Abstract
Findings from epidemiologic studies of oxidative stress biomarkers and breast cancer have been mixed, although no studies have focused on estrogen receptor-negative (ER−) tumors which may be more strongly associated with oxidative stress. We examined prediagnostic plasma fluorescent oxidation products (FlOP), a global biomarker of oxidative stress, and risk of ER− breast cancer in a nested case-control study in the Nurses’ Health Study and Nurses’ Health Study II. ER− breast cancer cases (n = 355) were matched to 355 controls on age, month/time of day of blood collection, fasting status, menopausal status, and menopausal hormone use. Conditional logistic regression models were used to examine associations of plasma FlOP at three emission wavelengths (FlOP_360, FlOP_320, and FlOP_400) and risk of ER− breast cancer. We did not observe any significant associations between FlOP measures and risk of ER− breast cancer overall; the RRQ4vsQ1 (95 %CI) 0.70 (0.43–1.13), p trend = 0.09 for FlOP_360; 0.91(0.56-1.46), p trend = 0.93 for FlOP_320; and 0.62 (0.37-1.03), p trend = 0.10 for FlOP_400. Results were similar in models additionally adjusted for total carotenoid levels and in models stratified by age and total carotenoids. Although high (vs. low) levels of FIOP_360 and FIOP_400 were associated with lower risk of ER− breast cancer in lean women (body mass index (BMI) < 25 kg/m2) but not in overweight/obese women, these differences were not statistically significant (pint = 0.23 for FlOP_360; pint = 0.37 for FlOP_400). Our findings suggest that positive associations of plasma FlOP concentrations and ER− breast cancer risk are unlikely.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oxidative stress, resulting from inadequate clearance of reactive oxygen species (ROS), causes damage to lipids, proteins, and DNA, and may be related to carcinogenesis [1–3]. While several small studies have observed positive associations between lipid peroxidation markers of oxidative stress, including malondialdehyde (MDA) and 15-F2T-isoprostanes (15-F2T-IsoP), and overall breast cancer risk [4–12], these findings have not been confirmed in larger prospective studies [13, 14]. Plasma fluorescent oxidation products (FlOP) quantify the interaction of oxidative products with proteins, lipids, and DNA and thus represent a more global measure of oxidative stress compared to traditional biomarkers of lipid peroxidation [16]. Further, unlike MDA and 15-F2T-IsoP, FlOP are stable in blood with delayed processing between collection and freezing [15]. In our prior nested case-control studies, we did not observe consistent associations between plasma FlOP and overall breast cancer risk [16, 17], although an elevated risk of breast cancer was observed among women with persistently high concentrations of FlOP_320 [16].
Given the role of carotenoids as antioxidants reducing oxidative stress-induced DNA damage [18] and the suggestion from large pooled analyses that carotenoids are inversely associated with estrogen receptor-negative (ER−) breast cancer [19, 20], the role of oxidative stress on tumorigenesis may conceivably be more important in the etiology of this subset of breast tumors. However, to our knowledge, no prior study has examined associations of plasma FlOPs with ER− breast cancer specifically, while accounting for carotenoid measures. Thus, we used a nested case-control design within the Nurses’ Health Study (NHS) and Nurses’ Health Study II (NHSII) to examine associations between prediagnostic plasma FlOP concentrations and ER− breast cancer and evaluated whether associations were modified by total plasma carotenoids. Our two prior investigations included 45 [16] and 150 [15] ER− cases, and here we include those cases along with additional 160 ER− cases (total = 355) for a more thorough examination of oxidative stress in this aggressive tumor subtype.
Methods
Study population
The NHS began in 1976 when 121,700 female registered nurses, aged 30–55 years, completed a mailed questionnaire. The NHSII was established in 1989 among 116,430 female registered nurses, aged 25–42 years. Women in both ongoing cohorts continue to be followed via biennial questionnaire to assess lifestyle factors and disease diagnoses. Between 1989 and 1990, 32,826 NHS participants, aged 43–70 years, provided blood samples. NHSII participants, aged 32–54 years, provided blood samples between 1996 and 1999. Further details of the blood collection procedure for NHS [21, 22] and NHSII [23] have been described previously. Briefly, participants had their blood drawn and shipped the sample on ice to our laboratory via overnight courier. All samples were processed in our laboratory into plasma, white blood cell, and red blood cell components and have been stored at <130 °C in continuously monitored liquid nitrogen freezers. The stability of plasma FlOP concentrations using these procedures has been previously demonstrated [15].
Case and control selection
A total of 710 NHS and NHSII participants who contributed blood samples and were cancer free at the time of the blood collection were included in this nested case-control study. A total of 355 ER− invasive breast cancer cases were diagnosed after the blood collection and before June 1, 2006 (NHS) and June 1, 2007(NHSII); all cases were confirmed via medical record review. Information on ER, progesterone receptor (PR) status, and tumor characteristics were abstracted from pathology reports.
A single control was matched to each case on factors at blood collection: age (within 1 year), month (± 1 month) and time of day (± 2 h) of blood collection; fasting status (≥10 h since last meal vs. <10 h or unknown); and menopausal status and menopausal hormone therapy (HT) use (premenopausal, postmenopausal/no HT use, postmenopausal/HT use, unknown menopausal status). Cases and controls were also matched on menopausal status at the time of the case diagnosis. This study was approved by the Committee on the Use of Human Subjects in Research at the Brigham and Women’s Hospital (Boston, MA,USA).
Laboratory assays
Laboratory personnel, blinded to case-control status, assayed case-control sets together in random order. Details of the laboratory procedures used to quantify plasma FlOP concentrations have been described previously [24]. Briefly, plasma samples were mixed with ethanol/ether and with supernatant added for spectrofluorometric readings in the laboratory of coauthor (TW) at the University of Cincinnati. Fluorescence was determined as relative fluorescent intensity per milliliter of plasma (Fl/ml). FlOP measures were assayed at three excitation levels: FlOP_360 (excitation 360 nm, emission 420 nm), FlOP_ 320 (excitation 320 nm, emission 420 nm), and FlOP_400 (excitation 400 nm, emission 475 nm). FlOP_360 characterizes the interaction between lipid oxidation productions and protein, DNA, and carbohydrates [24]. FlOP_320 represents the interaction between lipid oxidative products, particularly lineolate, with DNA and metals [25, 26]. FlOP_400 represents the interaction between MDA, proteins, and phospholipids [26, 27]. Intraclass correlation coefficients (ICC) for a single FlOP measure over 3 years in NHS women ranged from 0.44 (FlOP_360) to 0.70 (FlOP_400); ICCs over 10 years ranged from 0.14 (FlOP_320) to 0.30 (FlOP_360) [28]. The three FlOP measures were moderately-to-strongly correlated with Spearman correlations r = 0.69 between FlOP_360 and FlOP_320, r = 0.45 between FlOP_320 and FlOP_400, and r = 0.73 between FlOP_360 and FlOP_400. In prior epidemiologic research, FlOP_360 has been the most commonly used FlOP measure [15, 29].
Plasma carotenoids may be associated with FlOP measures and breast cancer, and could confound or modify associations. Therefore, total plasma carotenoid concentrations were considered as potential confounders and/or effect modifiers in this analysis. For this analysis, we included 643 (91 %) women for whom the total carotenoid information was available. Carotenoids were assayed using reverse-phase high-performance liquid chromatography [30] at the Micronutrient Analysis Laboratory in the Department of Nutrition at the Harvard School of Public Health. Total carotenoids were calculated as the sum of α-carotene, β-carotene, β-cryptoxanthin, lycopene, and lutein/zeaxanthin. Total carotenoids were weakly correlated with FlOP measures (Spearman correlations r = 0.15 between FlOP_360 and total carotenoids, r = −0.12 between FlOP_320 and total carotenoids, and r = −0.06 between FlOP_400 and total carotenoids) [16].
We observed batch variation for FlOPs in the 10 % of samples included as masked quality control samples. Thus, we adjusted for this batch variation using methods described by Rosner et al. [31], as we have used previously [32]. After recalibration, overall CVs for each FlOP were <20 %.
Statistical methods
Statistical outliers in FlOP concentrations were identified using the generalized extreme studentized deviate many-outlier detection approach [33]; n = 13 (FlOP_400), n = 15 (FlOP_360), and n = 44 (FlOP_320) extreme values were identified and excluded in sensitivity analyses. Quartiles were created based on the distribution of FlOP concentrations among controls. Wald tests for trend were conducted by modeling the median across quartiles of FlOP concentrations as a continuous variable.
NHS and NHSII data were pooled and we used conditional logistic regression models to estimate relative risks (RR) and 95 % confidence intervals (CI) adjusting for matching factors and covariates. Information on potential covariates, including family history of breast cancer (yes/no), history of benign breast disease (yes/no), age at menarche (<12, 12, 13, 14 + years), age at first birth and parity (nulliparous, 1–2 children < 25 years, 3 + children <25 years, 1–2 children >25 years, 3 + children >25 years), alcohol intake (0, 1 to <5, 5 to <15, >15 g/day), smoking status (never, past, current), physical activity (<3, 3 to <9, 9 to <18, 18 to <27, and 27 + MET-h/week), and body mass index (BMI; <25, 25 to <30 and >30 kg/m2), were collected on the biennial questionnaires or the questionnaires returned with the blood samples. We additionally examined models including measured total carotenoid concentrations as a covariate. We evaluated whether the association between FlOP and ER− breast cancer risk varied by BMI (<25 vs. >25 kg/m2), age at blood collection (<50 vs. >50 years), and total carotenoids (low vs. high, dichotomized at the median) using unconditional logistic regression, controlling for matched factors and covariates. We additionally examined models restricted to fasting samples (8 + hours) and models stratified by lag time from blood collection to breast cancer diagnosis (dichotomized at median) to assess whether blood fasting status or lag time influenced results. All statistical tests were two-sided, and p values were considered statistically significant at <0.05; analyses were conducted in SAS v. 9.3 (SAS Institute, Cary, NC).
Results
Cases and controls were similar with regard to BMI, smoking status, alcohol consumption, age at menarche, age at first birth, and plasma FlOP concentrations, although cases were more likely than controls to report a family history of breast cancer and a prior diagnosis of benign breast disease and were less physically active (Table 1).
We did not observe any significant associations between plasma FlOP levels and risk of ER− breast cancer overall (Table 2). For example, the RRQ4vsQ1 (95 %CI) 0.70 (0.43–1.13), p trend = 0.09 for FlOP_360; 0.91(0.56–1.46), p trend = 0.93 for FlOP_320; and 0.62(0.37–1.03), p trend = 0.10 for FlOP_400. Results were similar when we additionally adjusted for total carotenoid levels; RRQ4vsQ1 (95 %CI) 0.77 (0.45–1.33), p trend = 0.26 for FlOP_360; 0.95(0.57–1.60) , p trend = 0.57 for FlOP_320; and 0.69(0.40–1.18) , p trend = 0.30 for FlOP_400. Plasma FlOP levels also were not significantly associated with ER− breast cancer in models restricted to women fasting at least 8 h prior to blood collection, in analyses excluding outliers and in analysis stratified by lag time between blood collection and breast cancer diagnosis (data not shown).
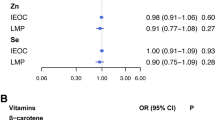
We did not observe any heterogeneity in associations in analysis stratified by age (<50 vs. >50 years), or by total carotenoid level (dichotomized at median); and no significant interaction was apparent for any of the FlOPs (all pint >0.25) (Table 3). For FIOP_360 and FIOP_400, results did appear to differ according to BMI at blood collection, although the interactions were not statistically significant (p int = 0.23 and p int = 0.37, respectively). For example, risk of ER− breast cancer was 60 % lower among lean women (BMI <25 kg/m2) in the highest vs. lowest quartile of FlOP_360 (RRQ4vsQ1(95 %CI) 0.40 (0.20–0.81), p trend = 0.01) and FlOP_400 (0.42 (0.22-0.82), p trend = 0.02), while no significant associations were observed among women with BMI >25 kg/m2; FlOP_360 (RRQ4vsQ1(95 %CI) 1.10 (0.54–2.24), p trend = 0.93) and FlOP_400 (0.96 (0.46–1.99), p trend = 0.88).
Discussion
In this large, nested case-control study, we did not observe any significant associations between plasma FlOP levels and ER− breast cancer overall, or in analyses stratified by age and total plasma carotenoid concentrations. However, plasma FlOP_360 and FlOP_400 were associated with a reduced risk of ER− breast cancer among lean women, while no significant associations were observed for women with BMI > 25 kg/m2, although the interaction was not significant.
While this study is the first to focus primarily on the role of plasma FlOP and ER− breast cancer, our null findings are generally consistent with prior prospective studies of both urinary [13, 14] and plasma [16, 17] markers of oxidative stress and overall breast cancer risk. We unexpectedly observed significant inverse associations of FlOP_360 and FlOP_400 and risk of ER− breast cancer among women with BMI <25 kg/m2 in this study, however the interactions by BMI were not statistically significant. A reduced risk of overall breast cancer in relation to a urinary marker of lipid peroxidation was also observed among lean women in a prior prospective study of Chinese women [13]; however, in our prior smaller study, we observed a positive association of FlOP_320 and overall breast cancer risk among lean women and no heterogeneity in associations of FlOP_360 and FlOP_400 by BMI [16]. While associations did not vary by total carotenoids in this study, nor in our prior study of premenopausal FlOP measures and total breast cancer [15], a suggestion of an increased risk of overall breast cancer in relation to FlOP_360 and FlOP_320 among women with low plasma carotenoid levels was observed in our prior study of primarily postmenopausal women [16].
Reactive oxygen species (ROS), generated from both endogenous metabolic processes [34–36] and exogenous exposures including alcohol and radiation [37, 38], are generally cleared through enzymatic destruction or exogenous antioxidants. Given that antioxidants, including carotenoids, may neutralize these reactive molecules, thereby reducing the burden of oxidative stress and potentially inhibiting carcinogenesis, the reduced risk of ER− breast cancer in relation to carotenoids [19] may be partially explained through oxidative stress pathways. If carotenoids reduce oxidative stress-induced cell damage, we might expect oxidative stress biomarkers to be more strongly associated with ER− breast cancer. Further, chronic exposure to oxidative stress, through hydrogen peroxidate-induced proliferation of intracellular ROS, has been shown to cause loss of ER− alpha expression and conversion of estrogen-dependent breast cancer cells into estrogen-independent phenotype [39], suggesting the importance of oxidative stress on ER− breast cancer risk. However, despite the biological plausibility of positive associations between oxidative stress and ER− breast cancer, we did not observe any significant positive associations in this study. In fact, inverse associations of plasma FlOP and ER− breast cancer were observed among lean women in this study, although the interaction with BMI was not significant, and the finding may be due to chance. While it is plausible that ROS may induce DNA damage, promoting lipid peroxidation and playing a role in etiology of cancer, ROS might also mediate or trigger protective mechanisms, such as apoptosis, which could have beneficial function in breast cancer [40], and may be more apparent in proliferative subtypes, such as ER− tumors. Future studies are warranted to elucidate the complex biological pathways whereby oxidative stress may promote, or perhaps inhibit, breast carcinogenesis.
Strengths of this study include the relatively large sample size of ER− breast cancer cases with measured carotenoid levels and use of comprehensive plasma measures of oxidative stress. Plasma FlOP concentrations, which are thought to reflect global levels of oxidation, have been associated with exposures related to oxidative stress including cigarette smoking and cholesterol [29]. However, given our lack of findings with breast cancer, other specific markers of oxidative stress may be more important in breast cancer etiology, although urinary markers of lipid peroxidation also were not associated with breast cancer risk in the prospective Shanghai Women’s Health Study [13, 14]. Due to the uncommon nature of ER− tumors, we were somewhat limited in our ability to conduct stratified analyses as part of this study. While our study relied on a single measurement of FlOP levels, reproducibility over a 2- to 3-year period (ICCs = 0.44–0.70) [28], though a bit lower for a 10-year period (ICCs = 0.14–0.30) [16], suggests that one measure is an adequate reflection of longer-term exposure. However, persistently high levels of FlOP_320 were associated with a suggested elevated risk of breast cancer in our prior study [16], suggesting that duration of exposure to ROS could be important. It is also possible that different time periods of exposure may have differing effects for carcinogenesis. In fact, timing during the menstrual cycle, pregnancy, and lactation have been suggested as important etiologic windows for the influence of oxidative stress in breast cancer [40]. Thus, future studies are warranted to examine whether the risk of breast cancer in relation to oxidative stress may vary depending upon the timing and duration of the exposure.
In summary, we did not observe significant associations between plasma FlOP measures and risk of ER− breast cancer overall in this large nested case-control study. Our findings suggest that positive associations of plasma FlOP concentrations and ER− breast cancer risk are unlikely. Although a suggested inverse association of plasma FlOP_360 and FlOP_400 and ER− breast cancer was observed among lean women, the interaction was not significant and there is no strong biologic plausibility for this finding. Given the consistent findings of inverse associations of carotenoids and ER− breast cancer, oxidative stress pathways should continue to be investigated as a potential etiologic mechanism for this aggressive breast cancer subtype.
References
Dreher D, Junod AF (1996) Role of oxygen free radicals in cancer development. Eur J Cancer 32A(1):30–38
Halliwell B (2007) Oxidative stress and cancer: have we moved forward? Biochem J 401(1):1–11. doi:10.1042/bj20061131
Klaunig JE, Kamendulis LM (2004) The role of oxidative stress in carcinogenesis. Annu Rev Pharmacol Toxicol 44:239–267. doi:10.1146/annurev.pharmtox.44.101802.121851
Sener DE, Gonenc A, Akinci M, Torun M (2007) Lipid peroxidation and total antioxidant status in patients with breast cancer. Cell Biochem Funct 25(4):377–382. doi:10.1002/cbf.1308
Khanzode SS, Muddeshwar MG, Khanzode SD, Dakhale GN (2004) Antioxidant enzymes and lipid peroxidation in different stages of breast cancer. Free Radic Res 38(1):81–85
Huang YL, Sheu JY, Lin TH (1999) Association between oxidative stress and changes of trace elements in patients with breast cancer. Clin Biochem 32(2):131–136
Gonenc A, Ozkan Y, Torun M, Simsek B (2001) Plasma malondialdehyde (MDA) levels in breast and lung cancer patients. J Clin Pharm Ther 26(2):141–144
Akbulut H, Akbulut KG, Icli F, Buyukcelik A (2003) Daily variations of plasma malondialdehyde levels in patients with early breast cancer. Cancer Detect Prev 27(2):122–126
Polat MF, Taysi S, Gul M, Cikman O, Yilmaz I, Bakan E, Erdogan F (2002) Oxidant/antioxidant status in blood of patients with malignant breast tumour and benign breast disease. Cell Biochem Funct 20(4):327–331. doi:10.1002/cbf.980
Ray G, Batra S, Shukla NK, Deo S, Raina V, Ashok S, Husain SA (2000) Lipid peroxidation, free radical production and antioxidant status in breast cancer. Breast Cancer Res Treat 59(2):163–170
Rossner P Jr, Gammon MD, Terry MB, Agrawal M, Zhang FF, Teitelbaum SL, Eng SM, Gaudet MM, Neugut AI, Santella RM (2006) Relationship between urinary 15-F2t-isoprostane and 8-oxodeoxyguanosine levels and breast cancer risk. Cancer Epidemiol Biomarkers Prev 15(4):639–644. doi:10.1158/1055-9965.epi-05-0554
Tas F, Hansel H, Belce A, Ilvan S, Argon A, Camlica H, Topuz E (2005) Oxidative stress in breast cancer. Med Oncol 22(1):11–15. doi:10.1385/mo:22:1:011
Dai Q, Gao YT, Shu XO, Yang G, Milne G, Cai Q, Wen W, Rothman N, Cai H, Li H, Xiang Y, Chow WH, Zheng W (2009) Oxidative stress, obesity, and breast cancer risk: results from the Shanghai Women’s Health Study. J Clin Oncol 27(15):2482–2488. doi:10.1200/jco.2008.19.7970
Lee KH, Shu XO, Gao YT, Ji BT, Yang G, Blair A, Rothman N, Zheng W, Chow WH, Kang D (2010) Breast cancer and urinary biomarkers of polycyclic aromatic hydrocarbon and oxidative stress in the Shanghai Women’s Health Study. Cancer Epidemiol Biomarkers Prev 19(3):877–883. doi:10.1158/1055-9965.epi-09-1098
Wu T, Willett WC, Rifai N, Rimm EB (2007) Plasma fluorescent oxidation products as potential markers of oxidative stress for epidemiologic studies. Am J Epidemiol 166(5):552–560. doi:10.1093/aje/kwm119
Fortner RT, Tworoger SS, Wu T, Eliassen AH (2013) Plasma florescent oxidation products and breast cancer risk: repeated measures in the Nurses’ Health Study. Breast Cancer Res Treat 141(2):307–316. doi:10.1007/s10549-013-2673-0
Sisti JS, Lindstrom S, Kraft P, Tamimi RM, Rosner BA, Wu T, Willett WC, Eliassen AH (2015) Premenopausal plasma carotenoids, fluorescent oxidation products, and subsequent breast cancer risk in the nurses’ health studies. Breast Cancer Res Treat 151(2):415–425. doi:10.1007/s10549-015-3391-6
Frei B (1994) Reactive oxygen species and antioxidant vitamins: mechanisms of action. Am J Med 97(3A):5S–13S discussion 22S-28S
Eliassen AH, Hendrickson SJ, Brinton LA, Buring JE, Campos H, Dai Q, Dorgan JF, Franke AA, Gao YT, Goodman MT, Hallmans G, Helzlsouer KJ, Hoffman-Bolton J, Hulten K, Sesso HD, Sowell AL, Tamimi RM, Toniolo P, Wilkens LR, Winkvist A, Zeleniuch-Jacquotte A, Zheng W, Hankinson SE (2012) Circulating carotenoids and risk of breast cancer: pooled analysis of eight prospective studies. J Natl Cancer Inst 104(24):1905–1916. doi:10.1093/jnci/djs461
Zhang X, Spiegelman D, Baglietto L, Bernstein L, Boggs DA, van den Brandt PA, Buring JE, Gapstur SM, Giles GG, Giovannucci E, Goodman G, Hankinson SE, Helzlsouer KJ, Horn-Ross PL, Inoue M, Jung S, Khudyakov P, Larsson SC, Lof M, McCullough ML, Miller AB, Neuhouser ML, Palmer JR, Park Y, Robien K, Rohan TE, Ross JA, Schouten LJ, Shikany JM, Tsugane S, Visvanathan K, Weiderpass E, Wolk A, Willett WC, Zhang SM, Ziegler RG, Smith-Warner SA (2012) Carotenoid intakes and risk of breast cancer defined by estrogen receptor and progesterone receptor status: a pooled analysis of 18 prospective cohort studies. Am J Clin Nutr 95(3):713–725. doi:10.3945/ajcn.111.014415
Zhang X, Tworoger SS, Eliassen AH, Hankinson SE (2013) Postmenopausal plasma sex hormone levels and breast cancer risk over 20 years of follow-up. Breast Cancer Res Treat 137(3):883–892. doi:10.1007/s10549-012-2391-z
Hankinson SE, Willett WC, Manson JE, Colditz GA, Hunter DJ, Spiegelman D, Barbieri RL, Speizer FE (1998) Plasma sex steroid hormone levels and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 90(17):1292–1299
Tworoger SS, Sluss P, Hankinson SE (2006) Association between plasma prolactin concentrations and risk of breast cancer among predominately premenopausal women. Cancer Res 66(4):2476–2482. doi:10.1158/0008-5472.can-05-3369
Wu T, Rifai N, Roberts LJ 2nd, Willett WC, Rimm EB (2004) Stability of measurements of biomarkers of oxidative stress in blood over 36 hours. Cancer Epidemiol Biomarkers Prev 13(8):1399–1402
Frankel EN (1987) Secondary products of lipid oxidation. Chem Phys Lipids 44(2–4):73–85
Fujimoto K, Neff WE, Frankel EN (1984) The reaction of DNA with lipid oxidation products, metals and reducing agents. Biochim Biophys Acta 795(1):100–107
Flynn TP, Allen DW, Johnson GJ, White JG (1983) Oxidant damage of the lipids and proteins of the erythrocyte membranes in unstable hemoglobin disease. Evidence for the role of lipid peroxidation. J Clin Invest 71(5):1215–1223
Jensen MK, Wang Y, Rimm EB, Townsend MK, Willett W, Wu T (2013) Fluorescent oxidation products and risk of coronary heart disease: a prospective study in women. J Am Heart Assoc 2(5):e000195. doi:10.1161/jaha.113.000195
Wu T, Rifai N, Willett WC, Rimm EB (2007) Plasma fluorescent oxidation products: independent predictors of coronary heart disease in men. Am J Epidemiol 166(5):544–551. doi:10.1093/aje/kwm120
El-Sohemy A, Baylin A, Kabagambe E, Ascherio A, Spiegelman D, Campos H (2002) Individual carotenoid concentrations in adipose tissue and plasma as biomarkers of dietary intake. Am J Clin Nutr 76(1):172–179
Rosner B, Cook N, Portman R, Daniels S, Falkner B (2008) Determination of blood pressure percentiles in normal-weight children: some methodological issues. Am J Epidemiol 167(6):653–666. doi:10.1093/aje/kwm348
Hirko KA, Spiegelman D, Willett WC, Hankinson SE, Eliassen AH (2014) Alcohol consumption in relation to plasma sex hormones, prolactin, and sex hormone-binding globulin in premenopausal women. Cancer Epidemiol Biomarkers Prev 23(12):2943–2953. doi:10.1158/1055-9965.epi-14-0982
Rosner B (1983) Percentage points for a generalized ESD many-outlier procedure. Technometrics 25:165–172
Valko M, Izakovic M, Mazur M, Rhodes CJ, Telser J (2004) Role of oxygen radicals in DNA damage and cancer incidence. Mol Cell Biochem 266(1–2):37–56
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J (2007) Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol 39(1):44–84. doi:10.1016/j.biocel.2006.07.001
Yager JD (2000) Endogenous estrogens as carcinogens through metabolic activation. J Natl Cancer Inst Monogr 27:67–73
Brooks PJ (1997) DNA damage, DNA repair, and alcohol toxicity–a review. Alcohol Clin Exp Res 21(6):1073–1082
Sies H (1997) Oxidative stress: oxidants and antioxidants. Exp Physiol 82(2):291–295
Mahalingaiah PK, Ponnusamy L, Singh KP (2015) Chronic oxidative stress causes estrogen-independent aggressive phenotype, and epigenetic inactivation of estrogen receptor alpha in MCF-7 breast cancer cells. Breast Cancer Res Treat 153(1):41–56. doi:10.1007/s10549-015-3514-0
Gago-Dominguez M, Castelao JE, Pike MC, Sevanian A, Haile RW (2005) Role of lipid peroxidation in the epidemiology and prevention of breast cancer. Cancer Epidemiol Biomarkers Prev 14(12):2829–2839. doi:10.1158/1055-9965.EPI-05-0015
Acknowledgments
This research was supported from the NIH RO1 CA131218, NHS and NHSII UM1: CA186107 and CA176726. KA Hirko was supported by the R25 CA098566 and the T32 CA009001 training grants. RT Fortner was supported by the T32 CA009001 training grant. We would like to thank the participants and staff of the Nurses’ Health Study and the Nurses’ Health Study II for their valuable contributions as well as the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, WY. The authors assume full responsibility for analyses and interpretation of these data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest. The analysis presented here complies with current laws of the country in which they were performed.
Rights and permissions
About this article
Cite this article
Hirko, K.A., Fortner, R.T., Hankinson, S.E. et al. Plasma fluorescent oxidation products and risk of estrogen receptor-negative breast cancer in the Nurses’ Health Study and Nurses’ Health Study II. Breast Cancer Res Treat 158, 149–155 (2016). https://doi.org/10.1007/s10549-016-3861-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3861-5