Abstract
Epidemiological studies have demonstrated associations between circulating levels of sex steroid hormones and risk of breast cancer in postmenopausal women. However, data on associations with breast cancer survival are limited. We measured levels of estradiol, estrone, testosterone, and sex hormone-binding globulin (SHBG), in serum collected on average 30 months after diagnosis from 358 postmenopausal women diagnosed with stage I-IIIA breast cancer between 1995 and 1998 who participated in a multiethnic, prospective cohort study. Women were followed through December, 2012. We evaluated associations between log-transformed analytes and breast cancer-specific and all-cause mortality fitting multivariable Cox proportional hazards models. Over a median of 14.5 years of follow-up, 102 deaths occurred; 43 of these were due to breast cancer. In models adjusted for ethnicity/study site, age, body mass index, and tumor stage, increased levels of log-transformed SHBG were associated with reduced risk of both breast cancer-specific mortality (hazard ratio, HR 0.48; 95 % confidence interval, CI 0.26–0.89) and all-cause mortality (HR 0.64, 95 % CI 0.43–0.97). There were no associations between levels of estradiol, estrone, or testosterone for either endpoint. In subgroup analyses, after correction for multiple testing, increased estrone was significantly associated with reduced risk for breast cancer-specific mortality among participants with ER-negative tumors (HR 0.16, 95 % CI 0.05–0.63) but not among participants with ER-positive tumors. Increased serum levels of SHBG were associated with decreased risk of breast cancer-specific and all-cause mortality in women with breast cancer. These results should be confirmed in larger breast cancer survivor cohorts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postmenopausal women with elevated levels of serum sex steroid hormones including estradiol, testosterone, and estrone, are at increased risk for developing breast cancer [1]. Paradoxically, conjugated equine estrogen alone reduced breast cancer risk in the Women’s Health Initiative clinical trial, while conjugated equine estrogen plus medroxyprogesterone acetate increased risk [2, 3]. However, those receiving estrogen alone had a prior hysterectomy (with or without bilateral salpingo-oophorectomy) while those receiving estrogen plus progesterone had no history of hysterectomy so the underlying risk factors and exposures to endogenous estrogens was likely different between women from the two trials. Medications to inhibit or block estrogens are the mainstay of treatment for women with hormone receptor-positive breast cancer [4]. However, data on the association between circulating sex steroid hormones and prognosis in breast cancer survivors are limited [5–7].
Here we report on the association between circulating levels of estradiol (total and free), estrone, testosterone (total and free), and SHBG, and breast cancer-specific and all-cause mortality in the Health Eating Activity and Lifestyle (HEAL) study, a multiethnic cohort of breast cancer survivors, diagnosed with Stage I–IIIA breast cancer.
Materials and methods
Study setting, participants, and recruitment
The HEAL Study is a multicenter, multiethnic prospective cohort study that enrolled 1183 women newly diagnosed with breast cancer to evaluate effects of diet, weight, physical activity, other lifestyle factors, hormones, and other exposures on breast cancer prognosis. Aims, study design, and recruitment procedures have been published previously [8].
Briefly, women were recruited through Surveillance, Epidemiology, and End Results (SEER) registries in New Mexico (NM), Los Angeles County (CA), and western Washington (WA). Baseline surveys were conducted on average 6-month post-diagnosis. In NM, we recruited 615 women, ≥18 years, diagnosed with in situ to Stage IIIA breast cancer between 1996 and 1999. In WA, we recruited 202 women, aged 40–64 years, diagnosed with Stage 0–Stage IIIA breast cancer between 1997 and 1998. In CA, we recruited 366 Black women aged 35–64 years, with Stage 0–Stage IIIA breast cancer, who had participated in the Los Angeles portion of the Women’s Contraceptive and Reproductive Experiences Study or a parallel study of in situ breast cancer, and were diagnosed with breast cancer between 1995 and 1998. Recruitment was restricted to women aged 35–64 at diagnosis because of competing studies in WA and parent study design in CA. The HEAL study was performed with the approval of the Institutional Review Boards of participating centers in accordance with assurances filed with and approved by the U.S. Department of Health and Human Services. Written informed consent was obtained from each participant.
A total of 944 women completed in-person interviews in approximately 30 months after breast cancer diagnosis. Of these, 804 provided a blood sample and had complete data on all sex steroid hormones. Analysis was restricted to women who had a diagnosis of local or regional breast cancer, who were postmenopausal at the time of blood draw, and not taking hormone replacement therapy (HRT) at the time of blood draw. We thus excluded 188 participants with in situ (Stage I) breast cancer. We excluded a further 25 who had non-fatal breast cancer events less than 9 months before their 30-month interview dates to avoid potential confounding from possible recent treatments, 130 who had levels of FSH <25 mIU/mL, and 49 with estradiol levels >45 pg/ml as these participants were likely to be pre- or peri-menopausal. A further 33 participants who reported being pre-menopausal and 20 who reported taking HRT were excluded from the analysis. Finally, 1 participant who was missing data on a variety of variables was excluded. The final sample comprised the remaining 358 participants.
Data collection and covariates
Assays
A 30-ml fasting blood sample was collected from patients at the 30-month interview, processed within 3 h of collection, and stored at −80 ºC until analysis. Sex steroid hormones measured were estrone, estradiol, testosterone, and sex hormone-binding globulin (SHBG). Free (non-SHBG bound) estradiol and testosterone levels were calculated as described in Sodergard et al. [9]. All samples were randomly assigned to assay batches and were randomly ordered within each batch. Laboratory personnel performing the assays were blinded to patient identity. Estrone, estradiol, and SHBG were measured at Quest Diagnostics at the Nichols Institute (San Juan Capistrano, CA) for WA samples; the Endocrine Research Laboratory at the University of Southern California for CA samples; and the University of New Mexico (UNM) endocrinology laboratory for UNM samples. Testosterone was measured for all sites at UNM.
All sex hormones were analyzed using radioimmunoassay (RIA) as previously described [8]. Serum extraction and chromatographic purification were performed prior to analysis of estrone and estradiol. Assay sensitivities and inter-assay precision were <10 pg/ml and 10 %, respectively for estrone; and <2 pg/ml and 8 % for estradiol. For testosterone, analysis was performed using an RIA kit (Siemens Healthcare Diagnostics, formerly Diagnostic Products Corporation, Deerfield, IL), with a sensitivity of 40 pg/ml and inter-assay precision of 5.9–11 %. SHBG was measured by direct immunoassay (Wein Laboratories, Inc), with a sensitivity of 6 nmol/l and inter-assay precision of 5.9 %.
Covariates
Standardized questionnaire information including medical history, demographic, and lifestyle information, was collected at baseline (corresponding to an average of 6-month post-diagnosis), and on average 30-month post-diagnosis. Information on disease stage, hormone receptor status, and adjuvant therapy was abstracted from medical records. Weight and height were measured at approximately 30-month post-diagnosis, and BMI was calculated as kg/m2. A race/ethnicity/study site four-category variable was created to adjust for race and site-associated confounding because these were highly correlated. The variable had 4 categories: Non-Hispanic whites at UNM; Non-Hispanic whites at FHCRC; Hispanics; African-Americans. Estrogenic botanical supplement use was coded and included as defined previously, and described as any use (yes/no) [10].
Stage of disease and cancer treatment
We obtained data on disease stage from SEER registry records prior to study enrollment. Participants were classified as having Stage 0 (in situ), Stage I (localized), or Stage II–IIIA (regional) breast cancer based on AJCC stage of disease classification contained within SEER. The present analysis included only women with Stage I–IIIA breast cancer at diagnosis. Estrogen receptor (ER) and progesterone receptor (PR) status of tumors was categorized as (1) positive, (2) negative, or (3) unknown/borderline. Treatment and additional clinical data were obtained from a review of medical records. Adjuvant treatment was categorized into 4 groups: surgery only, surgery and radiation, surgery and chemotherapy, or surgery, radiation, and chemotherapy.
Outcome assessment
Information on vital status was obtained from the SEER registry which obtains cause of death codes from linkages with state and national death certificate files and the Social Security Death Index. Reports examining the accuracy of the use of death certificate data found that their use did not result in a meaningful change to mortality-based outcomes [11, 12]. If alive, women were followed through their last follow-up assessment or SEER vital status update, whichever was more recent. All-cause mortality was defined as time from the 30-month follow-up interview (when serum samples were collected) to death from any cause, or end of follow-up (31 December 2012). Breast cancer mortality was defined as death from breast cancer or end of follow-up, with the same intervals as for all-cause mortality. Women with other causes of death were censored on their dates of death.
Statistical analysis
Differences in distribution of sex steroid hormones between racial/ethnic groups, and other categorical patient characteristics were estimated using analysis of covariance (ANCOVA), adjusting for age. Pearson correlation coefficients were obtained to represent associations between the analytes, corrected for multiple comparisons. Analytes were log-transformed as none were normally distributed.
Hazard ratios (HR) and 95 % confidence intervals (CI) for breast cancer-specific or all-cause mortality were based on the partial likelihood for Cox’s proportional hazards model [13]. The proportional hazard assumption was tested using Schoenfeld residuals, and no violation of the proportionality assumption was found. Age was used as the underlying time variable, with entry and exit time defined as the participant’s age at the 30-month follow-up interview, and age at death from either breast cancer or any cause, or end of follow-up, respectively. We based variable inclusion on a likelihood ratio test, and tested the following covariates: study enrollment (race/ethnicity/study site); BMI (categorical <18.5 kg/m2; ≥18.5 and <25 kg/m2; ≥25 and <40 kg/m2; ≥40 kg/m2); tumor stage; tumor hormone status (ER; PR); treatment at diagnosis (surgery; surgery + radiotherapy; chemotherapy); use of estrogenic botanical supplements; parity; and at 30-month post-diagnosis blood draw (age; tamoxifen use, yes/no; SHBG levels; smoking status, current/former/never). We included the race/ethnicity/study site variable to adjust for different distributions of race/ethnicity by study site; this also adjusted for the fact that some of the assays were carried out at different sites. Covariates included in the final model were: race/ethnicity/study site; BMI, age; tumor stage and levels of SHBG. Treatment was not included in the model as it had the same effect as tumor stage. Neither tamoxifen use nor ER status changed the HR (change in HR < 10 %).
We estimated the relationship between levels of sex steroid hormones and breast cancer-specific mortality and all-cause mortality, using unadjusted and fully adjusted models. We also examined outcome by median splits of each analyte, i.e., greater and less than the median value.
We determined whether the association of each analyte with breast cancer mortality was the same across subgroup categories, specifically stage, ER status, BMI ≤25 and >25 (events were too few to investigate additional BMI subgroups), and tamoxifen use at the time of blood draw. Statistical significance was set at P = 0.006 to adjust for multiple comparisons, i.e., P = 0.05/8 for each analyte. For analytes with significantly different results by subgroup we used a test of homogeneity of trends to test for interactions across groups.
All P values are two sided. Analyses were performed using STATA 11 (Statacorp, TX USA).
Results
Participants were followed for a median of 14.5 years. Mean age at the 30-month follow-up interview was 60.6 years; mean BMI was 27.5 kg/m2. One hundred and two deaths occurred, of which 43 were due to breast cancer. Characteristics of HEAL participants are shown in Table 1. Estrone and testosterone levels were statistically significantly higher in African-Americans compared to Hispanics and non-Hispanic whites (P = 0.0002 for estrone and P < 0.0001 for testosterone), adjusted for age. Statistically significantly higher levels of SHBG were observed in women with lower BMI (P = 0.006) and in those taking tamoxifen (P < 0.0001). Higher levels of testosterone were found in women with Stage I–II tumors (P < 0.0001), with ER-positive tumors (P < 0.0001) those not taking tamoxifen (P < 0.0001) or estrogenic supplements (P < 0.0001), and in women with the highest BMI (P < 0.0001). Estradiol levels did not vary by any characteristics examined. All associations were adjusted for age.
Estrone correlated strongly and significantly with testosterone (r = 0.56, P < 0.0001), and more weakly with both estradiol and BMI (r = 0.21, P < 0.0001; r = 0.31, P < 0.0001, Table 2). Estradiol correlated only with free testosterone (r = 0.17, P = 0.001,); testosterone correlated weakly but significantly with BMI (r = 0.23, P < 0.0001); however free testosterone correlated with estrone (r = 0.53, P < 0.0001) with BMI (r = 0.34, P < 0.0001) and negatively with SHBG (r = −0.35, P < 0.0001). SHBG correlated negatively with BMI (−0.33, P < 0.0001).
Table 3 shows the associations between circulating concentrations of sex steroid hormones and breast cancer-specific and all-cause mortality, analyzed as log-transformed variables and stratified according to median cut-points. Increased levels of log-transformed SHBG were associated with reduced risk of both breast cancer-specific mortality (HR 0.48; 95 % CI 0.26–0.89) and all-cause mortality (HR 0.64, 95 % CI 0.43–0.97), but not when analyzed as a median split, i.e., categorized as greater and less than the median value. There were no associations between levels of estradiol, estrone, or testosterone either as log-transformed variable, or as a median split for either endpoint. Associations between free estradiol or free testosterone and outcomes did not differ significantly from total estradiol or testosterone.
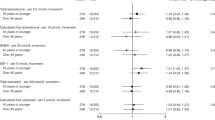
In subgroup analyses after correction for multiple testing (Table 4), increased estrone was significantly associated with reduced risk for breast cancer-specific mortality in participants with ER-negative tumors (HR 0.16, 95 % CI 0.05–0.63) but not in participants with ER-positive tumors. A similar trend was seen for women not taking tamoxifen, but this did not achieve statistical significance (P > 0.006). Estradiol was also inversely associated with breast cancer-specific mortality, but again the association was not statistically significant. There was no evidence of effect modification for any subgroup for all-cause mortality.
Discussion
In this study, increased SHBG levels in postmenopausal breast cancer survivors were significantly and inversely associated with both breast cancer-specific and all-cause mortality in a multivariate adjusted model. Testosterone, estrone, and estradiol were not significantly associated with either breast cancer-specific or all-cause mortality. Inclusion of ER status or tamoxifen use in the model did not alter the results. In subgroup analyses, estrone was significantly associated with reduced risk of breast cancer-specific mortality in women with ER-negative tumors.
While the associations between elevated levels of sex steroid hormones and increased risk of breast cancer are well established [1], the link between circulating sex steroid hormones and breast cancer-specific and all-cause mortality in breast cancer survivors are limited. In contrast to our study, one study of 194 postmenopausal women with stage T1-2N0M0 breast cancer treated with surgery alone, found that women with high levels of testosterone (>median) had a significantly lower event-free survival than those with low levels (HR 2.05; 95 % CI 1.28–3.27). Increased testosterone was also associated with a higher risk of breast cancer events (HR 1.77; 95 %; CI 1.06–2.96) [14].
In contrast to our findings, increased levels of estrogens have been linked to higher risk of recurrence in other studies. A case–control study (N = 153 pairs) of peri- and postmenopausal women, nested in the Women’s Healthy Eating and Living (WHEL) study reported that total and free estradiol were positively and statistically significantly associated with risk of recurrence (HR 1.41; 95 % CI 1.01–1.97; HR 1.31; 95 % CI 1.03–1.65, respectively), in models that adjusted for grade. Neither testosterone nor SHBG levels were associated with recurrence [5]. In a study which followed 110 breast cancer patients for 5.5 years, serum levels of estradiol were significantly higher in patients who experienced breast cancer recurrence than in those who did not; and higher levels of testosterone were associated with increased risk of recurrence (HR 1.8, 95 % CI 0.5–6.3 for the middle, and HR 7.2 95 % CI 2.4–21.4) comparing the upper tertile of baseline testosterone distribution, to the lowest. Other hormones had only a minor influence on prognosis [6]. The association between levels of estrone and improved survival among patients with ER-negative tumors is difficult to explain in the context of established associations between elevated sex steroid hormones and increased risk of breast cancer development [1].
Our data which show that elevated levels of SHBG are associated with reduced risk of breast cancer-associated and all-cause mortality may be associated with the fact that bioavailable concentrations of estrogens and its access to target cells are regulated by SHBG. In two case–control studies, SHBG was associated with lower risk of breast cancer [1], and lower levels of SHBG were observed in postmenopausal women who developed breast cancer compared to controls [15]. A meta-analysis of postmenopausal women demonstrated that high levels of SHBG were significantly associated with decreased risk of breast cancer [16]. However, it has also been postulated that SHBG has direct effects on cells, mediated by its unliganded binding to a cell-membrane receptor. [17] Activation of the receptor–SHBG complex by binding to estradiol induces a number of downstream effects, [18] including inhibition of progesterone receptor expression [19], increased apoptosis, [20] and regulation of cell growth. In ERα-positive MCF-7 cells, SHBG/estradiol membrane-initiated pathways can inhibit cell proliferation and induce apoptosis by counteracting estradiol-induced ERK activation [20–22]. Finally, inter- and intra-assay CVs for SHBG were lower than those of the other analytes. Given the limited sample size, the higher CVs for the estrone, estradiol, and testosterone assays may have reduced our ability to detect associations between these analyses and outcomes.
Our study has important limitations. First, we have only a single measure of sex hormones (mean 30-month post-diagnosis), and therefore we cannot completely characterize the women’s exposure to sex steroid hormones. The cohort was established before some current treatments such as aromatase inhibitors and trastuzumab were available, and therefore we cannot estimate what associations the analytes might have with survival in women using these treatments. There was also a possible selection bias in this study; blood was obtained approximately 30-month post-diagnosis, and we excluded participants who were under treatment for recurrence; therefore associations with early breast cancer mortality could not be estimated. We did not perform central pathological review. Therefore there could have been misclassification of hormone receptor status and possibly a larger proportion of women had hormone receptor-positive tumors. We did validate the receptor status for LA women who participated in the Women’s CARE Study prior to joining the HEAL Study [23] and found strong agreement of ER and PR when results as recorded in the SEER registry were compared to those from a single centralized reference laboratory. Furthermore, adjusting for ER status did not affect our results. Finally, the relatively small number of deaths in this study does not allow accurate assessment of risk in specific subcategories.
In summary, high levels of SHBG were associated with decreased risk of breast and all-cause cancer-specific mortality, in this cohort of postmenopausal breast cancer survivors. These results should be confirmed in larger cohorts with sufficient number of outcomes to provide adequate statistical power in determining associations.
Abbreviations
- SHBG:
-
Sex steroid hormone-binding globulin
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- HEAL:
-
Health, eating, activity, and lifestyle study
- SEER:
-
Surveillance, epidemiology, and end results
- HR:
-
Hazard ratio
- HRT:
-
Hormone replacement therapy
- CI:
-
Confidence interval
References
Key T, Appleby P, Barnes I, Reeves G (2002) Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst 94(8):606–616
Chlebowski R, Hendrix S, Langer R, Stefanick M, Gass M, Lane D, Rodabough R, Gilligan M, Cyr M, Thomson C, Khandekar J, Petrovitch H, McTiernan A, Investigators W (2003) Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the Women’s Health Initiative Randomized Trial. JAMA J Am Med Assoc 289(24):3243–3253
Stefanick ML, Anderson GL, Margolis KL, Hendrix SL, Rodabough RJ, Paskett ED, Lane DS, Hubbell FA, Assaf AR, Sarto GE, Schenken RS, Yasmeen S, Lessin L, Chlebowski RT, Investigators WHI (2006) Effects of conjugated equine estrogens on breast cancer and mammography screening in postmenopausal women with hysterectomy. JAMA J Am Med Assoc 295(14):1647–1657. doi:10.1001/jama.295.14.1647
Burstein HJ, Prestrud AA, Seidenfeld J, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, Giordano SH, Hudis CA, Malin J, Mamounas EP, Rowden D, Solky AJ, Sowers MR, Stearns V, Winer EP, Somerfield MR, Griggs JJ, American Society of Clinical O (2010) American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol 28(23):3784–3796. doi:10.1200/jco.2009.26.3756
Rock CL, Flatt SW, Laughlin GA, Gold EB, Thomson CA, Natarajan L, Jones LA, Caan BJ, Stefanick ML, Hajek RA, Al-Delaimy WK, Stanczyk FZ, Pierce JP, Women’s Healthy E, Living Study G (2008) Reproductive steroid hormones and recurrence-free survival in women with a history of breast cancer. Cancer Epidemiol Biomarkers Prev 17(3):614–620. doi:10.1158/1055-9965.epi-07-0761
Berrino F, Pasanisi P, Bellati C, Venturelli E, Krogh V, Mastroianni A, Berselli E, Muti P, Secreto G (2005) Serum testosterone levels and breast cancer recurrence. Int J Cancer 113(3):499–502. doi:10.1002/ijc.20582
Lonning P, Helle S, Johannessen D, Ekse D, Aldercreutz H (1996) Influence of plasma estrogen levels on the length of the disease-free interval in postmenopausal women with breast cancer. Br Cancer Res Treat 39:335–341
McTiernan A, Rajan KB, Tworoger SS, Irwin M, Bernstein L, Baumgartner R, Gilliland F, Stanczyk FZ, Yasui Y, Ballard-Barbash R (2003) Adiposity and sex hormones in postmenopausal breast cancer survivors. J Clin Oncol 21(10):1961–1966
Sodergard R, Backstrom T, Shanbhag V, Carstensen H (1982) Calculation of free and bound fractions of testosterone and estradiol-17 beta to human plasma proteins at body temperature. J Steroid Biochem 16(6):801–810
Ma H, Sullivan-Halley J, Smith AW, Neuhouser ML, Alfano CM, Meeske K, George SM, McTiernan A, McKean-Cowdin R, Baumgartner KB, Ballard-Barbash R, Bernstein L (2011) Estrogenic botanical supplements, health-related quality of life, fatigue, and hormone-related symptoms in breast cancer survivors: a HEAL study report. BMC Complement Altern Med 11:109. doi:10.1186/1472-6882-11-109
Doria-Rose VP, Marcus PM (2009) Death certificates provide an adequate source of cause of death information when evaluating lung cancer mortality: an example from the Mayo Lung Project. Lung Cancer 63(2):295–300
Engel LW, Strauchen JA, Chiazze L Jr, Heid M (1980) Accuracy of death certification in an autopsied population with specific attention to malignant neoplasms and vascular diseases. Am J Epidemiol 111(1):99–112
Cox DR (1972) Regression models and life tables (with discussion). JR Stat Soc B 34:187–220
Micheli A, Meneghini E, Secreto G, Berrino F, Venturelli E, Cavalleri A, Camerini T, Di Mauro MG, Cavadini E, De Palo G, Veronesi U, Formelli F (2007) Plasma testosterone and prognosis of postmenopausal breast cancer patients. J Clin Oncol 25(19):2685–2690. doi:10.1200/jco.2006.09.0118
Kaaks R, Rinaldi S, Key TJ et al (2005) Postmenopausal serum androgens, oestrogens and breast cancer risk: the European prospective investigation into cancer and nutrition. Endocr Relat Cancer 12(4):1071–1082
He XY, Liao YD, Yu S, Zhang Y, Wang R (2015) Sex hormone binding globulin and risk of breast cancer in postmenopausal women: a meta-analysis of prospective studies. Horm Metab Res 47(7):485–490. doi:10.1055/s-0034-1395606
Fortunati N, Becchis M, Catalano MG, Comba A, Ferrera P, Raineri M, Berta L, Frairia R (1999) Sex hormone-binding globulin, its membrane receptor, and breast cancer: a new approach to the modulation of estradiol action in neoplastic cells. J Steroid Biochem Mol Biol 69(1–6):473–479
Kahn SM, Li YH, Hryb DJ, Nakhla AM, Romas NA, Cheong J, Rosner W (2008) Sex hormone-binding globulin influences gene expression of LNCaP and MCF-7 cells in response to androgen and estrogen treatment. Adv Exp Med Biol 617:557–564. doi:10.1007/978-0-387-69080-3_57
Fazzari A, Catalano MG, Comba A, Becchis M, Raineri M, Frairia R, Fortunati N (2001) The control of progesterone receptor expression in MCF-7 breast cancer cells: effects of estradiol and sex hormone-binding globulin (SHBG). Mol Cell Endocrinol 172(1–2):31–36
Catalano MG, Frairia R, Boccuzzi G, Fortunati N (2005) Sex hormone-binding globulin antagonizes the anti-apoptotic effect of estradiol in breast cancer cells. Mol Cell Endocrinol 230:31–37
Fortunati N, Catalano MG (2006) Sex hormone-binding globulin (SHBG) and estradiol cross-talk in breast cancer cells. Horm Metab Res 38(4):236–240
Fortunati N, Catalano MG, Boccuzzi G, Frairia R (2010) Sex Hormone-Binding Globulin (SHBG), estradiol and breast cancer. Mol Cell Endocrinol 316(1):86–92. doi:10.1016/j.mce.2009.09.012
Ma H, Wang Y, Sullivan-Halley J, Weiss L, Burkman RT, Simon MS, Malone KE, Strom BL, Ursin G, Marchbanks PA, McDonald JA, Spirtas R, Press MF, Bernstein L (2009) Breast cancer receptor status: do results from a centralized pathology laboratory agree with SEER registry reports? Cancer Epidemiol Biomarkers Prev 18(8):2214–2220. doi:10.1158/1055-9965.epi-09-0301
Acknowledgments
We would like to thank the HEAL participants for their dedication to this study
Funding
National Cancer Institute (N01-CN-75036-20, N01-CN-05228, N01-PC-67010, U54-CA116847, U54CA116848, R25-CA94880); National Institutes of Health (M01-RR-00037); University of New Mexico (NCRR M01-RR-0997); National Institute of Child Health and Human Development (N01-HD-3-3175); California Department of Health Services (050Q-8709-S1528).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Ethical Statement
This study was performed with the approval of the Institutional Review Boards of participating centers in accordance with assurances filed with and approved by the U.S. Department of Health and Human Services.
Rights and permissions
About this article
Cite this article
Duggan, C., Stanczyk, F., Campbell, K. et al. Associations of sex steroid hormones with mortality in women with breast cancer. Breast Cancer Res Treat 155, 559–567 (2016). https://doi.org/10.1007/s10549-016-3704-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3704-4