Abstract
Vitamin supplement use after breast cancer diagnosis is common, but little is known about long-term effects on recurrence and survival. We examined postdiagnosis supplement use and risk of death or recurrence in the After Breast Cancer Pooling Project, a consortium of four cohorts of 12,019 breast cancer survivors from the United States and China. Post-treatment supplement use (vitamins A, B, C, D, E, and multivitamins) was assessed 1–5 years postdiagnosis. Associations with risk of recurrence, breast cancer-specific mortality, or total mortality were analyzed in Cox proportional hazards models separately by cohort. Individual cohort results were combined using random effects meta-analysis. Interactions with smoking, treatment, and hormonal status were examined. In multivariate models, vitamin E was associated with a decreased risk of recurrence (RR: 0.88; 95 % CI 0.79–0.99), and vitamin C with decreased risk of death (RR: 0.81; 95 % CI 0.72–0.92). However, when supplements were mutually adjusted, all associations were attenuated. There were no statistically significant associations with breast cancer mortality. The use of antioxidant supplements (multivitamins, vitamin C, or E) was not associated with recurrence, but was associated with a 16 % decreased risk of death (95 % CI 0.72–0.99). In addition, vitamin D was associated with decreased risk of recurrence among ER positive, but not ER negative tumors (p-interaction = 0.01). In this large consortium of breast cancer survivors, post-treatment use of vitamin supplements was not associated with increased risk of recurrence or death. Post-treatment use of antioxidant supplements was associated with improved survival, but the associations with individual supplement were difficult to determine. Stratification by ER status and considering antioxidants as a group may be more clinically relevant when evaluating associations with cancer risk and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Use of vitamin supplements after breast cancer diagnosis is common; 45–80 % of patients use some form of supplement [1]. However, the potential risks and benefits of these supplements remain unclear. The antioxidant effects of some supplements may protect normal tissue during treatment [2]; however, there is concern that these same effects may also protect tumor tissue from the effects of treatment [2]. In addition, the effects of non-antioxidant supplements have not been studied in depth. Therefore, the role of vitamin supplements on risk of recurrence or death among breast cancer survivors remains to be resolved.
Although some studies have investigated specific supplements in relation to breast cancer outcomes [3–9], most have focused on antioxidants and had limited power to simultaneously control for the use of multiple supplements. Therefore, we investigated the associations of antioxidants and other commonly used vitamin supplements on risk of breast cancer recurrence, breast cancer-specific mortality, and total mortality in the After Breast Cancer Pooling Project (ABCPP).
Methods
The After Breast Cancer Pooling Project
The ABCPP is a consortium of four prospective studies of 18,333 stage I–IV breast cancer survivors. Details on the consortium have been published previously [10]. In brief, two cohorts specifically recruited breast cancer patients: the Shanghai Breast Cancer Survival Study (SBCSS) [11] and the Life After Cancer Epidemiology (LACE) Study [12]. The third, the Women’s Healthy Eating and Living (WHEL) Study, was a randomized dietary intervention trial among breast cancer patients [13]. The fourth study included breast cancer patients from the Nurses’ Health Study (NHS), a large prospective study of female nurses [14].
Each cohort collected data on tumor characteristics, cancer treatment, reproductive factors, family history of breast cancer, quality of life, medical history, anthropometry, smoking history, alcohol intake, supplement use, physical activity, and diet. These data have been harmonized into a common dataset. Investigators of each individual cohort received IRB approval from their respective institutions to participate in this collaboration.
Ascertainment of supplement use and covariates
Supplement use
Regular supplement use was assessed through self-report. Because the effects of supplements and use patterns may differ during and after chemotherapy/radiation, we restricted this analysis to regular supplement use (ever vs. never) at least 1-year postdiagnosis. The supplements included in this analysis were those queried by all four studies: multivitamins, vitamins A, B, C, D, and E. Details on how supplements were queried in each study have been published previously [3, 5, 6, 15]. In brief, LACE participants reported supplement use (ever vs. never), postdiagnosis duration, and frequency at study enrollment. Supplements queried included beta-carotene, vitamins A, B, C, D, and E, calcium, and multivitamins [3]. NHS participants were queried about current regular use of multivitamins, vitamins A, C, and E on biennial questionnaires and vitamins D, B, and calcium at least every other questionnaire. For some supplements, women also reported frequency or dose [15]. SBCSS queried women about use of supplements, including vitamins A, B, C, D, E, and multivitamins, at least once a week for 1 month or more at the 6-month and 36-month postdiagnosis interviews, including duration and dose information [5]. In the WHEL study, participants reported the brand and number of supplements that were taken in the previous 24 h at baseline as well as at each follow-up visit [6].
Sociodemographic and lifestyle factors
Data assessed at first postdiagnosis survey included race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Asian, Hispanic, Other), menopausal status at diagnosis (premenopausal, postmenopausal, unknown), and smoking history (never, former, current <25 pack-years, current 25+ pack-years). Body mass index (BMI) was categorized as follows: underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), or obese (≥30.0 kg/m2). Postdiagnosis exercise participation in metabolic equivalents (MET-hours/week) was determined from semiquantitative questionnaires.
Clinical characteristics
Data included age at diagnosis (years), AJCC pathologic stage (I, II, III, IV), ER/PR status (ER+/PR+, ER+/PR−, ER−/PR+, ER−/PR−), and cancer therapy (none, chemotherapy only, radiation therapy only, hormonal therapy only, or some combination of the three therapy types).
Ascertainment of breast cancer outcomes
The main outcomes were breast cancer recurrence, breast cancer-specific mortality, and all-cause mortality. Recurrence was defined as recurrence/metastasis or development of new primary breast cancer. Each cohort followed participants to ascertain breast cancer outcomes. Detailed methods were previously published for each cohort [10]; in brief, outcomes were ascertained through a combination of self-report, medical record review, and linkage to vital statistics registries.
Statistical analysis
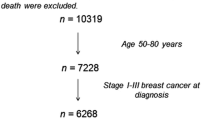
Users of multivitamins were not considered users of single supplements unless they also reported separate use of that supplement. For each supplement, nonusers of that supplement were considered the reference group. Women were excluded from the analysis if they had in situ or stage IV metastatic breast cancer (n = 1,072), they were missing information on any of the supplements (n = 3,608), or did not report on their supplement use in the post-treatment period (n = 11). Because the other cohorts recruited patients after 1990, 1,623 women from NHS who were diagnosed before 1990 were excluded to improve comparability across cohorts. Thus, 12,019 breast cancer survivors were included in the analysis. As sensitivity analyses, we included intervention group as a covariate for the WHEL study, limited the analysis to the US studies, included those missing supplement use as a separate category, and used as the reference group nonusers of any type of supplement or multivitamin.
Delayed-entry Cox proportional hazards regression with time since diagnosis as the time scale was used to estimate study-specific adjusted hazard ratios (HRs), and 95 % confidence intervals (CIs). The entry date was the date of the questionnaire on which supplement use was reported. The exit date was the event date (recurrence or death) or last contact (i.e., date of last survey or registry linkage, whichever was most recent). Studies were combined using random-effects meta-analysis [16]. The Q statistic was used to test for heterogeneity across studies [17]. To test for interactions, we created multiplicative interaction terms in the four studies pooled due to small numbers in the individual studies. All models were adjusted for age at diagnosis, AJCC stage, menopausal status, chemotherapy, radiotherapy, hormonal therapy, BMI, physical activity, and smoking history. We additionally adjusted each supplement for the other supplements to estimate the association with the supplement of interest independent of other supplements.
Results
Characteristics of the ABCPP participants are shown in Table 1 and by cohort in supplemental Table 1. 60.6 % of participants reported supplement use in 1–5 years of postdiagnosis; of these, 27.5 % reported use of a multivitamin only. Supplement users were more likely to be white and meet physical activity recommendations. In contrast, supplement nonusers were more likely to have received chemotherapy and be nonsmokers, but this is likely due to the fact that the 50 % of the nonusers were from SBCSS, where chemotherapy is much more common than in the US cohorts, and smoking is much less. Of the women who died during the study period (N = 1,298), 65 % died due to their breast cancer.
Use of vitamin E was associated with decreased risk of recurrence (HR: 0.88; 95 % CI 0.79–0.99) and suggestively associated with decreased risk of breast cancer-specific death (HR: 0.86; 95 % CI 0.69–1.07) and death due to any cause (HR: 0.85; 95 % CI 0.71–1.03; Table 2). In addition, vitamin C use was associated with a decreased risk of death due to any cause (HR: 0.81; 95 % CI 0.72–0.92), and suggestively associated with decreased risk of recurrence (HR: 0.90; 95 % CI 0.80–1.01) and breast cancer-specific death (HR: 0.87; 95 % CI 0.75–1.01). However, after adjusting for use of other supplements, the associations were attenuated. Since vitamins C and E have antioxidant properties, we examined use of antioxidant supplements (vitamins C, E, or multivitamins) in relation to risk of recurrence, breast cancer-specific mortality, or total mortality. Use of any antioxidant supplement was not associated with recurrence, but was associated with a 16 % decreased risk of death due to any cause (95 % CI 0.72–0.99) in models adjusting for use of other supplements. Women who reported use of all three antioxidant-containing supplements had a 21 % decreased risk of death due to any cause (95 % CI 0.66–0.95). Women who used two types of antioxidants had similar, but nonsignificant associations (HR: 0.75; 95 % CI 0.54–1.05). Results were similar, but not statistically significant for breast cancer-specific mortality.
Analyses limited to the US cohorts yielded results similar to the main analysis; however, power was limited and none of the associations were statistically significant (supplemental Table 2). Results were also similar when women who used none of the supplements were considered the reference group, rather than nonusers of the single supplement of interest (supplemental Table 3). Adjusting for intervention group in the WHEL study did not affect the results (data not shown).
Vitamin D use was associated with decreased risk of recurrence among ER+ (HR: 0.64; 95 % CI 0.47–0.87) but not ER−tumors (HR: 1.25; 95 % CI 0.78–1.98; p-interaction = 0.01; Table 3). When stratified by joint ER/PR status, vitamin D use was only associated with a decreased risk of recurrence among ER+/PR+ and ER+/PR− tumors, but not ER−/PR+ or ER−/PR− tumors (p-interaction = 0.002). However, this low p value was partially driven by an HR of 4.5 in the ER−/PR+ tumors (N = 9 vitamin D users). Because the ER/PR interaction looked very similar to the ER interaction described in this article and there were few subjects in the ER−/PR+ subgroup, we elected to show only the ER stratification results. A similar pattern was observed for risk of breast cancer-specific mortality and total mortality, but the p-interaction was not statistically significant (0.07). We observed no interactions between supplements or by chemotherapy, radiation therapy, smoking, or menopausal status (data not shown).
Discussion
In over 12,000 breast cancer survivors from 4 cohort studies, we observed no increased risk of breast cancer recurrence, breast cancer-specific mortality, or total mortality associated with use of supplements. Vitamin E use was associated with decreased recurrence risk, and vitamin C use was associated with decreased risk of death due to any cause; however, these associations did not retain statistical significance when supplements were mutually adjusted. These findings demonstrate the difficulty of understanding the independent contribution of specific supplements when the use of multiple supplements is common. In contrast, we observed a 15 % risk reduction for use of any antioxidant supplement, with stronger effects among women who used more than one type of antioxidant, suggesting that grouping supplements with similar physiologic effects may better capture the underlying biology. In addition, we found that among ER+ tumors, vitamin D was associated with decreased risk of recurrence, suggesting that the effects of certain supplements may differ by tumor subtype.
Most women (60.6 %) in this study used at least one supplement, and, of these, 59.6 % used multiple supplements. Thus, use of any supplement is correlated with use of other supplements and determining the independent effects of each supplement is difficult. To address this methodologic issue, we examined two reference groups: (1) nonusers of the supplement of interest, and (2) nonusers of any supplement included in this analysis. These two reference groups enabled us to test two somewhat different hypotheses: (1) users of a specific supplement have different risks than nonusers of that supplement, and (2) users of a specific supplement have different risks than women who do not take any supplements. Since results of these two analyses were similar, we used analysis 1 in our main tables and provided results from analysis 2 in supplemental tables. In addition, use of western vitamin supplements is rare in China and reasons for use may differ in China versus the US. If we had pooled the four ABCPP cohorts, most of the nonusers would have been from the SBCSS. We were concerned that a pooled analysis might be biased if the predictors of use versus nonuse of supplements differed by study and were related to breast cancer outcomes. In particular, one potentially important variable, socio-economic status, was not available in the pooled dataset. Therefore, we chose to use meta-analysis to combine studies due to concern about unmeasured confounding by study.
Four previous prospective cohorts have examined supplements and breast cancer prognosis [3–7]; three are ABCPP contributing cohorts. The LACE study found that frequent use of vitamins C and E was associated with decreased recurrence risk, but that carotenoids were associated with increased risk of death [3]. However, the total number of events was low (n = 316 deaths due to any cause). The SBCSS also found reduced risk of recurrence for antioxidant use (multivitamin, vitamin C, or vitamin E), but use of western vitamin supplements was infrequent and that analysis combined supplement use during and after treatment [5]. In the current study, to avoid potential differences in the effects of supplement use during and post-treatment, we focused on supplement use more than 1-year postdiagnosis. The WHEL study examined supplement use in combination with food sources of vitamins and found no association with all-cause mortality [6]. The Iowa Women’s Health Study examined folate from diet and supplements and found no association with all-cause mortality [7]. We do not have detailed information on dietary sources of nutrients in the ABCPP, and therefore could not address whether total intake of specific nutrients is associated with breast cancer outcomes.
The association between supplements and breast cancer survival has also been assessed in two case–control studies. In 220 breast cancer cases from the Boston area, the use of antioxidant supplements (β-carotene, vitamins C or E, or selenium) was associated with a nonsignificant decreased risk of recurrence [8]. However, the number of cases was small, 21 % used proxy respondents and the questionnaire was sent for 10 years after the initial recruitment into the study, raising a concern about the validity of the exposure assessment. A second study examined prediagnostic B-vitamin use among 1,479 breast cancer cases from the Long Island Breast Cancer Study Project [9] and found decreased risk of all-cause and breast cancer-specific mortality among users of vitamins B1 and B3. However, use of vitamin supplements were assessed at baseline to reflect use in the year before breast cancer diagnosis; thus postdiagnosis vitamin use was not included in this study. The ABCPP does not have detailed information on specific types of B vitamins, so we could not attempt to replicate these findings.
Several clinical trials in cancer survivors have found increased risk of death among smokers randomized to receive antioxidant supplements [18–20]. Although these trials were not conducted among breast cancer patients, there is concern that antioxidants may be harmful in breast cancer survivors, particularly those who smoke. In our study, we observed no interaction with smoking. One limitation of our analysis is that we intentionally restricted our analysis to the post-treatment period to remove the potential for different effects of supplement use during and after treatment. Thus, we cannot rule out the possibility that antioxidant supplements may have different effects during active breast cancer treatment versus post-treatment.
Studies of circulating vitamin D levels suggest that higher vitamin D may improve prognosis for several cancer types [21–26], although not always consistently [27–29]. However, studies of vitamin D supplements in cancer patients are limited [30]. We found no overall association with use of vitamin D supplements, but vitamin D was associated with a 46 % decreased risk of breast cancer recurrence among women with ER+ tumors. However, vitamin D from supplements contributes a relatively small amount to the total available vitamin D, compared to sunlight exposure. Two recent studies of breast cancer patients suggested that circulating vitamin D levels were higher in ER+ patients compared with ER-patients [31, 32]. No information on prognosis, however, was available from these two studies. In addition, vitamin D has been associated with BMI [27, 33], suggesting that the role of vitamin D in breast cancer survivors may also differ by adiposity. We found no interaction between vitamin D and BMI in the current study (data not shown). Further, circulating vitamin D levels have been shown to differ between Caucasians and east Asians [34]; therefore, racial differences in total vitamin D should also be accounted for in studies of the role of vitamin D in breast cancer survivors. In the current study, vitamin D supplement use was low in the SBCSS and the US-based studies were >85 % Caucasian; our ability to address potential racial differences was limited. However, when we performed analyses restricted to the US cohorts, we observed very similar results, suggesting that racial differences did not play an important role in the current study. Additional studies, particularly with measurement of circulating vitamin D, incorporating ER status would help to confirm our observed ER–/vitamin D interaction and shed light on the biologic pathways through which vitamin D supplementation may impact ER+, but not ER− tumors.
One limitation of this study is the lack of detailed dose and duration information across studies. For example, not all studies collected dose information and those that did not do so in a consistent manner; in the NHS, dose was not collected in for all supplements on all questionnaires and was collected in wide categories and in various units. In the SBCSS, both the dose and its units were collected for each supplement by write-in; thus units were not consistent within the study. In the WHEL study, total supplement intake was calculated by summing over the ingredients in multivitamins and single supplements, whereas NHS and SBCSS only had dose of single supplements. Dose was not collected in the LACE study. In addition, not all studies collected the same supplements; hence, we could not investigate supplements such as beta-carotene or specific types of B-vitamins. Nevertheless, this is the largest study of postdiagnosis supplement use and breast cancer outcomes to date. Due to the large sample size, we could control for use of multiple supplements simultaneously, obtaining an estimate of the effects of each specific supplement. Further, we could account for important prognostic variables, including stage and treatment, as well as important potential confounders of the associations between supplements and breast cancer outcomes, including body size, smoking, and physical activity.
In summary, post-treatment supplement use was not associated with increased risk of breast cancer recurrence or all-cause mortality. Importantly, grouping supplements by their biologic effects may be a better way of measuring associations with breast cancer prognosis. In addition, it is crucial to consider the concomitant use of other supplements when evaluating effects of specific supplements. Future studies should take dose and duration into account, and specifically evaluate the associations with supplement use during active treatment.
References
Greenlee H, Gammon MD, Abrahamson PE, Gaudet MM, Terry MB, Hershman DL, Desai M, Teitelbaum SL, Neugut AI, Jacobson JS (2009) Prevalence and predictors of antioxidant supplement use during breast cancer treatment: the Long Island Breast Cancer Study Project. Cancer 115:3271–3282. doi:10.1002/cncr.24378
Lawenda BD, Kelly KM, Ladas EJ, Sagar SM, Vickers A, Blumberg JB (2008) Should supplemental antioxidant administration be avoided during chemotherapy and radiation therapy? J Natl Cancer Inst 100:773–783. doi:10.1093/jnci/djn148
Greenlee H, Kwan ML, Kushi LH, Song J, Castillo A, Weltzien E, Quesenberry CP Jr, Caan BJ (2011) Antioxidant supplement use after breast cancer diagnosis and mortality in the Life After Cancer Epidemiology (LACE) cohort. Cancer. doi:10.1002/cncr.26526
Kwan ML, Greenlee H, Lee VS, Castillo A, Gunderson EP, Habel LA, Kushi LH, Sweeney C, Tam EK, Caan BJ (2011) Multivitamin use and breast cancer outcomes in women with early-stage breast cancer: the Life After Cancer Epidemiology study. Breast Cancer Res Treat 130:195–205. doi:10.1007/s10549-011-1557-4
Nechuta S, Lu W, Chen Z, Zheng Y, Gu K, Cai H, Zheng W, Shu XO (2011) Vitamin supplement use during breast cancer treatment and survival: a prospective cohort study. Cancer Epidemiol Biomarkers Prev 20:262–271. doi:10.1158/1055-9965.EPI-10-1072
Saquib J, Rock CL, Natarajan L, Saquib N, Newman VA, Patterson RE, Thomson CA, Al-Delaimy WK, Pierce JP (2011) Dietary intake, supplement use, and survival among women diagnosed with early-stage breast cancer. Nutr Cancer 63:327–333. doi:10.1080/01635581.2011.535957
Sellers TA, Alberts SR, Vierkant RA, Grabrick DM, Cerhan JR, Vachon CM, Olson JE, Kushi LH, Potter JD (2002) High-folate diets and breast cancer survival in a prospective cohort study. Nutr Cancer 44:139–144. doi:10.1207/S15327914NC4402_03
Fleischauer AT, Simonsen N, Arab L (2003) Antioxidant supplements and risk of breast cancer recurrence and breast cancer-related mortality among postmenopausal women. Nutr Cancer 46:15–22
Xu X, Gammon MD, Wetmur JG, Bradshaw PT, Teitelbaum SL, Neugut AI, Santella RM, Chen J (2008) B-vitamin intake, one-carbon metabolism, and survival in a population-based study of women with breast cancer. Cancer Epidemiol Biomarkers Prev 17:2109–2116. doi:10.1158/1055-9965.EPI-07-2900
Nechuta SJ, Caan BJ, Chen WY, Flatt SW, Lu W, Patterson RE, Poole EM, Kwan ML, Chen Z, Weltzien E, Pierce JP, Shu XO (2011) The After Breast Cancer Pooling Project: rationale, methodology, and breast cancer survivor characteristics. Cancer Causes Control 22:1319–1331. doi:10.1007/s10552-011-9805-9
Shu XO, Zheng Y, Cai H, Gu K, Chen Z, Zheng W, Lu W (2009) Soy food intake and breast cancer survival. JAMA 302:2437–2443. doi:10.1001/jama.2009.1783
Caan B, Sternfeld B, Gunderson E, Coates A, Quesenberry C, Slattery ML (2005) Life After Cancer Epidemiology (LACE) Study: a cohort of early stage breast cancer survivors (United States). Cancer Causes Control 16:545–556. doi:10.1007/s10552-004-8340-3
Pierce JP, Natarajan L, Caan BJ, Parker BA, Greenberg ER, Flatt SW, Rock CL, Kealey S, Al-Delaimy WK, Bardwell WA, Carlson RW, Emond JA, Faerber S, Gold EB, Hajek RA, Hollenbach K, Jones LA, Karanja N, Madlensky L, Marshall J, Newman VA, Ritenbaugh C, Thomson CA, Wasserman L, Stefanick ML (2007) Influence of a diet very high in vegetables, fruit, and fiber and low in fat on prognosis following treatment for breast cancer: the Women’s Healthy Eating and Living (WHEL) randomized trial. JAMA 298:289–298. doi:10.1001/jama.298.3.289
Colditz GA, Hankinson SE (2005) The Nurses’ Health Study: lifestyle and health among women. Nat Rev Cancer 5:388–396. doi:10.1038/nrc1608
Cui X, Rosner B, Willett WC, Hankinson SE (2011) Antioxidant intake and risk of endometrial cancer: results from the Nurses’ Health Study. Int J Cancer 128:1169–1178. doi:10.1002/ijc.25425
Smith-Warner SA, Spiegelman D, Ritz J, Albanes D, Beeson WL, Bernstein L, Berrino F, van den Brandt PA, Buring JE, Cho E, Colditz GA, Folsom AR, Freudenheim JL, Giovannucci E, Goldbohm RA, Graham S, Harnack L, Horn-Ross PL, Krogh V, Leitzmann MF, McCullough ML, Miller AB, Rodriguez C, Rohan TE, Schatzkin A, Shore R, Virtanen M, Willett WC, Wolk A, Zeleniuch-Jacquotte A, Zhang SM, Hunter DJ (2006) Methods for pooling results of epidemiologic studies: the Pooling Project of Prospective Studies of Diet and Cancer. Am J Epidemiol 163:1053–1064. doi:10.1093/aje/kwj127
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, Keogh JP, Meyskens FL, Valanis B, Williams JH, Barnhart S, Hammar S (1996) Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med 334:1150–1155. doi:10.1056/NEJM199605023341802
(1994) The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. The Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. N Engl J Med 330:1029–1035. doi:10.1056/NEJM199404143301501
Meyer F, Bairati I, Fortin A, Gelinas M, Nabid A, Brochet F, Tetu B (2008) Interaction between antioxidant vitamin supplementation and cigarette smoking during radiation therapy in relation to long-term effects on recurrence and mortality: a randomized trial among head and neck cancer patients. Int J Cancer 122:1679–1683. doi:10.1002/ijc.23200
Ng K, Meyerhardt JA, Wu K, Feskanich D, Hollis BW, Giovannucci EL, Fuchs CS (2008) Circulating 25-hydroxyvitamin d levels and survival in patients with colorectal cancer. J Clin Oncol 26:2984–2991. doi:10.1200/JCO.2007.15.1027
Ng K, Wolpin BM, Meyerhardt JA, Wu K, Chan AT, Hollis BW, Giovannucci EL, Stampfer MJ, Willett WC, Fuchs CS (2009) Prospective study of predictors of vitamin D status and survival in patients with colorectal cancer. Br J Cancer 101:916–923. doi:10.1038/sj.bjc.6605262
Fedirko V, Riboli E, Tjonneland A, Ferrari P, Olsen A, Bueno-de-Mesquita HB, van Duijnhoven FJ, Norat T, Jansen EH, Dahm CC, Overvad K, Boutron-Ruault MC, Clavel-Chapelon F, Racine A, Lukanova A, Teucher B, Boeing H, Aleksandrova K, Trichopoulou A, Benetou V, Trichopoulos D, Grioni S, Vineis P, Panico S, Palli D, Tumino R, Siersema PD, Peeters PH, Skeie G, Brustad M, Chirlaque MD, Barricarte A, Ramon Quiros J, Sanchez MJ, Dorronsoro M, Bonet C, Palmqvist R, Hallmans G, Key TJ, Crowe F, Khaw KT, Wareham N, Romieu I, McKay J, Wark PA, Romaguera D, Jenab M (2012) Prediagnostic 25-hydroxyvitamin D, VDR and CASR polymorphisms, and survival in patients with colorectal cancer in western European populations. Cancer Epidemiol Biomarkers Prev 21:582–593. doi:10.1158/1055-9965.EPI-11-1065
Ren C, Qiu MZ, Wang DS, Luo HY, Zhang DS, Wang ZQ, Wang FH, Li YH, Zhou ZW, Xu RH (2012) Prognostic effects of 25-hydroxyvitamin D levels in gastric cancer. J Transl Med 10:16. doi:10.1186/1479-5876-10-16
Thomas X, Chelghoum Y, Fanari N, Cannas G (2011) Serum 25-hydroxyvitamin D levels are associated with prognosis in hematological malignancies. Hematology 16:278–283. doi:10.1179/102453311X13085644679908
Goodwin PJ (2009) Vitamin D in cancer patients: above all, do no harm. J Clin Oncol 27:2117–2119. doi:10.1200/JCO.2008.20.8629
Eaton CB, Young A, Allison MA, Robinson J, Martin LW, Kuller LH, Johnson KC, Curb JD, Van Horn L, McTiernan A, Liu S, Manson JE (2011) Prospective association of vitamin D concentrations with mortality in postmenopausal women: results from the Women’s Health Initiative (WHI). Am J Clin Nutr 94:1471–1478. doi:10.3945/ajcn.111.017715
Avenell A, MacLennan GS, Jenkinson DJ, McPherson GC, McDonald AM, Pant PR, Grant AM, Campbell MK, Anderson FH, Cooper C, Francis RM, Gillespie WJ, Robinson CM, Torgerson DJ, Wallace WA (2012) Long-term follow-up for mortality and cancer in a randomized placebo-controlled trial of vitamin D(3) and/or calcium (RECORD trial). J Clin Endocrinol Metab 97:614–622. doi:10.1210/jc.2011-1309
Meyer F, Liu G, Douville P, Samson E, Xu W, Adjei A, Bairati I (2011) Dietary vitamin D intake and serum 25-hydroxyvitamin D level in relation to disease outcomes in head and neck cancer patients. Int J Cancer 128:1741–1746. doi:10.1002/ijc.25496
Giovannucci E, Chan AT (2010) Role of vitamin and mineral supplementation and aspirin use in cancer survivors. J Clin Oncol 28:4081–4085. doi:10.1200/JCO.2009.27.3219
Yao S, Sucheston LE, Millen AE, Johnson CS, Trump DL, Nesline MK, Davis W, Hong CC, McCann SE, Hwang H, Kulkarni S, Edge SB, O’Connor TL, Ambrosone CB (2011) Pretreatment serum concentrations of 25-hydroxyvitamin D and breast cancer prognostic characteristics: a case–control and a case–series study. PLoS ONE 6:e17251. doi:10.1371/journal.pone.0017251
Peppone LJ, Rickles AS, Janelsins MC, Insalaco MR, Skinner KA (2012) The association between breast cancer prognostic indicators and serum 25-OH vitamin D levels. Ann Surg Oncol 19:2590–2599. doi:10.1245/s10434-012-2297-3
Rock CL, Emond JA, Flatt SW, Heath DD, Karanja N, Pakiz B, Sherwood NE, Thomson CA (2012) Weight loss is associated with increased serum 25-hydroxyvitamin D in overweight or obese women. Obesity (Silver Spring). doi:10.1038/oby.2012.57
Gozdzik A, Zhu J, Wong BY, Fu L, Cole DE, Parra EJ (2011) Association of vitamin D binding protein (VDBP) polymorphisms and serum 25(OH)D concentrations in a sample of young Canadian adults of different ancestry. J Steroid Biochem Mol Biol 127:405–412. doi:10.1016/j.jsbmb.2011.05.009
Acknowledgments
The NHS thanks the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, and WY. This study was supported by the National Institutes of Health (R01 CA118229-03S1, R01 CA118229, R01 CA129059, P01 CA87969, and T32 CA009001); the U.S. Army Medical Research and Materiel Command (DAMD 17-02-1-0607); and Susan G. Komen for the Cure (KG100988).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Poole, E.M., Shu, X., Caan, B.J. et al. Postdiagnosis supplement use and breast cancer prognosis in the After Breast Cancer Pooling Project. Breast Cancer Res Treat 139, 529–537 (2013). https://doi.org/10.1007/s10549-013-2548-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2548-4