Abstract
Using the M05 mouse mammary tumor model and the MCF-7 cell line, we investigated the effect of tamoxifen treatment on the fraction of breast cancer cells with self-renewing capacity both in vitro and in vivo. We found that pretreatment with 4-OH-tamoxifen leads to an increase in cells with the ability of forming mammospheres that express lower levels of ER-α and increased expression of transcription factors associated with pluripotency. Moreover, exposure on plastic to 4-OH-tamoxifen by itself leads to an upregulation of these transcription factors. M05 tumors grown in mice treated with tamoxifen have a higher percentage of cells with self-renewing capacity and this proportion is conserved when tumors are passaged to nontreated mice. Furthermore, interruption of tamoxifen leads to increased tumor growth compared to tumors grown in mice that were never exposed to the antiestrogen. In addition, these tumors are characterized by a higher number of CD24lCD29h cells compared to tumors grown in nontreated mice. Treatment in vitro with 4-OH-tamoxifen for 5 days leads to a long lasting increase in the proportion of cells with self-renewing capacity even after 1 month of growth in the absence of the antiestrogen. Finally, we compared the mammosphere forming capacity of hormone dependent and independent passages of the M05 tumor and found that hormone independence is associated to an increase in cells with self-renewing capacity. Our results support previous findings that suggest that endocrine treatment selects for cells with stem cell properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Estrogen receptor (ER) positive mammary tumors account for 75 % of breast cancer cases in women around the world [1]. Adjuvant endocrine therapy in the form of tamoxifen or aromatase inhibitors has been the current recommended 5 years therapy. In the case of tamoxifen in particular, approximately 35 % of patients have a recurrence within 15 years of the initial diagnosis [2]. Interestingly recent advances are starting to recommend the use of tamoxifen for 10, rather than 5 years [3]. Thus, understanding the mechanisms that are implicated in endocrine resistance is of great clinical relevance.
Cancer stem cells have gained attention in the last years as responsible for tumor progression and resistance to therapy [4]. Experiments carried out with human samples have clearly shown that both chemo and radiotherapy increase the percentage of breast cancer stem cells in a neo-adjuvant setting [5]. However, endocrine therapy is seldom used in neo-adjuvancy. There are still confusing results regarding the role of 4-OH-tamoxifen and/or estrogen on breast cancer stem cells. Initially, a paper by Fillmore et al. [6] showed that estrogen, through the FGF/Tbx signaling pathway, leads to an increase in breast cancer stem cells. This effect was abrogated by treatment with 4-OH-tamoxifen. Subsequently, Simoes et al. [7] showed results that suggest the contrary: they found that estrogens reduce and 4-OH-tamoxifen increases both the normal mammary and the cancer stem cell populations. Ao et al. [8] at about the same time showed similar results supporting the notion that 4-OH-tamoxifen selects for cells with stem cell properties. In addition, a clinical paper by Creighton et al. [9] reported that neo-adjuvant treatment with letrozol in breast cancer patients leads to an enrichment in cells with a stem cell gene expression signature, associated to tumor initiating and mesenchymal features. Thus, the role of endocrine treatment on the breast cancer stem cell population is still controversial.
We have developed a syngeneic model of endocrine responsive breast cancer from a spontaneous mouse mammary tumor that arose in our animal facility [10]. The M05 mouse mammary tumor is ER positive, estrogen dependent, and sensitive to tamoxifen within the first 9 in vivo passages [10]. From it we developed a continuous epithelial cell line, LM05-E, that is ER-positive and 4-OH-tamoxifen sensitive [11]. This model is thus very useful to investigate both in vitro and in vivo, in an immune competent setting, the impact endocrine treatment has on stem cell populations. Thus, using this system, together with MCF-7 cells, we investigated the effect of 4-OH-tamoxifen treatment on cells with self-renewing capacity. Our results suggest that tamoxifen leads to a selection of cells with stem cell properties, supporting the previous findings by Simoes et al. and Ao et al. [7, 8]. These results may help interpret the high recurrence rate found in the clinic after endocrine treatment is ended.
Materials and methods
Cell culture
The MCF-7 and LM05-E cell lines were routinely maintained in growth medium, consisting of DMEM/F12 medium (Sigma-Aldrich), supplemented with 10 % fetal calf serum (FCS, GenSA, Buenos Aires, Argentina) and gentamicin, in a humidified 5 % CO2/air atmosphere. Serial passages were carried out by treatment of 80 % confluent monolayers with 0.25 % trypsin (Invitrogen) and 0.02 % EDTA in Ca2+ −free and Mg2+ −free PBS. Experiments were carried out with charcoal stripped serum and phenol red free DMEM/F12 as previously described [12].
Reagents
Estradiol and 4-OH-tamoxifen (both from Sigma-Aldrich) were prepared 1,000× in absolute ethanol and used at a final concentration of 10 nM and 1 μM, respectively, [12]. Controls were subjected to the same dilution of absolute ethanol. For in vivo studies 2.5 mg silastic pellets were prepared with tamoxifen citrate (Gador Laboratories, Buenos Aires, Argentina). Empty pellets were used as controls.
Tamoxifen pretreatment for in vitro experiments
LM05-E or MCF-7 cells were cultured for 5 days with 10−8 M estradiol or 10−8 M estradiol plus 10−6 M 4-OH-tamoxifen in DMEM/F12 supplemented with 1 % charcoal stripped FBS. Then, either crystal violet, RT-PCR or mammosphere assays were performed.
Preparation of single mammary tumor cell suspensions from M05 tumors
M05 tumors were minced using razor blades and digested in 5 ml digestion media [digestion buffer containing DMEM/F12, 100 mg/ml gentamycin and 0.15 % collagenase type III (Sigma-Aldrich)]. Samples were incubated at 37 °C for 1 h, while shaking on a rotary shaker. Cells were washed with DMEM/F12 10 % FBS twice or until the supernatant was clear in the presence of DNase (Sigma-Aldrich). Then, a final wash with DMEM/F12 without serum was performed in order to wash serum before cells were used for mammosphere assays or flow cytometry.
Mammosphere assays
Single cells derived from M05 tumors or from LM05-E and MCF-7 cell lines were plated in 6-well low attachment suspension culture plates (Greiner Bio-One, Koln, Germany) or 2 % agarose coated plates (for LM05-E cells) at a density of 10,000–15,000 viable cells/ml. Cells were grown in 2 ml serum-free media, supplemented with B27 (Gemini Bioproducts, California), and 20 ng/ml EGF as previously described [13]. Mammospheres were counted after 5–8 days in culture with a Nikon eclipse TE2000-S inverted microscope.
Flow cytometry
Cells from the LM05-E cell line were trypsinzed, washed, and resuspended in PBS containing 2 % FCS at a concentration of 1.106 cells/ml. Mammospheres were dissociated enzymatically (10 min at 37 °C in 0.05 % trypsin, 0.53 mM EDTA), and mechanically by gently pipetting, and resuspended in PBS with 2 % FCS at a final concentration of 1.106 cells/ml. Cell were labeled under optimized conditions (1:100 for CD29-FITC and 1:300 for CD24-APC and 1:7 for LIN-PE (antibodies were purchased from BioLegend, San Diego, California) during 1 h on ice and were subjected to FACS analysis (PASIII, PARTEC, Munich, Germany).
RT-PCR
RNA from subconfluent monolayers or from mammosphere cultures was prepared using TRIzol® Reagent (Invitrogen Life technologies, Carlsbad, CA, USA). cDNA was prepared with the iScript cDNA synthesis kit (Bio Rad, Richmond, CA, USA). PCR products were obtained by use of the human primers to Nanog, Sox2 and Oct4 previously published by Lengerke et al. [14], and the mouse primers Nanog, Sox2, Oct4 from Zhang et al. [15]. Band densitometry was analyzed using Gel-Pro Analyzer.
Western immunoblot
Protein extracts were prepared by homogenizing cells on ice in RIPA buffer (50 mM Tris, pH 8.0 containing 150 mM NaCl, 0.1 % SDS, 0.5 % deoxycholate, and 1 % NP40) containing protease inhibitors (40 μm phenylmethylsulfonyl fluoride, 5 μg/ml leupeptin, 50 μg/ml aprotinin, and 200 μM orthovanadate) [12]. Protein concentrations were measured using the Bradford method. Samples were mixed with 4× sample buffer containing β-mercaptoethanol and boiled for 2 min. One hundred micrograms of each sample were then separated in SDS-PAGE mini gels (BioRad) and transferred to PVDF membranes (Amersham Biosciences, Sweden). The membranes were blocked overnight in 5 % fat free milk, 0.1 % Tween-20 in PBS at 4 °C. Primary antibodies were used at a 1/200–1/2000 dilution in PBS containing 0.1 % Tween-20 (PBST) and 5 % fat free milk, and were incubated at 4 °C overnight. After washing with PBST, membranes were incubated with secondary antibodies at a 1/1000 dilution for 1 h at room temperature. Signals were detected with an enhanced chemiluminescence kit (ECL, Amersham Biosciences). The following primary antibodies were used: rabbit anti-ER alpha and rabbit anti-E-cadherin (Santa Cruz Biotechnology, Dallas, Texas). The following secondary antibody was used: donkey-antirabbit HRP (Santa Cruz Biotechnology, Dallas, Texas).
Animals
Inbred BALB/c female mice, 2–4 month old were obtained from our Animal Care Division. All animals were kept in metal cages (5–6 per cage) with controlled temperature (22 ± 1 °C) and light exposure of 12 h. Food and water were available ad libitum. Animal care and manipulation were in agreement with institutional guidelines and the Guide for the Care and Use of Laboratory Animals [16].
Histology and immunofluorescence
Specimens were fixed in 10 % formalin, dehydrated, and embedded in paraffin. Sections of approximately 3 μm of thickness were stained with hematoxylin and eosin and examined under a microscope. For immunofluorescence studies frozen tissues were mounted in OCT, and 15–20 μm thick sections were cut using a cryostat. They were air dried and fixed for 20 min in 10 % formalin in PBS. Subsequently, they were permeabilized by incubating in 0.1 % Triton X-100 in PBS for 30 min at 37 °C, and after that nonspecific binding sites were blocked by incubation in blocking buffer (PBS containing 2 % fetal calf serum) for 1 h at room temperature. Sections were then treated with primary antibodies dissolved in blocking buffer at a 1/100 dilution ON at 4 °C. Primary antibodies used were: rabbit anti-ER-α, rabbit anti-E-cadherin, and rabbit anti-pERK (all from Santa Cruz Biotechnology). After 3 washes in PBS sections were incubated with the corresponding fluorescein conjugated secondary antibody, goat antirabbit (1/100 dilution; Zymed, San Francisco, California) for 1 h at room temperature in blocking buffer. Slides were then washed with PBS, and nuclei were stained with propidium iodide and mounted with Vectashield (Vector Laboratories, Burlingame, CA). Sections were analyzed under a Nikon Laser Confocal Microscope.
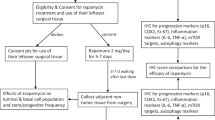
Experiments with the M05 mouse mammary tumor
The original tumor appeared spontaneously in a mammary gland of a 12-months-old virgin inbred female mouse of our BALB/c colony [10]. The M05 tumor is maintained in our laboratory by subcutaneous serial transplants in syngeneic mice performed every 7–8 weeks. Experiments were carried out with passage 8 tumors which are hormone dependent [10] and passage 20 tumors in the case of hormone independence. Tumors were measured once a week with a Vernier caliper in two different planes (height and width). Tumor volume was calculated using the following formula: (width)2 × length/2. Once tumors reached an average size of 10 × 10 mm, silastic pellets containing tamoxifen citrate, or empty pellets as controls, were implanted under general anesthesia by s.c. administration of 0.01 ml/g of body weight of a cocktail of Ketamine (Ketalar, Parke Davis 0.23 mg/ml) and Rompum (Bayer, 0.14 mg/ml). Mice were treated for 30 days and were then sacrificed by cervical dislocation. Tumors were collected and single cell suspensions were prepared as described to be used for mammosphere assays or flow cytometry. To investigate the effect of tamoxifen treatment interruption on tumor growth, tumors derived from tamoxifen and vehicle-treated mice were subsequently passaged to untreated animals. As tumor transplants were carried out using a trocar, each tumor was passaged to five independent mice, and the average size of the five mice was used as the value to plot on the growth curve. Tumors were grown for approximately 60 days before being analyzed by flow cytometry and mammosphere forming capacity.
Statistical analysis
The significance of the differences in the assays was analyzed by Student’s t test or one or two way ANOVA, followed by Tukey’s multiple comparisons test. A value of P < 0.05 was considered significant.
Results
4-OH-tamoxifen leads to an increase in cells with mammosphere forming capacity in MCF-7 and LM05-E cell lines
Cancer treatments such as chemo and radiotherapy have been shown to lead to an increase in cells with stem cell properties such as self-renewing capacity [5]. However, given that endocrine treatments such as tamoxifen are seldom administered in a neo-adjuvant setting, few papers have addressed whether they also select for this particular cell population. To answer this question, we treated the estrogen-dependent LM05-E and MCF-7 cells with 4-OH-tamoxifen for five consecutive days, and then carried out mammosphere assays. As shown in Fig. 1a, b, 4-OH-tamoxifen pretreatment led a to statistically significant increase in cells with self-renewing capacity in both cell lines. Figures c and d show the appearance of mammospheres of MCF-7 and LM05-E cells, respectively, after 6 days in culture. Mammospheres formed defined spheres in both cases. However we noticed, as shown in the picture, that in the case of MCF-7 cells some of the spheres were hollow suggesting that some degree of differentiation was taking place (Fig. 1c). This was never the case for LM05-E cells (Fig. 1d).
4-OH-tamoxifen leads to an increase in breast cancer cells with mammosphere forming capacity. MCF-7 (a) and LM05-E (b) cells were treated for 5 days in the presence of 1 % csFCS+ estradiol 10−8 M (control) or 1 % csFCS+ estradiol 10−8 M+ 4-OH-tamoxifen 10−6 M. They were then tripsinized, washed, and plated on nonadherent 6 well plates at a density of 10,000 and 15,000 cells/ml in mammosphere medium as explained in materials and methods. The graphs show the number of mammospheres/number of cells for each cell line. A statistically significant increase in mammosphere forming capacity was observed in the tamoxifen-treated cells (** P < 0.01). (c, d) Show representative pictures of mammospheres formed by MCF-7 and LM05-E cells, respectively. One of at least three independent experiments is shown. Scale 100 μm
Next we investigated whether 4-OH-tamoxifen increased the expression levels of transcription factors reported to be upregulated in cells with stem cell properties. We found that treatment with 4-OH-tamoxifen of human MCF-7 cells on plastic (2D) was itself capable of moderately increasing the expression Sox 9 (Fig. 2a and Supplementary Fig. 1a). In mouse LM05-E cells, on the other hand, treatment with 4-OH-tamoxifen led to an important increase in Nanog and Oct4 in 2D (Fig. 2b and Supplementary Fig. 1a). MCF-7 mammospheres showed increases in the expression of Nanog, Sox-2 and Slug, and moderate changes in Sox 9 and Oct4 compared to cells on 2D in the absence of 4-OH-tamoxifen (Fig. 2a and Supplementary Fig. 1a). LM05-E mammospheres, on the other hand, showed important increases in levels of Nanog and Oct4 (Fig. 2b and Supplementary Fig. 1b). These results show that treatment with 4-OH-tamoxifen by itself increases the expression of transcription factors associated to stem cell behavior, even for cells growing on 2D monolayers. Moreover, the pretreatment with 4-OH-tamoxifen selected for cells with self-renewing capacity as demonstrated by the mammosphere assays, and these express higher levels of transcription factors associated with pluripotency. We cannot discriminate with these experiments, however, whether 4-OH-tamoxifen increases the expression of genes associated to stemness, or whether the cells that are selected by the treatment have higher expression of these genes.
Changes in transcription factors associated to pluripotency, ER-α and E-cadherin levels in mammospheres. a RNA was extracted and processed for RT-PCR from cells treated for 5 days on plastic with 1 % csFCS+ estradiol 10−8 M (2D), or 1 % csFCS+ estradiol 10−8 M+ 4-OH-tamoxifen (2D + 4-OH-Tam) or from mammospheres. Treatment with 4-OH-tamoxifen on plastic led to an increase in the expression levels of Sox-9 compared to cells not exposed to the antiestrogen. Mammospheres, additionally, showed increases in Nanog as well as in Sox2, Slug and Sox9. One of three experiments is shown. b RNA of LM05-E cells was analyzed for the conditioned explained in A. Treatment with 4-OH-tamoxifen on 2D led to an increase in the levels of Nanog and Oct4. These same genes were upregulated in the mammospheres compared to the cells on 2D. One of two experiments is shown. c Western blot showing a significant decrease in the levels of ER-α in MCF-7 cultured as mammospheres compared to cells on 2D plastic (in the presence of 1 % csFCS+ estradiol 10−8 M). One of at least three experiments is shown. d E-cadherin levels were measured in MCF-7 cells cultured on 2D plastic (in the presence of 1 % csFCS+ estradiol 10−8 M) and in mammospheres. An increase in both the 120 and 100 kDa isoforms was detected. One of at least three experiments is shown
Next, to asses whether 4-OH-tamoxifen affects the self-renewing capacity of breast cancer cells once they were in suspension cultures in conditions to form mammospheres, the antiestrogen was added directly to these without pretreatment. Under these conditions, we did not find any differences in mammosphere forming capacity in either LM05-E or MCF-7 cells (not shown) thus suggesting that only cells that are resistant to 4-OH-tamoxifen are capable of giving rise to mammospheres in suspension cultures. We did notice, however, that in the case of MCF-7 cells, mammospheres were smaller in the presence of 4-OH-tamoxifen and did not last as long in culture (data not shown).
Others have previously reported a downregulation of ER-α and E-cadherin in mammospheres compared to MCF-7 cells cultured in 2D [7]. To test whether we could reproduce these results, protein extracts were prepared from MCF-7 cells cultured in both conditions. We found, as previously reported, that ER-α levels were decreased in the mammospheres compared to the cells on plastic monolayer (Fig. 2c). We also evaluated the levels of E-cadherin and found that in the mammospheres there was an increase in a previously described 100 kDa isoform of this molecule [17], but we did not reproducibly find a decrease in the levels of the 120 kDa isoform (Fig. 2d).
Tamoxifen increases the number of cells with mammosphere forming capacity in the M05 mouse mammary tumor in vivo
We previously showed that the M05 mouse mammary tumor is estrogen dependent and sensitive to tamoxifen [10]. This sensitivity is reflected by a halt in tumor growth upon treatment [10]. Figure 3a shows the H&E stained sections of the M05 tumor before and after treatment. As confirmed by immunofluorescence of frozen sections, tamoxifen leads to a decrease in the epithelial E-cadherin, ER-α positive cell compartment (Fig. 3b). A noticeable decrease in pERK staining supports the halt in tumor growth (Fig. 3b). Thus, as has been previously shown for other hormone responsive mouse mammary tumors [18], the pause in tumor growth is a dynamic process that involves changes within the tumor tissue composition. To assess whether tamoxifen modulates the percentage of cells with self-renewing capacity within the tumors, mice were inoculated with the M05 tumor that was allowed to grow for a month. At that point, mice were treated for an additional month with silastic pellets containing either tamoxifen or no antiestrogen, as a control. Tumors were then removed, and either passaged to mice with no treatment or processed to prepare single cell suspensions as explained in materials and methods. Mammosphere assays of these cell suspensions revealed that treatment with tamoxifen of mice carrying the M05 tumor led to an increase in the amount of cells capable of forming mammospheres (Fig. 4a). Figure 4b shows the appearance of the mammospheres derived from M05 tumors. We did not notice any morphological difference between those derived from tamoxifen or from vehicle-treated mice. On the other hand examination of the growth rate of the tumors passaged to untreated mice showed that tumors derived from mice previously treated with tamoxifen grew significantly faster than those that originated from the control-treated mice (Fig. 4c). Figure 4d shows the largest tumors for both conditions, clearly supporting the data represented in the graph. Finally, mammosphere assays carried out with cells derived from these “secondary” tumors showed that even though the selection pressure had been removed, there was a significant increase in cells capable to form mammospheres (Fig. 4e). Thus our results demonstrate that in the M05 mouse mammary tumor model, in vivo, treatment with tamoxifen leads to the selection of cells with self-renewing capacity and that these cells persist even after the antiestrogen is removed.
Impact of tamoxifen treatment on the M05 tumor. Female BALB/c mice bearing the M05 tumor were treated for 30 days with tamoxifen citrate pellets or vehicle as explained in materials and methods. a H&E stained section of the M05 tumor derived from mice treated with vehicle or tamoxifen. An increase in the stromal compartment can be appreciated in the sample exposed to the antiestrogen. Scale bars 100 μm. b Frozen sections of tumors derived from tamoxifen and vehicle-treated mice show a loss in the epithelial E-cadherin positive compartment (in accordance to what is observed by H&E). Residual epithelial cells are positive for ER-α. pMAPK staining shows a clear reduction in accordance to the halt in tumor growth. Scale bars 50 μm
Tamoxifen leads to an increase in cells with self-renewing capacity in M05 tumors together with increased malignancy. Female BALB/c mice bearing the M05 tumor were treated for 30 days with tamoxifen or vehicle pellets. Tumors were removed and either passaged to mice with no treatment or processed to prepare single cell suspension for mammosphere assays. a Quantification of mammospheres in cultures derived from single cell suspensions derived from tumors grown either in vehicle or tamoxifen-treated mice. A statistically significant increase in mammospheres was detected in those tumors derived from the tamoxifen-treated mice (P < 0.01). b Appearance of mammospheres derived from M05 tumors after 7 days in culture. No morphological differences were seen between those derived from tamoxifen or vehicle-treated mice. One of two independent experiments is shown; a total of 6 tumors per treatment were analyzed. c In vivo growth kinetics of M05 tumors grown in nontreated mice (derived from tamoxifen or vehicle-treated mice as explained in materials and methods). Tumors derived from tamoxifen-treated mice grew at a significantly faster rate than those derived from vehicle-treated mice; P < 0.001. d Representative tumors showing the size difference between treatments. e Mammosphere assays carried out with the tumors generated in c show a statistically significant increase in mammosphere forming capacity in those tumors derived from tamoxifen-treated mice, compared to controls; (P < 0.01). One of three independent experiments is shown, with a total of 8 tumors analyzed per treatment. Scale 100 μm
In vivo treatment with tamoxifen increases the percentage of CD29h/CD24l and decreases the percentage of CD29h/CD24h cells within the M05 tumor
We showed above that treatment with tamoxifen of BALB/c mice carrying the M05 tumor led to an increase in cells capable of forming mammospheres and that this feature was maintained even when the tumors were passaged to untreated mice. Other authors have reported that in the mouse mammary gland, cells with self-renewing capacity are CD29h/CD24l [19, 20]. We analyzed by flow cytometry the percentage of cells with these markers in tumors derived from mice treated with tamoxifen or vehicle. As seen in Fig. 5a and b, tamoxifen led to a statistically significant increase in the population of CD29h/CD24l and a reduction in the CD29h/CD24h cell populations. Figure 5a shows a representative scatter plot for one of these cytometries. Moreover, when we analyzed the tumors that had been passaged to the untreated mice and allowed to regrow this effect was maintained (Fig. 5c, d). Thus, our results show that tamoxifen selects for cells with self-renewing capacity and that this is correlated with an increase in the CD29h/CD24l cell population.
Tamoxifen increases the percentage of CD29hCD24l cells in M05 tumors. Single cell suspensions were prepared from M05 tumors derived from tamoxifen or vehicle-treated mice as explained in Fig. 4. a Representative scatter plot showing the decrease in CD24h cells upon tamoxifen treatment. b Bar graph showing the average of 3 independent tumors, where the increase in CD29hCD24l and the decrease in CD29hCD24l cells are shown (P < 0.05). c Single cell suspensions of tumors passaged to nontreated mice, derived from previously treated as explained in Fig. 4. Even though the treatment was removed, the decrease in CD24h cells remained. d Bar graph showing the average of three independent tumors confirms statistically significant difference even in the absence of treatment (P < 0.05). The results of three independent tumors are shown for each treatment. At least three independent experiments were carried out
Exposure to tamoxifen causes a long lasting selection of cells with mammosphere forming capacity in vitro
Having found both in vitro and in vivo that tamoxifen selects for cells with self-renewing capacity, and that in vivo this effect was maintained when the selection pressure was removed, we wondered whether the regrowth of cells that had been previously treated with 4-OH-tamoxifen in vitro would maintain an increased proportion of cells with self-renewing capacity, or if on the contrary, the original proportions would be restored. To answer this question we treated both MCF-7 and LM05-E cells with 4-OH-tamoxifen for 5 days. We carried out mammosphere assays and obtained results similar to those shown in Fig. 1 (not shown). Next we regrew the cells in growth medium for 1 month and then proceeded to carry out mammosphere assays. As shown in Fig. 6, the increased proportion of cells with self-renewing capacity was maintained even though exposure to 4-OH-tamoxifen had been removed 1 month before for both MCF-7 (Fig. 6a) and LM05-E (Fig. 6b) cells. Our results show that both in vitro and in vivo tamoxifen selects for cells with self-renewing capacity and that when the antiestrogen is removed the proportion of cells with this characteristic is maintained for at least 1 month.
Mammosphere forming capacity of MCF-7 and LM05-E cells is increased after 4-OH-tamoxifen removal. MCF-7 and LM05-E cells were treated for 5 days with 1 % csFCS + estradiol 10−8 M (control) or 1 % csFCS + estradiol 10−8 M + 4-OH-tamoxifen (4-OH-Tam). They were then grown during 1 month in growth medium and subsequently tested for mammosphere forming capacity. Both MCF-7 (a) and LM05-E (b) cells maintain a statistically significant increase in mammosphere forming ability when previously exposed to tamoxifen; P < 0.001. Three independent experiments were carried out for each condition
M05 tumors that have acquired resistance to tamoxifen have a higher proportion of cells with mammosphere forming capacity
We previously showed that the M05 mammary tumor progresses in vivo to tamoxifen resistance around passage 10 [10]. Hormone independent passages of the tumor express estrogen and progesterone receptors and do not differ histologically from the hormone respondent early passages [10]. To investigate whether hormone independent passages of the M05 tumor had an increased proportion of cells with self-renewing capacity compared to the early hormone responsive passages, we prepared cell suspensions from both estrogen dependent and independent tumors and carried out mammosphere assays. Figure 7 shows that there was a statistically significant increase in cells with mammosphere forming capacity in the hormone independent passages suggesting that in these tumors there are more stem/progenitor cells, compared to the responsive M05 tumors.
Tamoxifen resistant passages of the M05 tumor have an increased amount of cells with self-renewing capacity. Single cell suspensions were prepared from hormone dependent (HD) and hormone independent (HI) passages of the M05 tumor. Cells were assayed for mammosphere forming capacity. A statistically significant increase in mammosphere forming capacity was detected in cells derived from hormone independent tumors; ** P < 0.01. The experiment was carried out twice with three tumors per group
Discussion
In the current paper we show that tamoxifen selects for cells with stem cell properties in the human MCF-7 cells line, as well as in mouse LM05-E cells and the M05 tumor from which they derive. Mammosphere assays reveal that pretreatment of either cell line with 4-OH-tamoxifen leads to an increase in cells with increased clonogenicity in suspension. Additionally, we analyzed the gene expression of transcription factors associated with pluripotency and found that they were increased both in the mammospheres and in cells growing on 2D treated with 4-OH-tamoxifen for 5 days. In vivo studies using the M05 tumor showed similar results with an increase in the amount of cells with mammosphere forming capacity in tumors derived from mice treated with tamoxifen containing pellets. These tumors were enriched in CD29h/CD24l cells, in comparison to the parental tumor. Additionally, when passaged to untreated mice, those tumors that derived from mice that had been previously exposed to tamoxifen generated “secondary tumors” that grew at a faster rate compared to controls, and had a higher capacity of giving rise to mammospheres as well as maintaining an increased CD29h/CD24l cell population. Finally, M05 tumor passages that are hormone independent have a higher amount of cells with mammosphere forming capacity supporting the notion that increased aggressiveness and endocrine independence are correlated with an increase in cells with stem cell properties.
Several papers have previously addressed the putative role endocrine treatment could have on stem cell selection in the mammary gland and in breast cancer. However, to date results are still confusing. Initially a paper from Fillmore et al. [6] suggested that estradiol expands the stem cell population in MCF-7 cells. Although these data seem contradictory to ours, a closer analysis of the methods used may suggest that they are actually complementary, or the result of different experimental approaches. In Fillmore’s paper [6] MCF-7 cells were deprived of estradiol for 1 month before being treated with estradiol for 6 days, and then tested for mammosphere forming capacity. This led to approximately 1.75 % stem cells in the culture. Cells deprived of estradiol are known to have increased levels of estrogen receptors and be hypersensitive to hormone treatment [21]. Thus, the fact that in this particular paper, cells were deprived of estradiol for 30 days may account for the obtained results. In our case, we did not deprive the cells of estrogen signaling before pretreating with estradiol; in fact our cells were always maintained in regular FCS, and charcoal stripped serum was used at very low concentrations (1 %) when pretreatments with estradiol were carried out. Under these conditions, about 2 % of the cells were capable of forming mammosphere cultures (similar to Fillmore’s result when treating with estradiol). When adding 4-OH-tamoxifen to the pretreatment the number of mammosphere forming cells increases to approximately 4 % in our conditions, whereas in Fillmore’s 4-OH-tamoxifen was inhibitory. Simoes et al. [7] used a different strategy to analyze the impact of estrogen signaling on MCF-7 mammosphere forming capacity. They plated MCF-7 cells straight onto nonadherent plates and treated the suspension cultures with hormones finding that estradiol decreases, and 4-OH-tamoxifen increases mammosphere forming capacity. The same results were true for suspension cultures of primary human normal and tumor breast cell suspensions, where treatment with 4-OH-tamoxifen lead to an increase in Nanog and Sox-2. Ao et al. [8] on the other hand treated suspension cultures with 4-OH-tamoxifen (1 μM for 2 days) and then passaged the cells to media without antiestrogen (still in suspension) and found that under these conditions a greater amount of mammospheres were formed. Regarding experiments in vivo Fillmore’s paper shows an increase in tumor initiating cells when cells are pretreated with estradiol. Our experimental design was different as we treated tumor-bearing mice with tamoxifen for 30 days, and then assayed the mammosphere forming capacity of cell suspensions prepared from these tumors and the controls. Under these conditions, we found an increase in cells with self-renewing capacity in accordance to our in vitro data and that reported by Ao et al. [8] and Simoes et al. [7]. The CD24l cell population is associated to cells with repopulating capacity in the mouse mammary gland [19], and CD29 has been shown to be a stem cell marker as well [20]. It remains to be determined whether the CD29h/CD24l subpopulation in the normal mammary glands of our mice has stem cell activity. Ao et al. [8] did a similar experiment pretreating the cells in vitro, allowing them to recover for 6 days and then inoculating them to mice using a xenograph model. Under these conditions they did not find differences between the control, estrogen or 4-OH-tamoxifen-treated groups. However, they used higher 4-OH-tamoxifen concentrations and allowed the cells to recover for 6 days, which may account for the differences. Interestingly, the only report testing the effect of neo-adjuvant treatment in patients with letrozole shows that it leads to enrichment in cells with mammosphere forming capacity [9].
In agreement with Simoes et al. [7], Ao et al. [8] and Fillmore et al. [6] we find that mammospheres express lower amounts of ER-α compared to the parental cell line. These results suggest that within the tumor initiating cell population there are different variants some of which express ER-α and others that do not, as previously suggested [7].
Cells with stem cell properties have been characterized by the increase in the expression of transcription factors associated to pluripotency [22]. We found that by only treating cells plated on 2D with 4-OH-tamoxifen several of these genes were upregulated in both MCF-7 and LM05-E cells. These results are in accordance with the fact that pretreatment with 4-OH-tamoxifen leads to an increase in cells with mammosphere forming capacity. However, we cannot at this point differentiate whether 4-OH-tamoxifen actually rises the expression of these genes in the cells, or if the cells that are selected initially had higher expression levels.
Our in vitro results thus suggest that 4-OH-tamoxifen leads to an increase in cells with mammosphere forming capacity and a higher expression of transcription factors associated to pluripotency. Our experiments using the M05 tumor model in vivo show that suspending tamoxifen treatment in this setting leads to the selection of cells with increased growing capacity, mammosphere forming capacity, and higher percentage of CD29h/CD24l cells. In this context, nonetheless, tamoxifen is still for most patients, a very effective treatment. Further studies are necessary to unravel the mechanisms implicated in endocrine resistance and its relation to stem cell biology to find alternatives for those patients that do recur.
References
Sengupta S, Jordan VC (2008) Selective estrogen modulators as an anticancer tool: mechanisms of efficiency and resistance. Adv Exp Med Biol 630:206–219
Osborne CK, Schiff R (2011) Mechanisms of endocrine resistance in breast cancer. Annu Rev Med 62:233–247
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, Abraham M, Medeiros Alencar VH, Badran A, Bonfill X, Bradbury J, Clarke M, Collins R, Davis SR, Delmestri A, Forbes JF, Haddad P, Hou MF, Inbar M, Khaled H, Kielanowska J, Kwan WH, Mathew BS, Mittra I, Muller B, Nicolucci A, Peralta O, Pernas F, Petruzelka L, Pienkowski T, Radhika R, Rajan B, Rubach MT, Tort S, Urrutia G, Valentini M, Wang Y, Peto R, Adjuvant Tamoxifen: Longer Against Shorter Collaborative G (2013) Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet 381(9869):805–816. doi:10.1016/S0140-6736(12)61963-1
Ferrari P, Nicolini A, Carpi A (2013) Targeted therapies of metastatic breast cancer: relationships with cancer stem cells. Biomed Pharmacother 67(6):543–555. doi:10.1016/j.biopha.2013.03.006
Eyler CE, Rich JN (2008) Survival of the fittest: cancer stem cells in therapeutic resistance and angiogenesis. J Clin Oncol 26(17):2839–2845
Fillmore CM, Gupta PB, Rudnick JA, Caballero S, Keller PJ, Lander ES, Kuperwasser C (2010) Estrogen expands breast cancer stem-like cells through paracrine FGF/Tbx3 signaling. Proc Natl Acad Sci USA 107(50):21737–21742. doi:10.1073/pnas.1007863107
Simoes BM, Piva M, Iriondo O, Comaills V, Lopez-Ruiz JA, Zabalza I, Mieza JA, Acinas O, Vivanco MD (2011) Effects of estrogen on the proportion of stem cells in the breast. Breast Cancer Res Treat 129(1):23–35. doi:10.1007/s10549-010-1169-4
Ao A, Morrison BJ, Wang H, Lopez JA, Reynolds BA, Lu J (2011) Response of estrogen receptor-positive breast cancer tumorspheres to antiestrogen treatments. PLoS One 6(4):e18810. doi:10.1371/journal.pone.0018810
Creighton CJ, Li X, Landis M, Dixon JM, Neumeister VM, Sjolund A, Rimm DL, Wong H, Rodriguez A, Herschkowitz JI, Fan C, Zhang X, He X, Pavlick A, Gutierrez MC, Renshaw L, Larionov AA, Faratian D, Hilsenbeck SG, Perou CM, Lewis MT, Rosen JM, Chang JC (2009) Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc Natl Acad Sci USA 106(33):13820–13825. doi:10.1073/pnas.0905718106
Simian M, Manzur T, Rodriguez V, de Kier Joffe EB, Klein S (2009) A spontaneous estrogen dependent, tamoxifen sensitive mouse mammary tumor: a new model system to study hormone-responsiveness in immune competent mice. Breast Cancer Res Treat 113(1):1–8
Pontiggia O, Rodriguez V, Fabris V, Raffo D, Bumaschny V, Fiszman G, de Kier Joffe EB, Simian M (2009) Establishment of an in vitro estrogen-dependent mouse mammary tumor model: a new tool to understand estrogen responsiveness and development of tamoxifen resistance in the context of stromal-epithelial interactions. Breast Cancer Res Treat 116(2):247–255
Pontiggia O, Sampayo R, Raffo D, Motter A, Xu R, Bissell MJ, de Kier Joffe EB, Simian M (2012) The tumor microenvironment modulates tamoxifen resistance in breast cancer: a role for soluble stromal factors and fibronectin through beta1 integrin. Breast Cancer Res Treat 133(2):459–471. doi:10.1007/s10549-011-1766-x
Dontu G, Wicha MS (2005) Survival of mammary stem cells in suspension culture: implications for stem cell biology and neoplasia. J Mammary Gland Biol Neoplasia 10(1):75–86
Lengerke C, Fehm T, Kurth R, Neubauer H, Scheble V, Muller F, Schneider F, Petersen K, Wallwiener D, Kanz L, Fend F, Perner S, Bareiss PM, Staebler A (2011) Expression of the embryonic stem cell marker SOX2 in early-stage breast carcinoma. BMC Cancer 11:42. doi:10.1186/1471-2407-11-42
Zhang L, Luo YB, Bou G, Kong QR, Huan YJ, Zhu J, Wang JY, Li H, Wang F, Shi YQ, Wei YC, Liu ZH (2011) Overexpression Nanog activates pluripotent genes in porcine fetal fibroblasts and nuclear transfer embryos. Anat Rec (Hoboken) 294(11):1809–1817. doi:10.1002/ar.21457
Institute of Laboratory Animal Resources CoLSNRC (1996) Guide for the care and use of laboratory animals national. Academy Press, Washington, DC
Rios-Doria J, Day KC, Kuefer R, Rashid MG, Chinnaiyan AM, Rubin MA, Day ML (2003) The role of calpain in the proteolytic cleavage of E-cadherin in prostate and mammary epithelial cells. J Biol Chem 278(2):1372–1379
Simian M, Molinolo A, Lanari C (2006) Involvement of matrix metalloproteinase activity in hormone-induced mammary tumor regression. Am J Pathol 168(1):270–279. doi:10.2353/ajpath.2006.050012
Sleeman KE, Kendrick H, Robertson D, Isacke CM, Ashworth A, Smalley MJ (2007) Dissociation of estrogen receptor expression and in vivo stem cell activity in the mammary gland. J Cell Biol 176(1):19–26
Taddei I, Deugnier MA, Faraldo MM, Petit V, Bouvard D, Medina D, Fassler R, Thiery JP, Glukhova MA (2008) [beta]1 Integrin deletion from the basal compartment of the mammary epithelium affects stem cells. Nat Cell Biol 10(6):716–722
Martin LA, Farmer I, Johnston SR, Ali S, Marshall C, Dowsett M (2003) Enhanced estrogen receptor (ER) alpha, ERBB2, and MAPK signal transduction pathways operate during the adaptation of MCF-7 cells to long term estrogen deprivation. J Biol Chem 278(33):30458–30468. doi:10.1074/jbc.M305226200
Polyak K, Weinberg RA (2009) Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer 9(4):265–273. doi:10.1038/nrc2620
Acknowledgments
This work is supported by Grants from MINCYT (PICT 2008-0325) and Florencio Fiorini Foundation to MS, Conicet PIP 112 20110100557 grant to LT, and PICT 2010-01296 (MINCYT) and M00243 (UBACyT) to EBKJ.
Conflict of interests
The authors declare they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Laura Todaro, Elisa Bal de Kier Joffé and Marina Simian are members of the Research Career, Consejo Nacional de Investigaciones Científicas y Técnicas.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. S1
Quantification of the changes in levels of transcription factors associated to stemness. a Densitometry of RT-PCR results shown in Fig. 2a corresponding to MCF-7 cells grown on plastic and treated with 4-OH-tamoxifen (2D-4-OH-TAM) or grown as mammospheres. Values are expressed as arbitrary units (A.U.) relative to the levels of GADPH. They are normalized against the bands corresponding to the cells grown on 2D in the absence of 4-OH-Tamoxifen (2D). b The same analysis was carried out for the results obtained with LM05-E cells. (EPS 55300 kb)
Rights and permissions
About this article
Cite this article
Raffo, D., Berardi, D.E., Pontiggia, O. et al. Tamoxifen selects for breast cancer cells with mammosphere forming capacity and increased growth rate. Breast Cancer Res Treat 142, 537–548 (2013). https://doi.org/10.1007/s10549-013-2760-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2760-2