Abstract
Patients with locally advanced breast cancer treated with neoadjuvant chemotherapy are at risk of cancer treatment–induced bone loss and consequently of increased skeletal morbidity. In addition, this situation could be worsened by the fact that only a minority of patients with breast cancer have sufficient vitamin D. A comprehensive evaluation of bone homeostasis is critical in this context. We retrospectively evaluated the serum levels of calcium, vitamin D, TRAIL, RANK ligand (RANKL), Osteoprotegerin (OPG), Bone TRAP, CrossLaps and DKK1 in 77 patients (median age: 50 years; range 25–74), with locally advanced breast cancer treated in our institute with anthracyclines-taxane neoadjuvant chemotherapy (7 cycles of 21 days/each) between March 2007 and August 2008. Serum samples were collected before the first (baseline) and the last treatment cycle. Variations and correlations between biomarker levels were evaluated. At baseline, 79.5 % of patients had vitamin D insufficiency (<30 ng/ml), increasing to 97.4 % at the end of the neoadjuvant chemotherapy (p < 0.0001). Calcium and RANKL serum concentrations were also significantly decreased, while OPG was significantly increased, resulting in lower RANKL/OPG ratio. Calcium and vitamin D, RANKL and vitamin D and RANKL and OPG levels were significantly correlated (Spearman’s coefficient r = 0.2721, p = 0.0006; r = 0.1916, p = 0.002; and r = −0.179, p = 0.03, respectively). Nearly all included patients suffered from vitamin D insufficiency by the end of the neoadjuvant chemotherapy with changes in the calcium/RANKL/OPG axis that are evocative of deregulation of a functional regulatory mechanism. Further studies are needed to determine how drugs modulate this regulatory mechanism to preserve bone homeostasis in patients with breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with early stage or locally advanced breast cancer are often treated with chemotherapy and anti-hormonal therapy [1]. Such therapies can lead to cancer treatment–induced bone loss [2], because of premature ovarian failure or direct cytotoxic effects of the chemotherapy that cause bone mineral density reduction and increase of skeletal morbidity risk compared with women without breast cancer history [2–6]. Furthermore, only a minority of patients with early breast cancer have sufficient vitamin D levels [7]. Understanding the multiple factors underlying cancer treatment–induced bone loss is critical for bone risk assessment and to guide screening and early therapeutic interventions.
Vitamin D is a fat-soluble vitamin that regulates calcium and bone homeostasis. Vitamin D3 (cholecalciferol) is mainly synthesized by the skin from 7-dehydrocholesterol on ultraviolet B exposure. Vitamin D is carried in blood by the vitamin D binding protein, the polymorphism of which may influence the circulating level of 25-hydroxy vitamin D (25OHD) [8], to the liver where it is hydroxylated on carbon 25 to form 25OHD. In the renal proximal tubule cells, circulating 25OHD is hydroxylated by 1-alpha hydroxylase to form the active metabolite 1,25 dihydroxy vitamin D (1,25(OH)D2, calcitriol). Renal hydroxylation is strictly regulated and is stimulated primarily by circulating parathormone or low dietary calcium and inhibited by FGF-23 and low phosphorus level [9]. The best known role of 1,25(OH)D2 is the maintenance of the phosphorus–calcium homeostasis by increasing their intestinal absorption.
Severe vitamin D insufficiency can lead to defective bone mineralization, rickets in children and osteomalacia in adults. In less severe insufficiencies, the decrease in intestinal calcium absorption and the subsequent hypocalcemia increase serum parathormone level that stimulates bone remodeling and contributes to osteoporosis in elderly patients. Several interventional studies to evaluate the effect of vitamin D supplementation on fracture risk reduction in elderly populations found that high vitamin D doses (>700−800 IU/day) were associated with significant reduction of fracture risk [10, 11], improvement of muscle performance and relative reduction of the fall risk (partly explaining the reduced risk of peripheral fractures) [12].
Besides the bone complications [13, 14], many observational studies showed associations between insufficient vitamin D levels and cancer risk; however, the impact of vitamin D supplementation on cancer prevention remains controversial [15, 16]. Many data support the hypothesis that vitamin D might have anti-cancer activity in breast cancer. Indeed, breast cells contain all the components of the vitamin D signaling pathway, and pre-clinical studies have demonstrated that vitamin D has a protective effect against breast cancer development through several mechanisms, such as cell-cycle arrest (stimulation of Cyclin-dependent kinase inhibitors [17, 18]), anti-inflammatory activity (inhibition of COX 2 expression [19]) and inhibition of the estrogen pathway (anti-aromatase and anti-estrogen receptor alpha activity [20]). In epidemiological studies, exposure to sunlight was inversely correlated with breast cancer incidence and mortality. Furthermore, in white women, breast cancer death rates increased with the distance from the equator [21]. Recently, Song Yao et al. reported that women of African ancestry had more frequently severe vitamin D deficiency than women of European ancestry. This deficit was associated with ER-negative breast cancer, but this correlation became non-significant after adjusting for SNPs of CYP24A1, a gene involved in vitamin D metabolism. According to these results, low level of vitamin D or specific genetic variants in the vitamin D pathway may be associated with more aggressive breast cancer disease [22]. Among the six studies that analyzed the link between vitamin D intake and breast cancer risk [23], only three found an inverse association between vitamin D intake and risk of breast cancer development. However, the more robust of these studies show a decreased risk of breast cancer particularly in pre-menopausal women with higher vitamin D intake [24, 25]. Most of the works (including two prospective studies) on vitamin D status and breast cancer risk [26–35] found a statistically significant correlation between low level of vitamin D and increased risk of breast cancer. In the study by Goodwin et al. [7], women with very low levels of vitamin D presented worse distant disease-free survival. Vitamin D insufficiency may also contribute to the musculoskeletal pain induced by aromatase inhibitors [36] because of its role in the estrogen-related pathway. Finally, all those data are strongly consistent with a new concept of breast cancer etiology in which the contribution of vitamin D-dependent pathways must be taken into account.
Circulating 25OHD is considered the best indicator of vitamin D body stores, providing an integrated measure of all vitamin D sources [37–39]. A minimum target 25OHD blood level of 30 ng/mL (75 nmol/L) is generally recommended. Below this value, patients suffer of mild (29–20 ng/mL), moderate (19–10 ng/mL) or severe vitamin D insufficiency (or vitamin D deficiency, less than 10 ng/mL). Vitamin D insufficiency is widespread in Western societies, and it affects about 50 % of women and even more patients with breast cancer [7, 33, 40]. This insufficiency worsens the multifactorial bone metabolism alterations observed in such patients, increasing the osteoporosis risk [41], particularly in women with early breast cancer [7, 33, 40].
Adult bone is in constant flux between resorption of old or damaged bone by osteoclasts and formation of new bone by osteoblasts. The net balance between bone resorption and formation ultimately defines the bone mass variations. Biochemical markers of bone turnover can be measured in blood and/or urine, allowing a comprehensive assessment of this process. Dickkopf 1 (DKK1) serum level is used to evaluate osteoblast bone-forming activity. DKK1, a soluble inhibitor of the canonical Wingless (Wnt) signaling pathway, blocks the terminal differentiation of osteoblasts and decreases the viability of osteoblast stem cells, resulting in inhibition of osteogenesis [42]. Elevated serum DKK1 levels are associated with osteolytic bone lesions in patients with multiple myeloma [43] and with bone metastases in patients with breast cancer [44].
During bone resorption, activated osteoclasts attach to the bone surface and digest bone type I collagen, releasing calcium, phosphorus, cytokines and growth factors present within the bone matrix [45, 46]. Bone resorption markers include collagen degradation products and type I collagen telopeptides (N- and C-terminal cross-linked telopeptides: NTX or PINP, CTX or CrossLaps) measurable in serum or urine. CrossLaps and PINP are secreted after cleavage of type I collagen by osteoclasts and their serum concentration is related with bone remodeling. High serum CrossLaps and PINP concentrations have been associated with highly aggressive metastatic behavior of breast cancer [47].
The serum tartrate-resistant acid phosphatase (or Bone TRAP) [48], a 35–37 kDa glycoprotein that is highly expressed in osteoclasts, alveolar macrophages and dendritic cells, is a marker of bone resorption and its blood concentration could be related with bone remodeling. Elevated TRAP serum levels have been detected in post-menopausal women without hormone replacement therapy, Paget’s disease of bone, primary hyperparathyroidism, bone metastases and multiple myeloma.
RANK Ligand (RANKL), the receptor activator of nuclear factor (NF)-κB ligand also known as osteoprotegerin ligand (OPGL), is a member of the tumor necrosis factor (TNF) superfamily. The soluble form arises by proteolytic processing of membrane RANKL. RANKL is the major stimulatory factor for the formation and survival of mature osteoclasts. 1,25(OH)D2 stimulates the production of RANKL by osteoblasts. Increased RANKL expression leads to bone resorption and bone loss [49]. Furthermore, preclinical data suggest the implication of RANKL in breast tumorigenesis and metastasis formation [50].
Osteoprotegerin (OPG), a secreted glycoprotein belonging to the TNF receptor superfamily, acts as a decoy soluble receptor and hinders binding of RANK to RANKL, leading to inhibition of osteoclast recruitment, proliferation and activation. The RANKL/RANK/OPG system is, thus, the key molecular regulation system of bone remodeling. Imbalances of this system have been related to the pathogenesis of Paget’s disease of bone, benign and malignant bone tumors, post-menopausal osteoporosis and bone metastases [51–53]. The elevation of the RANKL/OPG ratio has been associated with the establishment of de novo bone metastases and the progression of skeletal tumors [50, 54].
TNF-related apoptosis-inducing ligand (TRAIL), a transmembrane protein that can also exist in a soluble form, belongs to the TNF superfamily. Both cell surface and soluble TRAIL induce apoptosis through binding to the TRAIL receptors 1 and 2. TRAIL also binds to its decoy receptors TRAIL R3, TRAIL R4 and OPG [55]. TRAIL may play an important role in bone resorption directly or through OPG [56].
Although bone metabolism in patients with breast cancer is the focus of much interest, a comprehensive evaluation of the variations of the mineral metabolism profile in patients with early or locally advanced breast cancer treated by chemotherapy is lacking. This study was thus undertaken to determine the prevalence of vitamin D insufficiency before (baseline) and after neoadjuvant chemotherapy in a population of 77 women with locally advanced breast cancer. Concomitantly, bone metabolism was comprehensively evaluated by measuring the serum levels of 25OHD, calcium, CrossLaps, Bone TRAP, TRAIL, DKK-1, soluble RANKL (sRANKL) and OPG at baseline and after neoadjuvant chemotherapy.
Patients and methods
Patients
From March 2007 to August 2008, 77 patients with a first history of histologically proven locally advanced breast cancer and biobank-stored serum samples were treated in our institute with a neoadjuvant chemotherapy regimen consisting of three FEC-100 cycles (5-fluorouracile, epirubicin and cyclophosphamide) and then four cycles of 100 mg/m² docetaxel every 21 days (total treatment duration for any given patient: 21 weeks). Patients with HER-2 overexpressing tumors received also trastuzumab injections, beginning at the first docetaxel cycle. Breast surgery with axillary lymphadenectomy was performed 4–6 weeks after the last treatment. The pathological response, to identify the patients with pathological complete response, was evaluated using the Sataloff classification [57]. Patients with known comorbid conditions that might affect the vitamin D–calcium metabolism were not included in this study. Ethical approval was provided by the local research ethics committee.
Collection and storage of serum samples
Serum samples for tumor markers determination were collected using standard phlebotomy procedures and without anti-coagulant before the start of neoadjuvant chemotherapy and before the last docetaxel cycle. Blood was allowed to coagulate for up to 2 h at room temperature. Serum was then separated by centrifugation, used for clinical routine dosages and excess serum was immediately aliquoted, frozen and stored at −80 °C in our dedicated biobank following the patients’ written informed consent for its use for research purposes. No more than two freeze–thaw cycles were allowed for any sample for measuring serum bone markers. To compare the baseline vitamin D level of the study population with that of a control group, we analyzed the results of 6,948 vitamin D determinations in serum samples from women referred to our clinical laboratory throughout 2009. We performed a case–control analysis by matching the control and study populations for age, ethnic group and month of vitamin D determination (±30 days), with a 1:3 case:control ratio.
Laboratory assessments
Biochemical analyses (calcium) were performed on a Cobas 6000 automaton (Roche Diagnostics, Meylan, France). 25OHD was measured using the DiaSorin 25-Hydroxyvitamin D-125I RIA kit. Serum bone markers were analyzed by using ELISA or IRMA techniques with the following commercial immunoassays: Human sRANKL (Total) Elisa (Biovendor, Heidelberg, Germany) for soluble RANKL quantification (pmol/L), Quantikine Human TRAIL/TNFSF10 (R&D System, Abingdon, UK) for TRAIL quantification (pg/mL), Bone Trap® Assay (Immunodiagnostic Systems, Paris, France) for bone TRAP quantification (U/L), OPG ELISA (Immunodiagnostic Systems, Paris, France) for OPG quantification (mol/L), Serum CrossLaps® ELISA (Immunodiagnostic Systems, Paris, France) for CrossLaps quantification (ng/mL) and BI-20412 DKK-1 (Biomedica, Wien, Austria) for DKK1 quantification (pmol/L).
Statistical methods
Descriptive analyses were used for the demographic and clinical characteristics. The distribution of serum 25OHD levels was categorized as adequate (25OHD serum level >30 ng/mL) or as mild (29–20 ng/mL), moderate (19–10 ng/mL) and severe vitamin D insufficiency (<10 ng/mL). Categorical variables were reported in contingency tables. To investigate the association of classical clinico-pathological parameters with 25OHD blood levels, univariate statistical analyses were performed for categorical variables using the Pearson’s chi-square test or Fisher’s exact test, when applicable. For continuous variables, median and range were computed. The non-parametric Kruskal–Wallis test or Mann–Whitney test were used, as appropriate, to evaluate significant differences between groups of interest. Kinetic changes between baseline and end of treatment values for the same individual were evaluated using the Wilcoxon matched pairs signed rank sum test. Patients with missing baseline and/or end of treatment values because of limited quantity of serum sample were not considered in the statistical analysis by using a matched pairs test. The Spearman’s correlation was performed to investigate the strength of the relationship between pairs of variables. All reported p values are two sided and the significance level was set at 5 % (p < 0.05). Statistical analysis was performed using the STATA 11 software (Stata Corporation, College Station, TX).
Results
The main clinico-pathological characteristics of the study group (n = 77) were those typical of patients with breast cancer selected for neoadjuvant chemotherapy (Table 1). The population was ethnically homogeneous (74 Caucasian and 3 North African women). Median age was 50 years (range 25–74). All patients received the planned seven neoadjuvant chemotherapy cycles. Four tumors were not scored using the Elston and Ellis modified SBR score because of the biopsy size. The majority (57.1 %) of patients was pre-menopausal and had large tumors; 23 % of patients achieved a pathologic complete response. Among the tumors, 23.4 % were triple negative, 31.2 % overexpressed HER2 and 45.4 % were HR+/HER2−.
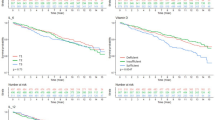
At baseline, 79.5 % of the patients had vitamin D insufficiency that was moderate in 33.8 % and severe in 10.4 % of the cases (i.e., 25OHD <20 and <10 ng/mL, respectively). Comparison of the 77 patients and 231 matched controls indicated that the baseline serum vitamin D levels were significantly lower in the patients’ population than in controls (median [range]: 21.3 [1.7–50.7] vs. 24.2 [4.7–71.8], respectively, p = 0.03). The proportion of vitamin D insufficiency increased to 97.4 % at the end of neoadjuvant chemotherapy (p < 0.0001) (49.4 % with moderate and 23.4 % with severe insufficiency). The median serum 25OHD values at baseline and at the end of treatment were 21.3 ng/mL (range, 1.7–50.7 ng/mL) and 14.7 ng/mL (range, 2.4–42.7 ng/mL), respectively (Fig. 1). Baseline vitamin D insufficiency was marginally associated with the tumor phenotype (p = 0.066), as it was detected in 18, 31.1 and 50.8 % of patients with triple negative, HER2+ and HER2−/HR+ cancers, respectively. No other significant association with clinico-pathological characteristics was found (data not shown).
Comparison of the concentration of bone metabolism markers at baseline and at the end of neoadjuvant chemotherapy showed a significant decrease in the serum levels of calcium and RANKL concomitantly with a significant increase of OPG, resulting in a significant decrease of the RANKL/OPG ratio. No significant variations were found for CrossLaps, Bone TRAP, TRAIL and DKK-1 serum levels (Table 2). The serum levels of calcium and vitamin D, RANKL and vitamin D and RANKL and OPG were significantly correlated (Spearman’s coefficient r = 0.2721, p = 0.0006; r = 0.1916, p = 0.002 and r = −0.179, p = 0.03 respectively).
To evaluate the impact of ethnic heterogeneity, we performed a second analysis in which only the 74 patients of European ancestry were included. While the demographic data did not significantly change, the baseline vitamin D insufficiency, which was only marginally associated with the tumor phenotype (p = 0.066) in the whole population, became significantly associated in this sub-population (p = 0.0498). Conversely, the significant inverse correlation between RANKL and OPG levels (Spearman’s coefficient r = −0.179, p = 0.03) found in the whole population showed only a statistical trend towards significance in the 74 patients’ group (Spearman’s coefficient r = −0.165, p = 0.0512), probably because of the reduction of the number of patients.
Discussion
In our homogeneous population of patients with locally advanced breast cancer, 79.5 % had baseline vitamin D insufficiency, which was severe in 10.4 % of the cases, and 97.4 % at the end of neoadjuvant chemotherapy (23.4 % with severe insufficiency). As the study period covered 18 months (i.e., the time elapsed between the baseline sampling for the first patient and the end of treatment sampling for the last patient), including two summers, the observed high frequency of vitamin D insufficiency cannot be explained by seasonal variations. Furthermore, in the control group (matched for age, ethnicity and month of vitamin D determination), vitamin D levels were overall higher than in the patients’ group, supporting the hypothesis that the important vitamin D deficiency observed in the study population was related to breast cancer. Vitamin D insufficiency was also associated with changes in the calcium/RANKL/OPG axis, with a significant decrease of the serum calcium level and of the RANKL/OPG ratio. Finally, the observation that the patients with HER2−/HR+ tumors were more likely to have vitamin D insufficiency already at baseline might be important given the recent description of the association between vitamin D insufficiency and poor prognosis mainly in luminal-like breast cancers [58].
As vitamin D insufficiency is particularly common in patients with breast cancer [7, 33, 40], current guidelines encourage daily supplementation with 1,200 mg calcium and 400 IU vitamin D, like in the general population [59, 60]. However, this seems insufficient. Indeed, Crew and colleagues reported that, after 1 year of standard supplementation (400 IU vitamin D3 daily), the serum values of 25OHD were normalized in less than 15 % of the 74 % pre-menopausal patients with early breast cancer who had baseline vitamin D insufficiency [33]. Similarly, in the retrospective study by Peppone et al., daily low-dose vitamin D supplementation failed to significantly increase 25OHD levels in patients with breast cancer who had insufficient vitamin D levels (<32 ng/mL) at baseline (66.5 %) [61]. These patients were affected by a significantly lower lumbar BMD (p = 0.03). On the other hand, in the study by Khan and colleagues [62], supplementation with weekly vitamin D3 doses of 50,000 IU was well tolerated and was associated with a lower incidence of musculoskeletal pain. Thus, vitamin D insufficiency in patients with breast cancer does not seem to respond to standard low-dose vitamin D supplementation and might be linked to decreased BMD [61, 63]. Conversely, optimal vitamin D correction has been associated with increased BMD and better response to anti-resorbing agents [64, 65]. Similarly, an international experts group recently highlighted that low-dose supplementation was not sufficient to achieve adequate vitamin D blood levels and recommended that patients with breast cancer treated with aromatase inhibitors should receive daily vitamin D doses between 1,000 and 5,000 IU [66]. The identification and correction of vitamin D insufficiency in patients with breast cancer is crucial; however, the efficacy of high-dose vitamin D supplementation in breast cancer needs to be validated in a phase III randomized study.
Our study also shows a significant decrease of the RANKL/OPG ratio by the end of the neoadjuvant chemotherapy. The balance between OPG and RANKL is important for bone homeostasis and is linked to vitamin D levels [51]. In a pre-clinical model, incubation with 1,25OHD induced a significant (>200 %) increase of RANKL and, to a less extent, of OPG mRNA expression in human osteoblasts [67]. These effects of 1,25OHD were more important in osteoblasts from osteoporotic women than in osteoblasts from osteoarthritic women. The greater bone loss that characterizes osteoporotic patients could thus be mediated by an imbalance of the RANKL/OPG system, involving vitamin D. Indeed, the serum RANKL/OPG ratio was significantly correlated with BMD in a population of 382 healthy post-menopausal women [68] and in a sample of 163 Apulian women [69]. Conversely, in a Korean study, the decrease in serum RANKL/OPG ratio was not associated with changes in BMD in a population of 143 post-menopausal women after 1 year of estrogen plus progestogen replacement therapy [70]. An important increase in the RANKL/OPG ratio was described in Paget’s disease of bone and this imbalance could be modified using bisphosphonates [71]. Thus, the therapeutic effect of bisphosphonates in the treatment of Paget’s disease of bone may be because of the suppression of RANKL-induced bone resorption through decreased RANKL and increased OPG production. However, the clinical implication of the OPG–RANKL system varies in different pathological situations, as no variation in the RANKL/OPG ratio was reported following treatment with ibandronate for hypercalcemia of malignancies [72]. Furthermore, Mountzios et al. [73] reported a significantly lower RANKL/OPG ratio in patients with prostate cancer than in patients with breast cancer, suggesting variations of this system involvement in different malignancies. The clinical and biological impact of an anti-RANKL treatment, such as denosumab, in breast cancer patients’ bone well-being might thus be relevant [74], but needs to be evaluated in dedicated randomized studies. We did not find any variation in the metabolism of bone markers, such as TRAIL, Bone TRAP, CrossLaps and DKK-1. Actually, bone disorders are associated with much stronger deficit of vitamin D that, in case of deficiency, is also preferentially used for its classical effects on bone metabolism. Our data suggest that, in early stage breast cancer, the bone structure is not or only weakly modified by the low level of vitamin D. It is also possible that these markers are not sensitive enough to detect minor modifications of bone metabolism. Indeed, in the clinical practice, because of its lack of sensitivity, CrossLaps measurement is not recommended for the diagnosis of osteoporosis, but only for the follow-up of patients with osteoporosis treated with bisphosphonate. Variations in Bone TRAP, Crosslaps and DKK-1 serum concentrations have been previously reported only in metastatic disease [44, 75]. Except for OPG and RANKL, bone markers seem to be unchanged during the early stage of breast cancers.
In conclusion, in this clinical study, we comprehensively evaluated the changes in bone metabolism during neoadjuvant chemotherapy of locally advanced breast cancer. The baseline serum vitamin D levels were significantly lower in the study population than in the matched controls. At the end of treatment, nearly all patients suffered from vitamin D insufficiency that was associated with changes in the calcium/RANKL/OPG axis, evocative of deregulation of a functional regulatory mechanism. These results require further analyses to define the role of pharmacologic modulation, such as adequate correction of the vitamin D insufficiency or the use of agents that target bone remodeling, in correcting the bone metabolism changes and thus improving bone homeostasis in patients with non-metastatic breast cancer. A French study is currently evaluating the best way to correct vitamin D insufficiency in patients with breast cancer (ClinicalTrials.gov Identifier NCT01480869). This study is associated with an ancillary comprehensive analysis of serum biomarkers to better understand the complex mechanisms underlying bone metabolism modifications in breast cancer.
References
Brufsky AM (2008) Cancer treatment-induced bone loss: pathophysiology and clinical perspectives. Oncologist 13(2):187–195
Pfeilschifter J, Diel IJ (2000) Osteoporosis due to cancer treatment: pathogenesis and management. J Clin Oncol 18(7):1570–1593
Chen Z, Maricic M, Bassford TL, Pettinger M, Ritenbaugh C, Lopez AM, Barad DH, Gass M, Leboff MS (2005) Fracture risk among breast cancer survivors: results from the Women’s Health Initiative Observational Study. Arch Intern Med 165(5):552–558
Mincey BA (2003) Osteoporosis in women with breast cancer. Curr Oncol Rep 5(1):53–57
Saarto T, Blomqvist C, Valimaki M, Makela P, Sarna S, Elomaa I (1997) Chemical castration induced by adjuvant cyclophosphamide, methotrexate, and fluorouracil chemotherapy causes rapid bone loss that is reduced by clodronate: a randomized study in premenopausal breast cancer patients. J Clin Oncol 15(4):1341–1347
Shapiro CL, Manola J, Leboff M (2001) Ovarian failure after adjuvant chemotherapy is associated with rapid bone loss in women with early-stage breast cancer. J Clin Oncol 19(14):3306–3311
Goodwin PJ, Ennis M, Pritchard KI, Koo J, Hood N (2009) Prognostic effects of 25-hydroxyvitamin D levels in early breast cancer. J Clin Oncol 27(23):3757–3763
Sinotte M, Diorio C, Berube S, Pollak M, Brisson J (2009) Genetic polymorphisms of the vitamin D binding protein and plasma concentrations of 25-hydroxyvitamin D in premenopausal women. Am J Clin Nutr 89(2):634–640
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281
Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B (2005) Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA 293(18):2257–2264
Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A (2007) Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet 370(9588):657–666
Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, Wong JB (2004) Effect of vitamin D on falls: a meta-analysis. JAMA 291(16):1999–2006
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, Bassford T, Beresford SA, Black HR, Blanchette P et al (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354(7):669–683
Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B (2006) Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr 84(1):18–28
Wactawski-Wende J, Kotchen JM, Anderson GL, Assaf AR, Brunner RL, O’Sullivan MJ, Margolis KL, Ockene JK, Phillips L, Pottern L et al (2006) Calcium plus vitamin D supplementation and the risk of colorectal cancer. N Engl J Med 354(7):684–696
Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP (2007) Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr 85(6):1586–1591
Jensen SS, Madsen MW, Lukas J, Binderup L, Bartek J (2001) Inhibitory effects of 1alpha,25-dihydroxyvitamin D(3) on the G(1)-S phase-controlling machinery. Mol Endocrinol 15(8):1370–1380
Colston KW, Hansen CM (2002) Mechanisms implicated in the growth regulatory effects of vitamin D in breast cancer. Endocr Relat Cancer 9(1):45–59
Wang D, Dubois RN (2004) Cyclooxygenase-2: a potential target in breast cancer. Semin Oncol 31(1 Suppl 3):64–73
Krishnan AV, Swami S, Feldman D (2010) Vitamin D and breast cancer: inhibition of estrogen synthesis and signaling. J Steroid Biochem Mol Biol 121(1–2):343–348
Garland CF, Garland FC, Gorham ED (1999) Calcium and vitamin D. Their potential roles in colon and breast cancer prevention. Ann N Y Acad Sci 889:107–119
Yao S, Zirpoli G, Bovbjerg DH, Jandorf L, Hong CC, Zhao H, Sucheston LE, Tang L, Roberts M, Ciupak G et al (2012) Variants in the vitamin D pathway, serum levels of vitamin D, and estrogen receptor negative breast cancer among African-American women: a case–control study. Breast Cancer Res 14(2):R58
Shao T, Klein P, Grossbard ML (2012) Vitamin D and breast cancer. Oncologist 17(1):36–45
Lin J, Manson JE, Lee IM, Cook NR, Buring JE, Zhang SM (2007) Intakes of calcium and vitamin D and breast cancer risk in women. Arch Intern Med 167(10):1050–1059
Shin MH, Holmes MD, Hankinson SE, Wu K, Colditz GA, Willett WC (2002) Intake of dairy products, calcium, and vitamin d and risk of breast cancer. J Natl Cancer Inst 94(17):1301–1311
Freedman DM, Chang SC, Falk RT, Purdue MP, Huang WY, McCarty CA, Hollis BW, Graubard BI, Berg CD, Ziegler RG (2008) Serum levels of vitamin D metabolites and breast cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Epidemiol Biomarkers Prev 17(4):889–894
Abbas S, Linseisen J, Slanger T, Kropp S, Mutschelknauss EJ, Flesch-Janys D, Chang-Claude J (2008) Serum 25-hydroxyvitamin D and risk of post-menopausal breast cancer—results of a large case–control study. Carcinogenesis 29(1):93–99
Garland CF, Gorham ED, Mohr SB, Grant WB, Giovannucci EL, Lipkin M, Newmark H, Holick MF, Garland FC (2007) Vitamin D and prevention of breast cancer: pooled analysis. J Steroid Biochem Mol Biol 103(3–5):708–711
Janowsky EC, Lester GE, Weinberg CR, Millikan RC, Schildkraut JM, Garrett PA, Hulka BS (1999) Association between low levels of 1,25-dihydroxyvitamin D and breast cancer risk. Public Health Nutr 2(3):283–291
Abbas S, Linseisen J, Chang-Claude J (2007) Dietary vitamin D and calcium intake and premenopausal breast cancer risk in a German case–control study. Nutr Cancer 59(1):54–61
Bertone-Johnson ER (2007) Prospective studies of dietary vitamin D and breast cancer: more questions raised than answered. Nutr Rev 65(10):459–466
Chlebowski RT, Johnson KC, Kooperberg C, Pettinger M, Wactawski-Wende J, Rohan T, Rossouw J, Lane D, O’Sullivan MJ, Yasmeen S et al (2008) Calcium plus vitamin D supplementation and the risk of breast cancer. J Natl Cancer Inst 100(22):1581–1591
Crew KD, Shane E, Cremers S, McMahon DJ, Irani D, Hershman DL (2009) High prevalence of vitamin D deficiency despite supplementation in premenopausal women with breast cancer undergoing adjuvant chemotherapy. J Clin Oncol 27(13):2151–2156
Engel P, Fagherazzi G, Boutten A, Dupre T, Mesrine S, Boutron-Ruault MC, Clavel-Chapelon F (2010) Serum 25(OH) vitamin D and risk of breast cancer: a nested case–control study from the French E3N cohort. Cancer Epidemiol Biomarkers Prev 19(9):2341–2350
Lowe LC, Guy M, Mansi JL, Peckitt C, Bliss J, Wilson RG, Colston KW (2005) Plasma 25-hydroxy vitamin D concentrations, vitamin D receptor genotype and breast cancer risk in a UK Caucasian population. Eur J Cancer 41(8):1164–1169
Khan QJ, Reddy PS, Kimler BF, Sharma P, Baxa SE, O’Dea AP, Klemp JR, Fabian CJ (2010) Effect of vitamin D supplementation on serum 25-hydroxy vitamin D levels, joint pain, and fatigue in women starting adjuvant letrozole treatment for breast cancer. Breast Cancer Res Treat 119(1):111–118
Iqbal SJ (1994) Vitamin D metabolism and the clinical aspects of measuring metabolites. Ann Clin Biochem 31(Pt 2):109–124
Holick MF (1995) Defects in the synthesis and metabolism of vitamin D. Exp Clin Endocrinol Diabetes 103(4):219–227
Hollis BW (1996) Assessment of vitamin D nutritional and hormonal status: what to measure and how to do it. Calcif Tissue Int 58(1):4–5
Tangpricha V, Pearce EN, Chen TC, Holick MF (2002) Vitamin D insufficiency among free-living healthy young adults. Am J Med 112(8):659–662
Mann GB, Kang YC, Brand C, Ebeling PR, Miller JA (2009) Secondary causes of low bone mass in patients with breast cancer: a need for greater vigilance. J Clin Oncol 27(22):3605–3610
Gregory CA, Gunn WG, Reyes E, Smolarz AJ, Munoz J, Spees JL, Prockop DJ (2005) How Wnt signaling affects bone repair by mesenchymal stem cells from the bone marrow. Ann N Y Acad Sci 1049:97–106
Tian E, Zhan F, Walker R, Rasmussen E, Ma Y, Barlogie B, Shaughnessy JD Jr (2003) The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med 349(26):2483–2494
Voorzanger-Rousselot N, Goehrig D, Journe F, Doriath V, Body JJ, Clezardin P, Garnero P (2007) Increased Dickkopf-1 expression in breast cancer bone metastases. Br J Cancer 97(7):964–970
Raisz LG (2005) Pathogenesis of osteoporosis: concepts, conflicts, and prospects. J Clin Invest 115(12):3318–3325
Calvo MS, Eyre DR, Gundberg CM (1996) Molecular basis and clinical application of biological markers of bone turnover. Endocr Rev 17(4):333–368
Jukkola A, Tahtela R, Tholix E, Vuorinen K, Blanco G, Risteli L, Risteli J (1997) Aggressive breast cancer leads to discrepant serum levels of the type I procollagen propeptides PINP and PICP. Cancer Res 57(24):5517–5520
Minkin C (1982) Bone acid phosphatase: tartrate-resistant acid phosphatase as a marker of osteoclast function. Calcif Tissue Int 34(3):285–290
Rogers A, Eastell R (2005) Circulating osteoprotegerin and receptor activator for nuclear factor kappaB ligand: clinical utility in metabolic bone disease assessment. J Clin Endocrinol Metab 90(11):6323–6331
Dougall WC (2012) Osteoclast-dependent and -independent roles of the RANKL/RANK/OPG pathway in tumorigenesis and metastasis. Clin Cancer Res 18(2):326–335
Delmas PD (2008) Clinical potential of RANKL inhibition for the management of postmenopausal osteoporosis and other metabolic bone diseases. J Clin Densitom 11(2):325–338
Ibrahim T, Sacanna E, Gaudio M, Mercatali L, Scarpi E, Zoli W, Serra P, Ricci R, Serra L, Kang Y et al (2011) Role of RANK, RANKL, OPG, and CXCR4 tissue markers in predicting bone metastases in breast cancer patients. Clin Breast Cancer 11(6):369–375
Whyte MP (2006) Paget’s disease of bone and genetic disorders of RANKL/OPG/RANK/NF-kappaB signaling. Ann N Y Acad Sci 1068:143–164
Schramek D, Sigl V, Penninger JM (2011) RANKL and RANK in sex hormone-induced breast cancer and breast cancer metastasis. Trends Endocrinol Metab 22(5):188–194
Holen I, Shipman CM (2006) Role of osteoprotegerin (OPG) in cancer. Clin Sci 110(3):279–291
Kawano Y, Ueno S, Abe M, Kikukawa Y, Yuki H, Iyama K, Okuno Y, Mitsuya H, Hata H (2012) TRAIL produced from multiple myeloma cells is associated with osteolytic. Oncol Rep 27(1):39–44
Sataloff DM, Mason BA, Prestipino AJ, Seinige UL, Lieber CP, Baloch Z (1995) Pathologic response to induction chemotherapy in locally advanced carcinoma of the breast: a determinant of outcome. J Am Coll Surg 180(3):297–306
Kim HJ, Lee YM, Ko BS, Lee JW, Yu JH, Son BH, Gong GY, Kim SB, Ahn SH (2011) Vitamin D deficiency is correlated with poor outcomes in patients with luminal-type breast cancer. Ann Surg Oncol 18(7):1830–1836
Hillner BE, Ingle JN, Chlebowski RT, Gralow J, Yee GC, Janjan NA, Cauley JA, Blumenstein BA, Albain KS, Lipton A et al (2003) American Society of Clinical Oncology 2003 update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 21(21):4042–4057
Van Poznak CH, Temin S, Yee GC, Janjan NA, Barlow WE, Biermann JS, Bosserman LD, Geoghegan C, Hillner BE, Theriault RL et al (2011) American Society of Clinical Oncology executive summary of the clinical practice guideline update on the role of bone-modifying agents in metastatic breast cancer. J Clin Oncol 29(9):1221–1227
Peppone LJ, Huston AJ, Reid ME, Rosier RN, Zakharia Y, Trump DL, Mustian KM, Janelsins MC, Purnell JQ, Morrow GR (2011) The effect of various vitamin D supplementation regimens in breast cancer patients. Breast Cancer Res Treat 127(1):171–177
Khan QJ, Reddy PS, Kimler BF, Sharma P, Baxa SE, O’Dea AP, Klemp JR, Fabian CJ (2010) Effect of vitamin D supplementation on serum 25-hydroxy vitamin D levels, joint pain, and fatigue in women starting adjuvant letrozole treatment for breast cancer. Breast Cancer Res Treat 119(1):111–118
Nogues X, Servitja S, Pena MJ, Prieto-Alhambra D, Nadal R, Mellibovsky L, Albanell J, Diez-Perez A, Tusquets I (2010) Vitamin D deficiency and bone mineral density in postmenopausal women receiving aromatase inhibitors for early breast cancer. Maturitas 66(3):291–297
Grados F, Brazier M, Kamel S, Duver S, Heurtebize N, Maamer M, Mathieu M, Garabedian M, Sebert JL, Fardellone P (2003) Effects on bone mineral density of calcium and vitamin D supplementation in elderly women with vitamin D deficiency. Joint Bone Spine 70(3):203–208
Adami S, Giannini S, Bianchi G, Sinigaglia L, Di Munno O, Fiore CE, Minisola S, Rossini M (2009) Vitamin D status and response to treatment in post-menopausal osteoporosis. Osteoporos Int 20(2):239–244
Roux C, Bischoff-Ferrari HA, Papapoulos SE, de Papp AE, West JA, Bouillon R (2008) New insights into the role of vitamin D and calcium in osteoporosis management: an expert roundtable discussion. Curr Med Res Opin 24(5):1363–1370
Giner M, Rios MA, Montoya MA, Vazquez MA, Naji L, Perez-Cano R (2009) RANKL/OPG in primary cultures of osteoblasts from post-menopausal women. Differences between osteoporotic hip fractures and osteoarthritis. J Steroid Biochem Mol Biol 113(1–2):46–51
Nabipour I, Larijani B, Vahdat K, Assadi M, Jafari SM, Ahmadi E, Movahed A, Moradhaseli F, Sanjdideh Z, Obeidi N et al (2009) Relationships among serum receptor of nuclear factor-kappaB ligand, osteoprotegerin, high-sensitivity C-reactive protein, and bone mineral density in postmenopausal women: osteoimmunity versus osteoinflammatory. Menopause 16(5):950–955
D’Amore M, Fanelli M, D’Amore S, Fontana A, Minenna G (2006) Receptor activator of NF(Kappa)B ligand/osteoprotegerin (RANKL/OPG) system and osteopontin (OPN) serum levels in a population of apulian postmenopausal women. Panminerva Med 48(4):215–221
Kim JG, Kim JH, Lee DO, Kim H, Kim JY, Suh CS, Kim SH, Choi YM (2008) Changes in the serum levels of osteoprotegerin and soluble receptor activator for nuclear factor kappaB ligand after estrogen–progestogen therapy and their relationships with changes in bone mass in postmenopausal women. Menopause 15(2):357–362
Martini G, Gennari L, Merlotti D, Salvadori S, Franci MB, Campagna S, Avanzati A, De Paola V, Valleggi F, Nuti R (2007) Serum OPG and RANKL levels before and after intravenous bisphosphonate treatment in Paget’s disease of bone. Bone 40(2):457–463
Zojer N, Brenner K, Beke D, Kudlacek S, Hawa G, Woloszczuk W, Hofbauer LC, Pecherstorfer M (2005) Bisphosphonate treatment does not affect serum levels of osteoprotegerin and RANKL in hypercalcemic cancer patients. Anticancer Res 25(5):3607–3612
Mountzios G, Terpos E, Syrigos K, Papadimitriou C, Papadopoulos G, Bamias A, Mavrikakis M, Dimopoulos MA (2010) Markers of bone remodeling and skeletal morbidity in patients with solid tumors metastatic to the skeleton receiving the biphosphonate zoledronic acid. Transl Res 155(5):247–255
Kearns AE, Khosla S, Kostenuik PJ (2008) Receptor activator of nuclear factor kappaB ligand and osteoprotegerin regulation of bone remodeling in health and disease. Endocr Rev 29(2):155–192
Voorzanger-Rousselot N, Juillet F, Mareau E, Zimmermann J, Kalebic T, Garnero P (2006) Association of 12 serum biochemical markers of angiogenesis, tumour invasion and bone turnover with bone metastases from breast cancer: a crossectional and longitudinal evaluation. Br J Cancer 95(4):506–514
Acknowledgments
This study was supported by an unrestricted research grant from Amgen France and by the Centre Régional de Lutte Contre le Cancer Val d’Aurelle.
Conflict of interest
Honoraria: Dr Stéphane Pouderoux, AMGEN.
Ethical standards
This project was performed in compliance with the relevant ethical standards in France.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacot, W., Pouderoux, S., Thezenas, S. et al. Increased prevalence of vitamin D insufficiency in patients with breast cancer after neoadjuvant chemotherapy. Breast Cancer Res Treat 134, 709–717 (2012). https://doi.org/10.1007/s10549-012-2084-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2084-7