Abstract
Purpose
Basal marker expression in triple-negative breast cancers identifies basal-like tumours, and thus separates the TN group into two prognostic groups. However, the expression and prognostic significance of basal markers in luminal breast cancers are poorly described. The aim of this study was to investigate the expression and prognostic value of basal markers (CK5, CK14 and EGFR) in luminal breast cancer.
Methods
A total of 1423 formalin-fixed, paraffin-embedded breast cancer tumours from a well-characterized cohort of Norwegian women, previously reclassified into molecular subtypes using IHC and ISH, were included in the study. For the present study, tumours expressing at least one of the basal markers CK5, CK14 or EGFR were defined as basal marker positive. Cumulative incidence of death from breast cancer and hazard ratio analyses were used to assess prognosis according to basal marker expression.
Results and conclusion
In total, 470 cases (33.0%) were basal marker positive. A higher proportion of the basal marker-positive tumours were of histopathological grade 3 compared to basal marker negative. For hormone receptor-positive, HER2-negative cases, we found better prognosis for basal marker-positive breast cancer compared to basal marker negative. For all subtypes combined, poorer prognosis for basal marker-negative cases was found in histopathological grade 2 tumours but not among grade 1 and 3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Classification of breast cancer into molecular subtypes based on gene expression patterns [23] has improved our understanding of the heterogeneity of breast cancer. Immunohistochemistry (IHC) and in situ hybridization (ISH) are often used as surrogates for gene expression analyses [5, 10, 27] and to a great extent reflect the genetic subtypes [6].
Luminal (oestrogen and/or progesterone receptor positive) tumours can be further divided into three subtypes based on their expression of Human epidermal growth factor receptor 2 (HER2) and expression of the proliferation marker Ki67. Non-luminal tumours can be classified into the HER2 subtype and the triple-negative (TN) subtype. Based on expression of basal markers, TN can be further subdivided into the basal phenotype and the non-basal or five-negative phenotype [5, 10, 15, 22]. Basal marker expression in TN breast cancers has been extensively studied. However, the prognostic value of basal markers in luminal breast cancer is still unresolved.
Luminal breast cancers are generally associated with a better prognosis compared to non-luminal. The Luminal A subtype has the best prognosis followed by the other luminal subtypes [5, 10, 11]. However, studies of long-term survival have shown that luminal breast cancers can recur up to decades after primary diagnosis. Luminal tumours are heterogeneous, and there is a need for further classification into prognostic groups in order to differentiate treatment and follow-up. The aim of this study was to investigate the expression and prognostic value of three basal markers [cytokeratin 5 (CK5), cytokeratin 14 (CK14) and epithelial growth factor receptor 1 (EGFR)] in luminal breast cancer tumours from a well-characterized cohort of Norwegian women with long-term follow-up.
Materials and methods
Study population
The study population has been described in detail previously [10, 14, 18, 32]. The patients are from two population-based surveys conducted in Nord-Trøndelag (NT) County in Norway, and the participants were born between 1886 and 1977. The women were followed for breast cancer occurrence, and, in total, formalin-fixed, paraffin-embedded (FFPE) tissue was available from 1423 cases. All cases were previously reclassified into molecular subtypes based on surrogate markers according to the algorithm shown in Fig. 1 [10, 31]. After linkage with the Cause of Death Registry of Norway and the Norwegian Cancer Registry, survival data were generated.
Algorithm for molecular subtyping based on surrogate markers (Engstrom et al. [10])
Specimen characteristics
Haematoxylin–erythrosine–saffron (HES)-stained full-face sections from all tumours were already classified into histopathological type and grade according to current guidelines [9, 19]. Methods for tissue microarray (TMA) construction, IHC and ISH are described elsewhere [10, 31]. Briefly, TMAs comprising three 1-mm-diameter tissue cores from all suitable cases were made and 4 μm sections were cut and stained. In total, 118 cases comprised only core biopsies or small tissue fragments unsuitable for TMA construction. From these, serial sections were made. IHC was done to assess ER, PR, Ki67, CK5, EGFR and HER2, and ISH was done for HER2 gene status. For the present study, IHC for CK14 was added. Two researchers assessed all IHC markers independently. Discordant results were discussed and consensus reached.
Assay methods
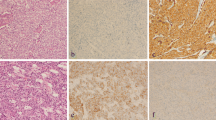
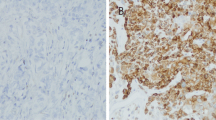
IHC for detection of CK14 was carried out according to the manufacturer’s guidelines (Dako, Glostrup, Denmark). Sections were mounted on Superfrost + glass slides, dried at 37 °C overnight and stored at −20 °C. Slides were heated at 60 °C for 2 h and pretreated in a PT Link pretreatment module for tissue specimens (Dako) with buffer (high pH target retrieval solution K8004) at 97 °C for 20 min. before staining. Mouse monoclonal antibody CK14 was applied (clone LL002, concentration 36 mg/l, dilution 1:20). Dako REAL™ EnVision™ detection system was used with peroxidase/diaminobenzidine (DAB)+, rabbit/mouse, code K5007, for visualization.
Scoring and reporting
Assessment and cut-off levels for all markers except CK14 have been explained previously [10, 32]. A staining index (SI) for CK14 was calculated as staining intensity multiplied by the proportion of cells showing positive staining. Cytoplasmic staining intensity was graded as 0 (no staining), 1 (weak), 2 (moderate) and 3 (strong). The proportion of positively stained cells was scored as 1 (<10%), 2 (10–50%) and 3 (>50%). Cases with SI 0–1 were considered negative and cases with SI 2–9 were regarded as positive. Basal marker-positive (BM+) cases were defined as positive for at least one of the basal markers CK5, CK14 and EGFR. The REMARK recommendations for tumour marker studies were followed [20].
Statistical analyses
All women were followed for breast cancer occurrence and censored at the time of death or emigration. End of follow-up was December 31st, 2010 for the oldest cohort and December 31st, 2013 for the youngest. Cumulative incidence of breast cancer death was calculated, and deaths from other causes were treated as competing events. Cumulative incidence curves were compared using Gray′s test. Cox proportional hazards models were used to compare the risk of death from breast cancer according to BM status, calculating hazard ratios (HR) with 95% confidence intervals (CI). Adjustments were made for age; stage (in five categories: stage I–IV and unknown) at diagnosis according the data from the Cancer Registry [13]; and histopathological grade. Stata version 13.1 (Stata Corp., College Station, TX, USA) was used for the statistical analyses.
Ethics
The study was approved by the Regional Committee for Medical and Health Sciences Research Ethics, and dispensation from the requirement of patient consent was granted (REK, Midt-Norge, ref. nr: 836/2009).
Results
Descriptive statistics
Table 1 shows the clinicopathological characteristics of all cases. Mean age at diagnosis was 67.3 years. Women with BM+ tumours were younger than women with BM− tumours (62.7 vs. 69.6 years of age). BM+ tumours were more often of histopathological grade 3 (44.2 vs. 26.1%). The proportion of invasive lobular carcinoma was lower for BM+ cases (4.7 vs. 16.2%). Of the 1423 cases included in the study, 1194 were luminal and 229 were non-luminal (Table 2). Of the luminal cases, 324 (27.1%) were BM+. Table 3 shows the number of basal marker-positive cases for each marker and in combination.
Survival analyses
Figure 2a–c and Table 4 show cumulative incidence of death from breast cancer according to BM status for all breast cancer cases and for luminal and non-luminal cases separately. For all cases, the curves overlap the first eight years (Fig. 2a), and the cumulative risk of death after 5 years of follow-up was 19.2% (95% CI 15.9–23.1) for BM+ and 19.1% (95% CI 16.7–21.7) for BM−. However, the corresponding risks of death after 15 years of follow-up were 28.4% (95% CI 24.2–33.2) for BM+ and 33.6% (95% CI 30.4–37.1) for BM−.
BM− luminal tumours had a poorer prognosis than BM+ luminal tumours (Gray’s test: p = 0.003) (Fig. 2b). The cumulative risk of death from BM+ luminal breast cancer was 11.5% (95% CI 8.4–15.5) after 5 years of follow-up and 21.2% (95% CI 16.6–26.9) after 15 years. The corresponding risks for BM− luminal cases were 17.2% (95% CI 14.8–19.9) and 32.3 (95% CI 28.9–35.9), respectively. For all non-luminal cases combined, no difference in prognosis was seen according to BM status (Gray’s test: p = 0.69) (Fig. 2c).
Figure 3a–c and Table 5 show cumulative incidence of death from breast cancer according to BM status for all three luminal subtypes separately. For Luminal A and Luminal B (HER2−), BM+ cases had better prognosis compared to BM− (Gray’s test: p = 0.003 and p = 0.04, respectively) (Fig. 3a–b). For Luminal B (HER2+), no difference was seen according to BM status (Gray’s test: p = 0.79) (Fig. 3c).
Figure 4 is a summary and relative comparison of Figs. 3a–c showing cumulative risks of death from breast cancer for all luminal subtypes according to BM status. There was no clear difference in prognosis for Luminal A BM− compared to Luminal B (HER2−) BM+. The cumulative risk of death from Luminal A BM− breast cancer was 13.4% (95% CI 10.7–16.6) and 28.6% (95% CI 24.4–33.4) after 5 and 15 years of follow-up, respectively. The corresponding cumulative risk of death for Luminal B (HER2−) BM+ was 11.3% (95% CI 6.6–19.1) and 25.4% (95% CI 17.2–36.7).
Figures 5 a–c and Table 6 show results from survival analyses for BM+ and BM− for histopathological grades 1, 2 and 3 separately. For grade 2 tumours, the prognosis was significantly poorer for BM− compared to BM+ (Gray’s test: p = 0.0004) (Fig. 5b). For histopathological grades 1 and 3 separately, we found no clear differences in prognosis according to BM status.
Cox regression analysis was done to compare rates of breast cancer death according to BM status for all cases combined, for all luminal cases combined and for each luminal subtype separately (Table 7). Comparing BM+ and BM− for all breast cancer cases irrespective of subtypes, there was a tendency toward better prognosis for BM+. However, there was no difference after adjusting for age. The first ten years after diagnosis, there were no clear differences in prognosis, but from ten years and onwards, BM− had poorer prognosis compared to BM+ [hazard ratio (HR) 1.98 (95% CI 1.09–3.63)] (Table 7). For all luminal cases combined, BM+ had better prognosis compared to BM− [HR 1.71 (95% CI 1.30–2.25)]. Luminal A BM− had higher risk of death from breast cancer compared to Luminal A BM+ [HR 2.16 (95% CI 1.39–3.33)]. Corresponding results were found for Luminal B (HER2−). However, HRs were attenuated after adjustment for age, stage and histopathological grade, where age had the greatest attenuating effect.
Discussion
We have studied the expression and prognostic impact of basal markers CK5, CK14 and EGFR in a well-characterized cohort of women with breast cancer. The cohort comprises 1423 breast cancer patients with long-term follow-up. We have studied risk of death from breast cancer according to BM status for all breast cancer cases combined, for all luminal cases combined and for each luminal subtype separately. We found better prognosis for BM-positive luminal breast cancer compared to BM-negative. This result was restricted to the Luminal A and Luminal B (HER2−) subtypes. For Luminal B (HER2+) tumours, we found no clear differences according to BM status.
HRs were weakened after adjustment for known prognostic markers (Table 7). Adjusting for age had the greatest influence on the results. Nevertheless, the tendency toward better prognosis for BM+ cases compared to BM− remained. When adjusting for stage and histopathological grade, only minor changes were seen. The mean age of the women with BM+ tumours was lower compared to the women with BM− tumours (62.7 vs. 69.6 years of age). The time of diagnosis in this cohort spans over several decades and treatment would have been largely determined by age at diagnosis and time of diagnosis. A high proportion of women in our cohort received no therapy after surgery, but new treatment modalities were gradually introduced in the latter part of the study period. Previously, our group has shown improved prognoses for Luminal A, Luminal B (HER2−) and Basal phenotype diagnosed after 1995 compared to cases diagnosed before 1995 [31], probably partly due to the implementation of modern treatment protocols. These changes over time may have influenced the results.
In the present study, basal marker expression had prognostic value for histopathological grade 2 tumours but not for grade 1 and 3. Grade 2 tumours represent a heterogeneous group with diverging risk of recurrence and breast cancer death [8, 10, 25]. Therefore, further subclassification of grade 2 tumours is of interest. However, even in a large study like this, some groups were too small for further subclassification, and in some of the results presented here confidence intervals were broad, probably due to low numbers of cases.
The expression and prognostic impact of basal markers in luminal breast cancer have not been widely studied. Previous studies by Blows et al. [5] and Sung et al. [27] had diverging results regarding prognosis compared to ours. In order to compare with Blows et al., we analysed prognosis based on overall survival (data not shown), but the results did not change. Sung et al. found that basal-positive [(CK5+ or CK5/6+) and/or EGFR+] Luminal A tumours were smaller, had lower histopathological grade and more often tended to be lymph node-negative compared to basal-negative tumours. For all cancer subtypes combined, we found a higher proportion of histopathological grade 3 tumours among BM+ compared to BM− (Table 1). However, within the Luminal A subtype, we found similar results to Sung et al. with regard to tumour size, histopathological grade and lymph node status (data not shown).
In addition to the high number of cases and long follow-up, a further strength of the present study is that all laboratory tests were carried out in the same laboratory, with the same technical and scientific personnel, using the same IHC markers and algorithm in all cases. Histopathological diagnoses were revised, and assessment of IHC markers was performed by two researchers independently. However, in a cohort such as this, preanalytical conditions may have varied, possibly influencing the results. Furthermore, as discussed above, the patients in the study may have received differing adjuvant treatment, if any, due to time period and age at diagnosis.
Basal markers are often focally expressed in breast cancer [17, 30]. TMA is a high throughput method enabling analyses of tumour tissue from a high number of cases under the same conditions [6, 16, 24]. However, the method may have limitations regarding representativity and false-negative cases cannot be excluded. In addition, consensus-based cut-off levels for basal markers are not established. The results must be interpreted in light of these factors.
In previous studies of prognosis for molecular subtypes based on surrogate markers, we found a poorer prognosis for HER2+ and TN subtypes the first five years after diagnosis. For those who survived five years, the prognosis did not differ between the subtypes [10, 32]. We also found a steadily declining survival for the luminal HER2− subtypes throughout the follow-up period. Also in the present study, the period of time from diagnosis has impact on prognosis. As shown in Fig. 2a, the prognostic effect of basal markers may change with time from breast cancer diagnosis. Tischkowitz et al. showed that the prognostic value of different immunohistochemical markers varied with time after diagnosis and that after 10 years, basal markers might be of higher prognostic value than hormone receptors and HER2 [29]. This, along with the results in the present study, confirms that long-term follow-up is necessary to discover prognostic differences in breast cancer.
A number of studies have shown poorer prognosis for BM + TN breast cancer [5, 7, 29]. There are few published studies on the prognostic impact of BM in luminal breast cancer, but our results indicate a better prognosis for BM+ HER2− luminal tumours. Different prognostic markers and combinations of markers may have differing impact in the various subtypes of breast cancer. The expression of different sets of markers may reflect different routes of cell differentiation [21]. Interaction between, and mutual impact of the various prognostic markers remain to be elucidated. The prognostic impact of basal markers may differ depending on the presence or absence of hormone receptors or HER2 status.
Basal breast cancer is not clearly defined and a number of basal markers have been used to define this subtype [1, 3, 30, 33]. CKs are cytoplasmic proteins important for the cytoskeleton of eukaryotic cells and are, to a certain extent, differentially expressed in basal and luminal epithelial cells [26]. EGFR is a tyrosine kinase receptor, and activation plays a central role in regulation of proliferation, growth and cell survival. Overexpression of EGFR in epithelial tumours may lead to aggressive growth and invasion, and ultimately, a poorer prognosis [12, 28]. CK5 or CK5/6 are among the most widely used basal markers [3, 5]. EGFR is upregulated in the basal-like subtype of breast cancer [23] and is considered useful in combination with basal markers [22]. We chose CK5 instead of CK5/6 to identify basal-like phenotypes due to higher sensitivity [4]. In our material, there were few EGFR-positive cases compared to other studies [28] and therefore its value was limited. We found that three cases in the non-luminal subtype, 5NP, expressed CK14. Among luminal tumours, CK14 was the only positive basal marker in 88 cases. Other basal markers such as CK17, vimentin, nestin and p63 [1, 2] could have increased the number of tumours with basal traits in this material.
In conclusion, we found better prognosis for basal marker-positive breast cancer (defined as positive for CK5 and/or CK14 and/or EGFR) compared to basal marker-negative cases. This finding was restricted to hormone receptor-positive, HER2-negative cases. For all subtypes combined, we found better prognosis for basal marker-positive cases in histopathological grade 2 tumours but not in grades 1 and 3. Time from diagnosis may be crucial for the prognostic value of basal markers and in the present study, the differences were most apparent from ten years after diagnosis. There are few studies of the prognostic value of basal markers in luminal subtypes. The results are diverging and further studies are necessary.
References
Alshareeda AT, Soria D, Garibaldi JM, Rakha E, Nolan C, Ellis IO, Green AR (2013) Characteristics of basal cytokeratin expression in breast cancer. Breast Cancer Res Treat 139:23–37. doi:10.1007/s10549-013-2518-x
Asleh-Aburaya K, Sheffield BS, Kos Z, Won JR, Wang XQ, Gao D, Wolber R, Gilks CB, Bernard PS, Chia SK, Nielsen TO (2017) Basal biomarkers nestin and INPP4b identify intrinsic subtypes accurately in breast cancers that are weakly positive for oestrogen receptor. Histopathology 70:185–194. doi:10.1111/his.13038
Badve S, Dabbs DJ, Schnitt SJ, Baehner FL, Decker T, Eusebi V, Fox SB, Ichihara S, Jacquemier J, Lakhani SR, Palacios J, Rakha EA, Richardson AL, Schmitt FC, Tan PH, Tse GM, Weigelt B, Ellis IO, Reis-Filho JS (2011) Basal-like and triple-negative breast cancers: a critical review with an emphasis on the implications for pathologists and oncologists. Mod Pathol 24:157–167. doi:10.1038/modpathol.2010.200
Bhargava R, Beriwal S, McManus K, Dabbs DJ (2008) CK5 is more sensitive than CK5/6 in identifying the “basal-like” phenotype of breast carcinoma. Am J Clin Pathol 130:724–730. doi:10.1309/ajcp3kff1ltywqiy
Blows FM, Driver KE, Schmidt MK, Broeks A, van Leeuwen FE, Wesseling J, Cheang MC, Gelmon K, Nielsen TO, Blomqvist C, Heikkila P, Heikkinen T, Nevanlinna H, Akslen LA, Begin LR, Foulkes WD, Couch FJ, Wang X, Cafourek V, Olson JE, Baglietto L, Giles GG, Severi G, McLean CA, Southey MC, Rakha E, Green AR, Ellis IO, Sherman ME, Lissowska J, Anderson WF, Cox A, Cross SS, Reed MW, Provenzano E, Dawson SJ, Dunning AM, Humphreys M, Easton DF, Garcia-Closas M, Caldas C, Pharoah PD, Huntsman D (2010) Subtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10,159 cases from 12 studies. PLoS Med 7:e1000279. doi:10.1371/journal.pmed.1000279
Callagy G, Cattaneo E, Daigo Y, Happerfield L, Bobrow LG, Pharoah PD, Caldas C (2003) Molecular classification of breast carcinomas using tissue microarrays. Diagn Mol Pathol 12:27–34
Cheang MC, Voduc D, Bajdik C, Leung S, McKinney S, Chia SK, Perou CM, Nielsen TO (2008) Basal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clin Cancer Res 14:1368–1376. doi:10.1158/1078-0432.ccr-07-1658
Chowdhury N (2011) Histopathological and genomic grading provide complementary prognostic information in breast cancer: a study on publicly available datasets. Patholog Res Int 2011:890938. doi:10.4061/2011/890938
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19:403–410
Engstrom MJ, Opdahl S, Hagen AI, Romundstad PR, Akslen LA, Haugen OA, Vatten LJ, Bofin AM (2013) Molecular subtypes, histopathological grade and survival in a historic cohort of breast cancer patients. Breast Cancer Res Treat. doi:10.1007/s10549-013-2647-2
Hennigs A, Riedel F, Gondos A, Sinn P, Schirmacher P, Marme F, Jager D, Kauczor HU, Stieber A, Lindel K, Debus J, Golatta M, Schutz F, Sohn C, Heil J, Schneeweiss A (2016) Prognosis of breast cancer molecular subtypes in routine clinical care: a large prospective cohort study. BMC Cancer 16:734. doi:10.1186/s12885-016-2766-3
Herbst RS (2004) Review of epidermal growth factor receptor biology. Int J Radiat Oncol Biol Phys 59:21–26. doi:10.1016/j.ijrobp.2003.11.041
Hofvind S, Lee CI, Elmore JG (2012) Stage-specific breast cancer incidence rates among participants and non-participants of a population-based mammographic screening program. Breast Cancer Res Treat 135:291–299. doi:10.1007/s10549-012-2162-x
Holmen JMK, Kruger Ø, Langhammer A, Holmen TL, Bratberg GH et al (2003) The Nord-Trøndelag health study 1995–97 (HUNT 2): objectives, contents, methods and participation. Norsk Epidemiologi 13:19–32
Ishitha G, Manipadam MT, Backianathan S, Chacko RT, Abraham DT, Jacob PM (2016) Clinicopathological study of triple negative breast cancers. J Clin Diagn Res. doi:10.7860/JCDR/2016/20475.8539
Kononen J, Bubendorf L, Kallioniemi A, Barlund M, Schraml P, Leighton S, Torhorst J, Mihatsch MJ, Sauter G, Kallioniemi OP (1998) Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med 4:844–847
Korsching E, Packeisen J, Agelopoulos K, Eisenacher M, Voss R, Isola J, van Diest PJ, Brandt B, Boecker W, Buerger H (2002) Cytogenetic alterations and cytokeratin expression patterns in breast cancer: integrating a new model of breast differentiation into cytogenetic pathways of breast carcinogenesis. Lab Invest 82:1525–1533
Kvåle G, Heuch I, Eide G (1987) A prospective study of reproductive factors and breast cancer. Am J Epidemiol 126:831–841
Lakhani SR, Ellis I, Schnitt SJ, Tan PH, Van de Vijver M, World Health Organization (eds) (2012) WHO Classification of Tumours of the Breast. International Agency for Research on Cancer (IARC), Lyon
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100:229–235. doi:10.1007/s10549-006-9242-8
Moll RFW, Schiller DL (1982) The Catalog of human cytokeratins: patterns of expression in normal epithelia, tumors and cultured cells. Cell 31:11–24
Nielsen TO, Hsu FD, Jensen K, Cheang M, Karaca G, Hu Z, Hernandez-Boussard T, Livasy C, Cowan D, Dressler L, Akslen LA, Ragaz J, Gown AM, Gilks CB, van de Rijn M, Perou CM (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 10:5367–5374. doi:10.1158/1078-0432.ccr-04-0220
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lonning PE, Borresen-Dale AL, Brown PO, Botstein D (2000) Molecular portraits of human breast tumours. Nature 406:747–752. doi:10.1038/35021093
Pinder SE, Brown JP, Gillett C, Purdie CA, Speirs V, Thompson AM, Shaaban AM (2013) The manufacture and assessment of tissue microarrays: suggestions and criteria for analysis, with breast cancer as an example. J Clin Pathol 66:169–177. doi:10.1136/jclinpath-2012-201091
Rakha EA, Patel A, Powe DG, Benhasouna A, Green AR, Lambros MB, Reis-Filho JS, Ellis IO (2010) Clinical and biological significance of E-cadherin protein expression in invasive lobular carcinoma of the breast. Am J Surg Pathol 34:1472–1479. doi:10.1097/PAS.0b013e3181f01916
Schweizer J, Bowden PE, Coulombe PA, Langbein L, Lane EB, Magin TM, Maltais L, Omary MB, Parry DA, Rogers MA, Wright MW (2006) New consensus nomenclature for mammalian keratins. J Cell Biol 174:169–174. doi:10.1083/jcb.200603161
Sung H, Garcia-Closas M, Chang-Claude J, Blows FM, Ali HR, Figueroa J, Nevanlinna H, Fagerholm R, Heikkila P, Blomqvist C, Giles GG, Milne RL, Southey MC, McLean C, Mannermaa A, Kosma VM, Kataja V, Sironen R, Couch FJ, Olson JE, Hallberg E, Olswold C, Cox A, Cross SS, Kraft P, Tamimi RM, Eliassen AH, Schmidt MK, Bolla MK, Wang Q, Easton D, Howat WJ, Coulson P, Pharoah PD, Sherman ME, Yang XR (2016) Heterogeneity of luminal breast cancer characterised by immunohistochemical expression of basal markers. Br J Cancer 114:298–304. doi:10.1038/bjc.2015.437
Tas F, Bilgin E, Karabulut S, Duranyildiz D (2014) Clinical significance of serum epidermal growth factor receptor (EGFR) levels in patients with breast cancer. Cytokine 71:66–70. doi:10.1016/j.cyto.2014.09.001
Tischkowitz M, Brunet JS, Begin LR, Huntsman DG, Cheang MC, Akslen LA, Nielsen TO, Foulkes WD (2007) Use of immunohistochemical markers can refine prognosis in triple negative breast cancer. BMC Cancer 7:134. doi:10.1186/1471-2407-7-134
Valentin MD, da Silva SD, Privat M, Alaoui-Jamali M, Bignon YJ (2012) Molecular insights on basal-like breast cancer. Breast Cancer Res Treat 134:21–30. doi:10.1007/s10549-011-1934-z
Valla M, Vatten LJ, Engstrom MJ, Haugen OA, Akslen LA, Bjorngaard JH, Hagen AI, Ytterhus B, Bofin AM, Opdahl S (2016) Molecular subtypes of breast cancer: long-term incidence trends and prognostic differences. Cancer Epidemiol Biomarkers Prev. doi:10.1158/1055-9965.epi-16-0427
Valla M, Vatten LJ, Engstrom MJ, Haugen OA, Akslen LA, Bjorngaard JH, Hagen AI, Ytterhus B, Bofin AM, Opdahl S (2016) Molecular subtypes of breast cancer: long-term incidence trends and prognostic differences. Cancer Epidemiol Biomarkers Prev 25:1625–1634. doi:10.1158/1055-9965.EPI-16-0427
Yadav BS, Chanana P, Jhamb S (2015) Biomarkers in triple negative breast cancer: a review. World J Clin Oncol 6:252–263. doi:10.5306/wjco.v6.i6.252
Acknowledgements
The authors thank the Department of Pathology and Medical Genetics at St. Olav’s Hospital, Trondheim University Hospital, Norway for making the archives available for the study; the Cancer Registry of Norway, and the Norwegian Cause of Death Registry for providing the patient data. Biomedical scientists Borgny Ytterhus and Anette Skjervold have made invaluable contributions to the logistical and laboratory aspects of the study. The Cancer Registry of Norway; Research Council of Norway; and the Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology supported this work.
Authors’ contribution
MJE contributed to conception and design of the study, interpretation of the IHC markers, carried out statistical analyses, interpretation of the results and drafted the manuscript. MV contributed to discussion and interpretation of the results, interpretation of the IHC markers, review and revision of the manuscript. AMB contributed to discussion and interpretation of the results, interpretation of the IHC markers, review and revision of the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Engstrøm, M.J., Valla, M. & Bofin, A.M. Basal markers and prognosis in luminal breast cancer. Breast Cancer Res Treat 163, 207–217 (2017). https://doi.org/10.1007/s10549-017-4182-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4182-z