Abstract
Objective To assess the intraoperative positive sentinel lymph node (SLN) total tumor load (TTL, defined as the amount of CK19 mRNA copies [copies/μL] in all positive SLNs) obtained by one-step nucleic acid amplification (OSNA) and to determine whether it is predictive of non-SLNs involvement. Summary background data The OSNA assay (Sysmex Corporation, Kobe, Japan) is a new diagnostic technique that uses molecular biological techniques to analyze SLN that has been validated as an accurate method for detection of positive SLN. Although the American College of Surgeons Oncology Group Z0011 trial has defined a select cohort of patients in whom a completion axillary lymph node dissection (cALND) may be safely omitted, there are a still a number of patients where prediction of non-SLN metastasis may be helpful for cALND decision making. Multiple studies suggest that specific pathologic characteristics of the primary tumor and the SLN metastases are associated with an increased likelihood of additional positive non-SLN. Methods This is a retrospective multicentric cohort study of 697 patients with cT1-3N0 breast cancer, who had had intraoperative SLN evaluation by OSNA assay with a cALND. TTL is defined as the amount of CK19 mRNA copies number in all positives SLN (copies/μL). Results Univariate logistic regression showed that, in addition to TTL (p < 0.001), the number of affected SLNs (p < 0.001), tumor size (p < 0.001), HER2 status (p = 0.007), and lymphovascular invasion (LVI, p < 0.001) were predictive of ALND status. The multivariate logistic regression analysis showed that TTL is an independent predictor of metastatic non-SLNs, after adjusting for the tumor size, HER2 status, LVI and, in particular, the number of affected SLNs. Conclusions TTL by OSNA is a newly standardized and automated tool that predicts axillary node status better and independently of the number of affected SLNs and the type of surgery. This value can then help clinicians to personalize surgical treatment. Prospective studies will be carried out to determine the clinical impact of this variable in the management of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Axillary lymph node status remains the most powerful prognostic factor in breast cancer [1–3]. Sentinel lymph node (SLN) biopsy is currently the recommended procedure for axillary staging of early breast cancer with clinically negative axilla. It allows for a selective treatment of the axilla, limiting this to patients with involved SLNs [4]. However, despite recommendations from the College of American Pathologists and the American Society of Clinical Oncology, heterogeneity in the approach to SLN evaluation exists [4–6].
The one-step nucleic acid amplification (OSNA) assay (Sysmex Corporation, Kobe, Japan) is a new automatized, standardized, and reproducible diagnostic device that uses molecular biological techniques to analyze SLN [7, 8]. Intraoperative SLN assessed by OSNA has been validated as an accurate method for detection of SLN metastasis compared with conventional histological examination [9–12].
Recently, the American College of Surgeons Oncology Group (ACOSOG) Z0011 trial has defined a select cohort of patients with positive SLN in which a complete axillary lymph node dissection (cALND) may be safely omitted [13]. However, there are still a number of patients where prediction of non-SLN metastasis may be helpful for cALND decision making [14, 15]. Multiple studies have aimed to identify variables predictive of non-SLN metastases to select those patients who can be spared complete ALND (cALND) [16–19]. These suggest that specific pathologic characteristics of the primary tumor and the SLN metastases are associated with an increased likelihood of additional positive non-SLN. Those results led to multiple nomograms that predict axillary involvement. Nevertheless, they show some inconsistencies: first, many of them include features that cannot be used intraoperatively; and second, most of those variables are not easily reproducible.
The aim of this study is to determine whether a new variable, the total tumor load (TTL, defined as the amount of CK19 mRNA copies [copies/μl] in all positive SLNs) obtained by OSNA, which can be assessed intraoperatively and is automated, standardized, and reproducible, is predictive of non-SLNs metastasis in early breast cancer patients.
Methods
Patients
This is a multicentric cohort study. Seven hundred and one consecutive patients with clinically and ultrasonographically node-negative cT1-3 invasive breast cancer, who had undergone intraoperative SLN evaluation by OSNA with a positive finding, were included in the study. Exclusion criteria were patients with ipsilateral breast cancer recurrence, neoadjuvant treatment, and negative CK19 tumors in the preoperative biopsy. The study started in May 2012 when data was collected from medical records of nine Spanish institutions and included age, tumor size and grade, histological subtype, type of surgery, estrogen receptor (ER) and progesterone receptor (PR) status [20], HER2 status [21], Ki67 [22, 23], the presence of lymphovascular invasion (LVI), total number of SLN and non-SLN, the number of positive and negative non-SLNs, size of SLN and non-SLN metastases, and CK19 mRNA number copy/μL in each SLN.
Detection of the SLN
Types of injection and the use of radioisotope with or without blue dye were different depending on the institution [24]. SLNs were sent fresh to the Pathology Department. Levels I and II ALND were performed if the SLNs were positive for micro- or macrometastasis in the intraoperative analysis. Lumpectomy or mastectomy was performed as part of the planned breast cancer treatment.
Intraoperative OSNA evaluation
After the fatty tissue was removed, the SLN was weighed and cut along the short axis. An imprint cytology specimen was performed for morphological correlation. Afterward, the entire lymph node was homogenized with 4 mL of a lysis buffer solution (Lynorhag; Sysmex) and centrifuged at 10,000 × g at room temperature. A 2-μL sample of the supernatant was analyzed with the RD-100i system (Sysmex)—an automated gene-amplification detection system using a reverse transcription loop-mediated isothermal amplification method with the LynoampBC (Sysmex Corporation, Kobe, Japan). The degree of amplification was detected via a byproduct of the reaction. Upon precipitation of magnesium pyrophosphate, the resulting change in turbidity was in turn correlated to CK19 mRNA copy number/μL of the original lysate through a standard curve that was established beforehand with three calibrators containing different CK19 mRNA concentrations. A standard positive control sample containing 5 × 103 copies/μL of CK19 mRNA and a negative control sample not containing any CK19 mRNA were used for validation in every assay. Lymph nodes that exceeded the specified maximum weight of 600 mg were cut into two or more pieces and processed as separate nodes. Four lymph nodes were analyzed in a single run.
Based on the number calculated of CK19 mRNA copies/μL, the result was assessed in accordance with the cutoff level determined by Tsujimoto et al. [7]: macrometastasis (OSNA ++) was defined as >5 × 103 copies/μL of CK19 mRNA, micrometastasis (OSNA +) as 2.5 × 102–5 × 103 copies/μL, and non-metastasis (OSNA −) as <2.5 × 102 copies/μL. The TTL was defined as the amount of CK19 mRNA copy number in all the positive SLNs (copies/μL).
Permanent histology for non-SLN examination
All non-SLNs were sliced to half pieces along the long axis after formalin fixation. One of the cut surfaces was examined with hematoxylin and eosin staining. Immunohistochemical (IHC) staining was not used for evaluation of non-SLNs.
Axillary lymph nodes were staged according to the American Joint Committee on Cancer [25].
Statistical analyses
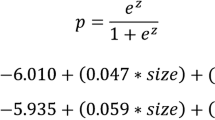
Logistic regression was used to investigate the capacity of TTL (after log transformation, to avoid nonlinearities in the logit) to explain a positive result in the assessment of non-SLN. Other explanatory variables considered in addition to log TTL were the number of affected SLN, patient’s age at surgery, tumor size, histologic type and tumor grade, ER, PR, HER2 receptor status, LVI, and type of surgery. Both uni- and multivariate analyses were conducted. In the multivariate analysis, we used a backward elimination procedure to drop variables that were not significant (p > 0.05) in Wald tests. A post-fit ROC analysis was carried out to identify the best cutoff of TTL.
All analyses were performed using SAS 9.2 for Windows.
Ethical considerations
This study was approved by the Ethics Committee of each participating institution.
Results
A total number of 701 patients were recruited, of which 697 (99.4 %) met the study selection criteria. Four patients were excluded from analysis because of previous chemotherapy or hormonal therapy (two patients) or cALND with less than five lymph nodes analyzed (two patients). All analyses were conducted on the 697 valid patients. Table 1 shows the baseline characteristics of the study sample. The median number of SLN was 2 (range 1–7), and the median number of positive SLN was 1 (range 1–5). The median number of non-SLN was 14 (range 1–42). Two hundred and two patients out of 697 (29.0 %) had positive lymph nodes in the ALND. Micrometastases were found in 19 patients (9.4 %), and macrometastasis in 183 (90.6 %) of the 202 patients. Four hundred and sixty three (66.4 %) patients had just one positive SLN, 166 (23.8 %) had two, 51 (7.3 %) had three, 16 (2.3 %) had four and one (0.1 %) had five positive SLNs. Five hundred and ninety five patients (85.3 %) were classified as pN1; 77 (11.0 %) as pN2; and 24 (3.4 %) as pN3.
When classified by molecular subtypes according to St. Gallen’s recommendations for classifying intrinsic subtypes of breast cancer [23], the highest frequency of positive non-SLN was observed in the HER2-enriched tumors (9/22, 59.1 %), followed by Luminal B-HER2 (22/62, 35.5 %), Luminal B (83/274, 30.3 %), Luminal A (77/298, 25.8 %), and triple negative (7/40, 17.5 %).
Uni- and multivariate logistic regression analyses
Univariate logistic regression showed that, in addition to (log) TTL (p < 0.001), the number of affected SLN (p < 0.001), tumor size (p < 0.001), HER2 status (p = 0.007), and LVI (p < 0.001) were associated to non-SLN metastases. Histological type did not reach a statistically significant result (p = 0.051), although patients with invasive lobular carcinoma (ILC) or -ductal carcinoma (IDC) seemed to show higher odds of positive cALND as compared with patients with other types of carcinoma. Even if grade III tumors had higher odds ratio (OR) than grades I or II, the overall grade effect was not statistically significant (p = 0.182). PR-positive tumors had lower OR of positive cALND as compared with PR-negative tumors (0.77 [0.52–1.15]) although the result failed to reach statistical significance (p = 0.203). Age and ER were clearly unrelated to non-SLN status (Table 2).
Multivariate logistic regression analysis: predictive model
The reduced model containing only variables available by the time of surgery (log TTL, HER2, and the number of affected SLN) produced a good overall fit and effect estimates that were similar to those observed in the previous explanatory model (Table 3). The multivariate logistic regression analysis showed that (log) TTL is an independent predictor of metastatic non-SLNs, after adjusting for the tumor size, HER2 status, LVI, and, in particular, the number of affected SLNs.
The ROC curve analysis showed that, as compared with the number of affected SLN, (log) TTL has a better ROC curve, as measured by the area under curve (AUC) (Fig. 1): (log) TTL 0.709 (95 % confidence interval [CI] 0.667–0.760); number of affected SLN 0.610 (95 % CI 0.570–0.652); p < 0.001 (Table 3).
Cut-point for log TLL
If we divide TTL in micro- and macrometastasis independent of the number of SLNs affected, from the 225 patients in whom TTL would be classified as micrometastasis, 28 (12.44 %) had further axillary involvement, compared with 174 (33.86 %) out of 472 patients in the group of macrometastasis (p < 0.001).
We then chose a cutoff point for TTL so as to reduce the probability of patients included as much as possible, while keeping an acceptably high negative predictive value (NPV) value. The chosen cutoff point was TTL = 15,000 (corresponding to [log] TTL = 4.1761) that had a NPV = 85.5 (95 % CI 81.0–88.8), positive predictive value (PPV) = 41.1 (95 % CI 36.3–46.1), sensitivity 76.7 (95 % CI 70.4–82.0), and specificity = 55.2 (95 % CI 50.7–59.5).
Discussion
Since the first description of breast SLN in 1993, it has been difficult to reach consensus on SLN standardization of evaluation [26]. Controversies and inconsistencies regarding the pathological work-up of SLNs led the European Working Group for Breast Screening Pathology to review the different protocols in 2003, finding multiple differences between institutions [27]. Intraoperative conventional histopathological examinations are then non-standardized and limited in their ability to detect metastasis because of the partial evaluation of the node. The evaluation of SLN by step-sectioning procedure, with or without IHC staining, has outperformed the false negative intraoperative rates.
The OSNA assay has been reported as a new standardized intraoperative technique that evaluates, for the first time, the whole SLN intraoperatively [28], thereby avoiding sampling errors and second-time surgeries due to false negative results. Validation studies published to date are consistent with a reliable quantitative test that allows final decisions related to axillary treatment of patients. The results are output automatically not only in a semiquantitative manner (− [negative] for CK19 mRNA copy numbers less than 250/μL; + [micrometastasis] for copy numbers between 250 and 5,000/μL; and ++ [macrometastasis] for copy numbers greater than 5,000/μL) but also as a continuous variable in the form of tumor load (CK19 mRNA copy number).
However, surgical implications of positive SLNs is under debate and discussion after the ACOSOG Z0011 trial demonstrated no difference in overall survival or locoregional recurrence rates between patients planned for breast conservation therapy including whole breast irradiation with one or two positive SLNs randomly selected to undergo axillary cALND versus no further surgery [13]. Although the Z0011 trial was expected to be “practice-changing,” controversies worth nothing still remain. One important point of debate regarding this trial is the applicability of the results to subsets of patients who were underrepresented or undefined in the trial such as young patients, patients with lobular histology, hormone receptor negative tumors, or HER2 positive tumors. Furthermore, contradicting results have been published recently, including the current analysis of the Dutch MIRROR cohort study, which showed an increased 5-year regional recurrence rate in patients with micrometastases in their SLN and no cALND performed [29]. This has made several institutions adapt Z0011 recommendations and still perform cALND in patients meeting the trial inclusion criteria. A recent article from Caudle et al. [14], reflects the impact of this trial in their institution, where the number of cALND in patients with positive SLN meeting ACOSOG Z0011 criteria has decreased from 85 to 24 % and intraoperative analyses of the SLN from 69 to 26 %. Reasons for performing still a cALND were based on tumor size, lobular histology, number of SLN, size of the SLN metastasis, extracapsular extension, and higher probability of positive non-SLNs based on their nomogram.
The use of nomograms to predict axillary involvement can then be helpful in guiding to make decisions for patients who meet Z0011 eligibility criteria but may not completely meet the characteristics of those who were enrolled on the trial or groups that were under-represented or even not represented in the trial. Van la Parra et al. performed a meta-analysis to identify the clinicopathological variables most predictive of non-sentinel node metastasis. They defined eight main factors: method of detection, SLN metastases >2 mm in size, extracapsular extension in the SLN, >1 positive SLN, 1 negative SLN, tumour size >2 cm, ratio of positive sentinel nodes >50 %, and LVI in the primary tumour [16]. Meretoja et al. [30] recently published a new tool to predict the risk of non-SLN metastases where HER2 status and histological and nuclear grade also seem to play an important role.
TTL, assessed by the OSNA assay, is a new value than, exclusively by itself, is able to predict the likelihood of more axillary metastasis. Even if its predictive value is lower than other nomograms (AUC = 0.709 vs 0.80 of the most widely used model—the nomogram developed by Van Zee et al. [17] at Memorial Sloan-Kettering Cancer Center, after incorporating the SLN metastasis size [19] −), TTL is automatized, reproducible, and can be assessed intraoperatively. Another important point is that, compared with the number of positive SLNs, the TTL is independent of the number of metastatic SLNs and a better predictor of further nodal metastasis. Furthermore, it is not correlated with the type of surgery and/or the histological tumor subtype (IDC vs ILC vs others). This value can then be helpful in guiding to make decisions for patients who do not completely meet Z0011 eligibility criteria or for groups who were under-represented (e.g., in our study 73 [10.5 %] had an ILC and 84 [12.1 %] were HER2 positive).
Even if establishing specific cutoff-points can be questionable because they may change in the future and increasingly become more patient specific, we have seen that TTL = 15,000 could be a good candidate because of its high NPV, PPV, sensitivity, and specificity. Compared with Z0011 where the rate of positive non-SLNs was 27 %, just 14.7 % patients with TTL <15,000 had other positive non-SLNs and 41 % of patients with 1 or 2 positive SLNs with TTL >15,000 had other positive non-SLNs. Furthermore, taking this value as a cutoff point, 92 (13.2 %) patients who were not meeting Z0011 eligibility criteria (85 patients with mastectomy and 7 patients with ≥3 positive SLN) had a TTL <15,000, and so they may have spared a cALND considering the predictive results of the TTL and the low risk of other positive non-SLN.
In conclusion, this study is the largest to date that demonstrates that TTL by OSNA is a newly standardized and automated tool that predicts axillary node status better and independently of the number of affected SLNs. Prospective studies will be carried out to determine the clinical impact of this variable in terms of locoregional recurrence and overall survival in the management of patients.
References
Weaver DL, Ashikaga T, Krag DN, Skelly JM, Anderson SJ, Harlow SP, Julian TB, Mamounas EP, Wolmark N (2011) Effect of occult metastases on survival in node-negative breast cancer. N Engl J Med 364(5):412–421
Fisher B, Bauer M, Wickerham DL, Redmond CK, Fisher ER, Cruz AB, Foster R, Gardner B, Lerner H, Margolese R et al (1983) Relation of number of positive axillary nodes to the prognosis of patients with primary breast cancer. An NSABP update. Cancer 52(9):1551–1557
Michaelson JS, Silverstein M, Sgroi D, Cheongsiatmoy JA, Taghian A, Powell S, Hughes K, Comegno A, Tanabe KK, Smith B (2003) The effect of tumor size and lymph node status on breast carcinoma lethality. Cancer 98(10):2133–2143
Lyman GH, Giuliano AE, Somerfield MR, Benson AB III, Bodurka DC, Burstein HJ, Cochran AJ, Cody HS III, Edge SB, Galper S et al (2005) American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol 23(30):7703–7720
Weaver DL (2010) Pathology evaluation of sentinel lymph nodes in breast cancer: protocol recommendations and rationale. Mod Pathol 23(Suppl 2):S26–S32
Cserni G, Amendoeira I, Apostolikas N, Bellocq JP, Bianchi S, Bussolati G, Boecker W, Borisch B, Connolly CE, Decker T et al (2003) Pathological work-up of sentinel lymph nodes in breast cancer. Review of current data to be considered for the formulation of guidelines. Eur J Cancer 39(12):1654–1667
Tsujimoto M, Nakabayashi K, Yoshidome K, Kaneko T, Iwase T, Akiyama F, Kato Y, Tsuda H, Ueda S, Sato K et al (2007) One-step nucleic acid amplification for intraoperative detection of lymph node metastasis in breast cancer patients. Clin Cancer Res 13(16):4807–4816
Tamaki Y, Akiyama F, Iwase T, Kaneko T, Tsuda H, Sato K, Ueda S, Mano M, Masuda N, Takeda M et al (2009) Molecular detection of lymph node metastases in breast cancer patients: results of a multicenter trial using the one-step nucleic acid amplification assay. Clin Cancer Res 15(8):2879–2884
Visser M, Jiwa M, Horstman A, Brink AA, Pol RP, van Diest P, Snijders PJ, Meijer CJ (2008) Intra-operative rapid diagnostic method based on CK19 mRNA expression for the detection of lymph node metastases in breast cancer. Int J Cancer 122(11):2562–2567
Tamaki Y, Sato N, Homma K, Takabatake D, Nishimura R, Tsujimoto M, Yoshidome K, Tsuda H, Kinoshita T, Kato H et al (2012) Routine clinical use of the one-step nucleic acid amplification assay for detection of sentinel lymph node metastases in breast cancer patients: results of a multicenter study in Japan. Cancer 118(14):3477–3483
Snook KL, Layer GT, Jackson PA, de Vries CS, Shousha S, Sinnett HD, Nigar E, Singhal H, Chia Y, Cunnick G et al (2011) Multicentre evaluation of intraoperative molecular analysis of sentinel lymph nodes in breast carcinoma. Br J Surg 98(4):527–535
Feldman S, Krishnamurthy S, Gillanders W, Gittleman M, Beitsch PD, Young PR, Streck CJ, Whitworth PW, Levine EA, Boolbol S et al (2011) A novel automated assay for the rapid identification of metastatic breast carcinoma in sentinel lymph nodes. Cancer 117(12):2599–2607
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, McCall LM, Morrow M (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305(6):569–575
Caudle AS, Hunt KK, Tucker SL, Hoffman K, Gainer SM, Lucci A, Kuerer HM, Meric-Bernstam F, Shah R, Babiera GV et al (2012) American College of Surgeons Oncology Group (ACOSOG) Z0011: impact on surgeon practice patterns. Ann Surg Oncol 19(10):3144–3151
Gainer SM, Hunt KK, Beitsch P, Caudle AS, Mittendorf EA, Lucci A (2012) Changing Behavior in Clinical Practice in Response to the ACOSOG Z0011 Trial: a survey of the American Society of Breast Surgeons. Ann Surg Oncol 19(10):3152–3158
van la Parra RF, Peer PG, Ernst MF, Bosscha K (2011) Meta-analysis of predictive factors for non-sentinel lymph node metastases in breast cancer patients with a positive SLN. Eur J Surg Oncol 37(4):290–299
Van Zee KJ, Manasseh DM, Bevilacqua JL, Boolbol SK, Fey JV, Tan LK, Borgen PI, Cody HS III, Kattan MW (2003) A nomogram for predicting the likelihood of additional nodal metastases in breast cancer patients with a positive sentinel node biopsy. Ann Surg Oncol 10(10):1140–1151
Houvenaeghel G, Nos C, Giard S, Mignotte H, Esterni B, Jacquemier J, Buttarelli M, Classe JM, Cohen M, Rouanet P et al (2009) A nomogram predictive of non-sentinel lymph node involvement in breast cancer patients with a sentinel lymph node micrometastasis. Eur J Surg Oncol 35(7):690–695
Mittendorf EA, Hunt KK, Boughey JC, Bassett R, Degnim AC, Harrell R, Yi M, Meric-Bernstam F, Ross MI, Babiera GV et al (2012) Incorporation of sentinel lymph node metastasis size into a nomogram predicting nonsentinel lymph node involvement in breast cancer patients with a positive sentinel lymph node. Ann Surg 255(1):109–115
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M et al (2010) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28(16):2784–2795
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A et al (2007) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 25(1):118–145
Dowsett M, Nielsen TO, A’Hern R, Bartlett J, Coombes RC, Cuzick J, Ellis M, Henry NL, Hugh JC, Lively T et al (2011) Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer Working Group. J Natl Cancer Inst 103(22):1656–1664
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ, Members P (2011) Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 22(8):1736–1747
Rubio IT, Aznar F, Lirola J, Peg V, Xercavins J (2010) Intraoperative assessment of sentinel lymph nodes after neoadjuvant chemotherapy in patients with breast cancer. Ann Surg Oncol 17(1):235–239
Edge SB, Byrd DR, Compton CC, Fritz AG et al (2010) AJCC cancer staging manual, 7th edn. Springer, New York
Krag DN, Weaver DL, Alex JC, Fairbank JT (1993) Surgical resection and radiolocalization of the sentinel lymph node in breast cancer using a gamma probe. Surg Oncol 2(6):335–339; discussion 340
Cserni G, Amendoeira I, Apostolikas N, Bellocq JP, Bianchi S, Boecker W, Borisch B, Connolly CE, Decker T, Dervan P et al (2004) Discrepancies in current practice of pathological evaluation of sentinel lymph nodes in breast cancer. Results of a questionnaire based survey by the European Working Group for Breast Screening Pathology. J Clin Pathol 57(7):695–701
Cserni G (2012) Intraoperative analysis of sentinel lymph nodes in breast cancer by one-step nucleic acid amplification. J Clin Pathol 65(3):193–199
Pepels MJ, de Boer M, Bult P, van Dijck JA, van Deurzen CH, Menke-Pluymers MB, van Diest PJ, Borm GF, Tjan-Heijnen VC (2012) Regional recurrence in breast cancer patients with sentinel node micrometastases and isolated tumor cells. Ann Surg 255(1):116–121
Meretoja TJ, Leidenius MH, Heikkilä PS, Boross G, Sejben I, Regitnig P, Luschin-Ebengreuth G, Zgajnar J, Perhavec A, Gazic B et al (2012) International multicenter tool to predict the risk of nonsentinel node metastases in breast cancer. J Natl Cancer Inst 104(24):1888–1896. doi:10.1093/jnci/djs455
Acknowledgments
This study was supported by a Grant from the Sysmex España S.L. The sponsor had no role in the study design, analysis, or interpretation of the data.
Conflict of interest
All authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Peg, V., Espinosa-Bravo, M., Vieites, B. et al. Intraoperative molecular analysis of total tumor load in sentinel lymph node: a new predictor of axillary status in early breast cancer patients. Breast Cancer Res Treat 139, 87–93 (2013). https://doi.org/10.1007/s10549-013-2524-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2524-z