Abstract
Anthracycline is a DNA topoisomerase 2-α (TOP2A) inhibitor and its concomitant over expression with Human Epidermal Growth Factor Receptor 2 (HER2) was investigated of being predictive for the response to anthracycline-based chemotherapies in breast cancer. 309 early and local advanced breast cancer patients were treated with anthracycline-based neoadjuvant chemotherapies in intense dose dense (IDD) (CE, Cyclophosphamide + Epirubicin) or conventional (TE, Paclitaxel + Epirubicin) regimens. HER2 proteins were qualitatively analyzed by immunohistochemistry (IHC) of primary tumor core biopsies, and TOP2A gene amplification levels of HER2 over-expressing cases were quantified by quantitative real-time polymerase chain reaction (qRT-PCR). Overall pathological complete response rate (pCR) was achieved in 14.3 %. HER2 was over expressed in 80/309 (25.9 %) cases, of which 61/80 cases have been tested for their TOP2A status. Over expression of HER2 was significantly positively correlated with higher pCR rates compared to low HER2 expression (27.5 % vs. 9.6 %, P < 0.001). Concurrent high TOP2A amplification led to a significantly higher pCR rate compared to low or no TOP2A amplification (56.3 % vs. 13.8 %, P = 0.001). HER2 over expression was associated with a significantly higher pCR rate only when TOP2A was also amplified (56.3 % vs. 9.6 %, P < 0.001), but not when it was deleted or normal (13.8 % vs. 9.6 %, P = 0.183) compared to HER2 low-expressing tumors. The interaction between HER2 or TOP2A and anthracycline-based regimen was observed in IDD and conventional neoadjuvant chemotherapies. The TOP2A amplification is related to anthracycline-based neoadjuvant chemotherapy sensitivity, and TOP2A should be included in future studies in breast cancer as a predictive marker.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the past decade, a large number of studies have shown that HER2-positive breast cancers may be more sensitive to an anthracycline-based chemotherapy, compared to non-anthracycline agents [1–5] and a comprehensive meta-analysis based on published studies has indicated that the benefit of anthracycline-based adjuvant therapies is largely restricted to the HER2-positive subgroup of human breast cancers [6]. However, recent clinical studies showed that the predictive value of anthracycline efficacy in HER2-positive breast cancers may be related to TOP2A co-expression and clinical studies about adjuvant chemotherapy revealed that TOP2A amplification is only occurring simultaneously with HER2 over expression which might play a role in predicting the efficacy of anthracycline-based regimens [7–12]. The TOP2A protein, encoded by the TOP2A gene, is a key enzyme of DNA replication, cell-cycle progression, as well as chromosome segregation and a target of anthracycline [13]. However, the opinions are inconclusive concerning the predictive role of the TOP2A status due to a lack of measurements in primary tumors so far [14–17] and most of the studies were performed in either the metastatic or adjuvant settings. Therefore, we analyzed the efficacy and prognostic factors in patients treated with 2 anthracycline-based neoadjuvant chemotherapy regimens and designed pCR as a direct measure of neoadjuvant chemosensitivity. We hypothesized that an association between the sensitivity to anthracyclines and HER2 expression is mainly derived from the chromosomal co-amplification of the TOP2A gene [18, 19]. Preliminary results showed that HER2 over expression was significantly related to the efficacy of anthracycline-based neoadjuvant chemotherapies and the correlation between HER2 over expression and TOP2A gene amplification in respect to treatment sensitivity was further analyzed.
Methods
Patients
Clinical data were collected from 309 eligible patients who received neoadjuvant chemotherapy in our hospital from 2003 to 2008 in this study. The 309 patients in this trial were randomly distributed into a CE and TE group (1:2) and treated concurrently. All patients received either four cycles neoadjuvant chemotherapy of cyclophosphamide (600 mg/m2, q14d) and epirubicin (80 mg/m2, q14d) on day 1 followed by postoperative four cycles paclitaxel (175 mg/m2, q14d) on day 1 (CE regimen) or four cycles TE regimen of epirubicin (75 mg/m2, q21d) on day 1, and paclitaxel (175 mg/m2, q21d) on day 2 and 2 cycles repeated after surgery. The clinical response was evaluated according to the RECIST 1.0 criteria every 2 cycles and the toxicity was recorded every cycle (according to CTC 3.0 version). Patients with partial response (PR) received surgical treatment after 4 cycles of chemotherapy and sequential paclitaxel or repeated TE regimen after surgery. Patient who met the criteria for progressive disease (PD) at the initial efficacy evaluation received surgery as soon as possible and alternative postoperative regimens. There was a balanced distribution in both CE and TE groups among age, menstrual status, estrogen receptor (ER)/progesterone receptor (PR) status, HER2 status, tumor size, and lymph node metastasis (Table 1). Last follow-up date was October 2010, with median follow-up of 38 months (range: 12–39 months).
Collection and testing methods of primary tumor specimens
All patients’ histopathological specimens of primary tumors were obtained by core needle biopsy before the onset of neoadjuvant chemotherapies and the ER, PR and HER2 status of the invasive primary tumor regions were determined. In this study, we analyzed 61 paraffin blocks containing residual tumor tissues of 80 patients with HER2 over expression (HER2 3+ detected by immunohistochemistry assays).
Immunochemistry (IHC) measurements
For IHC we used a HER2-specific antibody (clone A-0485; DAKO; dilution 1:100). HER2 staining was graded according to staining observed in <10 % of the tumor cells (score 0); faint/barely perceptible staining detected in ≥10 % of the tumor cells (score 1+); and a moderate or uniform, intense membrane staining observed in ≥10 % of invasive cells (score 2+ or 3+, respectively) [20].
TOP2A genomic copy number detection
During the study, the paraffin blocks were used to determine TOP2A gene amplification by qRT-PCR of the HER2 over-expressing patients with known clinical and pathological data. We extracted total DNA from the paraffin-embedded tissues by ambion nucleic acid isolation kit, according the manufacturer’s protocol (Ambion, USA), and then analyzed the DNA using TaqMan TOP2A copy number assays (ABI) (Hs02497108_cn and Hs02221874_cn) from which one amplification site was located adjacent to the TOP2A-coding region and the other site was in the opposite direction, far from the HER2 3′-end. In order to account for increased TOP2A gene copy number due to chromosome 17 polysomy, we selected the relatively stable gene COL1A1 using TaqMan assay (Hs00453869_cn) from ABI also located on chromosome 17 as internal marker gene. The genomic COL1A1 gene copy number, tested by qRT-PCR, was regarded as the number of chromosome 17. TOP2A gene amplification was defined as a ratio of absolute genomic TOP2A gene copy number, measured by fluorescent qRT-PCR to the reference gene COL1A1 (>2.0). In case the ratio was ≤2.0, the specimen was considered to lack gene amplification [21].
Results
The effect of TOP2A amplification on the efficacy of anthracycline-based neoadjuvant chemotherapy
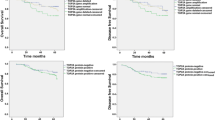
Overall pathological complete response rate (pCR) was achieved in 14.3 %. 80 of 309 (25.9 %) enrolled patients were pathologically diagnosed with HER2 positivity by core needle biopsy of primary tumors. The objective response rates (ORR) and pathological complete response (pCR) rates in patients with HER2 over expression were significantly higher than in patients with low HER2 expression (ORR of 86.3 and 72.9 %, respectively, P = 0.010; pCR of 27.5 and 9.6 %, respectively, P < 0.001). The higher response was observed in patients with HER2 over expression in both the CE (IDD) and the TE chemotherapy group. The pCR rate in patients with versus without HER2 over expression in the CE group and TE group were 20.0 % versus 5.6 % (P = 0.029), and 29.1 % versus 12.6 % (P = 0.007), respectively (Table 1). A TOP2A amplification was demonstrated in 52.5 % (32/61) and normal TOP2A coding or deletion was detected in 47.5 % (29/61) cases. A pCR could be achieved in 22 cases with HER2 over expression. A significant difference of the pCR rate was observed between the patients with and without TOP2A amplification (56.2 % vs. 13.8 %, P = 0.001). The HER2 low expression group was further compared with HER2 over expression patients with and without TOP2A amplification, respectively. The results revealed that the drug response efficacy of HER2 over expression without TOP2A amplification (pCR of 13.8 %) was not significantly higher (P = 0.183) than in patients with low HER2 expression (pCR of 9.5 %). In contrast, comparing the same low HER2-expressing group (pCR of 9.5 %) with HER2 over expressing and TOP2A amplified subgroup (pCR of 56.2 %), there was a significant difference in drug response (P < 0.001). Therefore, the difference in efficacy between the HER2 low expression and HER2 over expression groups was mainly derived from the sensitivity of anthracycline-based neoadjuvant chemotherapy in the subgroup population with both HER2 over expression and TOP2A amplification (Table 2; Fig. 1). Twenty-two cases with pCR in the HER2 over expression group were included in the 61 patients whose TOP2A gene status were identified, whereas 19 cases with unknown TOP2A gene status did not achieve pCR. In order to adjust for statistical bias caused by excessive cases (23.8 %) that did not receive a TOP2A test, we did an inferiority-prior hypothesis: Under assumption that the 19 non-PCR patients without TOP2A test showed TOP2A amplifications, the rate of pCR was reduced to 35.3 % (18/(32 + 19)) in the TOP2A amplification group, whereas the rate of pCR in no TOP2A amplification group was kept at 13.8 %. There is a statistically significant difference in pCR rates between TOP2A amplification and no TOP2A amplification groups via Chi-square test (35.3 % vs. 13.8 %, P = 0.039). This result suggested that the cases with HER2 over expression and TOP2A amplification obtained more benefit from anthracycline-based neoadjuvant chemotherapy (Table 3).
The effect of HER2 over expression with TOP2A amplification on the efficacy of different neoadjuvant chemotherapy regimens
This study revealed that HER2 over expression had a significant effect on the efficacy of neoadjuvant chemotherapy in either CE intensive regimen or TE standard regimen. Does the TOP2A gene also have such a predictive value for different anthracycline-based regimens? We assigned 61 cases with TOP2A test results available in terms of neoadjuvant chemotherapy regimens they received. 6 of 21 cases in the CE intensive chemotherapy group achieved pCR and had TOP2A amplifications, whereas none of the other 8 cases without TOP2A amplification achieved pCR. The pCR rate for patients with and without TOP2A amplification in this group was 46.2 % and 0, respectively, with a significant difference (P = 0.032). In the TE standard 3-week chemotherapy group, the pCR rate for cases with TOP2A amplification was higher than in cases without TOP2A amplification (75.0 % vs. 16.7 %, P < 0.001) (Table 4).
Discussion
Despite the proved association between HER2 and anthracycline-based chemotherapies in a large number of studies, it is still under discussion whether HER2 expression is the only cause of the sensitivity to anthracyclines. It has been found that a complex diversity of HER2 gene aberrations is occurring in terms of length, frequency, and amplification. Because of its close location on chromosome 17, about half of the HER2 amplifications are accompanied by concomitant TOP2A gene co-amplifications as an amplicon which spans the complete genomic area of both genes [13, 22]. On the other hand, in other cells HER2 aberration led to interstitial TOP2A deletions, probably due to an assumed DNA repair mechanism after initial solely HER2 amplification [13]. A recent meta-analysis of 8 independent clinical studies showed that breast cancer patients with HER2 over expression obtained more benefits from an anthracycline-based adjuvant chemotherapy [5]. However, this clinical finding was contradictory to the results of preclinical studies in which the effect of a representative anthracycline drug, doxorubicin, on the sensitivity of breast cancer cell lines transfected with the HER2 gene was not higher than in HER2-negative cell lines [23]. The only explanation of this contradiction was that the cell lines in that laboratories were transfected with the solely HER2 gene, whereas HER2 gene amplification in clinical breast cancers are frequently accompanied by co-amplification or deletion of TOP2A [13]. The results of adjuvant chemotherapy studies suggested that HER2 and TOP2A are a harmonious gene combination. In breast cancers with excessive tumor cell proliferation caused by HER2 amplification or over expression, a part of the cases may obtain benefits from a concurrent TOP2A amplification [24, 25]. The result of this study supported our hypothesis that the efficacy advantage of anthracycline-based chemotherapy regimens presented in breast cancer with HER2 over expression could be attributed to TOP2A amplification in some patients, and the predictive factor for response to anthracyclines was not only HER2, as been well known, but also TOP2A amplification at the neoadjuvant chemotherapy level in primary breast cancer. A retrospective study [12] of HER2 and TOP2A as predictive factors for response to anthracyclines reported by Knoop et al. in 2005 found that there was no efficacy difference between anthracycline-based chemotherapy and non-anthracycline chemotherapy in patients with HER2-positive primary breast cancer (P = 0.81); however, TOP2A amplification (or deletion) had a potential predictive role for anthracycline-based chemotherapies with a P value close to statistical significance (P = 0.06). This study supports the opinion that TOP2A rather than HER2 is the predictive factor for anthracycline-based chemotherapy response. Another study reported by Gottfried et al. confirmed this opinion for neoadjuvant therapy of breast cancer. They compared normal HER2 status breast cancer patients (pCR of 11 %) with HER2 and TOP2A co-amplification patients (pCR of 30 %, P = 0.002) and suggested benefits of anthracycline-based chemotherapy for these patients rather than for patients with HER2 over expression and normal or deleted TOP2A (pCR of 13 %, P = 0.755) [21]. The effect of TOP2A on the efficacy of anthracycline-based chemotherapy showed a high consistency between different administration methods and dose intensity regimens. We found that with intensive chemotherapy (CE) or standard 3-week regimen (TE), the pCR rate of a neoadjuvant chemotherapy was significantly improved in primary HER2 over-expressing breast cancer patients with TOP2A amplification compared to HER2 over-expressing breast cancer patients without TOP2A amplification. In this study, the predictive role of HER2 positivity with TOP2A amplification for intensive chemotherapy response confirmed previous studies of adjuvant chemotherapies [26–28]. All these studies found that compared with HER2-negative patients, patients with HER2 over-expressing breast cancers obtained more survival benefit from an intensive adjuvant chemotherapy. The concordance of this neoadjuvant study with other studies also supports the view that pathological complete response is an appropriate surrogate marker for disease-free and overall survival. Our study deeply explored the sensitivity of HER2-positive breast cancers to intensive chemotherapy at the neoadjuvant chemotherapy level, which was actually derived from an efficacy advantage of anthracycline-based intensive chemotherapy in TOP2A-amplified breast cancers. The results of this study cannot distinguish whether the high pCR rate for patients receiving neoadjuvant therapy in the TOP2A amplification group was attributed to higher sensitivity to anthracyclines or whether TOP2A might be only a predictive factor for anthracycline responses. The common study design for response predictive factors to drug regimens should be randomized to assign patients with common pathological or biological characteristics (such as TOP2A amplification) to receive specific chemotherapy regimens (such as anthracyclines) or not. Both the two neoadjuvant chemotherapy regimens in our study contained anthracyclines (epirubicin), thereby not being a predictive factor study design parameter. However, we can come to the conclusion that anthracycline-based neoadjuvant chemotherapy may significantly improve the pCR rate for breast cancer patients with TOP2A amplification. In our study, TE regimen achieved a pCR rate of 56.2 % in the HER2 and TOP2A positive group, which is similar to Trustuzumab as a drug used in neoadjuvant treatment [29]. It is worth to design a new clinical study to demonstrate whether anthracycline-based neoadjuvant chemotherapy alone is as good as a Trustuzumab-combined chemotherapy for breast cancer with HER2 & TOP2A co-amplification treatments.
Conclusion
Anthracycline-based neoadjuvant chemotherapy regimens can significantly improve the pCR rate for patients with HER2 over expression, and this efficacy advantage can be attributed to concurrent TOP2A amplification. We suggest that TOP2A amplification is a predictive marker for anthracycline-based neoadjuvant chemotherapy sensitivity.
References
Pritchard KI, Shepherd LE, O’Malley FP, Andrulis IL, Tu D, Bramwell VH, Levine MN (2006) HER2 and responsiveness of breast cancer to adjuvant chemotherapy. N Engl J Med 354(20):2103–2111
Colozza M, Bisagni G, Mosconi AM, Gori S, Boni C, Sabbatini R, Frassoldati A, Passalacqua R, Bian AR, Rodino C, Rondini E, Algeri R, Di Sarra S, De Angelis V, Cocconi G, Tonato M (2002) Epirubicin versus CMF as adjuvant therapy for stage I and II breast cancer: a prospective randomised study. Eur J Cancer 38(17):2279–2288
Fisher B, Brown AM, Dimitrov NV, Poisson R, Redmond C, Margolese RG, Bowman D, Wolmark N, Wickerham DL, Kardinal CG et al (1990) Two months of doxorubicin-cyclophosphamide with and without interval reinduction therapy compared with 6 months of cyclophosphamide, methotrexate, and fluorouracil in positive-node breast cancer patients with tamoxifen-nonresponsive tumors: results from the National Surgical Adjuvant Breast and Bowel Project B-15. J Clin Oncol 8(9):1483–1496
Fisher B, Redmond C, Wickerham DL, Bowman D, Schipper H, Wolmark N, Sass R, Fisher ER, Jochimsen P, Legault-Poisson S et al (1989) Doxorubicin-containing regimens for the treatment of stage II breast cancer: The National Surgical Adjuvant Breast and Bowel Project experience. J Clin Oncol 7(5):572–582
Dhesy-Thind B, Pritchard KI, Messersmith H, O’Malley F, Elavathil L, Trudeau M (2008) HER2/neu in systemic therapy for women with breast cancer: a systematic review. Breast Cancer Res Treat 109(2):209–229
Gennari A, Sormani MP, Pronzato P, Puntoni M, Colozza M, Pfeffer U, Bruzzi P (2008) HER2 status and efficacy of adjuvant anthracyclines in early breast cancer: a pooled analysis of randomized trials. J Natl Cancer Inst 100(1):14–20
Jarvinen TA, Tanner M, Rantanen V, Barlund M, Borg A, Grenman S, Isola J (2000) Amplification and deletion of topoisomerase IIalpha associate with ErbB-2 amplification and affect sensitivity to topoisomerase II inhibitor doxorubicin in breast cancer. Am J Pathol 156(3):839–847
Di Leo A, Gancberg D, Larsimont D, Tanner M, Jarvinen T, Rouas G, Dolci S, Leroy JY, Paesmans M, Isola J, Piccart MJ (2002) HER-2 amplification and topoisomerase IIalpha gene aberrations as predictive markers in node-positive breast cancer patients randomly treated either with an anthracycline-based therapy or with cyclophosphamide, methotrexate, and 5-fluorouracil. Clin Cancer Res 8(5):1107–1116
Durbecq V, Paesmans M, Cardoso F, Desmedt C, Di Leo A, Chan S, Friedrichs K, Pinter T, Van Belle S, Murray E, Bodrogi I, Walpole E, Lesperance B, Korec S, Crown J, Simmonds P, Perren TJ, Leroy JY, Rouas G, Sotiriou C, Piccart M, Larsimont D (2004) Topoisomerase-II alpha expression as a predictive marker in a population of advanced breast cancer patients randomly treated either with single-agent doxorubicin or single-agent docetaxel. Mol Cancer Ther 3(10):1207–1214
Knoop AS, Knudsen H, Balslev E, Rasmussen BB, Overgaard J, Nielsen KV, Schonau A, Gunnarsdottir K, Olsen KE, Mouridsen H, Ejlertsen B (2005) Retrospective analysis of topoisomerase IIa amplifications and deletions as predictive markers in primary breast cancer patients randomly assigned to cyclophosphamide, methotrexate, and fluorouracil or cyclophosphamide, epirubicin, and fluorouracil: Danish Breast Cancer Cooperative Group. J Clin Oncol 23(30):7483–7490
Tanner M, Isola J, Wiklund T, Erikstein B, Kellokumpu-Lehtinen P, Malmstrom P, Wilking N, Nilsson J, Bergh J (2006) Topoisomerase IIalpha gene amplification predicts favorable treatment response to tailored and dose-escalated anthracycline-based adjuvant chemotherapy in HER-2/neu-amplified breast cancer: Scandinavian Breast Group Trial 9401. J Clin Oncol 24(16):2428–2436
Slamon D, Eiermann W, Robert N, Pienkowski T, Martin M, Press M, Mackey J, Glaspy J, Chan A, Pawlicki M, Pinter T, Valero V, Liu MC, Sauter G, von Minckwitz G, Visco F, Bee V, Buyse M, Bendahmane B, Tabah-Fisch I, Lindsay MA, Riva A, Crown J (2011) Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med 365(14):1273–1283
Jarvinen TA, Tanner M, Barlund M, Borg A, Isola J (1999) Characterization of topoisomerase II alpha gene amplification and deletion in breast cancer. Genes Chromosomes Cancer 26(2):142–150
Pritchard KI (2009) Are HER2 and TOP2A useful as prognostic or predictive biomarkers for anthracycline-based adjuvant chemotherapy for breast cancer? J Clin Oncol 27(24):3875–3876
Desmedt C, Di Leo A, de Azambuja E, Larsimont D, Haibe-Kains B, Selleslags J, Delaloge S, Duhem C, Kains JP, Carly B, Maerevoet M, Vindevoghel A, Rouas G, Lallemand F, Durbecq V, Cardoso F, Salgado R, Rovere R, Bontempi G, Michiels S, Buyse M, Nogaret JM, Qi Y, Symmans F, Pusztai L, D’Hondt V, Piccart-Gebhart M, Sotiriou C (2011) Multifactorial approach to predicting resistance to anthracyclines. J Clin Oncol 29(12):1578–1586
Romero A, Caldes T, Diaz-Rubio E, Martin M (2012) Topoisomerase 2 alpha: a real predictor of anthracycline efficacy? Clin Transl Oncol 14(3):163–168
Di Leo A, Isola J (2003) Topoisomerase II alpha as a marker predicting the efficacy of anthracyclines in breast cancer: are we at the end of the beginning? Clin Breast Cancer 4(3):179–186
Hajduk M, Olszewski WP, Smietana A (2009) Evaluation of the predictive value of topoisomerase II alpha in patients with breast carcinoma. Pol J Pathol 60(3):115–123
Fountzilas G, Valavanis C, Kotoula V, Eleftheraki AG, Kalogeras KT, Tzaida O, Batistatou A, Kronenwett R, Wirtz RM, Bobos M, Timotheadou E, Soupos N, Pentheroudakis G, Gogas H, Vlachodimitropoulos D, Polychronidou G, Aravantinos G, Koutras A, Christodoulou C, Pectasides D, Arapantoni P (2012) HER2 and TOP2A in high-risk early breast cancer patients treated with adjuvant epirubicin-based dose-dense sequential chemotherapy. J Transl Med 10:10
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344:783–792
Konecny GE, Pauletti G, Untch M, Wang HJ, Mobus V, Kuhn W, Thomssen C, Harbeck N, Wang L, Apple S, Janicke F, Slamon DJ (2010) Association between HER2, TOP2A, and response to anthracycline-based preoperative chemotherapy in high-risk primary breast cancer. Breast Cancer Res Treat 120(2):481–489
Murphy DS, McHardy P, Coutts J, Mallon EA, George WD, Kaye SB, Brown R, Keith WN (1995) Interphase cytogenetic analysis of erbB2 and topoII alpha co-amplification in invasive breast cancer and polysomy of chromosome 17 in ductal carcinoma in situ. Int J Cancer 64(1):18–26
Pegram MD, Finn RS, Arzoo K, Beryt M, Pietras RJ, Slamon DJ (1997) The effect of HER-2/neu overexpression on chemotherapeutic drug sensitivity in human breast and ovarian cancer cells. Oncogene 15(5):537–547
Press MF, Sauter G, Buyse M, Bernstein L, Guzman R, Santiago A, Villalobos IE, Eiermann W, Pienkowski T, Martin M, Robert N, Crown J, Bee V, Taupin H, Flom KJ, Tabah-Fisch I, Pauletti G, Lindsay MA, Riva A, Slamon DJ (2012) Alteration of topoisomerase II-alpha gene in human breast cancer: association with responsiveness to anthracycline-based chemotherapy. J Clin Oncol 29(7):859–867
Konecny GE, Pauletti G, Untch M, Wang HJ, Mobus V, Kuhn W, Thomssen C, Harbeck N, Wang L, Apple S, Janicke F, Slamon DJ (2012) Association between HER2, TOP2A, and response to anthracycline-based preoperative chemotherapy in high-risk primary breast cancer. Breast Cancer Res Treat 120(2):481–489
Del Mastro L, Bruzzi P, Nicolo G, Cavazzini G, Contu A, D’Amico M, Lavarello A, Testore F, Castagneto B, Aitini E, Perdelli L, Bighin C, Rosso R, Venturini M (2005) HER2 expression and efficacy of dose-dense anthracycline-containing adjuvant chemotherapy in breast cancer patients. Br J Cancer 93(1):7–14
Muss HB, Thor AD, Berry DA, Kute T, Liu ET, Koerner F, Cirrincione CT, Budman DR, Wood WC, Barcos M et al (1994) c-erbB-2 expression and response to adjuvant therapy in women with node-positive early breast cancer. N Engl J Med 330(18):1260–1266
Thor AD, Berry DA, Budman DR, Muss HB, Kute T, Henderson IC, Barcos M, Cirrincione C, Edgerton S, Allred C, Norton L, Liu ET (1998) erbB-2, p53, and efficacy of adjuvant therapy in lymph node-positive breast cancer. J Natl Cancer Inst 90(18):1346–1360
Gianni L, Pienkowski T, Im YH, Roman L, Tseng LM, Liu MC, Lluch A, Staroslawska E, de la Haba-Rodriguez J, Im SA, Pedrini JL, Poirier B, Morandi P, Semiglazov V, Srimuninnimit V, Bianchi G, Szado T, Ratnayake J, Ross G, Valagussa P (2012) Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol 13(1):25–32
Acknowledgments
We thank the patients who participated in this study and their families. We are grateful to the doctors in the Department of Pathology for their technical assistance. National Natural Science Foundation of China (30972934); National Natural Science Foundation of China (81000991).
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, J., Xu, B., Yuan, P. et al. TOP2A amplification in breast cancer is a predictive marker of anthracycline-based neoadjuvant chemotherapy efficacy. Breast Cancer Res Treat 135, 531–537 (2012). https://doi.org/10.1007/s10549-012-2167-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2167-5