Abstract
The study investigated the anti-tumour effect of zoledronic acid (ZA) administered alone in a biological window therapy in naïve bone-only metastatic and locally advanced breast cancer (LABC) patients. 33 patients with LABC (Group 1) and 20 patients with a first diagnosis of bone metastasis only (Group 2) received 4 mg single dose of ZA, 14 days (biological window) before starting any treatment. In Group 1, Ki67, CD34, p53/bcl-2 and caspase 3 expression along with the adenosine triphosphate (ATP) levels and RNA disruption index were evaluated as markers of tumor growth in tumour specimens obtained before and after ZA administration (basal, day 14). In Group 2, the total enumeration of circulating tumour cells (CTCs), and of M30+ve CTCs along with the soluble marker of cell death (M30/M65) were carried-out as markers of tumor dissemination at baseline, at 48 h and day 14th. In Group 1, there was a significant reduction in Ki67, CD34, bcl-2 expression after 14 days ZA based-treatment (p = 0.0032; p = 0.0001, p < 0.00001 respectively). ZA showed a significant increase of RNA disruption (p < 0.0076). In Group 2, we observed a significant reduction of CTCs number after 48 h (p = 0.0012), followed by a significant rebound at 14 days (p = 0.012). The apoptotic CTCs/M30+ve and M65 levels significantly increased under treatment (p = 0.018 and p = 0.039 respectively) after drug administration when compared to the baseline. These results are the first prospective in vivo data showing the direct pure anti-tumour effect (either on the tumour cell or on CTCs) of ZA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of metastatic disease is the major cause of death in patients with breast cancer [1]. Metastasizing breast cancer cells disseminate to lymph nodes, peripheral blood, bone marrow and/or other distant sites, in the course of the disease. Metastatic spread often occurs at early stages of the disease and is present in ~30–40 % of patients with apparently a localized disease which will be responsible for the disease progression [2, 3].
Recent preclinical and clinical studies have suggested that bone provides a permissive niche to tumor cell growth, and targeting the interactions within the bone milieu may represent an important strategy to suppress tumor development [4]. Although the precise molecular mechanisms underlying this process remain to be elucidated, it is now increasingly being recognized that the unique characteristics of the bone niche provide homing signals to cancer cells, and create a microenvironment conducive for the cancer cells to colonize. Concomitantly, cancer cells release regulatory factors that result in abnormal bone destruction and/or formation [5]. This bidirectional interaction between the cancer cells and bone microenvironment results in the creation of a “vicious cycle” that increases bone destruction, facilitating the establishment/development of cancer micrometastases. Thus, targeting the pre-metastatic niche, and manipulation of its regulatory mechanisms of indwelling cells may prove highly advantageous in ameliorating the progression of micrometastases and impact on the cancer patients outcome [6].
Bisphosphonates (BP)s have been widely used for the prevention and management of skeletal related event (SRE)s in patients with osteolytic/osteoblastic metastasis. An increasing body of evidence supports their direct and indirect anticancer actions both in vitro and in vivo (reviewed by Clezardin [7]). The BP zoledronic acid (ZA) inhibits tumor cell growth, induces tumor cell apoptosis, and synergizes with chemotherapy and radiotherapy in vitro [8]. Also in vivo, BP induces inhibition of cancer cell proliferation, induction of apoptosis inhibition of angiogenesis, inhibition of tumor migration, invasion, and metastasis, reduction in disseminated tumor cells (DTCs), stimulation of immune surveillance and suppression of bone-derived growth factors [9–14].
However, the clinical evidence of the BPs anti-tumor effect is still under evaluation, although recent data suggest that the addition of ZA to oncologic therapies improves disease response rate and also outcomes in postmenopausal (or receiving ovarian suppression therapy) women with early breast cancer [15]. Thus, the neoadjuvant subgroup analysis of the AZURE trial showed a significant increase in pCRs in patients treated with ZA and the ABCSG-12 and Z/Zo-FAST have shown a disease-free survival benefit with ZA in women receiving adjuvant endocrine therapy [15, 16]. These experimental and clinical findings carry important clinical implications not only for the treatment of bone metastases but also for strategies to reduce the probability of tumor progression [17]. They suggest that BPs should be used early in the clinical management of cancers to positively impact on patients’ survival. Despite these data, the concomitant administration of an active anti-neoplastic treatment is a confounding factor to evaluate the real antitumor effect of ZA.
Therefore in order to elucidate this important clinical issue, we performed a prospective pivotal study to investigate the in vivo role of ZA, administered alone in a “biological window therapy” opportunity in two different settings: Group 1 of breast cancer patients with locally advanced breast cancer and Group 2 of “bone only” metastatic breast cancer patients at their first relapse. The anti-tumor action of ZA was evaluated by analyzing proliferation/angiogenesis/death-rate as markers of tumor growth in Group 1 and circulating tumor cell (CTC) number (total and M30+ve) along with soluble markers of cell death as marker of tumor dissemination in Group 2.
Materials and methods
Patients’ characteristics
Thirty-three patients with locally advanced breast cancer (Group 1) and twenty patients at their first relapse with bone metastasis only (Group 2) were eligible for the study. They had a histologically confirmed solid neoplasm in Group 1 and presence of only bone metastases in Group 2 as evaluated with 18FDG-PET/CT or CT scan identification and radiographic confirmation of bone metastases. Patients’ characteristics are shown in Table 1.
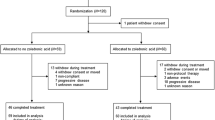
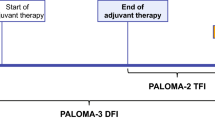
Enrolled patients received 4 mg single dose of ZA (Zometa®, Novartis, Milan, Italya) before starting any treatment (biological window of 14 days) (Fig. 1). All patients were required to have at study inclusion a baseline Eastern Cooperative Oncology Group (ECOG) performance status ≤2, a neutrophil count ≥1.5 × 109/l, a platelet count >100 × 109/l, normal hepatic and renal function as determined by serum creatinine <1.5 times the upper limit of normal and creatinine clearance >60 ml/min and no acute or chronic infections or inflammatory diseases. Patients were considered ineligible for accrual when they had reported fever (body temperature >38.0 °C) during the last week before study entry or had received any radiotherapy, chemotherapy, immunotherapy, or growth factors during the last 4 weeks before study accrual. Any chemotherapy or hormone therapy were excluded during the “biological window” opportunity treatment (2 weeks). During the study period no patient received daily calcium and vitamin D supplementation. All patients received ZA on an out-patients basis and provided written informed consent prior to screening. The institutional review board approved this prospective study (CE Approval Prot 21938/2011LB).
Treatment schedule
Patients received a single dose of 4 mg diluted in 100 ml saline, intravenously, in about 15 min of ZA without any other active concomitant treatments (i.e. chemotherapy or endocrine therapy) (Groups 1 and 2). In patients with locally advanced disease, the biological evaluations were performed at baseline on the diagnostic biopsy and repeated after 14 days from ZA administration on a second tru-cut biopsy (Group 1) whereas in patients with bone metastatic disease, CTCs counts along with serological markers were performed before ZA administration, at 48 h and at 14 days after treatment (Group 2) (Fig. 1).
Immunohistochemistry
Immunohistochemical evaluation was performed on formalin-fixed paraffin-embedded tumor samples obtained at diagnosis and at 14th days on tru-cut. ER, PgR, overexpression of HER2 and Ki67, CD34 with p53 and bcl-2 staining were performed at the Pathology Unit of the Azienda Ospedaliera-Istituti Ospitalieri of Cremona (Italy). The immunohistochemical methodology is fully described elsewhere [18]. The Caspase 3 immunohistochemistry was performed at the Pathology Unit of Peter MacCallum Cancer Centre (Australia) [19].
ATP
ATP content was assayed as previously described [20] using a luminescence assay system (ATPlite, PerkinElmer) according to manufacturing instructions. Briefly, frozen tumor biopsies were minced and homogenized in ice-cold lysis solution provided with the kit using a homogenizer. Membranes and cellular debris were eliminated by centrifuging at 12,000×g for 10 min at 4 °C. Protein concentrations were determined by DC protein-assay (Bio-Rad Laboratories). Equal amounts of tissue proteins from each sample (30 μg/50 μl of lysis solution) were incubated with 50 μl of luciferine/luciferase substrate solution and analyzed for ATP content by using a Luminescence Counter (Enspire, PerkinElemer). ATP concentrations were calculated on the basis of an ATP standard-curve and expressed as pmol/mg protein.
RNA disruption index (RDI)
Tumour samples were shipped in a RNA preservative to Rna Diagnostics (Sudbury, Canada) where they were sub-sectioned based on gross pathology. RNA was then isolated using the Qiagen miRNeasy kit from each portion of the tumour and the RNA analysed using an Agilent Bioanalyzer 2100. Data from the resulting RNA electropherograms were analysed using proprietary algorithms and an RNA Disruption Index (RDI) value was established for each RNA isolate. Mean RDI values were calculated for each tumour sample.
Circulating tumor cells (CTCs) assay
The enumeration of CTC in whole blood was done by the CellSearch System according to manufacturer’s instruction as described by Cristofanilli et al. [21]. Results are expressed as number of cells/7.5 ml of blood. Quality control was maintained via the CellSearch CTC Control Kit used to standardize reagents, instruments, and operator technique.
To quantify the fraction of apoptotic CTC, M30-positive CTC were detected integrating CTC assay with a specific mAb (M30 PEVIVA AB, Bromma, Sweden), recognizing the M30 neoepitope of cytokeratin 18 (CK18), analyzed with the fourth filter of the CellSearch System; results were expressed as the total number of CTC and M30-positive CTC per 7.5 ml of blood as described elsewhere [22].
M30/M65 apoptosense assay
The M30 is a biomarker assay for the quantitative determination of caspase-cleaved cytokeratin 18 (CK18) released from apoptotic carcinoma cells into blood and may estimate the tumour response to the treatment. Total CK18 (cleaved and non cleaved) is detected by M65. Blood samples were collected from patients at the same time-point as indicated for Group 2 into the K2EDTA anticoagulant tubes, and then centrifuged at 1,500 g for 10 min to obtain plasma. Levels of M30 and M65 were measured in blood samples drawn at 8 am before starting ZA administration and thereafter at 48 h and at 14 days after the initial treatment (Fig. 1). M30 and M65 measurements were tested in triplicate accordingly to the manufacturers’ instructions (PEVIVA AB, Bromma, Sweden) as previously described in detail [23].
Statistical analysis
Changes in Ki-67 labelling indices, CD31, p53, bcl-2, caspase 3 expression, CTCs counts, M65 and M30 expression over time were tested with the Wilcoxon signed rank test. Relationships were examined using the Spearman’s rank correlation. All tests were performed two-sided and p values <0.05 were considered statistically significant. Statistics on ATP and RDA values were done with paired t test. All analyses were performed with STATA software system (version 12.1, Taxas, USA: www.stata.com).
Results
Patients’ characteristics and treatment tolerability
Thirty-three patients with locally advanced breast cancer (Group 1) and twenty patients at their first relapse with bone metastasis only (Group 2), were considered eligible for the study. Baseline characteristics of the enrolled patients are summarized in Table 1 Patients were evaluated by physical examination, and blood samples were obtained for laboratory analysis. ZA administration was well tolerated. Mean serum creatinine level did not vary with treatment. ZA administration did not lead significant difference on the levels of bone-turnover markers, as calcium, PTH, BALP and VIT-D3 [1–25]. No patient developed osteonecrosis of the jaw or other significant adverse events.
Markers of tumor proliferation
In Group 1, no clinical variation in tumour size was detected after treatment with ZA. The median Ki67 basal value (18 %; range 3–90) showed a significant decrease after 14 days of ZA infusion (16 %; range 0–90) (p = 0.0032); 22 (66,6 %) patients had a decrease, 6 (18.2 %) had an increase and 5 (15.2 %) were stable in Ki67 expression under treatment (Fig. 2). The median CD34 expression (27 %; range 10–53) at baseline showed a significant reduction in expression after treatment (16 %; range 9–39) (p = 0.0001) (Fig. 2).
Changes in Ki-67 (a), CD34 (b), bcl-2 (c) expression for patients at baseline and post-treatment histology according to treatment received. The large majority of patients randomized receiving ZA showed a suppression of Ki-6, CD34 and bcl-2 expression. Non changes in caspase 3 and p53 expression were noted
With regards to the markers of apoptosis bcl-2 expression also showed a statistically significant decrease (p < 0.00001) from baseline (100 %; range 20–100) to the 14 days (40 %; range 0–80), being decreased in 30 specimens (96.8 %), and increased in only 1 (3.2 %) (Fig. 2). No changes in caspase 3 expression before and after treatment were detected; p53 expression was also not affected (p = 0.3) by the treatment, being unchanged in 27 specimens (87.1 %), increased in 1 (3.2 %) and decreased in 3 (9.7 %) (data not shown).
In 24 analysed matched-pairs samples, the average of ATP value was 230,93 pmol/mg protein at the incisional biopsy and 216.57 pmol/mg protein after administration of ZA, respectively, indicating a slight increase of antitumor activity of ZA detected by the reduction of tumour energy in primary breast cancer. However, the difference between the two groups was not significant (p = 0.79) (data not shown).
Also, in 14 matched-pairs samples, analysing the RDI induced by the treatment after the single administration of ZA showed a significant increase (p < 0.0076) of RDI levels after treatment (baseline: 0.63; range 0.29–0.95; 14 days: 1.21; range 0.53–7.51) suggesting an alteration of RNA integrity by the BP (Fig. 3).
Marker of tumor dissemination
The effects on median alive circulating CTC levels tested at 0, 2 and 14 days after the first ZA infusion were observed. The median CTC basal value (12 cells/7.5 ml of blood; range 0–71) showed an early statistically significant (p = 0.0012) decrease already 48 h after the first ZA infusion (4 cells/7.5 ml of blood; range 0–54). However, after 14 days after ZA infusion there was a rebound of CTC levels (12 cells/7.5 ml of blood; range 0–69) (p = 0.012) (Fig. 3) and thus no difference was noted between baseline and 14 days (p = 0.6574).
With regards to the apoptotic CTCs/M30+ve, the median of basal CTC/M30+ve value (2 cells/7.5 ml of blood; range 0–11) showed a significant increase after treatment: at 14 days (3 cells/7.5 ml of blood; range 0–25) (p = 0.018) (Fig. 3): no significant changes at 48 h (2 cells/7.5 ml of blood; range 0–11) (p = 0.7065) were observed. Significant increase of CTC/M30+ve cells were noted between 48 h and 14 days (p < 0.019).
The levels of M30 and M65 were determined on blood samples of metastatic breast cancer patients (Group 2) collected at baseline, at 48 h and at 14 days after ZA administration at the same time point of CTCs evaluation to assess apoptosis and cell death induced by the treatment. In Group 2, no statistically significant change in serum M30 level was observed before and after ZA treatment (p = 0.9811) or at 48 h after administration (p = 0.2461). M65 levels were statistically significant higher after drug administration (14 days) when compared with the baseline (370,69 U/l versus 335.3 U/l; range 174.2–1646.5 versus 113.7–596.4; p = 0.039). A non-significant increase was detected after 48 h from infusion (p = 0.1128). Serum M30 and M65 levels during ZA treatment are summarized in Fig. 4.
Changes in CTCs at baseline, at 48 h and at 14 days after ZA administration. a Alive CTCs; the number of CTCs decrease after treatment (p = 0.0012) at 48 h; the effect still present after 14 days (p = 0.012) b Apoptotic CTCs/M30+ve; the number of CTC/M30+ve increase after treatment (p = 0.018) at 14 days
Discussion
Zoledronic acid is now the standard clinical care in the management of patients with metastatic bone disease in preventing SRE [24] and evidence from its antitumor activity suggest a further role in the adjuvant treatment of breast cancer to improve the disease free survival [17]. Recent studies have showed the capacity of ZA to improve chemotherapy activity inducing a higher rate of pCR in neoadjuvant setting [15] and, in postmenopausal, to induce a consistent improvement in both DFS and OS [25, 26]. The trend for a higher proportion of patients treated with the combination achieving pCR compared with chemotherapy (CT) alone led to the antitumor hypothesis of ZA in vivo, although the molecular mechanisms behind this synergy remain to be established. Winter et al. [27] have tried to explain the phenomenon analysing the role of ZA on cell growth index (increased apoptosis and reduced proliferation) along with an early greater reduction in serum VEGF with the combination compared with CT only (Fig. 5).
In order to understand the pure anti-tumor activity of ZA along with the possible implicated molecular mechanisms in breast cancer patients our study investigated the biologic effects of ZA in neo-adjuvant setting and “in bone only” metastatic breast cancer at their first relapse administered alone in a “biological window therapy” opportunity.
In neo-adjuvant setting, ZA exerts anti proliferative antitumor activity with a significant reduction of Ki67 after 14 days. These data are aligned with the early reduction of proliferation induced by hormone therapy or CT suggesting a real effect of BP on tumor proliferation [28]. ZA also showed a concomitant reduction of the proliferation of endothelial cells, evaluated by immunohistochemical staining (CD34) confirming in breast cancer patients its anti-angiogenic activity that has already been shown in vitro [29].
Focusing of apoptosis-related markers, our study showed a significant ZA-induced decrease in bcl-2 expression and in p53 and caspase 3 expression after 14 days. This induction of apoptosis includes the activation of the intrinsic mitochondrial pathway leading to a release of cytochrome c into the cytosol where it triggers a number of apoptotic events, including the activation of AIF (Apoptosis Inducing Factor) or caspase 9 which in turn activates caspase 3 and caspase 7 [30, 31]. The unchanged expression of caspase 3 induced by the treatment suggests that the apoptotic event could be dependent on AIF which exits through the mitochondrial membrane, enters the cytosol, and finally ends up in the cell nucleus where it signals the cell to condense chromosomes and fragment its DNA molecules in order to prepare for cell death [32]. In our study, p53 expression was also not affected by the treatment suggesting that ZA could exert cytotoxic effects against p53-mutant cancer cells similar to those against the wt-p53 parental cells [33], demonstrating for the first time in vivo that ZA-induced apoptosis does not involve the p53 signaling cascade.
Nutrient and metabolic molecules as intracellular amino acid and ATP availability are crucial for cell-life and their absence leads to cell-death. We measured the intracellular content of ATP as possible surrogate marker of anti-tumor activity of ZA. Our data showed only a slightly reduction in ATP level at the tumor level induced by a single admonstration of ZA. However, they are in accordance with Fehm et al.’s report [34] who investigated the anti-proliferative effect of ZA in ex vivo resected human breast specimens and compared it with the commonly used chemotherapeutic regimens using an ATP luminescence assay. Knowing that with a larger sample-size the magnitude of the detected ZA effects on ATP levels should be more pronounced, however, our data altogether suggest that ZA seems to induce tumor cell apoptosis via mitochondrial pathway associated via a reduction in ATP levels.
The antitumor effect of ZA was seen also at RNA level where our study showed a significant increase of rRNA disruption after treatment indicating decreased rRNA integrity induced by the administered treatment. These data enforce the previous results related to the antitumor effect of ZA.
We also used a CTC approach in patients at their first relapse with bone metastasis only to understand the anti-tumor effect of ZA. We detected a significant reduction after 48 h only with a slight increase till the 14 days. Concomitantly we have found a significant increase of apoptotic circulating tumor cells marked with M30 (as described before [22]) after 14 days. These data are in agreement with the reports on ZA based-treatment, which showed a reduction of disseminated tumor cells (DTCs) in the bone marrow of patients with breast cancer [35, 36]. ZA showed a decrease in tumor cell proliferation as it occurs under chemotherapy, as early as 24–48 h [37, 41]. The early reduction of viable CTCs/increased of M30+ve CTCs could be explained by the pharmacokinetic of ZA. ZA plasma disposition is multiphasic: half-lives of 0.2 and 1.4 h represent an early rapid decline of peak concentrations from the end of infusion to <1 % of C max at 24 h post-dose during which ZA shows its activity, and half-lifes of 39 and 4,526 h describe subsequent phases of very low concentrations between days 2 and 28 post-dose [38]. Elimination occurs almost exclusively by the kidney. Within 24 h after ZA administration, up to 41 % of the dose infused is excreted un-metabolized in the urine, suggesting that 60 % of the dose is retained in the skeleton or in fat tissue. Bone remodelling processes or fat tissue will slowly release retained ZA back into the systemic circulation where it could exert its activity before being excreted [39].
M30 and M65 are biomarker of apoptosis and they are increasingly used for the evaluation of responses to anti-cancer drugs in several tumor types [40]. In our series M30 did not show a significant change in an early phase or in a late phase under ZA administration. This data is aligned with the late increase of M30+ve CTCS, suggesting that the induction of apoptosis by ZA is a slow process.
Although deregulated control of apoptosis has been suggested to contribute to tumor development and progression in most cancers, increased levels of M65 might indicate that predominant cell death might be caused by necrosis rather than apoptosis in this setting. It has been proven that cells undergo necrosis instead of apoptosis due to insufficient production of ATP [41] and in our series ZA was able to reduce the tumoral ATP level after treatment. In the present study, M30 levels were not statistically modified by the treatment; in contrast, serum M65 levels were associated with significant increase. Increase of cell death, especially necrotic cell death, might be reflecting the ZA activity on the most aggressive behaviour of cancer cells; on the counterpart the induction of apoptosis by ZA is confined to the less aggressive cancer cells. These data, taken together, support the hypothesis that ZA is able to modulate the tumor dissemination reducing the alive CTCs and increasing the apoptotic counterpart, mirroring what found on tumor tissue exposed to ZA in the same biological window treatment.
In conclusion the changes in the analysed biomarkers suggest a critical role of zoledronic acid in anti-tumor proliferation and anti-tumor dissemination maybe due to relevant interactions between ZA, tumor biology and bone microenvironment. Thee data strongly support the use of ZA in combination to oncological treatments in breast cancer patients in order to achieve a better outcome.
References
Manders K, van de Poll-Franse LV, Creemers GJ, Vreugdenhil G, van der Sangen MJ, Nieuwenhuijzen GA et al (2006) Clinical management of women with metastatic breast cancer: a descriptive study according to age group. BMC Cancer 6:179
Braun S, Pantel K, Muller P, Janni W, Hepp F, Kentenich CR et al (2000) Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer. N Engl J Med 342:525–533
Cristofanilli M (2006) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. Semin Oncol 33:S9–S14
Sceneay J, Smyth MJ, Moller A (2013) The pre-metastatic niche: finding common ground. Cancer Metastasis Rev. doi:10.1007/s10555-013-9420-1
Kingsley LA, Fournier PG, Chirgwin JM, Guise TA (2007) Molecular biology of bone metastasis. Mol Cancer Ther 6:2609–2617
Zoccoli A, Iuliani M, Pantano F, Imperatori M, Intagliata S, Vincenzi B et al (2012) Premetastatic niche: ready for new therapeutic interventions? Expert Opin Ther Targets 16(Suppl 2):S119–S129
Clezardin P (2005) Anti-tumour activity of zoledronic acid. Cancer Treat Rev 31(Suppl 3):1–8
Gnant M, Clezardin P (2012) Direct and indirect anticancer activity of bisphosphonates: a brief review of published literature. Cancer Treat Rev 38:407–415
Neville-Webbe HL, Evans CA, Coleman RE, Holen I (2006) Mechanisms of the synergistic interaction between the bisphosphonate zoledronic acid and the chemotherapy agent paclitaxel in breast cancer cells in vitro. Tumour Biol 27:92–103
Ottewell PD, Monkkonen H, Jones M, Lefley DV, Coleman RE, Holen I (2008) Antitumor effects of doxorubicin followed by zoledronic acid in a mouse model of breast cancer. J Natl Cancer Inst 100:1167–1178
Santini D, Vincenzi B, Dicuonzo G, Avvisati G, Massacesi C, Battistoni F et al (2003) Zoledronic acid induces significant and long-lasting modifications of circulating angiogenic factors in cancer patients. Clin Cancer Res 9:2893–2897
Jagdev SP, Coleman RE, Shipman CM, Rostami HA, Croucher PI (2001) The bisphosphonate, zoledronic acid, induces apoptosis of breast cancer cells: evidence for synergy with paclitaxel. Br J Cancer 84:1126–1134
Kunzmann V, Bauer E, Feurle J, Weissinger F, Tony HP, Wilhelm M (2000) Stimulation of gammadelta T cells by aminobisphosphonates and induction of antiplasma cell activity in multiple myeloma. Blood 96:384–392
Aft R, Perez JR, Raje N, Hirsh V, Saad F (2012) Could targeting bone delay cancer progression? Potential mechanisms of action of bisphosphonates. Crit Rev Oncol Hematol 82:233–248
Coleman RE, Winter MC, Cameron D, Bell R, Dodwell D, Keane MM et al (2010) The effects of adding zoledronic acid to neoadjuvant chemotherapy on tumour response: exploratory evidence for direct anti-tumour activity in breast cancer. Br J Cancer 102:1099–1105
Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Heck D, Menzel C et al (2011) Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol 12:631–641
Coleman R, Gnant M, Morgan G, Clezardin P (2012) Effects of bone-targeted agents on cancer progression and mortality. J Natl Cancer Inst 104:1059–1067
Bottini A, Berruti A, Bersiga A, Brizzi MP, Bruzzi P, Aguggini S et al (2001) Relationship between tumour shrinkage and reduction in Ki67 expression after primary chemotherapy in human breast cancer. Br J Cancer 85:1106–1112
Nakopoulou L, Alexandrou P, Stefanaki K, Panayotopoulou E, Lazaris AC, Davaris PS (2001) Immunohistochemical expression of caspase-3 as an adverse indicator of the clinical outcome in human breast cancer. Pathobiology 69:266–273
Fumarola C, La Monica S, Guidotti GG (2005) Amino acid signaling through the mammalian target of rapamycin (mTOR) pathway: role of glutamine and of cell shrinkage. J Cell Physiol 204:155–165
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC et al (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 351:781–791
Rossi E, Basso U, Celadin R, Zilio F, Pucciarelli S, Aieta M et al (2010) M30 neoepitope expression in epithelial cancer: quantification of apoptosis in circulating tumor cells by Cell Search analysis. Clin Cancer Res 16:5233–5243
Come PC, Come SE, Hawley CR, Gwon N, Riley MF (1982) Echocardiographic manifestations of carcinoid heart disease. J Clin Ultrasound 10:233–237
Coleman RE, McCloskey EV (2011) Bisphosphonates in oncology. Bone 49:71–76
Coleman RE, Marshall H, Cameron D, Dodwell D, Burkinshaw R, Keane M et al (2011) Breast-cancer adjuvant therapy with zoledronic acid. N Engl J Med 365:1396–1405
Gnant M, Mlineritsch B, Schippinger W, Luschin-Ebengreuth G, Postlberger S, Menzel C et al (2009) Endocrine therapy plus zoledronic acid in premenopausal breast cancer. N Engl J Med 360:679–691
Winter MC, Wilson C, Syddall SP, Cross SS, Evans A, Ingram CE et al (2013) Neoadjuvant chemotherapy with or without zoledronic acid in early breast cancer–a randomized biomarker pilot study. Clin Cancer Res 19:2755–2765
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J et al (2011) Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer working group. J Natl Cancer Inst 103:1656–1664
Ottewell PD, Woodward JK, Lefley DV, Evans CA, Coleman RE, Holen I (2009) Anticancer mechanisms of doxorubicin and zoledronic acid in breast cancer tumor growth in bone. Mol Cancer Ther 8:2821–2832
Brenner C, Grimm S (2006) The permeability transition pore complex in cancer cell death. Oncogene 25:4744–4756
Garrido C, Galluzzi L, Brunet M, Puig PE, Didelot C, Kroemer G (2006) Mechanisms of cytochrome c release from mitochondria. Cell Death Differ 13:1423–1433
Cande C, Cohen I, Daugas E, Ravagnan L, Larochette N, Zamzami N et al (2002) Apoptosis-inducing factor (AIF): a novel caspase-independent death effector released from mitochondria. Biochimie 84:215–222
Kuroda J, Kimura S, Segawa H, Sato K, Matsumoto S, Nogawa M et al (2004) p53-independent anti-tumor effects of the nitrogen-containing bisphosphonate zoledronic acid. Cancer Sci 95:186–192
Fehm T, Zwirner M, Wallwiener D, Seeger H, Neubauer H (2012) Antitumor activity of zoledronic acid in primary breast cancer cells determined by the ATP tumor chemosensitivity assay. BMC Cancer 12:308
Solomayer EF, Gebauer G, Hirnle P, Janni W, Luck HJ, Becker S et al (2012) Influence of zoledronic acid on disseminated tumor cells in primary breast cancer patients. Ann Oncol 23:2271–2277
Chang J, Ormerod M, Powles TJ, Allred DC, Ashley SE, Dowsett M (2000) Apoptosis and proliferation as predictors of chemotherapy response in patients with breast carcinoma. Cancer 89:2145–2152
Archer CD, Parton M, Smith IE, Ellis PA, Salter J, Ashley S et al (2003) Early changes in apoptosis and proliferation following primary chemotherapy for breast cancer. Br J Cancer 89:1035–1041
Lin JH (1996) Bisphosphonates: a review of their pharmacokinetic properties. Bone 18:75–85
Chen T, Berenson J, Vescio R, Swift R, Gilchick A, Goodin S et al (2002) Pharmacokinetics and pharmacodynamics of zoledronic acid in cancer patients with bone metastases. J Clin Pharmacol 42:1228–1236
Cummings J, Ward TH, LaCasse E, Lefebvre C, St-Jean M, Durkin J et al (2005) Validation of pharmacodynamic assays to evaluate the clinical efficacy of an antisense compound (AEG 35156) targeted to the X-linked inhibitor of apoptosis protein XIAP. Br J Cancer 92:532–538
Leist M, Single B, Naumann H, Fava E, Simon B, Kuhnle S et al (1999) Inhibition of mitochondrial ATP generation by nitric oxide switches apoptosis to necrosis. Exp Cell Res 249:396–403
Acknowledgments
This study was partly funded by Associazione Ricerca in Campo Oncologico Onlus, Cremona, Italy
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Foroni, C., Milan, M., Strina, C. et al. Pure anti-tumor effect of zoledronic acid in naïve bone-only metastatic and locally advanced breast cancer: proof from the “biological window therapy”. Breast Cancer Res Treat 144, 113–121 (2014). https://doi.org/10.1007/s10549-014-2840-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-2840-y