Abstract
There is growing evidence that certain breast cancer (BC) risk factors specifically increase the risk for specific molecular tumor subtypes. Different molecular subtypes of BC can partly be described by analyzing proliferation in tumors. Very few data are available regarding the association of mammographic density (MD), as a BC risk factor, with proliferation. The aim of this study was to analyze the association between Ki-67 expression in BCs and MD. In this case-only study, data on BC risk factors, hormone receptor expression, and MD were available for 1,975 patients with incident BC. MD was assessed as percentage mammographic density (PMD) using a semiautomated method by two readers for every patient. The association of the Ki-67 proliferation index and PMD was studied using multifactorial analyses of covariance (ANCOVA), with PMD as the target variable and including well-known factors that are also associated with MD such as age, parity, use of hormone replacement therapy (HRT), and body mass index (BMI). There were no significant differences in PMD between women with BC who had low and high Ki-67 values (P = 0.31). However, there were relevant differences in women with low BMI (P = 0.07), and in women using postmenopausal HRT (P = 0.06) as well as in women with low PR values (P = 0.07). In these subgroups, the Ki-67 expression index increased with decreasing PMD. Likewise PMD is correlated with BMI, parity status, and menopausal status stronger in patients with low proliferating tumors, and with progesterone receptor expression in patients with high proliferating tumors. MD correlates inversely with Ki-67 proliferation in BC tumors only in some subgroups of BC patients, defined by commonly known BC risk factors that are usually associated with MD as well.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The molecular diversity of breast cancer (BC) is thought to be responsible for inter-individual differences in the prognosis and therapy response. The discovery of the molecular pathways that are involved in the pathogenesis of BC and therapy resistance not only helped to improve the ability to predict the prognosis and therapy response but also helped in developing new anticancer drugs [1]. Efforts to predict the risk of BC are increasingly focusing on identifying specific molecular subtypes of breast cancer [2] that may have implications for the development of new preventive drugs.
In relation to molecular characteristics and therapy decisions for BC patients, some parameters are already taken into consideration for stratifying the patients. These include the estrogen receptor (ER), progesterone receptor (PR), and HER2/neu receptor (HER2). Additionally, grading also reflects some molecular characteristics, such as proliferation. It has been debated in recent years whether the proliferation marker Ki-67 should be taken into account routinely in treatment decisions [3]. A high Ki-67 proliferation index has generally been described as a parameter associated with an unfavorable prognosis [4–6]. Ki-67 is helpful for categorizing hormone receptor-positive breast cancers further into subgroups that are similar to the molecular types luminal A and luminal B [7, 8] and for stratifying triple-negative and ER-positive BC into lesions that respond to chemotherapy and those that do not [9].
With regard to molecular characteristics and BC risk prediction, there have been studies in which specific risk factors were associated with molecular tumor characteristics. For example, nulliparity was found to be associated with a reduced risk for triple-negative breast cancers (TNBCs) and an increased risk for ER-positive BC [10]. Other reports have linked early age at menarche, nulliparity, and late age at first full-term pregnancy with an increased risk of ER-positive, but not ER-negative BC [11]. With regard to genetic risk factors, some variants have been associated with the risk for ER-positive BC, while others are specifically associated with ER-negative BC [12–19]. Some loci have even been associated with the risk for TNBC [19–22].
Mammographic density is one of the most important risk factors for breast cancer. The risk may be increased by a factor of five in women with a mammographically dense breast [23–25]. However, the available data on the association between MD and specific tumor characteristics are limited. MD appears to be associated with an increased risk for ER-negative cancer, rather than ER-positive cancer [26]. Our group has previously reported on an inverse association between MD and ER expression and a positive correlation with PR expression [27]. To the best of our knowledge, there have only been two negative reports that investigated MD and proliferation in tumors [28, 29] and only one study that has looked at MD and differential BC risk with regard to grading [26]. The latter study found that MD had a greater effect on the risk for higher-grade tumors.
The aim of the present study was therefore to investigate the association between MD and proliferation as assessed by Ki-67 immunohistochemistry in patients with invasive BC, in a large consecutive cohort of breast cancer patients, stratified for the main molecular subtypes: TNBC, HER2-overexpressing BC, and ER/PR-expressing BC.
Patients and methods
The patients were selected from the BC database at the University Breast Center for Franconia. A total of 5,110 patients with invasive BC are documented in the database for the period 1995–2008. In the analysis presented here, patients were excluded in the following hierarchical order: no mammogram performed at the University Breast Center at the time of the primary diagnosis or bilateral synchronous breast cancer (excluding 1,989 patients, 485 of whom had prevalent cases); unknown ER or unknown PR status (excluding 711 patients); and unknown Ki-67 status (excluding 435 patients). The final study population consisted of 1,975 patients with incident, unilateral, invasive BC.
Data collection and follow-up
All patient characteristics and tumor characteristics were documented as part of the certification processes required by the German Cancer Society (Deutsche Krebsgesellschaft) and by the German Society for Breast Diseases (Deutsche Gesellschaft für Senologie) [30]. Certification requires tumor characteristics, treatment data, some epidemiological data, histopathological characteristics, tumor treatments, and follow-up to be documented and audited annually. Information about HRT usage in the patient’s history was collected from the patients’ charts at the time of the primary diagnosis. BMI at the time of diagnosis was obtained from measurements in the hospital, which were carried out during treatment planning (i.e., before surgery or chemotherapy).
Mammographic density
The quantitative computer-based threshold density assessments and breast area measurements were made by two different readers with explicit training in the method used. Each mammogram was read by both readers independent of each other. The assessment method has been described and validated previously elsewhere [31].
Briefly, the images (analog images and printouts of processed digital images) were digitized using the CAD PRO Advantage® film digitizer (VIDAR®, Herndon, Virginia, USA), and for assessment of the density fraction, the reader used the Madena software program, Version X (Eye Physics, LLC, Los Alamitos, California, USA) [31]. All mammograms were read in random order by two different observers, who were unaware of any previous classifications or pathological findings. The average of the two observers’ values for percentage mammographic density (PMD) was used for this analysis, into which only measurements of contralateral cranio-caudal (CC) images were included.
Pathology
In the course of routine patient care, dedicated breast pathologists at the University Breast Center for Franconia examined pathologic specimens from all of the patients included in this study. The histological type, grade, resection status, and TNM stage were determined, and expression of ER, PR, and HER2 was analyzed immunohistochemically in accordance with the standard practice in certified breast centers in Europe [32]. ER and PR status are based on estimates of the percentage of clearly positive-stained nuclei of cancer cells (from 0 to 100 %). Ki-67 staining was performed with the MIB1 clone, yielding the percentage of positive nuclei of tumor cells (from 0 to 100 %). HER2 testing was performed with the DAKO test (Dako, Denmark). Information about tumor characteristics was subsequently transferred from the histopathological reports into our clinical database.
Statistical methods
The association between mammographic density and various patient and tumor characteristics was analyzed using linear models. Simple linear regression analyses were used for the ordinal predictors pT, grading, ER, and PR. Quadratic regression analyses were used for age at diagnosis and BMI, since a preliminary analysis had shown that models with age squared or BMI squared as additional predictor fitted better. The predictor Ki-67 was grouped into two categories (≤14 and >14), where the median Ki-67 value was used as the cut-off point. Ki-67 was categorized to simplify the interpretation of the multifactorial analyses introduced below. One-way analysis of variance (ANOVA) were used for the categorical predictors menopausal and HRT status, nodal status, HER2 status, and histology, each categorized as in Table 1. Mean PMDs with 95 % confidence intervals and the P-values of F-tests are shown.
The association between Ki-67 and mammographic density, taking into account the well-known predictors mentioned above, was studied using multifactorial analysis of covariance (ANCOVA) with PMD as the target variable. Initially, an ANCOVA with all predictors except Ki-67 was fitted. The predictors were used in the same way—i.e., categorical, linear, or quadratic, as above. Backward stepwise variable selection was then carried out to obtain the best model in accordance with the Akaike information criterion (final model without Ki-67). Next, another ANCOVA was fitted containing Ki-67, the predictors from the final model without Ki-67, and the interactions of Ki-67 with these predictors. The variable selection procedure described above was carried out again, but with the condition that the selected predictors from the final model without Ki-67 were kept. The resulting model (final model with Ki-67) was compared with the final model without Ki-67 using the likelihood ratio test. A significant test result means that Ki-67 has predictive value independent of the well-established predictors considered. P-values of F-tests (type III analysis) and P-values of linear contrasts of the final model with Ki-67 and adjusted mean PMD values with 95 % confidence intervals were shown.
The model selection procedure described above was evaluated by tenfold cross-validation with 20 replications. The mean R 2 statistic for the final models with Ki-67 constructed with training data sets and applied to validation data sets was shown.
Similar analyses were carried out for the subgroup of patients with triple-negative tumors (ER <10, PR <10, and HER2-negative), the subgroup of hormone receptor-positive (ER ≥10 or PR ≥10) and HER2-negative patients, and also the subgroup of HER2-positive patients. Obviously, ER, PR, and HER2 were not used as predictors.
All of the tests were two-sided, and a P-value <0.05 was regarded as statistically significant. Calculations were carried out using the SAS software package (version 9.2, SAS Institute Inc., Cary, North Carolina, USA) and the R system for statistical computing (version 2.13.1; R Development Core Team, Vienna, Austria, 2011).
Results
At least PMD, Ki-67, and one of the additional patient and tumor characteristics were available for a total of 1,975 patients. The patients’ mean age was 59.3 years (±12.8 years) and their mean BMI was 26.2 kg/m2 (±4.8 kg/m2). PMD was measured on average as a percentage of 36 % (±19 %). The study included 455 premenopausal or perimenopausal women (24.2 %), 1,425 postmenopausal patients (75.8 %), and 95 women with unknown menopausal status. The patients’ characteristics are shown in Table 1.
With regard to tumor characteristics, most of the patients had a pT1 tumor (n = 1,070, 55.4 %) and were node-negative (n = 1,212, 63.3 %). Most of the tumors were ER-positive and PR-positive, with medians of positively stained tumor cells at 70 and 30 %, respectively. HER2 status was available for 1,792 patients, and 281 were HER2-positive (15.7 %). The patient group was dichotomized into those with tumors in which more than 14 % of the tumor cells stained positive for Ki-67 and those in which ≤14 % of tumor cells stained positively.
The initial analysis of covariance, which did not include Ki-67, identified age, BMI, parity, menopausal and HRT status, pT, grading, and histology as relevant predictors of PMD. Nodal status and HER2 status were dropped during the variable selection process; that is, their predictive value appeared to be irrelevant, or was already explained by the other selected variables.
The ultimate analysis of covariance, taking into account the relevant predictors described above and also Ki-67 and its interactions with those predictors, showed that prediction of PMD can be improved overall by taking Ki-67 into account (P < 0.01, likelihood ratio test). In particular, interactions of Ki-67 with PR (P = 0.03, F test), BMI (P < 0.01, F-test), menopausal status and HRT usage (P = 0.02, F-test), and parity (P = 0.11, F test) improved the prediction. The other interaction terms were dropped during the variable selection process. The cross-validated R 2 was 0.39. Adjusted PMDs based on this final model are shown in Table 2.
Overall, there were no significant differences in adjusted PMD between women with low Ki-67 indices (PMD = 36; 95 % CI 34–38) and high Ki-67 indices (PMD = 35; 95 % CI 33–37). More precisely, however, there were relevant differences in women with a low BMI (P = 0.07), and in postmenopausal women using HRT (P = 0.06), as well as in women with low PR values (P = 0.07). In these three subgroups, PMD decreased with increasing Ki-67 indices.
As in the unadjusted analysis, the adjusted PMD is inversely associated with age (P < 0.00001) and ER (P < 0.01). BMI and PMD are also inversely associated; the differences are slightly larger in women who have developed a tumor with a low Ki-67 index than in women who have developed a tumor with a high Ki-67 index. Significant differences in PMD between women with and without children were detected in women with tumors with a low Ki-67 index (P < 0.01), but not in women who developed a tumor with a high Ki-67 index (P = 0.08).
PR expression was higher in women with a higher PMD in the subgroup of patients who developed a BC with a high Ki-67 index (P < 0.01), but there were no differences in PMD with regard to PR expression in women who developed a BC with a low Ki-67 index (P = 0.92).
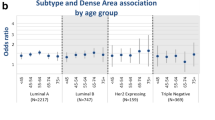
All of the above analyses were repeated for clinically relevant molecular subgroups—TNBC/(ER-positive or PR-positive) and HER2-negative/HER2-positive—but Ki-67 did not improve the prediction of PMD in the subgroup of triple-negative patients (n = 243; P = 0.12, likelihood ratio test) or in the subgroup of HER2-positive patients (n = 280; P = 0.13, likelihood ratio test).
Ki-67 improved the prediction of PMD in the subgroup of hormone receptor-positive and HER2-negative patients (n = 1,262; P = 0.03, likelihood ratio test). As in the main analyses, the interactions of Ki-67 with BMI and parity status were preserved in the final prediction model. The associations with PMD are the same as in the main analysis.
Discussion
This retrospective case-only study did not demonstrate a general association between tumor proliferation, as assessed by Ki-67 immunohistochemistry, and MD, measured as PMD. However, it does show that the commonly reported associations between PMD and BMI, menopausal and HRT status, as well as parity and PR expression, differ in patients with high-proliferation or low-proliferation tumors.
A few other case-only studies have also reported on the association of Ki-67 and MD. Two studies using the American College of Radiology (ACR) categories for MD assessment and with sample sizes of 546 and 434, respectively, found no association between MD and Ki-67 indices [28, 29]. A more recent study looked for associations between PMD and dense area and Ki-67 staining in 159 women with BC from the multiethnic cohort in Hawaii, and did not find any associations either [33]. The present generally negative findings are therefore also consistent with the findings of these published studies.
No Ki-67 staining was reported in a larger case–control study that analyzed associations between breast density and subsequent breast cancer, stratified by tumor characteristics. In women with higher PMD values, Yaghjyan et al. [26] reported a higher risk for tumors with a higher grading than for tumors with a lower grading. In comparison with women with a PMD <10 %, women with a PMD >50 % had an OR of 1.25 (95 % CI 0.6–2.6) for grade 1 tumors, an OR of 3.0 (95 % CI 1.8–5.1) for grade 2 tumors, and an OR of 5.3 (95 % CI 2.8–10.1) for grade 3 tumors. Although grading represents not only proliferation but also architectural and cytological characteristics, grading and the Ki-67 index are regularly strongly correlated with each other. The present study did not show any association between PMD and grading, nor did two of the above-mentioned case-only studies [28, 29]. In contrast to the correlation between PMD and grading reported by Yaghjyan et al., however, Aiello et al. [28] described a weak inverse association between MD and grading in a subgroup of BC patients in whom the disease was not detected during screening (i.e., interval cancers). The present study mainly included patients who were not taking part in a screening program, and the patients can therefore not be divided into these two groups.
The new finding in the present study is the interaction of the association between commonly reported factors influencing MD and Ki-67 expression in BC. This might shed some light on the way in which known risk factors for BC such as BMI, parity, and HRT use interact with MD with regard to molecular characteristics of the tumor—i.e., proliferation as assessed by Ki-67 in the present study.
The association between BMI, parity, and HRT use among postmenopausal women and PMD was stronger in patients who developed a tumor with a low Ki-67 index. It is known that analyzing proliferation helps classify tumors with regard to the molecular subtypes of breast cancer [7, 8, 34]. It helps classify hormone receptor-positive and luminal breast cancers into so-called luminal A breast cancers, which have a good prognosis, and luminal B breast cancers, which have a more unfavorable prognosis. Among the triple-negatives, Ki-67 is able to differentiate between tumors with a good response to chemotherapy and tumors that are treatment-resistant [9]. The subgroup analysis according to these molecular subtypes in this study confirmed the findings of the total study population only in the subgroup of patients with hormone receptor-positive/HER2-negative (luminal-type) BC. No associations were found in triple-negative BC or HER2-positive BC. However, the sample sizes of the two latter groups were only 243 and 280, so that this negative finding might be due to weak statistical power.
With regard to the findings concerning PR and Ki-67, our group previously reported a positive association between PR expression and PMD [27]. The analysis presented here provides some evidence that this association is stronger in patients who developed a tumor with a high Ki-67 index, whereas the association is not present in patients who developed a low-proliferation tumor.
The strengths of the present study are the large sample size and the fact that all of the mammograms were assessed by two independent readers who were not aware of the other reader’s findings. Another aspect implies advantages and disadvantages. On the one hand, the methods of Ki-67 staining and evaluation used are part of routine clinical practice. The staining and assessment of whole sections may be a strength, as most published studies use tissue microarrays and are unable to account for heterogeneously expressed Ki-67 in a whole slide section. In addition, the fixation and staining procedures were carried out directly after the fixation and embedding of the specimens into paraffin. This may have reduced the potential for variability in studies using paraffin blocks of different ages, ranging up to decades. On the other hand, routine clinical assessment means that different batches of chemicals and antibodies are used, and also that there are different observers involved. Another weakness is the design as a case-only study, as this means that no—or only very limited—interpretations with regard to breast cancer risk and the characteristics analyzed can be made. It has to be mentioned that both, analog films and printouts of processed, digital images were used and this might have an influence on the analyses, however including the type of mammogram (analog vs. digital printouts) into our prediction models and rerunning the analyses did not yield any evidence, that the correlation of PMD and Ki-67 is influenced by type of mammogram.
In conclusion, this study found evidence that the associations between MD and the commonly described BC risk factors BMI, HRT use, and parity differ in patients with high-proliferation and low-proliferation breast cancer tumors. Likewise this effect was seen as well concerning PR status. As breast cancer risk research has developed not only to describe the pure BC risk, but also to take molecular characteristics into account, Ki-67 appears to be a perfect candidate for inclusion in this type of research. Whether the associations described here have any impact on the risk associations of specific molecular subtypes of breast cancer will need to be investigated in further large case–control studies.
References
Liedtke C, Wolf MK, Kiesel L (2010) New concepts for targeted systemic therapy in breast cancer. Geburtsh Frauenheilkd 70(8):625–633. doi:10.1055/s-0030-1250182
Fasching PA, Ekici AB, Adamietz B et al (2011) Breast cancer risk—genes, environment, and clinical practice. Geburtsh Frauenheilkd 71(12):1056–1066. doi:10.1055/s-0031-1280437
Yerushalmi R, Woods R, Ravdin PM et al (2010) Ki67 in breast cancer: prognostic and predictive potential. Lancet Oncol 11(2):174–183. doi:10.1016/S1470-2045(09)70262-1
Dowsett M, Nielsen TO, A’Hern R et al (2011) Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer working group. J Natl Cancer Inst 103(22):1656–1664. doi:10.1093/jnci/djr393
Paik S, Shak S, Tang G et al (2004) A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351(27):2817–2826. doi:10.1056/NEJMoa041588
Cuzick J, Dowsett M, Pineda S et al (2011) Prognostic value of a combined estrogen receptor, progesterone receptor, Ki-67, and human epidermal growth factor receptor 2 immunohistochemical score and comparison with the Genomic Health recurrence score in early breast cancer. J Clin Oncol 29(32):4273–4278. doi:10.1200/JCO.2010.31.2835
Sotiriou C, Pusztai L (2009) Gene-expression signatures in breast cancer. N Engl J Med 360(8):790–800. doi:10.1056/NEJMra0801289
Cheang MC, Chia SK, Voduc D et al (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101(10):736–750. doi:10.1093/jnci/djp082
Fasching PA, Heusinger K, Haeberle L et al (2011) Ki67, chemotherapy response, and prognosis in breast cancer patients receiving neoadjuvant treatment. BMC Cancer 11:486. doi:10.1186/1471-2407-11-486
Phipps AI, Chlebowski RT, Prentice R et al (2011) Reproductive history and oral contraceptive use in relation to risk of triple-negative breast cancer. J Natl Cancer Inst 103(6):470–477. doi:10.1093/jnci/djr030
Yang XR, Chang-Claude J, Goode EL et al (2011) Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst 103(3):250–263. doi:10.1093/jnci/djq526
Stacey SN, Manolescu A, Sulem P et al (2008) Common variants on chromosome 5p12 confer susceptibility to estrogen receptor-positive breast cancer. Nat Genet 40(6):703–706. doi:10.1038/ng.131
Stacey SN, Manolescu A, Sulem P et al (2007) Common variants on chromosomes 2q35 and 16q12 confer susceptibility to estrogen receptor-positive breast cancer. Nat Genet 39(7):865–869. doi:10.1038/ng2064
Garcia-Closas M, Chanock S (2008) Genetic susceptibility loci for breast cancer by estrogen receptor status. Clin Cancer Res 14(24):8000–8009. doi:10.1158/1078-0432.CCR-08-0975
Garcia-Closas M, Hall P, Nevanlinna H et al (2008) Heterogeneity of breast cancer associations with five susceptibility loci by clinical and pathological characteristics. PLoS Genet 4(4):e1000054. doi:10.1371/journal.pgen.1000054
Thomas G, Jacobs KB, Kraft P et al (2009) A multistage genome-wide association study in breast cancer identifies two new risk alleles at 1p11.2 and 14q24.1 (RAD51L1). Nat Genet 41(5):579–584. doi:10.1038/ng.353
Turnbull C, Ahmed S, Morrison J et al (2010) Genome-wide association study identifies five new breast cancer susceptibility loci. Nat Genet 42(6):504–507. doi:10.1038/ng.586
Ahmed S, Thomas G, Ghoussaini M et al (2009) Newly discovered breast cancer susceptibility loci on 3p24 and 17q23.2. Nat Genet 41(5):585–590. doi:10.1038/ng.354
Broeks A, Schmidt MK, Sherman ME et al (2011) Low penetrance breast cancer susceptibility loci are associated with specific breast tumor subtypes: findings from the Breast Cancer Association Consortium. Hum Mol Genet 20(16):3289–3303. doi:10.1093/hmg/ddr228
Antoniou AC, Beesley J, McGuffog L et al (2010) Common breast cancer susceptibility alleles and the risk of breast cancer for BRCA1 and BRCA2 mutation carriers: implications for risk prediction. Cancer Res 70(23):9742–9754. doi:10.1158/0008-5472.CAN-10-1907
Antoniou AC, Wang X, Fredericksen ZS et al (2010) A locus on 19p13 modifies risk of breast cancer in BRCA1 mutation carriers and is associated with hormone receptor-negative breast cancer in the general population. Nat Genet 42(10):885–892. doi:10.1038/ng.669
Stevens KN, Vachon CM, Lee AM et al (2011) Common breast cancer susceptibility loci are associated with triple-negative breast cancer. Cancer Res 71(19):6240–6249. doi:10.1158/0008-5472.CAN-11-1266
McCormack VA, dos Santos SI (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev 15(6):1159–1169. doi:10.1158/1055-9965.EPI-06-0034
Boyd NF, Guo H, Martin LJ et al (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356(3):227–236. doi:10.1056/NEJMoa062790
Heusinger K, Loehberg CR, Haeberle L et al (2011) Mammographic density as a risk factor for breast cancer in a German case–control study. Eur J Cancer Prev 20(1):1–8. doi:10.1097/CEJ.0b013e328341e2ce
Yaghjyan L, Colditz GA, Collins LC et al (2011) Mammographic breast density and subsequent risk of breast cancer in postmenopausal women according to tumor characteristics. J Natl Cancer Inst 103(15):1179–1189. doi:10.1093/jnci/djr225
Heusinger K, Jud SM, Haberle L et al (2012) Association of mammographic density with hormone receptors in invasive breast cancers—results from a case-only study. Int J Cancer. doi:10.1002/ijc.27515
Aiello EJ, Buist DS, White E et al (2005) Association between mammographic breast density and breast cancer tumor characteristics. Cancer Epidemiol Biomarkers Prev 14(3):662–668. doi:10.1158/1055-9965.EPI-04-0327
Fasching PA, Heusinger K, Loehberg CR et al (2006) Influence of mammographic density on the diagnostic accuracy of tumor size assessment and association with breast cancer tumor characteristics. Eur J Radiol 60(3):398–404. doi:10.1016/j.ejrad.2006.08.002
Beckmann MW, Brucker C, Hanf V et al (2011) Quality assured health care in certified breast centers and improvement of the prognosis of breast cancer patients. Onkologie 34(7):362–367. doi:10.1159/000329601
Ursin G, Astrahan MA, Salane M et al (1998) The detection of changes in mammographic densities. Cancer Epidemiol Biomarkers Prev 7(1):43–47
Blamey RW, Cataliotti L (2006) EUSOMA accreditation of breast units. Eur J Cancer 42(10):1331–1337. doi:10.1016/j.ejca.2006.04.003
Verheus M, Maskarinec G, Erber E et al (2009) Mammographic density and epithelial histopathologic markers. BMC Cancer 9:182. doi:10.1186/1471-2407-9-182
Perou CM, Sorlie T, Eisen MB et al (2000) Molecular portraits of human breast tumours. Nature 406(6797):747–752. doi:10.1038/35021093
Acknowledgments
Katharina Heusinger was funded by the ELAN Program at Erlangen University Hospital, Friedrich Alexander University of Erlangen-Nuremberg, Germany. We are grateful to Michael Robertson for professional medical editing services.
Conflict of interest
The authors hereby declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Katharina Heusinger and Sebastian M. Jud contributed equally to this study.
Rights and permissions
About this article
Cite this article
Heusinger, K., Jud, S.M., Häberle, L. et al. Association of mammographic density with the proliferation marker Ki-67 in a cohort of patients with invasive breast cancer. Breast Cancer Res Treat 135, 885–892 (2012). https://doi.org/10.1007/s10549-012-2221-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2221-3