Abstract
Younger women with breast cancer consistently show greater psychological distress than older women. This study examined a range of factors that might explain these age differences. A total of 653 women within 8 months of a first-time breast cancer diagnosis provided data on patient characteristics, symptoms, and psychosocial variables. Chart reviews provided cancer and treatment-related data. The primary outcome was depressive symptomatology assessed by the Beck Depression Inventory. A succession of models that built hierarchically upon each other was used to determine which variables could account for age group differences in depression. Model 1 contained age group only. Models 2–5 successively added patient characteristics, cancer-related variables, symptoms, and psychosocial variables. As expected, in the unadjusted analysis (Model 1) younger women were significantly more likely to report depressive symptomatology than older women (p < 0.0001). Age remained significantly related to depression until Model 4 which added bodily pain and vasomotor symptoms (p = 0.24; R 2 = 0.27). The addition of psychosocial variables in Model 5 also resulted in a model in which age was nonsignificant (p = 0.49; R 2 = 0.49). Secondary analyses showed that illness intrusiveness (the degree that illness intrudes on specific areas of life such as work, sex life, recreation, etc.) was the only variable which, considered individually with age, made the age group-depression association nonsignificant. Age differences in risk of depression following a breast cancer diagnosis can be explained by the impact of cancer and its treatment on specific areas of a woman’s life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2012, an estimated 226,870 women in the US will be diagnosed with breast cancer, making it the most common cancer among women in this country [1]. A long history of research on psychological adjustment to breast cancer diagnosis and treatment finds that with few exceptions [2, 3], younger age is related to greater distress and poorer psychological adjustment following diagnosis [4–13]. Depression is a particularly common affective disorder among cancer patients, has a major impact on quality of life, and impacts treatment adherence [14–19]. As with general psychological distress, younger age has been shown to be associated with increased depression risk [5, 6, 8, 13, 20, 21].
Because younger women tend to be diagnosed at later stages and/or with more aggressive disease [22], their poorer adjustment may be a result of disease and/or treatment effects. Alternatively, other factors related to life stage, such as demands of childcare, employment, and abrupt menopause with associated symptoms may explain these findings [9, 11, 23]. However, empirical research to elucidate reasons for these age differences is lacking.
Few studies include both a wide age range of women and a wide array of both treatment and psychosocial variables to adequately explore the above hypotheses. Mosher and Danoff-Burg [7] suggest that treatment factors, as well as symptoms associated with premature menopause, psychosocial and economic factors, and less adaptive coping strategies may all account for these age differences and that a contextual perspective that includes all of these factors would help elucidate the mechanisms underlying these age differences. Although Wong-Kim and Bloom [24] used a biopsychosocial model to explain depression among newly diagnosed women with breast cancer, their study included only women under the age of 51 at diagnosis and did not include variables associated with premature menopause or coping strategies. The primary purpose of this study is to explain age differences in depression risk among women diagnosed with a first-time breast cancer by examining, through statistical modeling, a broad array of possible explanatory factors among a wide age range of women. The primary outcome is depressive symptomatology as assessed by the Beck Depression Inventory.
Methods
Setting and population
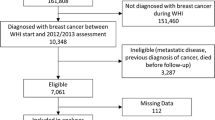
This observational study was conducted among women aged 25 years and older newly diagnosed with stage I, II, or III breast cancer. Recruitment was conducted at Memorial Sloan Kettering Cancer Center and the University of Texas—Southwestern Center for Breast Care from 2002 to 2006. Women were recruited through hospital clinics and advertisements and initially screened by chart review or telephone for eligibility. Eligible women were mailed a baseline questionnaire to return to the Coordinating Center at Wake Forest University. Baseline questionnaires were completed within 8 months of diagnosis. All sites obtained approval from their Institutional Review Boards.
Primary outcome
The primary outcome was depressive symptomatology as measured by the Beck Depression Inventory (BDI) version BDI-1A [25], a 21-item scale used to assess depressive symptomatology/general distress. Scores of 10 and above are thought to indicate presence of at least mild depressive symptoms warranting clinical evaluation. We thus dichotomized women according to BDI score into “depressed” (≥10) and “not depressed” (≤9) [26]. We refer to women as depressed or not depressed, though we recognize that the BDI is a measure of depressive symptomatology and not a diagnostic tool. We also performed secondary analyses considering BDI as a continuous outcome to verify findings from the dichotomized BDI score.
Independent variables
We selected independent variables for inclusion in analyses if they were characteristics of age/life stage (e.g., having children at home, being employed), related to cancer, or previously found to be associated with depression independently of age (e.g., illness intrusiveness, optimism, pain, social support).
Sociodemographic variables/patient characteristics. In addition to age, our main variable of interest, we included race, marital/partner status, presence of children under age 18 in the home, employment status, education, household income level, and number of self-reported comorbid conditions. Age categories were adapted from Rowland [27] a priori as follows: 25–44, 45–54, 55–64, 65–74, and ≥75 to examine the impact of cancer on women at various developmental stages.
Cancer-related variables. The following variables were obtained from chart review: time between cancer diagnosis and baseline questionnaire; cancer stage at diagnosis (I, II, or III); type of surgery (no surgery before completion of baseline survey, lumpectomy before baseline, mastectomy before baseline); radiation therapy before baseline survey (yes/no); and chemotherapy before completion of baseline survey (none, chemotherapy with doxorubicin, chemotherapy without doxorubicin). Doxorubicin, a foundational component of aggressive anthracycline chemotherapy regimens, was considered because it has particularly high toxicities and negative side effects [28], and is more likely to be given to younger women [29].
Symptoms. Two symptom variables associated with depression were included in analyses: severity of vasomotor symptoms in terms of degree of interference in usual activities (4-point ordinal scale ranging from none to severe) as used in the Women’s Health Initiative [30] and severity of bodily pain (6-point ordinal scale, ranging from none to very severe) from the SF-36.
Psychosocial variables. The Illness Intrusiveness Scale assessed the degree to which breast cancer diagnosis and treatment interfered with thirteen life areas: health, diet, paid work, active recreation, passive recreation, financial situation, relationship with spouse, sex life, family relations, other social relations, self-expression, religious expression and community [31]. We added three items to the standard scale that especially impact younger women: family responsibilities, social activities, and work around the house. For each item, respondents rated the degree that their illness or its treatment interfered with that area, based on a 7-point scale, ranging from 1 (not very much) to 7 (very much). The overall illness intrusiveness score is the sum of the 16 items (Cronbach’s alpha = 0.93).
Spirituality was measured by the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) scale [32], a 12-item scale with three subscales: meaning in one’s life, peacefulness, and the role of faith [33].
Coping was assessed with the 28-item Brief COPE scale [34] measuring 14 types of coping responses. Participants rated the extent to which each response was used in dealing with stresses associated with their cancer diagnosis and treatment. A second-order factor analysis on our data, as recommended by Carver [34], revealed two domains composed of 11 of the measure’s subscales: active coping (e.g., active coping, emotional support, instrumental support, and positive reframing) and passive coping (self-blame, denial, and behavioral disengagement). Scores were the mean for each domain.
Perceived attractiveness was based on three items from the Lasry body image scale [35] that assess how a woman perceives her general attractiveness. Women rate their agreement (1 = strongly agree, 5 = strongly disagree) to three statements: feeling attractive to others, feeling attractiveness has changed due to surgery; and fear of being unattractive sexually. Items are reverse scored and summed to provide a total score ranging from 3 to 15 with higher scores indicating greater perceived attractiveness.
Social support was assessed by the RAND Social Support Scale [36] measuring four aspects of support: emotional support, tangible support, affection, and social interaction. A total support score is the sum of these four categories.
Finally, we included an 8-item version of the self-report Life Orientation Test (LOT) [37] to measure optimism. Participants respond to eight statements on a 4-point scale ranging from agree to disagree. Scores are calculated as the sum of the items.
Statistical methods
We computed descriptive measures (percentages and means with standard deviations) after stratifying the sample on age group and covariates. In all analyses depression is treated as a dichotomous outcome variable.
We modeled the association between age group and depression using logistic regression. Our analysis goal was to determine which variables, if any, statistically accounted for crude age group differences in depression. We employed a modeling strategy whereby we created successively more detailed logistic models, and examined the resulting adjusted odds ratios and p values for the age group-depression association. Model 1 contained age group only. Model 2 contained age group plus the sociodemographic/patient characteristics (race, marital/partner status, children age <18, household income, employment, education, comorbidities). Model 3 contained age group, sociodemographic/patient variables, and cancer-related variables (time since diagnosis, stage, surgery, radiation, chemotherapy). Model 4 contained all the above variables plus vasomotor and pain symptoms. Finally, Model 5 added to Model 4 the psychosocial variables (spirituality, illness intrusiveness, coping, perceived attractiveness, social support, optimism). In all models, age group was treated as a categorical rather than ordinal variable.
The following predictor variables were parameterized as continuous variables: time since diagnosis (in months), severity of vasomotor symptoms (0–3), severity of physical pain (0–5), and all the psychosocial scales. All other variables were treated as nominal categorical variables.
For each logistic regression model, we computed Nagelkerke’s R 2 as a measure of model fit [38]. All analyses were conducted using SAS 9.1.3.
Results
Sample characteristics
A total of 740 surveys were mailed out to women deemed eligible from chart reviews or telephone screening; 653 women completed baseline surveys for a response rate of 88 %. The age distribution was as: 25–44 years (N = 132), 45–54 years (N = 209), 55–64 years (N = 167), 65–74 years (N = 102), and 75+ (N = 43).
Table 1 shows participant characteristics in terms of frequencies and percentages for categorical variables and means and standard deviations for the continuous variables, all stratified by age group. Age was significantly related to depression, employment status, income, having children at home, comorbid conditions, chemotherapy with doxorubicin, cancer stage, type of surgery, vasomotor symptoms, and bodily pain. Age was also significantly related to most of the psychosocial scales except for active coping, social support, and optimism.
Table 2 shows the percentage of women classified as depressed according to covariate stratum. Nonwhite women, those with children under 18 years of age in the home, with household incomes under $20,000, and who had either none or 3 or more comorbid conditions were more likely to be depressed. With respect to disease and treatment covariates, women diagnosed with stage II or III disease and those who received chemotherapy with doxorubicin reported more depression. Finally, there were monotonic gradients in percentage depressed according to degree of vasomotor symptoms and of bodily pain. Means of all psychosocial scores significantly differed by depression status (Table 3).
Regression models
Table 4 shows the results of our model-building strategy to explain age-related differences in odds of depression.
As expected, in the unadjusted analysis (Model 1) we found a statistically significant relationship (p < 0.0001) between age and depression, with younger women much more likely to be depressed than older women. There was a monotonic association between age group and the crude OR of depression: relative to the youngest age group, odds of depression ranged from 0.57 to 0.17. Model 2 added the sociodemographic/patient characteristics variables. Although income level (p = 0.007), presence of children under the age of 18 years in the home (p = 0.018), and number of comorbidities (p = 0.02) were significantly related to depression, age remained highly significant (p = <0.001), with the ORs maintaining their monotonicity of decline with increasing age group. Model 3 added the five cancer-related variables. Chemotherapy status was significantly associated with depression (p < 0.0001), with those receiving doxorubicin having significantly higher odds of depression than those who received no chemotherapy (OR = 2.66, 95 % CI 1.53–4.61). There was no significant difference in odds of depression between those who received chemotherapy without doxorubicin and those who received no chemotherapy. The same three sociodemographic/patient variables were significant in model 3 as in model 2: presence of children under the age of 18 years, household income level, and number of comorbidities. Age group remained significant at p = 0.014, though the ORs (now ranging from 0.88 to 0.33) moved closer to 1.0 relative to the reference group.
Model 4 added the two symptom variables to Model 3. This is the first model in the series in which age group was no longer statistically significantly associated with depression. (p = 0.24). The ORs for the age group-depression association moved even closer to 1.0 relative to the reference group. Nagelkerke’s R 2 increased from 0.18 to 0.27. Severity of vasomotor symptoms was significant (p = 0.012), as was severity of bodily pain (p < 0.0001). Income level (p = 0.02) and presence of children under age 18 (p = 0.004) were still significant in this model as was chemotherapy status (p = 0.003).
Model 5 added the psychosocial variables. In this full model, age was again non-significantly associated with depression (p = 0.49). Nagelkerke’s R 2 (0.49) was substantially higher than that for Model 4. Odds ratios and significance levels for all variables in model 5 are shown in Table 5. Severity of bodily pain remained a significant predictor of depression (p = 0.02, OR = 1.34, 95 % CI = 1.06-1.69), as did chemotherapy (p = 0.01, OR = 2.98 for comparison of chemotherapy with doxorubicin to those with no chemotherapy before baseline). Several psychosocial variables were significantly associated with depression, including spirituality-peace (p < 0.0001), illness intrusiveness (p < 0.0001), passive coping strategies (p = 0.01), and perceived attractiveness (p = 0.02).
We replicated the above-described five statistical models employing BDI as a continuous variable using linear rather than logistic models. Results were almost exactly the same: age group became statistically nonsignificant in model 4, following the addition of the symptom variables, and the same list of significant predictor variables were found in the full model 5.
In secondary analyses, we explored which variables most helped explain age group differences in depression. We found, in automated forward-selection logistic regression analyses, that among the eight variables selected for entry using a significance-level-for-entry criterion of 0.10 (illness intrusiveness, spirituality-peace, active coping, pain, perceived attractiveness, optimism, chemotherapy status, and number of comorbidities, the illness intrusiveness score was the first variable selected for entry as significantly associated with depression risk). In models which included a single predictor variable in addition to age, we also found that illness intrusiveness was the only variable which, alone, made the age group-depression association nonsignificant.
We further found a significant monotonic gradient by age for each of the illness intrusiveness questions with older women reporting less intrusiveness for each item. To examine whether illness intrusiveness was simply a proxy for more aggressive treatment, we limited analyses to women who had only stage I disease and no chemotherapy treatment. These strong age-related patterns in all the illness intrusiveness items held even among women who had the least objectively intrusive diagnoses and treatment regimens.
Discussion
These cross-sectional analyses confirm previous reports that younger women are more likely to report depressive symptoms following breast cancer diagnosis than older women. We found a monotonic gradient in the crude odds of depression by age, with those 75 and older at time of diagnosis having 83 % lower odds of depression in unadjusted analyses compared to women under age 45 at time of diagnosis.
Many of the variables significantly associated with depression in crude bivariate analyses are consistent with other studies [5, 18, 24, 39, 40]. However, only a subset of these remained significant following simultaneous adjustment in the full model: chemotherapy regimen, bodily pain, illness intrusiveness, sense of peace, passive coping, and perceived attractiveness. Contrary to Compas et al. [9], we found that younger women used more active coping. However, they also used more passive coping (although this was not statistically significant), suggesting that they may use more coping strategies in general. Although other studies have also found that psychosocial factors contribute more to depression than treatment factors [3, 5, 19] we would not conclude, as did Bardwell et al. [5], that cancer-related variables are unimportant when considering risk of depression. It should be noted that Bardwell et al. combined surgery and chemotherapy into one category and did not consider specific chemotherapy regimens. Our results suggest that it is important to consider aggressiveness of chemotherapy. As found by Wong-Kim and Bloom [24], a biopsychosocial approach provides the most comprehensive explanation of depression. However, our primary goal was not to confirm previous findings, but to better understand why younger women experience more depression after a breast cancer diagnosis than do older women. Adjustment for sociodemographic and cancer-related variables ameliorated the strong, crude age-related gradient in depression risk somewhat, but age remained a significant predictor of risk of depression. It was not until symptoms and certain psychosocial variables were included in the model that the inverse age-related gradient disappeared.
Of the psychosocial variables, and indeed of all the variables we examined, illness intrusiveness appears to be a key measure which helps to explain the age-related differences—younger women consistently report significantly higher levels of illness intrusiveness than do older women across all 16 domains covered by the illness intrusiveness measure. Although health, diet, active recreation, and social activities were among the top five areas that were most disrupted by cancer across all participants, there were some differences by age group. For example, sex life was the area most affected for those under age 45, while work around the house was in the top five for those 55 and older.
It is not possible to completely eliminate the intrusiveness of a breast cancer diagnosis on a younger woman. However, a focus on symptom management and on self-reports of illness intrusiveness in distinct areas of life may suggest possible interventions to lessen pain and intrusiveness, and consequently may lessen risk for depression. Younger women reported more severe pain and this may be an important factor that increases illness intrusiveness. For those under age 45, sex life was rated as the area most affected by cancer (4.5 on a 7-point scale) and other studies have shown that younger women often report significant sexual problems as a result of chemotherapy [41, 42]. Sexual functioning is an area where remedies to decrease vaginal dryness or interventions to increase feelings of sexual attractiveness may be beneficial.
This study has several limitations. The analyses are observational and cross-sectional only, so we cannot eliminate the possibility that women who are depressed are more likely to perceive their breast cancer as more intrusive. The Beck Depression Inventory is a self-report measure of depressive symptomatology and is not a measure of clinical depression. Although characteristic of many samples of breast cancer patients, this sample is relatively homogeneous (mostly white, educated) which limits the generalizability of our findings.
Overall, our results provide empirical support that age differences in psychological morbidity immediately following a breast cancer diagnosis may be accounted for by the greater impact cancer and its treatment have in the lives of younger women.
References
ACS. American Cancer Society, Cancer Facts & Figures 2012. Atlanta, American Cancer Society
Ganz PA, Lee JJ, Sims MS, Polinsky ML, Schag CA (1992) Exploring the influence of multiple variables on relationship of age to quality of life in women with breast cancer. J Clin Epidemiol 45:473–485
Golden-Kreutz DM, Andersen BL (2004) Depressive symptoms after breast cancer surgery: relationships with global, cancer-related, and life event stress. Psycho-Oncology 13:211–220
Avis NE, Deimling GT (2008) Cancer survivorship and aging. Cancer 113:3519–3529
Bardwell WA, Natarajan L, Dimsdale JE et al (2006) Objective cancer-related variables are not associated with depressive symptoms in women treated for early-stage breast cancer. J Clin Oncol 24:2420–2427
Broeckel JA, Jacobsen PB, Balducci L, Horton J, Lyman GH (2000) Quality of life after adjuvant chemotherapy for breast cancer. Breast Cancer Res Treat 62:141–150
Mosher CE, Danoff-Burg S (2005) A review of age differences in psychological adjustment to breast cancer. J Psychosocial Oncol 23:101–114
Wenzel LB, Fairclough DL, Brady MJ et al (1999) Age-related differences in the quality of life of breast carcinoma patients after treatment. Cancer 86:1768–1774
Compas BE, Stoll MF, Thomsen AH, Oppedisano G, Epping-Jordan JE, Krag DN (1999) Adjustment to breast cancer: age-related differences in coping and emotional distress. Breast Cancer Res Treat 54:195–203
Kroenke CH, Rosner B, Chen WY, Kawachi I, Colditz GA, Holmes MD (2004) Functional impact of breast cancer by age at diagnosis. J Clin Oncol 22:1849–1856
Mor V, Malin M, Allen S (1994) Age differences in the psychosocial problems encountered by breast cancer patients. J Natl Cancer Inst Monogr 16:191–197
Vinokur AD, Threatt BA, Vinokur-Kaplan D, Satariano WA (1990) The process of recovery from breast cancer for younger and older patients. Changes during the first year. Cancer 65:1242–1254
van’t Spijker A, Trijsburg RW, Duivenvoorden HJ (1997) Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosom Med 59:280–293
DiMatteo MR, Lepper HS, Croghan TW (2000) Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 160:2101–2107
Day R, Ganz PA, Costantino JP (2001) Tamoxifen and depression: more evidence from the National Surgical Adjuvant Breast and Bowel Project’s Breast Cancer Prevention (P-1) Randomized Study. J Natl Cancer Inst 93:1615–1623
Fann JR, Thomas-Rich AM, Katon WJ et al (2008) Major depression after breast cancer: a review of epidemiology and treatment. Gen Hosp Psychiatry 30:112–126
Bower JE (2008) Behavioral symptoms in patients with breast cancer and survivors. J Clin Oncol 26:768–777
Deshields T, Tibbs T, Fan MY, Taylor M (2006) Differences in patterns of depression after treatment for breast cancer. Psycho-Oncology 15:398–406
Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A (2005) Depression and anxiety in women with early breast cancer: five year observational cohort study. BMJ 330:702
Parker PA, Baile WF, de Moor C, Cohen L (2003) Psychosocial and demographic predictors of quality of life in a large sample of cancer patients. Psycho-Oncology 12:183–193
Howard-Anderson J, Ganz PA, Bower JE, Stanton AL (2012) Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst 104:386–405
Anders CK, Fan C, Parker JS et al (2011) Breast carcinomas arising at a young age: unique biology or a surrogate for aggressive intrinsic subtypes? J Clin Oncol 29:e18–e20
Avis NE, Crawford S, Manuel J (2004) Psychosocial problems among younger women with breast cancer. Psycho-Oncology 13:295–308
Wong-Kim EC, Bloom JR (2005) Depression experienced by young women newly diagnosed with breast cancer. Psycho-Oncology 14:564–573
Beck AT, Steer RA, Ball R, Ranieri W (1996) Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J Pers Assess 67:588–597
Beck AT, Steer RA (1987) Beck depression inventory manual. The Psychological Corporation, San Antonio, Texas
Rowland JH (1989) Developmental stage and adaptation: adult model. In: Holland JD, Rowalnd JH (eds) Handbook of psychoonocology. Oxford University Press, Oxford, pp 25–43
Pal SK, Childs BH, Pegram M (2010) Emergence of nonanthracycline regimens in the adjuvant treatment of breast cancer. Breast Cancer Res Treat 119:25–32
Lyman GH, Dale DC, Crawford J (2003) Incidence and predictors of low dose-intensity in adjuvant breast cancer chemotherapy: a nationwide study of community practices. J Clin Oncol 21:4524–4531
Barnabei VM, Cochrane BB, Aragaki AK et al (2005) Menopausal symptoms and treatment-related effects of estrogen and progestin in the Women’s Health Initiative. Obstet Gynecol 105:1063–1073
Devins GM (2010) Using the illness intrusiveness ratings scale to understand health-related quality of life in chronic disease. J Psychosom Res 68:591–602
Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D (2002) Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy–Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 24:49–58
Canada AL, Murphy PE, Fitchett G, Peterman AH, Schover LR (2008) A 3-factor model for the FACIT-Sp. Psycho-Oncology 17:908–916
Carver CS (1997) You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med 4:92–100
Lasry JC, Margolese RG, Poisson R et al (1987) Depression and body image following mastectomy and lumpectomy. J Chronic Dis 40:529–534
Sherbourne CD, Stewart AL (1991) The MOS social support survey. Soc Sci Med 32:705–714
Scheier MF, Carver CS (1985) Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol 4:219–247
Nagelkerke JD (1991) A note on a general definition of the coefficient of determination. Biometrika 78:691–692
Bloom JR, Stewart SL, Johnston M, Banks P (1998) Intrusiveness of illness and quality of life in young women with breast cancer. Psycho-Oncology 7:89–100
Dunn LB, Cooper BA, Neuhaus J et al (2011) Identification of distinct depressive symptom trajectories in women following surgery for breast cancer. Health Psychol 30(6):683–692
Burwell SR, Case LD, Kaelin C, Avis NE (2006) Sexual problems in younger women after breast cancer surgery. J Clin Oncol 24:2815–2821
Ganz PA, Rowland JH, Desmond K, Meyerowitz BE, Wyatt GE (1998) Life after breast cancer: understanding women’s health-related quality of life and sexual functioning. J Clin Oncol 16:501–514
Acknowledgments
The authors thank the funding provided by the Department of Defense Grant #DAMD 17-01-0447.
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Avis, N.E., Levine, B., Naughton, M.J. et al. Explaining age-related differences in depression following breast cancer diagnosis and treatment. Breast Cancer Res Treat 136, 581–591 (2012). https://doi.org/10.1007/s10549-012-2277-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2277-0