Abstract
Bloom’s syndrome is a rare autosomal recessive chromosomal instability disorder with a high incidence of various types of neoplasia, including breast cancer. Whether monoallelic BLM mutations predispose to breast cancer has been a long-standing question. A nonsense mutation, p.Q548X, has recently been associated with an increased risk for breast cancer in a Russian case–control study. In the present work, we have investigated the prevalence of this Slavic BLM founder mutation in a total of 3,188 breast cancer cases and 2,458 controls from Bashkortostan, Belarus, Ukraine, and Kazakhstan. The p.Q548X allele was most frequent in Russian patients (0.8 %) but was also prevalent in Byelorussian and Ukrainian patients (0.5 and 0.6 %, respectively), whereas it was absent in Altaic or other non-European subpopulations. In a combined analysis of our four case–control series, the p.Q548X mutation was significantly associated with breast cancer (Mantel–Haenszel OR 5.1, 95 % CI 1.2; 21.9, p = 0.03). A meta-analysis with the previous study from the St. Petersburg area corroborates the association (OR 5.7, 95 % CI 2.0; 15.9, p = 3.7 × 10−4). A meta-analysis for all published truncating mutations further supports the association of BLM with breast cancer, with an estimated two- to five-fold increase in risk (OR 3.3, 95 %CI 1.9; 5.6, p = 1.9 × 10−5). Altogether, these data indicate that BLM is not only a gene for Bloom’s syndrome but also might represent a breast cancer susceptibility gene.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Familial risk of breast cancer is associated with high- to moderate-penetrance mutations in genes encoding DNA double-strand break sensors and repair proteins, such as BRCA1, BRCA2, PALB2, ATM, NBN, and others [1–3]. The hitherto known susceptibility genes account for only part of the familial clustering, and remaining cases could thus be explained by mutations in further genes acting in the same biological pathways. One candidate is BLM, the gene mutated in Bloom’s syndrome [4].
Bloom’s syndrome is a rare autosomal recessive disorder characterized by sunlight sensitivity, short stature, and a very high incidence of various types of neoplasia, including breast cancer [5]. Cells from patients with Bloom’s syndrome exhibit chromosomal instability characterized by an elevated rate of sister chromatid exchanges and quadriradial configurations [6]. By exploiting this hyper-recombination phenotype, the underlying gene, BLM, had been isolated through a positional cloning strategy, and its gene product was found to have homology to the RecQ subfamily of DNA helicases [7].
The BLM protein rapidly localizes to DNA breaks after irradiation in an ATM-dependent manner [8–10]. BLM is part of the BRCA1-associated genome surveillance complex, BASC [11], and interacts with the DNA resection machinery that is guided by the MRE11-RAD50-NBN complex [12]. It has further been implicated in homologous recombinational repair and the Fanconi anemia pathway through interaction with RAD51, RAD51D, and FANCJ [13–16]. During mitosis, BLM appears to be required for proper chromosome segregation and the resolution of anaphase bridges [17].
Bloom′s syndrome is frequent in the Ashkenazim population [18]. There the predominant mutation, referred to as “BLM Ash,” is a 6-bp deletion and 7-bp insertion at nucleotide position 2281 in the BLM cDNA [7]. While homozygosity for the BLM Ash mutation causes Bloom’s syndrome, its possible role as a cancer susceptibility allele in heterozygotes has been difficult to prove [19–21]. There is renewed interest in this matter since a nonsense mutation, p.Q548X, has recently been identified as another common BLM mutation and has been associated with an increased risk for breast cancer in a Russian case–control study [22]. In the present study, we have investigated the prevalence of this Slavic BLM founder mutation in four different populations from Eastern Europe and Eurasia, including two large hospital-based series of breast cancer patients from Bashkortostan and from Belarus.
Patients and methods
Patients
We investigated two large case–control series from Bashkortostan, Russia, and from Belarus. Both series have been previously used for breast cancer association studies [23–25]. The series from Russia consisted of 1,059 breast cancer patients unselected for family history who had been diagnosed during the years 2000–2007 at the oncological center in Ufa (Bashkortostan). Breast cancer patients in this series belonged to different ethnic groups mainly living in the Volga Ural region of Russia, and included 453 Russians, 257 Tatars, 128 Bashkirs, 67 Ukrainians, also 60 Yakuts from Siberia, and 94 patients of other or mixed ancestry. Median age at diagnosis was 51 years (range 25–85 years), and 7 % of patients reported a first-degree relative diagnosed with breast cancer. Healthy population controls included 1,069 volunteers from the same geographic regions, with a similar ethnic distribution (incl. 411 Russians) and age distribution (median age 46 years, range 18–84 years). For the association study, cases and controls were stratified by their ancestry into Russians and non-Russians.
The series from Belarus consisted of 1,927 breast cancer patients diagnosed in the Republic of Belarus during the years 1998–2008. Patients were recruited at the Byelorussian Institute for Oncology and Medical Radiology Aleksandrov N.N. in Minsk or at one of five regional oncology centers in Gomel, Mogilev, Grodno, Brest, or Vitebsk. The Belarus series mainly consisted of consecutive patients unselected for family history, with the exception of an additional 28 cases with familial breast cancer ascertained at the center in Minsk. Median age at diagnosis in the Belarus cohort was 48 years, and a total of 302 patients (16 %) reported a first-degree relative with breast cancer. Byelorussian population controls were 1,235 healthy volunteers from the same population who had no personal history of breast cancer at the time when entering the study and were not known blood relatives of the study patients.
In addition to the two main series, we also genotyped two smaller case–control series from the Ukraine and from Kazakhstan. The Ukrainian study included 91 breast cancer patients and 37 controls that had been ascertained at the R.E.Kavetsky Institute of Experimental Pathology, Oncology and Radiobiology, National Academy of Sciences in Kyiv, Ukraine. The Ukrainian series was enriched for familial cases (n = 30), and median age at diagnosis was 47 years (range 31–63 years). The Kazakh study consisted of 281 breast cancer patients from Russian or Altaic subpopulations (111 Russians) and 653 healthy female controls (117 Russians) that had been ascertained at the State Oncology Institute, Almaty, Republic of Kazakhstan. Kazakh patients had a median age at diagnosis of 52 years (range 27–91 years) and the healthy controls a median age of 41 years (range 19–73 years). Genotyping for p.Q548X was limited to the Russian controls in the Kazakh series.
Our study was carried out with informed consent of the probands and was approved by local ethical boards at the respective institutions.
Mutation analyses
Genomic DNA was isolated from peripheral white blood cells by routine phenol–chloroform extraction. High-resolution melting analysis of PCR amplicons from the BLM exon 7 that harbors the p.Q548X mutation was performed on a Rotor-Gene 6000 real-time PCR machine (Corbett Research, Mortlake, Australia) using the primers 5′-TGT TCT CAC AAG CAC TGC TG-3′ and 5′-GAT ACT GAT TTA ATT GGC CGA-3′ [22], and EvaGreen as the fluorescent dye. Positive and negative controls were included in each assay, and all samples with suspicious melting behavior were subjected to direct sequencing using BigDye chemistry on a Genetic Analyser 3100 Avant (Applied Biosystems, Darmstadt, Germany). An example of HRM detection and sequencing analysis for p.Q548X is shown in Supplementary Figure 1. Another rare variant in this amplicon, c.1722A > G (rs28385011), was easily distinguished by both, HRM and sequencing, from the p.Q548X mutation.
Statistical analyses
The prevalence of the p.Q548X mutation was compared in cases and healthy population controls. Odds ratios (OR) were calculated from two-by-two tables and statistical significance was assessed with Fisher’s exact test using Yates’ correction. Crude and adjusted Mantel–Haenszel odds ratios were calculated using the EpiCalc v1.02 Software Package (Gilman J, Myatt M 1998, Brixton Books). All p values are two-sided. Q548X was the first BLM mutation investigated in the study populations, and results with p < 0.05 were considered significant. For a meta-analysis with published case–control studies, further genotype frequency data for p.Q548X were taken from the report of Sokolenko et al. [22], and four additional studies were identified via PubMed searches with the keywords “BLM and breast cancer” or “Bloom syndrome and breast cancer.” From these and our study populations, stratified by ancestry, adjusted Mantel–Haenszel odds ratios were again calculated using the EpiCalc v1.02 Software Package.
Results
We first scanned the exon 7 of BLM by high-resolution melting analysis in 1,059 cases and 1,069 controls from the Hannover-Ufa Breast Cancer Study to determine the frequency of the p.Q548X mutation in BLM and to validate its possible association with breast cancer. Heterozygosity for p.Q548X was confirmed in 5 cases, whereas the mutation was not found in controls (p = 0.09, Table 1). All carriers were of Russian descent, yielding a carrier frequency of 1.1 % in breast cancer patients from the Russian subpopulation of Bashkortostan. Histological data were available for four of the five carriers and documented advanced and high-grade tumors (stage T2–T3, G3), with a ductal histology in three and a lobular cancer in the fourth patient. None of these carriers had reported a positive family history for breast cancer, though one of the five patients was a carrier of BRCA1 mutation c.5266dupC (also known as 5382insC).
Since all identified carriers were Russians, we wanted to get further insight into the possible association of p.Q548X with breast cancer from another Slavic population and thus genotyped 1,927 Byelorussian cases and 1,235 Byelorussian controls from the Hannover-Minsk Breast Cancer Study. The mutation was identified in 9 cases (0.5 %) and 2 controls (0.2 %), showing again a non-significant excess of mutation carriers among the breast cancer patients (OR 2.9, 95 % CI 0.6; 13.4, p = 0.27, Table 1). The median age at diagnosis in p.Q548X heterozygous cases was 48 years (range 24–71 years) which was not different from the age at diagnosis in the total case series. Histological records were accessible for 6 of the 9 carriers and documented three ductal, one lobular, one medullary, and one tubular carcinoma. Positive or negative estrogen receptor status was equally distributed among these tumors. Again, two of the 9 breast cancer patients who were heterozygous for the p.Q548X mutation were also carriers of the common BRCA1 mutation, c.5266dupC. In addition, one of the 9 patients was a carrier of the CHEK2 dele9,10(5,395 bp) allele [26]. Four p.Q548X carriers had a first-degree family history of breast cancer, including the two double heterozygotes with c.5266dupC in BRCA1.
Since the p.Q548X mutation was present in patients from both, Russia and Belarus, we also genotyped two smaller case–control series from neighboring countries, Ukraine and Kazakhstan. No further carrier was identified among 111 Russian breast cancer cases and 117 Russian controls from the Republic of Kazakhstan. Some 170 Kazakh breast cancer cases from the other ethnic subgroups were also mutation-negative. One additional carrier was identified among 91 breast cancer patients from the Ukraine, suggesting that the p.Q548X allele may play some role also in this population (at a frequency of some 0.6 % when combined with 67 Ukrainian cases from Bashkortostan). This patient had been diagnosed by the age of 43 years with an advanced lobular breast cancer of grade 2; she also had a family history of breast cancer.
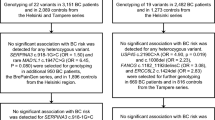
In a combined analysis of all four case–control series, the p.Q548X mutation was significantly associated with breast cancer (Mantel–Haenszel OR 5.1, 95 % CI 1.2; 21.9, p = 0.03) (Table 1). The effect sizes changed non-significantly when analyses were restricted to patients with age at diagnosis below 50 years (OR 5.4, 95 % CI 1.2; 24.4, p = 0.03) or to patients with a first-degree family history of breast cancer (OR 8.9, 95 % CI 1.6; 50.5, p = 0.02), but the numbers were small. The odds ratios obtained in our study were similar to the odds ratio reported in the hypothesis-generating study from the St. Petersburg area (OR 6.3) [22], and a meta-analysis of both studies confirmed the association of p.Q548X with breast cancer at a higher level of significance (OR 5.7, 95 %CI 2.0; 15.9, p = 3.7 × 10−4). When the analysis was restricted to patients without a known BRCA1 mutation, the association was slightly attenuated but remained significant (OR 4.9, 95 %CI 1.7; 14.0, p = 1.5 × 10−3). We also compared the results for p.Q548X with published data for other truncating mutations in BLM from the hitherto few available breast cancer studies [19, 27, 28]. A meta-analysis for all mutations further supported the association of BLM with breast cancer, with an estimated two- to five-fold increase in risk (OR 3.3, 95 %CI 1.9; 5.6, p = 1.9 × 10−5) (Table 2).
Discussion
Patients with Bloom’s syndrome face an increased risk not only for lymphomas and leukemias but also for epithelial carcinomas which occur much earlier than in the general population [29]. Breast cancers have been reported in several Bloom’s syndrome females, with a median age at onset of 32.4 years [29, 30]. There is little information available about whether blood relatives of Bloom’s syndrome patients also are at an increased cancer risk [31], and only few studies have addressed the heterozygote risk at the population level in case–control association studies after the identification of the BLM gene. In an early report, Ashkenazi Jews with colorectal cancer (CRC) were more than twice as likely to carry the 6-bp deletion/7-bp insertion, c.2207_2212delATCTGAinsTAGATTC (BLM Ash mutation), than Ashkenazi Jewish controls without CRC [19]. In this study, the risk for breast cancer appeared non-significantly increased in BLM Ash carriers (OR 1.8; 95 % CI 0.6, 4.9). Neither the increased risk for colorectal cancer nor an increased risk for any type of cancer was replicated in two subsequent studies [20, 21]. A familial breast cancer study found coinheritance of the BLM Ash mutation with BRCA1 mutations in two patients suggesting a potential modifier effect for the BLM Ash mutation [27].
The recent identification of a nonsense mutation, p.Q548X, as a recurrent BLM mutation in Russia has since enabled large case–control studies in this population [22]. This work from the St. Petersburg group revealed the p.Q548X allele in 1.1 % of Russian breast cancer patients, including 2.4 % of familial breast cancer patients, but only 0.2 % of healthy female controls, suggesting that p.Q548X may be associated with breast cancer risk [22]. Furthermore, a targeted next-generation sequencing study has provided further hints for BLM as a possible breast cancer gene as these authors identified BLM truncating mutations in two probands out of 438 BRCA1/2 mutation-negative hereditary breast cancer families from Australia, whereas no mutation carriers were found in 464 controls [28]. However, as pointed out by Ellis and Offit [32], the final proof of association is a question of statistical power, and the analysis of founder mutations such as p.Q548X can be helpful in this regard.
Our study has assessed the frequency distribution of the p.Q548X allele in 3,188 breast cancer cases and 2,458 controls from different populations across Eastern Europe and Eurasia. The mutation was solely identified in individuals with a Slavic background, including Russian, Byelorussian, and Ukrainian patients, whereas it was not seen in Altaic or other non-European subpopulations. This strongly corroborates the view of p.Q548X as a recurrent mutation in Slavic populations [22]. Although the heterozygote frequency of p.Q548X seems to be lower in Slavic populations than the frequency of the BLM Ash mutation in Ashkenazim, our study confirms the reported prevalence of p.Q548X in about 1 % of Russian breast cancer patients as well as its significant association with breast cancer. The combined odds ratios indicate an approximately five-fold increase in breast cancer risk in carriers of the p.Q548X mutation, consistent with an intermediate penetrance for breast cancer.
These estimates are comparable in size with the risk estimates for other Slavic founder mutations with intermediate penetrance in genes such as ATM or NBN that have been previously associated with breast cancer [23, 33, 34]. Their gene products interact with BLM in DNA double-strand break repair pathways and the biallelic mutant state results in a chromosomal instability syndrome, like Bloom’s syndrome. BRCA1 functions in a similar pathway, but BRCA1 mutations are usually associated with higher odds ratios in case–control studies such as HMBCS [24], with higher life-time risks and familial clustering. Double heterozygotes, such as reported here for BRCA1 and BLM, have previously been observed for several other breast cancer susceptibility genes including BRCA2 [35], PALB2 [36], ATM [23], or CHEK2 [37]. Evidence suggests that intermediate-penetrance mutations in ATM or CHEK2 are less common in BRCA1 mutation carriers than in non-carriers, consistent with their function in the same pathway [37]. With regard to BLM, the co-inheritance of a BRCA1 mutation in 3/14 p.Q548X heterozygous patients in our study, and in 1/17 BLM heterozygous patients in the study by Sokolenko et al. [22], indicates that mutations in BRCA1 and in BLM are not mutually exclusive. This may reflect that BLM functions independent of the ATM-CHEK2-BRCA1 pathway, as part of additional repair complexes such as BRAFT or the dissolvasome [38], so that BLM mutations could still augment the effect of BRCA1 deficiency. Alternatively, the predisposition may act at the level of haploinsufficiency when BRCA1 is not yet fully inactivated through methylation or a second hit. In both scenarios it would seem plausible to assume that p.Q548X acts as a breast cancer susceptibility allele in patients without a BRCA1 mutation, where it still constitutes a significant risk factor, and as a modifier of penetrance in BRCA1 mutation carriers. One previous report had suggested that, in Ashkenazim, BLM mutations may act as modifiers of penetrance for BRCA1 mutations [27], but additional and larger studies would be needed to clarify the degree of interaction, if any, between BLM and BRCA1 in the genetic susceptibility to breast cancer.
In a survey of hitherto published data, the p.Q548X mutation provides the strongest evidence to date for a role of BLM mutations in genetic breast cancer susceptibility, as the combined analysis of p.Q548X in cases and controls of Slavic ancestry suggests an approximately five-fold increase in breast cancer risk at a considerably high level of significance. An increased prevalence of any BLM mutation carriers among breast cancer cases is also supported by previous studies which were in the same direction but had revealed lower odds ratios and non-significant outcomes. Although the allelic effect of the BLM Ash mutation appears lower than that of the p.Q548X mutation, this difference was not statistically significant and could be due to low numbers, or perhaps relate to some residual function associated with the BLM Ash mutation that had originally been discovered in homozygous Bloom′s syndrome patients and could be hypomorphic [5]. Notably, some differences have also been observed in the viability of Blm−/− mice carrying different null alleles [39]. Further deleterious BLM mutations in more heterogeneous populations may become apparent in the future with the more widespread use of next-generation sequencing as indicated by one Australian study so far [28]. At present, our meta-analysis appears to be most consistent with an approximately two- to five-fold increase in breast cancer risk for carriers of any BLM truncating mutation.
In summary, our study has confirmed that a nonsense mutation, p.Q548X, in BLM is significantly associated with breast cancer and occurs at frequencies of 0.5–1 % of breast cancer patients in Slavic populations. The combined data indicate that BLM is not only a gene for Bloom’s syndrome but also might represent a further breast cancer susceptibility gene.
References
Turnbull C, Rahman N (2008) Genetic predisposition to breast cancer: past, present, and future. Annu Rev Genomics Hum Genet 9:321–345
Campeau PM, Foulkes WD, Tischkowitz MD (2008) Hereditary breast cancer: new genetic developments, new therapeutic avenues. Hum Genet 124:31–42
Bogdanova N, Dörk T (2012) Molecular genetics of breast and ovarian cancer. Balkan J Med Genet 15(1):75–80
Ellis NA, German J (1996) Molecular genetics of Bloom’s syndrome. Hum Mol Genet 5:1457–1463
German J (1993) Bloom syndrome: a mendelian prototype of somatic mutational disease. Medicine 72:393–406
German J, Archibald R, Bloom D (1965) Chromosomal breakage in a rare and probably genetically determined syndrome of man. Science 148:506–507
Ellis NA, Groden J, Ye TZ, Straughen J, Lennon DJ, Ciocci S, Proytcheva M et al (1995) The Bloom’s syndrome gene product is homologous to RecQ helicases. Cell 83:655–666
Ababou M, Dutertre S, Lécluse Y, Onclercq R, Chatton B, Amor-Guéret M (2000) ATM-dependent phosphorylation and accumulation of endogenous BLM protein in response to ionizing radiation. Oncogene 19:5955–5963
Bischof O, Kim SH, Irving J, Beresten S, Ellis NA, Campisi J (2001) Regulation and localization of the Bloom syndrome protein in response to DNA damage. J Cell Biol 153:367–380
Beamish H, Kedar P, Kaneko H, Chen P, Fukao T, Peng C, Beresten S, Gueven N, Purdie D, Lees-Miller S, Ellis N, Kondo N, Lavin MF (2002) Functional link between BLM defective in Bloom’s syndrome and the ataxia-telangiectasia-mutated protein, ATM. J Biol Chem 277:30515–30523
Wang Y, Cortez D, Yazdi P, Neff N, Elledge SJ, Qin J (2000) BASC, a super complex of BRCA1-associated proteins involved in the recognition and repair of aberrant DNA structures. Genes Dev 14:927–939
Nimonkar AV, Genschel J, Kinoshita E, Polaczek P, Campbell JL, Wyman C, Modrich P, Kowalczykowski SC (2011) BLM–DNA2–RPA–MRN and EXO1–BLM–RPA–MRN constitute two DNA end resection machineries for human DNA break repair. Genes Dev 25:350–362
Wu L, Davies SL, Levitt NC, Hickson ID (2001) Potential role for the BLM helicase in recombinational repair via a conserved interaction with RAD51. J Biol Chem 276:19375–19381
Braybrooke JP, Li JL, Wu L, Caple F, Benson FE, Hickson ID (2003) Functional interaction between the Bloom’s syndrome helicase and the RAD51 paralog, RAD51L3 (RAD51D). J Biol Chem 278:48357–48366
Ouyang KJ, Woo LL, Zhu J, Huo D, Matunis MJ, Ellis NA (2009) SUMO modification regulates BLM and RAD51 interaction at damaged replication forks. PLoS Biol 7(12):e1000252
Suhasini AN, Brosh RM Jr (2012) Fanconi anemia and Bloom’s syndrome crosstalk through FANCJ–BLM helicase interaction. Trends Genet 28:7–13
Chan KL, North PS, Hickson ID (2007) BLM is required for faithful chromosome segregation and its localization defines a class of ultrafine anaphase bridges. EMBO J 26(14):3397–3409
German J, Bloom D, Passarge E, Fried K, Goodman RM, Katzenellenbogen I, Laron Z et al (1977) Bloom’s syndrome. VI. The disorder in Israel and an estimation of the gene frequency in the Ashkenazim. Am J Hum Genet 29:553–562
Gruber SB, Ellis NA, Scott KK, Almog R, Kolachana P, Bonner JD, Kirchhoff T, Tomsho LP, Nafa K, Pierce H, Low M, Satagopan J, Rennert H, Huang H, Greenson JK, Groden J, Rapaport B, Shia J, Johnson S, Gregersen PK, Harris CC, Boyd J, Rennert G, Offit K (2002) BLM heterozygosity and the risk of colorectal cancer. Science 297:2013
Cleary SP, Zhang W, Di Nicola N, Aronson M, Aube J, Steinman A, Haddad R, Redston M, Gallinger S, Narod SA, Gryfe R (2003) Heterozygosity for the BLM(Ash) mutation and cancer risk. Cancer Res 63:1769–1771
Zauber NP, Sabbath-Solitare M, Marotta S, Zauber AG, Foulkes W, Chan M, Turner F, Bishop DT (2005) Clinical and genetic findings in an Ashkenazi Jewish population with colorectal neoplasms. Cancer 104:719–729
Sokolenko AP, Iyevleva AG, Preobrazhenskaya EV, Mitiushkina NV, Abysheva SN, Suspitsin EN, Kuligina ESh, Gorodnova TV, Pfeifer W, Togo AV, Turkevich EA, Ivantsov AO, Voskresenskiy DV, Dolmatov GD, Bit-Sava EM, Matsko DE, Semiglazov VF, Fichtner I, Larionov AA, Kuznetsov SG, Antoniou AC, Imyanitov EN (2012) High prevalence and breast cancer predisposing role of the BLM c.1642 C > T (Q548X) mutation in Russia. Int J Cancer 130:2867–2873
Bogdanova N, Cybulski C, Bermisheva M, Datsyuk I, Yamini P, Hillemanns P, Antonenkova NN, Khusnutdinova E, Lubinski J, Dörk T (2009) A nonsense mutation (E1978X) in the ATM gene is associated with breast cancer. Breast Cancer Res Treat 118:207–211
Bogdanova NV, Antonenkova NN, Rogov YI, Karstens JH, Hillemanns P, Dörk T (2010) High frequency and allele-specific differences of BRCA1 founder mutations in breast cancer and ovarian cancer patients from Belarus. Clin Genet 78:364–372
Ghoussaini M, Fletcher O, Michailidou K, Turnbull C, Schmidt MK, Dicks E, Dennis J et al (2012) Genome-wide association analysis identifies three new breast cancer susceptibility loci. Nat Genet 44:312–318
Bogdanova N, Feshchenko S, Cybulski C, Dörk T (2007) CHEK2 mutation and hereditary breast cancer. J Clin Oncol 25(19):e26
Koren-Michowitz M, Friedman E, Gershoni-Baruch R, Brok-Simoni F, Patael Y, Rechavi G, Amariglio N (2005) Coinheritance of BRCA1 and BRCA2 mutations with Fanconi anemia and Bloom syndrome mutations in Ashkenazi Jewish population: possible role in risk modification for cancer development. Am J Hematol 78:203–206
Thompson ER, Doyle MA, Ryland GL, Rowley SM, Choong DY, Tothill RW, Thorne H, kConFab, Barnes DR, Li J, Ellul J, Philip GK, Antill YC, James PA, Trainer AH, Mitchell G, Campbell IG (2012) Exome sequencing identifies rare deleterious mutations in DNA repair genes FANCC and BLM as potential breast cancer susceptibility alleles. PLoS Genet 8(9):e1002894
German J (1997) Bloom’s syndrome. XX. The first 100 cancers. Cancer Genet Cytogenet 93:100–106
Masmoudi A, Marrakchi S, Kamoun H, Chaaben H, Ben Salah G, Ben Salah R, Fakhfakh F, Zahaf A, Turki H (2012) Clinical and laboratory findings in 8 patients with Bloom’s syndrome. J Dermatol Case Rep 6:29–33
Baris HN, Kedar I, Halpern GJ, Shohat T, Magal N, Ludman MD, Shohat M (2007) Prevalence of breast and colorectal cancer in Ashkenazi Jewish carriers of Fanconi anemia and Bloom syndrome. Isr Med Assoc J 9:847–850
Ellis NA, Offit K (2012) Heterozygous mutations in DNA repair genes and hereditary breast cancer: a question of power. PLoS Genet 8(9):e1003008
Górski B, Cybulski C, Huzarski T, Byrski T, Gronwald J, Jakubowska A, Stawicka M, Gozdecka-Grodecka S, Szwiec M, Urbański K, Mituś J, Marczyk E, Dziuba J, Wandzel P, Surdyka D, Haus O, Janiszewska H, Debniak T, Tołoczko-Grabarek A, Medrek K, Masojć B, Mierzejewski M, Kowalska E, Narod SA, Lubiński J (2005) Breast cancer predisposing alleles in Poland. Breast Cancer Res Treat 92:19–24
Bogdanova N, Feshchenko S, Schürmann P, Waltes R, Wieland B, Hillemanns P, Rogov YI, Dammann O, Bremer M, Karstens JH, Sohn C, Varon R, Dörk T (2008) Nijmegen Breakage Syndrome mutations and risk of breast cancer. Int J Cancer 122:802–806
Heidemann S, Fischer C, Engel C, Fischer B, Harder L, Schlegelberger B, Niederacher D, Goecke TO, Doelken SC, Dikow N, Jonat W, Morlot S, Schmutzler RC, Arnold NK (2012) Double heterozygosity for mutations in BRCA1 and BRCA2 in German breast cancer patients: implications on test strategies and clinical management. Breast Cancer Res Treat 134:1229–1239
Pern F, Bogdanova N, Schürmann P, Lin M, Ay A, Länger F, Hillemanns P, Christiansen H, Park-Simon TW, Dörk T (2012) Mutation analysis of BRCA1, BRCA2, PALB2 and BRD7 in a hospital-based series of German patients with triple-negative breast cancer. PLoS One 7(10):e47993
Turnbull C, Seal S, Renwick A, Warren-Perry M, Hughes D, Elliott A, Pernet D, Peock S, Adlard JW, Barwell J, Berg J, Brady AF, Brewer C, Brice G, Chapman C, Cook J, Davidson R, Donaldson A, Douglas F, Greenhalgh L, Henderson A, Izatt L, Kumar A, Lalloo F, Miedzybrodzka Z, Morrison PJ, Paterson J, Porteous M, Rogers MT, Shanley S, Walker L, Breast Cancer Susceptibility Collaboration (UK), EMBRACE, Ahmed M, Eccles D, Evans DG, Donnelly P, Easton DF, Stratton MR, Rahman N (2012) Gene-gene interactions in breast cancer susceptibility. Hum Mol Genet 21:958–962
Hoadley KA, Xue Y, Ling C, Takata M, Wang W, Keck JL (2012) Defining the molecular interface that connects the Fanconi anemia protein FANCM to the Bloom syndrome dissolvasome. Proc Natl Acad Sci USA 109:4437–4442
Luo G, Santoro IM, McDaniel LD, Nishijima I, Mills M, Youssoufian H, Vogel H, Schultz RA, Bradley A (2000) Cancer predisposition caused by elevated mitotic recombination in Bloom mice. Nat Genet 26:424–429
Acknowledgments
We thank the patients and healthy volunteers for their participation and the clinicians at hospitals in Belarus, Kazakhstan, Russia, and Ukraine for their support of this work. We cordially thank Evgeny Imyanitov and his group for providing us with a positive control for this study. D.P. was supported by travel funds from the German Ministry of Education and Research and by grant 12-04-97026 of the Russian Foundation for Basic Research. N.B. was supported by an intramural Hannelore-Munke stipend at Hannover Medical School. I.D. was supported by a German Academic Exchange Program (DAAD). The Hannover laboratory was furthermore supported by the Rudolf Bartling Foundation.
Ethical Standards
The experiments in the present study comply with the current laws of the country in which they were performed.
Conflict of interest
None of the authors declares a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2012_2357_MOESM1_ESM.tif
Supplementary material 1 (TIFF 269 kb): Identification of the BLM mutation p.Q548X by means of high-resolution melting analysis (top) and direct sequencing (bottom). Top: Normalized fluorescence graph for high-resolution melting analysis of the mutant amplicon carrying the p.Q548X mutation in comparison with wildtype controls. Bottom: Direct sequencing of exon 7 in the BLM gene, sense strand, in a sample with heterozygosity for mutation p.Q548X (C/T, asterisk)
Rights and permissions
About this article
Cite this article
Prokofyeva, D., Bogdanova, N., Dubrowinskaja, N. et al. Nonsense mutation p.Q548X in BLM, the gene mutated in Bloom’s syndrome, is associated with breast cancer in Slavic populations. Breast Cancer Res Treat 137, 533–539 (2013). https://doi.org/10.1007/s10549-012-2357-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2357-1