Abstract
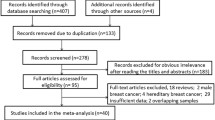
The purpose of this study is to investigate whether BRCA1 promoter methylation is associated with poorer outcome in sporadic breast cancer cases treated with tamoxifen. BRCA1 promoter methylation was determined by bisulfite pyrosequencing in two groups of sporadic breast cancer patients, systemically untreated (N = 497) and treated with adjuvant tamoxifen (N = 497). Associations of BRCA1 promoter methylation with clinopathological characteristics and the effect of BRCA1 promoter methylation on time to first recurrence (TTR) and overall survival (OS) were examined. No significant differences were observed between BRCA1 promoter methylation and clinopathological characteristics in untreated and tamoxifen-treated groups. Cut point analysis did not find any promising cut point for BRCA1 promoter methylation that would differentially influence TTR and OS in untreated and tamoxifen-treated group. Using the median (2.53 %) and an arbitrary value of 10 % as a cut point for methylation, we still found no significant effect of BRCA1 promoter methylation on TTR and OS in untreated and tamoxifen-treated group. Despite data suggesting that BRCA1 levels impact estrogen receptor response to tamoxifen, our results indicate that BRCA1 promoter methylation is not associated with poorer outcome in sporadic breast cancer cases treated with tamoxifen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer among women in the industrialized world. Although germline mutations in the BRCA1 gene are responsible for nearly half of the inherited breast cancer cases [1], there is very little evidence for BRCA1 mutations in the sporadic form of the disease. Despite the lack of BRCA1 somatic mutations, significantly reduced BRCA1 expression has been observed in 30–40 % of sporadic breast cancer cases [2, 3]. Several mechanisms presumably cooperate to mediate BRCA1 somatic inactivation with BRCA1 promoter methylation being the most widely examined and present in 9–59 % of sporadic breast cancer cases [4–10].
BRCA1 encodes a multifunctional protein with roles in many important cellular functions, including DNA repair, cell cycle control, protein ubiquitination, and transcriptional regulation [11]. Loss of these caretaker functions may explain why BRCA1 inactivation predisposes to the development of cancer; however, it does not explain the strong predilection to specific tumor types, particularly breast and other hormone-responsive tumors. It has therefore been hypothesized that BRCA1 may participate in sex steroid hormone activity. Indeed, prophylactic bilateral salpingo-oophorectomy has been shown to significantly reduce the rate of breast cancer in BRCA1 mutation carriers by 47 % [12].
Paradoxically, the majority of breast cancers developed in BRCA1 mutation carriers are estrogen receptor (ER) negative [13, 14]. Hosey and colleagues have suggested that BRCA1 mutant tumors fail to express ER due to the loss of BRCA1-mediated transcriptional activation of ER and propose a model in which the observed loss of ER expression in BRCA1 mutation carriers occurs only after the loss of the second BRCA1 allele [15, 16]. Animal studies have supported this possibility by showing that ER is highly expressed in premalignant lesions and initiation stages of tumorigenesis, and that its expression gradually declines during mammary tumor progression in BRCA1 mutant mice [17, 18]. Therefore, it is plausible that hormone deprivation could be preventive in BRCA1 mutation carriers if initiated at early stages of tumor development. In agreement, the impact of prophylactic bilateral salpingo-oophorectomy on the subsequent risk of contralateral breast cancer was shown to be more effective if performed at a younger age [19].
Confirming a link between BRCA1 levels and steroid hormone signaling in promoting mammary carcinogenesis, Lee and colleagues [20] demonstrated that mammary tumors in BRCA1 mutant mice could be prevented by the administration of progesterone antagonist mifepristone. In an analogous attempt to prevent mammary cancer initiation in BRCA1 mutant mice, Jones and colleagues found that tamoxifen paradoxically promoted the development of mammary tumors. In vitro experiments revealed that BRCA1 knockdown in breast cancer cells induced the agonist activity of tamoxifen [21]. Interestingly, in a re-analysis of the National Surgical Adjuvant Breast and Bowel Project (NSABP-P1) by BRCA status, the authors found that tamoxifen use was associated with an increased incidence of breast cancer with a hazard ratio of 1.67 among BRCA1 mutation carriers, whereas the incidence of breast cancer was decreased by 62 % in BRCA2 mutation carriers and by 48 % in the study population as a whole [22]. In addition, Beiner and colleagues found an elevated risk for endometrial cancer among BRCA1 mutation carriers who were treated with tamoxifen compared to non-carriers [23, 24]. Consistent with a possible enhanced agonistic role for tamoxifen in the presence of low levels of BRCA1, Wen and colleagues demonstrated that decreased BRCA1 expression in breast cancer cells contributed to tamoxifen resistance due to altered ER-coregulator interactions; tamoxifen-bound ER-regulated gene promoters did not associate with corepressors, but instead inappropriately recruited coactivators [25]. Overall, these observations suggest that cellular levels of BRCA1 not only play a role in breast cancer development but might also predict response to tamoxifen therapy.
The purpose of the current study was therefore to examine whether BRCA1 promoter methylation, a mechanism of BRCA1 down-regulation, is associated with poorer outcome in sporadic breast cancer cases treated with tamoxifen. To achieve this objective, we carried out a retrospective study to evaluate the association of BRCA1 promoter methylation with time to first recurrence (TTR) and overall survival (OS) in two cohorts of sporadic breast cancer patients, systemically untreated and treated with adjuvant tamoxifen. We further aimed to investigate the associations of BRCA1 promoter methylation with clinopathological characteristics.
Methods
Study population
Subjects presented in this study were diagnosed and treated between 1970 and 1999, and derived from two tumor banks (P01 and SPORE) with associated clinical annotations and long-term follow-up. These banks were constructed and maintained by the Smith Breast Center at Baylor College of Medicine, as previously described [26]. Briefly, the banks comprise 497 tumors from patients who did not receive adjuvant therapy after surgery (untreated) and 497 tumors from patients treated with tamoxifen (tamoxifen-treated). Additional selection criteria included: complete information about patient and tumor characteristics; early stage breast cancer; ER positivity by ligand-binding assay (≥3 fml/mg protein), no neoadjuvant therapy; no adjuvant chemotherapy; and sufficient tumor material for DNA extraction. A total of 213 samples came from the P01 and 787 from the SPORE banks. OS data were equally reliably obtained from both banks. Follow-up of P01 cases was obtained directly from treating physicians and recurrence information is quite complete. Follow-up of SPORE cases was obtained from hospital tumor registries and recurrence is somewhat under-reported. There is no evidence that the under-reporting is associated with prognostic or predictive variables of interest.
The study protocol was approved by the Institutional Review Board of the Baylor College of Medicine with a waiver of consent.
Methylation analysis
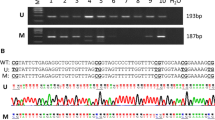
The pattern of CpG methylation within the promoter region of BRCA1 was quantified by bisulfite pyrosequencing as previously described [27]. The pyrosequencing assay assessed five adjacent CpG sites. These are located at −55, −37, −29, −21, and −19 relative to the BRCA1 transcription start site +1 (Fig. 1).
Schematic representation of the BRCA1 and NBR2 bidirectional core promoter. Legend: CpG dinucleotides are in upper case letters. CpG dinucleotides analyzed in the present study are in bold and underlined, located at −55, −37, −29, −21 and −19. The underlined ‘a’ indicates the BRCA1 transcriptional start site (+1). The underlined ‘t’ indicates the NBR2 transcriptional start site (+1). Gray boxes represent CREB, MyoD, c-Myb and E2F transcription factor binding sites, which are potentially regulated by methylation at −173, −29, −29 and −21 to −19, respectively. The arrow indicates the position of the pyrosequencing primer used in the present study
Briefly, genomic DNA was extracted from frozen tumor tissues using the Puregene DNA Purification Kit (Qiagen) and subjected to bisulfite conversion using EZ DNA Methylation Gold Kit (Zymo Research). Bisulfite-modified DNA was amplified in a two-step PCR. First PCR reaction (20 μl) included bisulfite-treated genomic DNA, 1 unit of Taq DNA Polymerase, 67 mmol/L Tris–HCl (pH = 8), 16 mmol/L ammonium sulfate, 2 mmol/L MgCl2, 0.125 mmol/L dNTPs, forward primer 5′-GGT GGT TAA TTT AGA GTT TAG AGA GA-3′ and reverse primer 5′-AAA ACT CCT AAC CTC ATA ACC AAC C-3′, each at 100 nmol/L. PCR conditions were as follows; initial denaturation at 95 °C for 5 min, followed by 38 cycles at 94 °C for 30 s, 62 °C for 45 s, 72 °C for 50 s, and a final extension at 72 °C for 10 min. The PCR product from the first PCR step was used as template to perform a second PCR step with forward primer 5′-TGA TTT AGT ATT TTG AGA GGT TGT TGT TTA -3′ and biotinylated reverse primer 5′-GGG ACA CCG CTG ATC GTT TAC AAT CCC AAT TTT AAT TTA TCT ATA ATT CCC-3′, which yielded a final 119-bp amplicon. PCR components and conditions for the second PCR reaction were as described before except that the annealing temperature was increased to 63 °C and 45 cycles were performed to completely exhaust the biotinylated primer. Biotin-labeled single-stranded templates were isolated and pyrosequencing reactions were run on PSQ HS 96 Pyrosequencing System (Biotage) with a specific pyrosequencing primer 5′-TTG AGA GGT TGT TGT TTA G-3′ and Pyro Gold CDT Reagents (Biotage).
Duplicate measurements were carried out for each sample. The pyrosequencing assay failed completely in two (0.2 %) samples due to poor DNA quality. For the CpG1, CpG2, CpG3, CpG4, and CpG5, the pyrosequencing assay failed in one of the two replicates in 30 (3.0 %), 40 (4.0 %), 67 (6.7 %), 111 (11.2 %), and 160 (16.1 %) samples, respectively. 95 % of samples had a difference between replicates of less than 15 % for all five CpG sites analyzed.
Statistical analysis
We found highly concordant methylation patterns between adjacent CpG positions (pairwise Spearman’s correlation coefficients ranged from 0.22 to 0.55, p < 0.001). In view of the redundancy of the sites, we constructed a single measure of methylation using the maximum of the duplicates and averaging the five sites.
Descriptive and summary statistics were used to describe patient and tumor characteristics. Associations between clinopathological characteristics and adjuvant therapy (untreated vs. tamoxifen-treated) and associations between clinopathological characteristics and BRCA1 promoter methylation (<median vs. >median) in untreated and tamoxifen-treated group were evaluated by χ2 test and Spearman’s rank correlation. Outcomes were TTR, defined as time from diagnosis to first recurrence or last follow-up whichever was first and censoring at death, and OS, defined as time from diagnosis to death or last follow-up. The effects of BRCA1 promoter methylation on TTR and OS were summarized by the Kaplan–Meier method and compared by log-rank test. Survival analyses were performed for untreated and tamoxifen-treated group and for each bank separately, as well as in combination by stratifying on bank. Cut points for methylation in the analyses were the median (2.53 %) and an arbitrary value of 10 %. To find an optimal dichotomous cut point, the functional form of continuous methylation was evaluated by means of Martingale residuals. In addition, a data-driven cut point in methylation percentage for both endpoints was identified by the method of Hilsenbeck and Clark [28].
A p value <0.05 was considered to indicate statistical significance. Statistical analyses were done using SAS 9.2 (SAS institute Inc., Cary, NC) and R 2.14.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 994 sporadic breast cancer patients were included in the present study. The first group consisted of 497 systemically untreated patients who underwent breast cancer surgery or surgery plus local radiation (untreated group). The second group comprised 497 patients who, in addition to breast cancer surgery ± local radiation, received adjuvant tamoxifen treatment (tamoxifen-treated group). Median follow-up time for patients alive at last follow-up was 123 months (range, 0–253 months), for untreated patients was 124 months (range, 0–253 months), and for tamoxifen-treated patients was 122 months (range, 1–225 months).
Clinopathological characteristics for the untreated and tamoxifen-treated groups are summarized in Table 1. More cases in the untreated group were derived from the SPORE bank. Cases in the untreated group were slightly younger (p < 0.001), had smaller tumors (p < 0.001), fewer positive nodes (p < 0.001), and were more likely to be diploid (p = 0.036), as be expected for cases not thought to need additional therapy. No differences were observed between the two groups with respect to other characteristics, including histological type, PR status, and S-phase fraction (p > 0.05).
The overall distribution of BRCA1 promoter methylation values for both groups is illustrated in Fig. 2. The first quartile, the median, and the third quartile were 1.72, 2.53, and 3.90 %, respectively, and 9.7 % of patients had BRCA1 promoter methylation of ≥10 %. Clinopathological characteristics according to BRCA1 promoter methylation (<median vs. >median) in untreated and tamoxifen-treated group are shown in Table 2. The small number of untreated cases derived from P01 bank tended to have lower methylation than SPORE cases (p < 0.001). No other differences were observed between BRCA1 promoter methylation and clinopathological characteristics, including age, histological type, tumor size, nodal status, PR status, ploidy, and S-phase fraction in untreated and tamoxifen-treated group (p > 0.05).
Using the median (2.53 %) and an arbitrary value of 10 % as a cut point for methylation, we found no significant effect of BRCA1 promoter methylation on TTR (Fig. 3—presented for each bank separately) and OS (data not shown) in untreated and tamoxifen-treated group. Similarly, cut point analysis, which included adjustment for multiple comparisons, did not find any promising cut point for BRCA1 promoter methylation that would differentially influence TTR or OS in untreated or tamoxifen-treated group (Table 3). A retrospective power analysis indicated that, at the 5 % level of significance, the study had 80 % power to detected hazard ratios of at least 1.76 and 1.92 in TTR for the treated and untreated group, respectively; 1.49 and 1.53 in OS for the treated and untreated group, respectively.
Discussion
In the breast, tamoxifen acts as an ER antagonist and its widespread use has significantly improved OS in women with ER-positive breast cancer [29]. Despite the obvious benefits, 30–50 % of women develop drug resistance in which either they do not respond to tamoxifen at all (intrinsic resistance) or they do initially respond but eventually relapse (acquired resistance) [30]. In order to better predict therapeutic responses to tamoxifen treatment, further improvements in understanding the mechanisms underlying tamoxifen resistance are thus of great importance. Given the recent findings of potential implications of BRCA1 function in tamoxifen resistance, we sought to evaluate the role of BRCA1 promoter methylation in predicting tamoxifen sensitivity in sporadic breast cancer patients.
The expression of BRCA1 gene is under complex regulation [31, 32]. BRCA1’s 5′ neighbor gene NBR2 lies in a head-to-head orientation with the BRCA1 gene, and both share the same bidirectional promoter (−218 to +1, relative to the BRCA1 transcription start site; Fig. 1). This essential regulatory region is part of a large, 2.7-kb long, CpG island and spans 11 CpG sites, which have been shown to be unmethylated in normal human mammary epithelial cells [4–8]. On the other hand, methylation of the same region was found to be a fairly frequent event in sporadic breast cancer cases with frequencies ranging from 9 to 59 % with most studies using 10 % of cells methylated as a cutoff for methylation if a quantitative method was applied [9, 10]. In our study, 9.7 % of patients had BRCA1 promoter methylation of ≥10 %. Large discrepancies in the reported frequency of BRCA1 promoter methylation across studies might be explained by potential infiltration with the unmethylated DNA from normal cells adjacent to the tumor, by the variable extent of BRCA1 regulatory region covered, which might lead to erroneously including the methylation signature related to the neighboring NBR2 gene and by different experimental methods employed. Most of the previous studies used methylation-specific PCR or restriction enzyme digestion as a method to detect BRCA1 promoter methylation, which, unlike pyrosequencing, are known to be prone to false positive results. Assay failure is another potential consideration in our study. However, since 95 % of the samples had the difference between the both replicates of less than 15 % for all five CpG sites analyzed and the higher percent of methylation from the two replicates was used in the analyses, the impact of the potential additional assay failure could not have been substantial.
The possibility of using epigenetic alteration as a surrogate marker to predict adjuvant tamoxifen efficacy was demonstrated by Fiegl and colleagues [33]. They showed that methylated RASSF1A in serum of breast cancer patients correlated with tamoxifen resistance, whereas loss of methylation portended a good response [33]. In order to explore if BRCA1 promoter methylation may serve as a potential additional biomarker to identify patients most likely to respond to adjuvant tamoxifen therapy, a pyrosequencing assay was developed to examine the methylation pattern of the BRCA1 promoter region directly upstream of the BRCA1 transcriptional start site, which encompasses MyoD, c-myc, and E2F transcription factor binding sites and was previously suggested to be a region of methylation initiation (Fig. 1) [34]. Since BRCA1 promoter methylation has been consistently observed to contribute to the BRCA1 gene silencing [3, 35, 36], we reasoned that, by reducing accessibility of transcription factors, the methylation of this particular region might have a considerable impact on repression of BRCA1 gene expression [34, 37, 38]. Nevertheless, no significant effect of BRCA1 promoter methylation on TTR and OS was found in either untreated or tamoxifen-treated patients. Owing to the minor differences between the P01 and SPORE bank in sampling and data collection and differences in the proportion of cases derived from each bank in the two treatment groups and somewhat lower methylation rate in untreated P01 cases, we performed stratified analyses and also analyzed each bank separately. By means of several methods, none of the approaches were able to find a promising cut point for BRCA1 promoter methylation that would differentially influence TTR and OS in the untreated and tamoxifen-treated groups. Our attempts to define a clinically meaningful data-driven cut point were similarly unsuccessful. There were some statistically significant cut points identified with the cut point analysis (p < 0.05); however, these were mostly at methylation values of less than 1 %, and consequently, only 0.6–3.4 % of cases ended up being potentially good responders. Furthermore, their significance was not distributed more widely around the proposed value, which would provide a better indication that this might indeed be an area of interest. Although our study may be biased by the retrospective design and lack of data on corresponding BRCA1 gene expression, we had a large community-based cohort of sporadic breast cancer patients and used a highly accurate method for detection and quantitation of DNA methylation. Retrospective power analysis indicated that we had excellent power to detect clinically meaningful difference.
In conclusion, our results suggest that BRCA1 promoter methylation is not associated with poorer outcome in sporadic breast cancer cases treated with tamoxifen.
Abbreviations
- ER:
-
Estrogen receptor
- OS:
-
Overall survival
- TTR:
-
Time to first recurrence
References
Narod SA, Foulkes WD (2004) BRCA1 and BRCA2: 1994 and beyond. Nat Rev Cancer 4:665–676
Thompson ME, Jensen RA, Obermiller PS, Page DL, Holt JT (1995) Decreased expression of BRCA1 accelerates growth and is often present during sporadic breast cancer progression. Nat Genet 9:444–450
Mueller CR, Roskelley CD (2003) Regulation of BRCA1 expression and its relationship to sporadic breast cancer. Breast Cancer Res 5:45–52
Dobrovic A, Simpfendorfer D (1997) Methylation of the BRCA1 gene in sporadic breast cancer. Cancer Res 57:3347–3350
Mancini DN, Rodenhiser DI, Ainsworth PJ, O’Malley FP, Singh SM, Xing W et al (1998) CpG methylation within the 5’ regulatory region of the BRCA1 gene is tumor specific and includes a putative CREB binding site. Oncogene 16:1161–1169
Rice JC, Massey-Brown KS, Futscher BW (1998) Aberrant methylation of the BRCA1 CpG island promoter is associated with decreased BRCA1 mRNA in sporadic breast cancer cells. Oncogene 17:1807–1812
Esteller M, Silva JM, Dominguez G, Bonilla F, Matias-Guiu X, Lerma E et al (2000) Promoter hypermethylation and BRCA1 inactivation in sporadic breast and ovarian tumors. J Natl Cancer Inst 92:564–569
Rice JC, Ozcelik H, Maxeiner P, Andrulis I, Futscher BW (2000) Methylation of the BRCA1 promoter is associated with decreased BRCA1 mRNA levels in clinical breast cancer specimens. Carcinogenesis 21:1761–1765
Birgisdottir V, Stefansson OA, Bodvarsdottir SK, Hilmarsdottir H, Jonasson JG, Eyfjord JE (2006) Epigenetic silencing and deletion of the BRCA1 gene in sporadic breast cancer. Breast Cancer Res 8:R38
Xu X, Gammon MD, Zhang Y, Bestor TH, Zeisel SH, Wetmur JG et al (2009) BRCA1 promoter methylation is associated with increased mortality among women with breast cancer. Breast Cancer Res Treat 115:397–404
Rosen EM, Fan S, Pestell RG, Goldberg ID (2003) BRCA1 gene in breast cancer. J Cell Physiol 196:19–41
Rebbeck TR, Levin AM, Eisen A, Synder C, Watson P, Cannon-Albright L et al (1999) Breast cancer risk after bilateral prophylactic oophorectomy in BRCA1 mutation carriers. J Natl Cancer Inst 91:1475–1479
Armes JE, Trute L, White D, Southey MC, Hammet F, Tesoriero A et al (1999) Distinct molecular pathogeneses of early-onset breast cancers in BRCA1 and BRCA2 mutation carriers: a population-based study. Cancer Res 59:2011–2017
Lakhani SR, Van De Vijever MJ, Jacquemier J, Anderson TJ, Osin PP, McGuffog L et al (2002) The pathology of familial breast cancer: predictive value of immunohistochemical markers estrogen receptor, progesterone receptor, HER-2, and p53 in patients with mutations in BRCA1 and BRCA2. J Clin Oncol 20:2310–2318
Hosey AM, Gorski JJ, Murray MM, Quinn JE, Chung WY, Stewart GE et al (2007) Molecular basis for estrogen receptor α deficiency in BRCA1-linked breast cancer. J Natl Cancer Inst 99:1683–1694
Gorski JJ, Kennedy RD, Hosey AM, Harkin DP (2009) The complex relationship between BRCA1 and Erα in hereditary breast cancer. Clin Cancer Res 15:1514–1518
Li W, Xiao C, Vonderhaar BK, Deng CX (2007) A role of estrogen/ERα signaling in BRCA1-associated tissue-specific tumor formation. Oncogene 26:7204–7212
Jones LP, Tilli MT, Assefnia S, Torre K, Halama ED, Parrish A et al (2008) Activation of estrogen signaling pathways collaborates with loss of BRCA1 to promote development of ERα-negative and ERα-positive mammary preneoplasia and cancer. Oncogene 27:794–802
Metcalfe K, Lynch HT, Ghadirian P, Tung N, Olivotto I, Warner E et al (2004) Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol 22:2328–2335
Poole AJ, Li Y, Kim Y, Lin SC, Lee WH, Lee EY (2006) Prevention of BRCA1-mediated mammary tumorigenesis in mice by a progesterone antagonist. Science 314:1467–1470
Jones LP, Li M, Halama ED, Ma Y, Lubet R, Grubbs CJ et al (2005) Promotion of mammary cancer development by tamoxifen in a mouse model of BRCA1-mutation-related breast cancer. Oncogene 24:3554–3562
King MC, Wieand S, Hale K, Lee M, Walsh T, Owens K et al (2001) Tamoxifen and breast cancer incidence among women with inherited mutations in BRCA1 and BRCA2. JAMA 286:2251–2256
Beiner ME, Finch A, Rosen B, Lubinski J, Moller P, Ghadirian P et al (2007) The risk of endometrial cancer in women with BRCA1 and BRCA2 mutations. A prospective study. Gynecol Oncol 104:7–10
Lu KH, Kauff ND (2007) Does a BRCA mutation plus tamoxifen equal hysterectomy? Gynecol Oncol 104:3–4
Wen J, Li R, Lu Y, Shupnik MA (2009) Decreased BRCA1 confers tamoxifen resistance in breast cancer cells by altering estrogen receptor-coregulator interactions. Oncogene 28:575–586
Pathiraja TN, Shetty PB, Jelinek J, He R, Hartmaier R, Margossian AL et al (2011) Progesterone receptor isoform-specific promoter methylation: association of PRA promoter methylation with worse outcome in breast cancer patients. Clin Cancer Res 17:4177–4186
Colella S, Shen L, Baggerly KA, Issa JP, Krahe R (2003) Sensitive and quantitative universal pyrosequencing methylation analysis of CpG sites. Biotechniques 35:146–150
Hilsenbeck SG, Clark GM (1996) Practical p-value adjustment for optimally selected cutpoints. Stat Med 15:103–112
Fisher B, Costantino J, Redmond C, Poisson R, Bowman D, Couture J et al (1989) A randomized clinical trial evaluating tamoxifen in the treatment of patients with node-negative breast cancer who have estroge-receptor-positive tumors. N Engl J Med 320:479–484
Clarke R, Liu MC, Bouker KB, Gu Z, Lee RY, Zhu Y et al (2003) Antiestrogen resistance in breast cancer and the role of estrogen receptor signaling. Oncogene 22:7316–7339
Xu CF, Chambers JA, Solomon E (1997) Complex regulation of the BRCA1 gene. J Biol Chem 272:20994–20997
Thakur S, Croce CM (1999) Positive regulation of the BRCA1 promoter. J Biol Chem 274:8837–8843
Fiegl H, Millinger S, Mueller-Holzner E, Marth C, Ensinger C, Berger A et al (2005) Circulating tumor-specific DNA: a marker for monitoring efficacy of adjuvant therapy in cancer patients. Cancer Res 65:1141–1145
Wilcox CB, Baysal BE, Gallion HH, Strange MA, DeLoia JA (2005) High-resolution methylation analysis of the BRCA1 promoter in ovarian tumors. Cancer Genet Cytogenet 159:114–122
Catteau A, Morris JR (2002) BRCA1 methylation: a significant role in tumor development? Semin Cancer Biol 12:359–371
Wei M, Grushko TA, Dignam J, Hagos F, Nanda R, Sveen L et al (2005) BRCA1 promoter methylation in sporadic breast cancer is associated with reduced BRCA1 copy number and chromosome 17 aneusomy. Cancer Res 65:10692–10699
Jin W, Liu Y, Chen L, Zhu H, Di GH, Ling H et al (2011) Involvement of MyoD and c-myb in regulation of basal and estrogen-induced transcriptional activity of the BRCA1 gene. Breast Cancer Res Treat 125:699–713
Xu J, Huo D, Chen Y, Nwachukwu C, Collins C, Rowell et al (2010) CpG methylation affects accessibility of the proximal BRCA1 promoter to transcription factors. Breast Cancer Res Treat 120:593–601
Acknowledgments
We thank Rong He for helping with bisulfite pyrosequencing. The study was partially supported by SPORE P50 CA58183 and CCSG P30 CA125123 grants.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cerne, J.Z., Zong, L., Jelinek, J. et al. BRCA1 promoter methylation status does not predict response to tamoxifen in sporadic breast cancer patients. Breast Cancer Res Treat 135, 135–143 (2012). https://doi.org/10.1007/s10549-012-2117-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2117-2