a subgroup of women with ADH on needle biopsy with low risk of upgrade to cancer, who may not require surgical excision of the biopsy site. Clinical, imaging, and histologic features of ADH were evaluated to characterize this low-risk subgroup.
Methods
Study population
Institutional Review Board was obtained. A combined search of our prospective breast surgery registry and institutional pathology database identified women with ADH by core needle biopsy, who were treated at Mayo Clinic Rochester from June 2005 to June 2013. Some data on pathology and radiology features were missing for patients whose core biopsy was performed elsewhere. To be included in the analysis, either core biopsy pathology slides or pre-biopsy radiographic images were required for review; remaining data elements were collected from clinical reports or were imputed. The majority (69%) had complete pre-excision data on radiographic and core biopsy pathology features by study team review of original imaging and biopsy slides; multiple imputation was used for missing data elements that could not be obtained from reports. Patients without surgical excision were excluded from multivariate modeling, but their follow-up data were collected and reported. Exclusion criteria included concurrent or prior diagnosis of ipsilateral breast cancer, multiple biopsy sites in the same breast (if final pathology outcomes for each distinct site could not be discriminated), or core biopsy performed elsewhere with neither images nor slides available for review.
Data collection
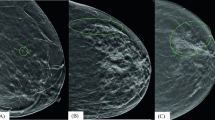
Subjects’ clinical features were abstracted from the electronic medical record. Imaging and histologic features were collected with blinding to the outcome of cancer upgrade. For each case, pre- and post-biopsy mammograms were reviewed by a single breast radiologist (RF) for the following imaging features: breast density (BIRADS), size of target lesion before biopsy; calcification features (extent, distribution, and morphology); size of biopsy needle; use of vacuum assistance; number of cores retrieved; and percentage of target lesion removed. Percentage of lesion removed was estimated visually by comparing pre- and post-biopsy mammograms and was grouped into categories of half or less removed (<50%), nearly all removed (≥90%), or majority removed (by default approximately 50–89%). Original slides from the core needle biopsy were reviewed by a single pathologist (SS) for the following histologic features: number of foci of ADH, individual cell necrosis (Fig. 1), micropapillary pattern, and presence of other lesions with possible high risk of upgrade [ALH (Atypical Lobular Hyperplasia), LCIS (Lobular Carcinoma in Situ), and FEA (Flat Epithelial Atypia)] [2, 18, 19]. In patients with core biopsy performed elsewhere, pathology features were collected from outside pathology reports, and study features not mentioned were treated as missing. Upgrade to cancer (DCIS or invasive cancer) was determined by final pathology reports from surgical excision.
Statistical approach
Multiple imputation was used for missing data. Specifically, twenty imputed datasets were created using the multiple imputation by chained equations approach implemented in the package mice for R statistical software [20,21,22,23]. Functions within this package were used to pool results across the 20 imputed datasets using the method described by Rubin [20]. The chained equations approach was chosen because of the mix of variable types (continuous, ordinal, nominal) that needed imputing; this approach allowed us to choose an appropriate model for each variable type. Continuous variables were imputed using the predictive mean matching method, ordinal variables using the linear discriminant analysis method, and nominal variables using the logistic method. Imputation was done under the assumption of missing at random because missingness was primarily due to core biopsies performed elsewhere. Variables included in the imputation model were upgrade outcome as well as covariates listed in Table 1 [21]. The model was then evaluated in both the imputed data as well as the complete case data, in order to assess the sensitivity of conclusions to imputation.
Association of potential predictors with the outcome of upgrade to cancer at excision was assessed with univariate and multivariate logistic regression. In developing a multivariate model, we followed the recommendation of ≥10 events per variable to avoid overfitting and to optimize generalizability to other settings [24, 25]. The multivariable logistic regression coefficients were used to estimate the predicted probability of upgrade for each factor combination, and those combinations with the lowest predicted probabilities (~5% or less) were identified as low risk of upgrade. Percentages with upgrade were estimated with 95% Wilson score confidence intervals for the complete case data; this was also estimated for the imputed data by pooling the intercept estimate from generalized linear models fit with the identity link across multiple imputations for imputed data. Analyses were performed using SAS (Version 9.3, SAS Institute Inc, Cary, NC) and R (Version 3.0.2, R Foundation for Statistical Computing, Vienna, Austria).
Results
Study population
We identified 485 women with 506 ADH lesions diagnosed by core biopsy between June 2005 and June 2013. Among the initial 506 lesions, 85 lesions in 80 patients were excluded for the following reasons: core biopsy elsewhere with neither mammograms nor pathology slides available (n = 37), subject had ipsilateral breast cancer previously (n = 16) or concurrent with the ADH biopsy (n = 31), and outcomes for multiple lesions in the same quadrant could not be distinguished (n = 1). An additional 22 lesions in 22 patients were not excised due to severe co-morbid conditions (n = 6), patient choice (n = 7), and reason not documented (n = 9). Among the 22 not excised, three died during follow-up (all from pre-existing conditions—cardiac/hepatic disease or melanoma), 13 (68%) had no follow-up documented, and six had a median mammographic follow-up of 3.7 years (range: 6 months–9 years) with no ipsilateral breast cancer. Thus, the final analysis dataset comprised 383 women with 399 biopsy sites excised at our institution.
Patient characteristics
Median age at breast biopsy was 58 years (range 36–86); median BMI was 27. First-degree family history of breast cancer was present in 29% of cases. Table 1 summarizes patient characteristics (clinical, radiological, and pathological), and association with upgrade.
Imaging and pathology findings
In 83% of cases, the initial clinical presentation was a screening mammographic abnormality; 10% presented with clinical symptoms (palpable mass or nipple discharge), and 7% were suspicious findings on supplemental screening modalities. Most cases (72%) demonstrated calcifications only, were biopsied with stereotactic guidance (74%), and vacuum assisted (86%) with 11G or larger needle (84%). Median number of cores per biopsy was 10 (range 1–24).
Regarding pathology findings in the core biopsies, the majority showed either one (38%), or 2–3 foci of ADH (43%). A minority of samples demonstrated other high-risk lesions (31%), had individual cell necrosis (28%), or micropapillary features (15%). Of 123 with additional high-risk lesions, 33 were ALH only, 74 FEA only, 1 LCIS only, 14 with both ALH and FEA, and 1 ALH and LCIS.
Upgrade rate and cancer characteristics
We found cancer at surgical excision in 64/399 cases for an overall upgrade rate of 16.0% (95% CI: 12.8–20.0%). Final pathology demonstrated nine invasive cancers (4 with DCIS) and 55 DCIS only. Of the nine invasive cancers, all were stage 1 invasive ductal (3 T1a, 5 T1b, and 1 T1c). Only one case was node positive with micrometastasis. All invasive cancers were ER+ , with one case also HER-2+.
Predictors of upgrade
Table 1 shows distributions of potential predictor variables and univariate associations with upgrade for cases with complete data. The strongest associations were for the estimated percent of lesion removed, the number of foci of ADH, and the presence of individual cell necrosis in the core biopsy specimen. Table 2 shows univariate analysis results after imputation for variables that had substantial missing data. Compared to the complete case data, the imputed data show a similar distribution for each variable and similar measures of univariate association with cancer upgrade (i.e., similar odds ratios for complete case data and imputed data), demonstrating the success of the imputation approach.
Multivariate model
To create a multivariate model for identifying a group with low risk of upgrade, our approach was to balance clinical simplicity (i.e., fewer variables) with good performance. While we identified several potentially important variables, with 64 events, the model should include ≤6 degrees of freedom to avoid overfitting and improve generalizability [24, 25]. A simple model including the three variables (5 degrees of freedom) with the strongest univariate associations is shown in Table 3. Each of the variables (individual cell necrosis, estimated percent of lesion removed, and number of foci of ADH) remained strongly significant in multivariate analysis. The median C-statistic for this model across imputations was 0.78. While we did not have an external validation sample available for this study, 10-fold cross-validation analyses showed continued good performance with a cross-validation C-statistic of 0.77.
Secondary approaches to model choice, including stepwise variable selection and also a model including all univariately significant variables, were explored but rejected due to concerns regarding multicollinearity of predictor variables, overfitting, and increased complexity for clinical use without substantial improvement in performance. Therefore, we opted for the original three-variable model as our final model (Fig. 2).
Low-risk definition
Using the model in Table 3 to estimate the predicted probability of upgrade for each factor combination, we identified the lowest risk categories (predicted probability ~5% or less) and developed a definition of low risk for upgrade, defined as women with (1) no individual cell necrosis, and (2) either 1 focus with ≥50% removal, or 2–3 foci with ≥90% removal. This represented an estimated 32% (95% CI: 27–38%) of the entire study set (using imputed data) with an upgrade risk of 4.9% (95% CI: 1.0–8.9%). In contrast, the remainder of the sample not meeting this definition of low risk had an estimated upgrade rate of 21.4% (95% CI: 16.4–26.3%). The upgrade risk findings from the imputed data (n = 20 datasets) are similar to the upgrade risk found when applying the low-risk criteria to the complete case data (N = 276), where 5/96 (5.2%) patients classified as low risk were upgraded to cancer at excision, compared to 39/180 (21.7%) patients classified as higher risk. This similarity between results for the imputed data and complete case data supports the validity of the imputation approach and findings.
Discussion
In this large single-institution study of ADH diagnosed on core needle biopsy, we found that the strongest factors affecting upgrade to cancer were percentage of lesion removed, number of foci of ADH, and the presence of individual cell necrosis in the core biopsy. With multivariate modeling, we identified a subgroup of women with ADH on core biopsy who have low risk (4.9%) of harboring cancer, in whom surgical excision might be avoided. Approximately one-third of the series met the low-risk criteria, defined as (1) no individual cell necrosis, and (2) either 1 focus with ≥50% removal, or 2–3 foci with ≥90% removal.
The overall upgrade rate in our large series was 16.0%, in the middle of the reported range in the literature (~7–37%) [2, 11,12,13,14,15,16]. Although we found many features associated with cancer upgrade by univariate analysis, several were redundant and not significant on multivariate analysis. The final three criteria in our model consist of radiographic and histologic factors that have all been associated with upgrade in prior studies. The radiographic percentage of the lesion removed has been associated with ADH upgrade to cancer in two prior studies [18, 26]. Nguyen et al. found that upgrade occurred in <3% of women who had >95% of the lesion removed, and Jackman et al. reported upgrade in only 8% of women who had 100% of the lesion removed. Increasing number of foci of ADH seen on core biopsy also has been associated with more frequent upgrade in several prior studies on this topic, using a cutoff of either >2 foci [2, 13, 18] or >3 foci [12, 15, 27]. The third factor in our model—individual cell necrosis—was suggested by two prior studies showing its association with cancer upgrade [18, 28].
Two prior multivariable predictive models have been developed to identify subsets of women with ADH who have a low risk of upgrade. In a paper by Ko et al., a model was created from 74 cases of ADH to predict upgrade, using the following features: age >50 years, palpable lesion, microcalcifications on mammogram, imaging size >15 mm, and multiple foci on core biopsy [17]. Applying this model to our dataset, we find that 13.2% of our subjects fit their defined low-risk criteria, and among these women, the actual upgrade rate was 2/36 (5.6%). In a more recent model from MD Anderson Cancer Center [18], 140 women with ADH were studied, creating low-risk criteria defined as calcifications only, >90% removal of calcifications, <3 foci of ADH, and no necrosis. Applying these low-risk criteria to our dataset, only 13.5% of women in our dataset would be classified as low risk, with 6% of them actually upgrading to cancer at surgical excision. Thus, both models successfully identify a subset with <10% risk of upgrade (~6% in each case), but both models apply to only ~13% of patients among the larger group of women who actually require surgical excision for ADH. One advantage of our model is that it may identify a larger proportion of women with ADH (32%) who have a low risk of upgrade (5%).
Our model and that of Nguyen et al. both include the presence of necrosis as a factor associated with increased risk of upgrade. Individual cell necrosis, also termed single-cell necrosis, likely represents the presence of apoptotic bodies [29]. Although the etiology of these cells is unclear, their presence may reflect alterations associated with neoplastic status, such as genetic instability or abnormal cell proliferation. As such, individual cell necrosis in histologically benign or atypical appearing proliferations may represent an early manifestation of malignancy. However, individual cell necrosis is neither a diagnostic criterion for ADH nor unique to ADH, as it is also a manifestation of normal, physiological cell turnover. Apoptosis can also be seen in columnar cell change or usual ductal hyperplasia, although it is more common in neoplastic lesions. We plan to further evaluate immunohistochemical stains to highlight apoptotic bodies and the utility of this approach in enhancing identification of individual cell necrosis in ADH lesions.
The current standard of care for core biopsies with ADH is to perform surgical excision, although NCCN guidelines do endorse omitting surgical excision in selected patients with other types of benign lesions (ALH, LCIS, FEA, papillomas, etc.) [30]. Due to overall higher upgrade risks for ADH in multiple published papers, ADH is not included in this list. However, we and others believe that some women with ADH are low risk and may safely avoid surgical excision. Furthermore, the small risk of upgrade to immediate cancer (usually DCIS) may be less clinically significant than their long-term breast cancer risk (usually invasive), which affects both breasts and is in the range of ~1–2% per year, also stratified by the number of foci of ADH [8, 31,32,33]. Thus for many women with ADH, addressing long-term breast cancer risk with prevention medications is the most important aspect of management, rather than surgical excision of the ADH site [32, 34,35,36,37].
For women with a low risk of upgrade, short-term radiographic follow-up should be adequate to detect progression. In the uncommon situation that an early malignancy is present at the ADH core biopsy site, prevention medications would likely be effective at treating it. This is supported by the fact that all the upgraded lesions in our study were ER+, with the majority being in situ disease (also consistent with prior studies), which has been shown to respond to endocrine therapy [38]. In situations where no excision is performed, short-term follow-up imaging would appear reasonable to establish a new baseline and would identify the unlikely event of radiographic progression. In fact, this has been confirmed in a recent paper by Menen et al., where 125 women with low-risk ADH (using criteria of Nguyen et al. above) were observed without surgical excision [39]. With a median follow-up of 3 years (and chemoprevention use by 23% of women), only seven breast cancers occurred (5.6%).
A major strength of our study is the large sample size, which allowed for multivariate analysis. Of the multiple prior studies on this topic, most have substantially smaller numbers of women with ADH who underwent surgical excision, with evaluation of a limited number of variables. The next largest sample size previously reported with multivariate analysis consists of 422 ADH core biopsies that were surgically excised [40]. In that report, 30% of women in the sample had no features associated with upgrade, yet carcinoma was identified in 17% of these low-risk women, leading the authors to conclude that a subgroup could not be identified with risk low enough to avoid excision. However, they did not evaluate several of the features that were important in our and others’ models (percentage of lesion removed and number of foci of ADH). With a larger sample size and multivariate analysis, we have identified features of a low-risk subgroup that may be more inclusive compared to prior models. Furthermore, the fact that our final model includes radiographic and histologic features that were previously associated with upgrade in both the Ko and Nguyen studies lends support to the likely validity of these low-risk features [17, 18].
Limitations of our study include the retrospective design which has inherent selection bias and some missing data. Selection bias is minimized by our routine clinical practice of performing surgical excision of ADH identified on core needle biopsy. We included some subjects who had imaging but not needle biopsy tissues available for re-review, which increased our sample size and power but resulted in missing data and imputation. However, imputation is an acceptable and established method, and consistent findings across both the complete case and imputed data support the robustness of the imputation approach [20, 21]. Although the features most strongly associated with upgrade are not currently standard components of radiology and pathology reports, they have all been proposed in prior studies and their utility is being increasingly recognized based on accumulating publications on this topic.
Conclusions
In summary, we describe a model incorporating pathology and imaging findings that identified a group of women diagnosed with ADH on percutaneous needle biopsy at low risk (<5%) of upgrade to cancer. However, prior to initiating use of low-risk criteria in clinical practice to avoid surgical excision, validation is desirable in other retrospective (and ideally prospective) cohorts. Such validation could lead to a new clinical management paradigm for women diagnosed with ADH on core needle biopsy.
References
McGhan LJ, Pockaj BA, Wasif N, Giurescu ME, McCullough AE, Gray RJ (2012) Atypical ductal hyperplasia on core biopsy: an automatic trigger for excisional biopsy? Ann Surg Oncol 19(10):3264–3269. doi:10.1245/s10434-012-2575-0
Wagoner MJ, Laronga C, Acs G (2009) Extent and histologic pattern of atypical ductal hyperplasia present on core needle biopsy specimens of the breast can predict ductal carcinoma in situ in subsequent excision. Am J Clin Pathol 131(1):112–121. doi:10.1309/AJCPGHEJ2R8UYFGP
Bleyer A, Welch HG (2012) Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med 367(21):1998–2005. doi:10.1056/NEJMoa1206809
Neal CH, Coletti MC, Joe A, Jeffries DO, Helvie MA (2013) Does digital mammography increase detection of high-risk breast lesions presenting as calcifications? AJR Am J Roentgenol 201(5):1148–1154. doi:10.2214/AJR.12.10195
Pearlman MD, Griffin JL (2010) Benign breast disease. Obstet Gynecol 116(3):747–758. doi:10.1097/AOG.0b013e3181ee9fc7
Dupont WD, Page DL (1985) Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med 312(3):146–151
Hartmann LC, Sellers TA, Frost MH, Lingle WL, Degnim AC, Ghosh K, Vierkant RA, Maloney SD, Pankratz VS, Hillman DW, Suman VJ, Johnson J, Blake C, Tlsty T, Vachon CM, Melton LJ 3rd, Visscher DW (2005) Benign breast disease and the risk of breast cancer. N Engl J Med 353(3):229–237
Hartmann LC, Radisky DC, Frost MH, Santen RJ, Vierkant RA, Benetti LL, Tarabishy Y, Ghosh K, Visscher DW, Degnim AC (2014) Understanding the premalignant potential of atypical hyperplasia through its natural history: a longitudinal cohort study. Cancer Prev Res 7(2):211–217. doi:10.1158/1940-6207.CAPR-13-0222
Tice JA, O’Meara ES, Weaver DL, Vachon C, Ballard-Barbash R, Kerlikowske K (2013) Benign breast disease, mammographic breast density, and the risk of breast cancer. J Natl Cancer Inst 105(14):1043–1049. doi:10.1093/jnci/djt124
Jacobs TW, Byrne C, Colditz G, Connolly JL, Schnitt SJ (2001) Pathologic features of breast cancers in women with previous benign breast disease. Am J Clin Pathol 115(3):362–369. doi:10.1309/UP07-K3KD-25NL-D3M8
Degnim AC, King TA (2013) Surgical management of high-risk breast lesions. Surg clin North Am 93(2):329–340. doi:10.1016/j.suc.2012.12.005
Allison KH, Eby PR, Kohr J, DeMartini WB, Lehman CD (2011) Atypical ductal hyperplasia on vacuum-assisted breast biopsy: suspicion for ductal carcinoma in situ can stratify patients at high risk for upgrade. Hum Pathol 42(1):41–50. doi:10.1016/j.humpath.2010.06.011
Forgeard C, Benchaib M, Guerin N, Thiesse P, Mignotte H, Faure C, Clement-Chassagne C, Treilleux I (2008) Is surgical biopsy mandatory in case of atypical ductal hyperplasia on 11-gauge core needle biopsy? A retrospective study of 300 patients. Am J Surg 196(3):339–345. doi:10.1016/j.amjsurg.2007.07.038
Ely KA, Carter BA, Jensen RA, Simpson JF, Page DL (2001) Core biopsy of the breast with atypical ductal hyperplasia: a probabilistic approach to reporting. Am J Surg Pathol 25(8):1017–1021
Sneige N, Lim SC, Whitman GJ, Krishnamurthy S, Sahin AA, Smith TL, Stelling CB (2003) Atypical ductal hyperplasia diagnosis by directional vacuum-assisted stereotactic biopsy of breast microcalcifications. Considerations for surgical excision. Am J Clin Pathol 119(2):248–253. doi:10.1309/0GYV-4F2L-LJAV-4GFN
Kim J, Han W, Go EY, Moon HG, Ahn SK, Shin HC, You JM, Chang JM, Cho N, Moon WK, Park IA, Noh DY (2012) Validation of a scoring system for predicting malignancy in patients diagnosed with atypical ductal hyperplasia using an ultrasound-guided core needle biopsy. J Breast Cancer 15(4):407–411. doi:10.4048/jbc.2012.15.4.407
Ko E, Han W, Lee JW, Cho J, Kim EK, Jung SY, Kang MJ, Moon WK, Park IA, Kim SW, Kim KS, Lee ES, Min KH, Kim SW, Noh DY (2008) Scoring system for predicting malignancy in patients diagnosed with atypical ductal hyperplasia at ultrasound-guided core needle biopsy. Breast Cancer Res Treat 112(1):189–195. doi:10.1007/s10549-007-9824-0
Nguyen CV, Albarracin CT, Whitman GJ, Lopez A, Sneige N (2011) Atypical ductal hyperplasia in directional vacuum-assisted biopsy of breast microcalcifications: considerations for surgical excision. Ann Surg Oncol 18(3):752–761. doi:10.1245/s10434-010-1127-8
Kunju LP, Kleer CG (2007) Significance of flat epithelial atypia on mammotome core needle biopsy: should it be excised? Hum Pathol 38(1):35–41. doi:10.1016/j.humpath.2006.08.008
Rubin DB (1987) Multiple imputations for nonresponse in surveys. Wiley, New York
Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR (2009) Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338:b2393. doi:10.1136/bmj.b2393
van Buuren S (2007) Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res 16(3):219–242. doi:10.1177/0962280206074463
van Buuren S, Groothuis-Oudshoorn K (2011) Mice: multivariate imputation by chained equations in R. J Stat Softw 45(3):1–67
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Harrell FE (2001) Regression modeling strategies: with applications to linear models, logistic regression, and survival. Springer, New York
Jackman RJ, Birdwell RL, Ikeda DM (2002) Atypical ductal hyperplasia: can some lesions be defined as probably benign after stereotactic 11-gauge vacuum-assisted biopsy, eliminating the recommendation for surgical excision? Radiology 224(2):548–554
Kohr JR, Eby PR, Allison KH, DeMartini WB, Gutierrez RL, Peacock S, Lehman CD (2010) Risk of upgrade of atypical ductal hyperplasia after stereotactic breast biopsy: effects of number of foci and complete removal of calcifications. Radiology 255(3):723–730. doi:10.1148/radiol.09091406
Yeh IT, Dimitrov D, Otto P, Miller AR, Kahlenberg MS, Cruz A (2003) Pathologic review of atypical hyperplasia identified by image-guided breast needle core biopsy. Correlation with excision specimen. Arch Pathol Lab Med 127(1):49–54. doi:10.1043/0003-9985(2003)127<49:PROAHI>2.0.CO;2
Kerr JF, Wyllie AH, Currie AR (1972) Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br J Cancer 26(4):239–257
NCCN (2016) National Comprehensive Cancer Network Clinical Guidelines, Breast Cancer Risk Reduction, v1,2916. http://www.nccn.org/professionals/physician_gls/pdf/breast_risk.pdf. Accessed 14 Dec 2016
Degnim AC, Visscher DW, Berman HK, Frost MH, Sellers TA, Vierkant RA, Maloney SD, Pankratz VS, de Groen PC, Lingle WL, Ghosh K, Penheiter L, Tlsty T, Melton LJ 3rd, Reynolds CA, Hartmann LC (2007) Stratification of breast cancer risk in women with atypia: a Mayo cohort study. J Clin Oncol 25(19):2671–2677. doi:10.1200/JCO.2006.09.0217
Coopey SB, Mazzola E, Buckley JM, Sharko J, Belli AK, Kim EM, Polubriaginof F, Parmigiani G, Garber JE, Smith BL, Gadd MA, Specht MC, Guidi AJ, Roche CA, Hughes KS (2012) The role of chemoprevention in modifying the risk of breast cancer in women with atypical breast lesions. Breast Cancer Res Treat 136(3):627–633. doi:10.1007/s10549-012-2318-8
Degnim AC, Dupont WD, Radisky DC, Vierkant RA, Frank RD, Frost MH, Winham SJ, Sanders ME, Smith JR, Page DL, Hoskin TL, Vachon CM, Ghosh K, Hieken TJ, Denison LA, Carter JM, Hartmann LC, Visscher DW (2016) Extent of atypical hyperplasia stratifies breast cancer risk in 2 independent cohorts of women. Cancer 122(19):2971–2978. doi:10.1002/cncr.30153
Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, Bevers TB, Kavanah MT, Atkins JN, Margolese RG, Runowicz CD, James JM, Ford LG, Wolmark N (2005) Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst 97(22):1652–1662. doi:10.1093/jnci/dji372
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, Bevers TB, Fehrenbacher L, Pajon ER, Wade JL 3rd, Robidoux A, Margolese RG, James J, Runowicz CD, Ganz PA, Reis SE, McCaskill-Stevens W, Ford LG, Jordan VC, Wolmark N (2010) Update of the national surgical adjuvant breast and bowel project study of tamoxifen and raloxifene (STAR) P-2 trial: preventing breast cancer. Cancer Prev Res 3(6):696–706. doi:10.1158/1940-6207.CAPR-10-0076
Goss PE, Ingle JN, Ales-Martinez JE, Cheung AM, Chlebowski RT, Wactawski-Wende J, McTiernan A, Robbins J, Johnson KC, Martin LW, Winquist E, Sarto GE, Garber JE, Fabian CJ, Pujol P, Maunsell E, Farmer P, Gelmon KA, Tu D, Richardson H (2011) Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med 364(25):2381–2391. doi:10.1056/NEJMoa1103507
Cuzick J, Sestak I, Forbes JF, Dowsett M, Knox J, Cawthorn S, Saunders C, Roche N, Mansel RE, von Minckwitz G, Bonanni B, Palva T, Howell A (2014) Anastrozole for prevention of breast cancer in high-risk postmenopausal women (IBIS-II): an international, double-blind, randomised placebo-controlled trial. Lancet 383(9922):1041–1048. doi:10.1016/S0140-6736(13)62292-8
Chen YY, DeVries S, Anderson J, Lessing J, Swain R, Chin K, Shim V, Esserman LJ, Waldman FM, Hwang ES (2009) Pathologic and biologic response to preoperative endocrine therapy in patients with ER-positive ductal carcinoma in situ. BMC Cancer 9:285. doi:10.1186/1471-2407-9-285
Menen RS, Ganesan N, Bevers T, Ying J, Coyne R, Lane D, Albarracin C, Bedrosian I (2017) Long-term safety of observation in selected women following core biopsy diagnosis of atypical ductal hyperplasia. Ann Surg Oncol. 24(1):70–76. doi: 10.1245/s10434-016-5512-9. Epub 2016 Aug 29. doi:10.1245/s10434-016-5512-9
Deshaies I, Provencher L, Jacob S, Cote G, Robert J, Desbiens C, Poirier B, Hogue JC, Vachon E, Diorio C (2011) Factors associated with upgrading to malignancy at surgery of atypical ductal hyperplasia diagnosed on core biopsy. Breast 20(1):50–55. doi:10.1016/j.breast.2010.06.004
Acknowledgements
The authors would like to thank Marilyn Churchward for assistance with manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflict of interest disclosures from the authors.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Peña, A., Shah, S.S., Fazzio, R.T. et al. Multivariate model to identify women at low risk of cancer upgrade after a core needle biopsy diagnosis of atypical ductal hyperplasia. Breast Cancer Res Treat 164, 295–304 (2017). https://doi.org/10.1007/s10549-017-4253-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4253-1