Abstract
Mammographic density is strongly and consistently associated with breast cancer risk. To determine if this association was modified by reproductive factors (parity and age at first birth), data were combined from four case–control studies conducted in the United States and Japan. To overcome the issue of variation in mammographic density assessment among the studies, a single observer re-read all the mammograms using one type of interactive thresholding software. Logistic regression was used to estimate odds ratios (OR) while adjusting for other known breast cancer risk factors. Included were 1,699 breast cancer cases and 2,422 controls, 74% of whom were postmenopausal. A positive association between mammographic density and breast cancer risk was evident in every group defined by parity and age at first birth (OR per doubling of percent mammographic density ranged between 1.20 and 1.39). Nonetheless, the association appeared to be stronger among nulliparous than parous women (OR per doubling of percent mammographic density = 1.39 vs. 1.24; P interaction = 0.054). However, when examined by study location, the effect modification by parity was apparent only in women from Hawaii and when examined by menopausal status, it was apparent in postmenopausal, but not premenopausal, women. Effect modification by parity was not significant in subgroups defined by body mass index or ethnicity. Adjusting for mammographic density did not attenuate the OR for the association between parity and breast cancer risk by more than 16.4%, suggesting that mammographic density explains only a small proportion of the reduction in breast cancer risk associated with parity. In conclusion, this study did not support the hypothesis that parity modifies the breast cancer risk attributed to mammographic density. Even though an effect modification was found in Hawaiian women, no such thing was found in women from the other three locations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mammographic density is a relatively strong and consistent risk factor for breast cancer [1, 2]. It reflects breast tissue composition: dense fibroglandular tissues appear light on mammograms, whereas nondense fatty tissues appear dark. Both the relative (percent) and absolute areas of density seen on mammograms are related to breast cancer risk and women within the highest categories of mammographic density are at four to six times higher risk than women within the lowest categories [2]. Mammographic density is being extensively studied with the purpose of improving both the prediction of breast cancer risk and the understanding of breast carcinogenesis.
In order to achieve these ends, it is helpful to examine whether the association between mammographic density and breast cancer risk is modified or mediated by another risk factor. Such factors include body mass index (BMI) [3, 4], family history [5], hormone replacement therapy (HRT) [6, 7], and selective estrogen receptor modulators [8]. Reproductive factors have not yet been comprehensively studied as effect modifiers although changes in the breast induced by pregnancy may make the tissue less susceptible to the risk of carcinogenesis related to mammographic density. In accordance with this hypothesis, the association between mammographic density and breast cancer risk has been observed to be stronger in nulliparous women than in parous women in a previous study [9]. That the association between reproductive factors and breast cancer risk could be mediated by mammographic density is supported by several observations: parity is associated with breast cancer risk [10–12]; parity is inversely correlated with mammographic density [13–18]; and, as noted above, mammographic density is associated with breast cancer risk [1, 2]. Another indication of whether mammographic density could lie on the causal chain between parity and breast cancer risk is if the association between parity and breast cancer risk is attenuated after adjustment for mammographic density [19].
Studies published to date show a consistent association between mammographic density and breast cancer risk [2], but they often do not have the statistical power to demonstrate effect modification by factors that define population subgroups. Combining data from several studies could result in sufficient power, but it is not straightforward due to variations in mammographic density assessment arising from different techniques and observers. To overcome this issue, we have obtained the mammographic images from four case–control studies, and a single observer has re-read them using one type of interactive thresholding software [20]. The primary objective of this analysis was to determine if the association between mammographic density and breast cancer risk was modified by reproductive factors, specifically parity and age at first birth. The secondary objective was to describe whether mammographic density accounted for any part of the association between these reproductive factors and breast cancer risk.
Materials and methods
Study design
The methods of this project and the case–control studies that contributed the data are reported elsewhere [3, 21–24] and will only be briefly described here. The Institutional Review Boards at the four institutions approved both the original case–control studies and this project. Each study used incident breast cancer cases. Controls came from the general population in California, from participants of the Multiethnic Cohort without cancer in Hawaii, and from a screening of clinic population in Minnesota and Japan. Covariate information comprised ethnicity/race, menopausal status, HRT use, family history of breast cancer, and height and weight (from which BMI was calculated). Reproductive information included the number of children (Hawaii, Minnesota), parity (California, Japan), and age at first birth. This information was collected with: face-to-face interview using a structured questionnaire in California (soon after case diagnosis or control recruitment); self-administered questionnaire in Hawaii (at cohort baseline with an update on HRT at the time of the nested study) and in Japan (at the time of screening); and medical chart abstraction and a clinical database in Minnesota.
Mammographic density
Although mammographic density had been determined for each original study, different thresholding software and observers were used. Therefore, the measurements used in this analysis were made by a single observer (CGW) who re-read all films for this project using Cumulus interactive thresholding software [20]. A single digitized mammographic image was obtained for each research participant: the contralateral side for cases, and a randomly selected side for controls to achieve the same right–left frequencies as in the cases. In the studies conducted in California, Hawaii, and Minnesota, digitized screen film craniocaudal (CC) images were available. In Japan, digital mediolateral oblique (MLO) images were printed on film and digitized to a file format usable with the Cumulus thresholding software. In studies with multiple mammographic images across time for each subject [21, 23], we chose the mammogram proximal to diagnosis for the cases to correspond most closely to the other studies in which films at only one time were available.
The mammographic images from 4,254 participants, plus 270 of these images that were randomly selected to be re-read both within and between batches to estimate reliability, were read in 45 batches of 106–107 images. Each batch was read in two stages: first, the breast area was manually delineated from the background and pectoral muscle, and second, a threshold was set between the radiologically dense fibroglandular tissues and the nondense fatty tissues based on gray-level. The number of pixels within the breast and dense areas was determined by the software and converted to square centimeters based on the pixel size at which the images for each study were digitized. Percent dense area was calculated as the dense area divided by the breast area. A conversion was applied to adjust the percent dense area measures made on MLO views from Japan to be equivalent to those made on CC views [CC = (MLO − 2.6)/0.86] [25]. The reliability of the dense area and percent dense area measurements was high (intraclass correlation coefficient = 0.96 and 0.97, respectively).
Statistical analysis
The primary outcome and covariate data from each study were merged together into a single standardized database. Women with missing information on BMI or HRT use, the main confounders of the association between mammographic density and breast cancer risk, were excluded. Women with missing values for parity (N = 21) or age at first birth (N = 30) were assigned the category that was most frequent for their location/ethnic group. To examine the effect of this imputation, all analyses described below were repeated excluding these participants; no substantive changes were observed, and so results are reported for the whole group. Because the mammograms from Japan were different with respect to being processed digital images and the MLO view, all analyses were repeated excluding this study; again no substantive changes in the results were observed.
Study participants were described on the basis of demographic and breast cancer risk factors using means and frequencies as appropriate. The association between reproductive factors (parity and age at first birth) and mammographic density in the control group was estimated with general linear models. Because dense area was positively skewed, this variable was square root-transformed for these analyses.
The association between mammographic density and breast cancer risk was represented by odds ratios (OR) with 95% confidence intervals (CI) estimated from unconditional logistic regression models. In these models, the mammographic variables were examined either in three categories representing the approximate tertiles of their distribution in the combined control group or logarithmically (base 2) transformed such that the OR estimated the risk associated with a doubling of mammographic density. All models were adjusted for age at mammogram (continuous), menopausal status/current HRT use (premenopausal, postmenopausal/no HRT, and postmenopausal/HRT), family history of breast cancer (1st degree, or no 1st degree), and location/ethnicity (California/Caucasian, California/Asian, California/African American, Minnesota/Caucasian, Hawaii/Caucasian, Hawaii/Asian, Hawaii/other, Japan/Asian).
To examine effect modification, that is, if the association between mammographic density and breast cancer risk was heterogeneous across subgroups defined by parity (0, 1–2, ≥3 children), the significance of the interaction term between log-transformed mammographic density and parity was determined with the likelihood ratio test. Similarly, the association between mammographic density and breast cancer risk was examined by age at first birth (<26, ≥26 years; among parous women only). To better illustrate and describe the difference between nulliparous and parous women in the dose–response relationship suggested by these results, a post-hoc logistic regression analysis using restricted cubic splines with knots at the 10th, 50th, and 90th percentiles of percent dense area (i.e., at 8, 29, and 56% dense areas) was done using a SAS macro kindly provided by Dr. Desquilbet [26]. Finally, it was of interest to describe whether the effect modification was of a similar strength in subgroups defined by location, ethnicity, BMI, and menopausal status. Subgroups with less than 20 cases or controls were omitted from these analyses.
If the association between parity or age at first birth and breast cancer risk was significant in these data, the percent change in the ORs with adjustment for mammographic density was estimated using the equation: 100% × (ORnot adjusted for MD − ORadjusted for MD)/(ORnot adjusted for MD − 1) [27]. As our objective was to describe if the association between reproductive factors and breast cancer risk was partially explained by mammographic density, we did not formally test the significance of the mediation effect [19].
All analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
Of the 4,254 women for whom a digitized mammographic image could be located, 133 were excluded because of suspected breast implants (N = 4), incomplete images (N = 2), or missing information on BMI (N = 49), current HRT use (N = 76), or both (N = 2). Thus, 1,699 cases and 2,422 controls were included (Table 1). Over 40% of the participants were Caucasian and approximately 40% were Asian; the remaining were African American or other ethnicities. Most of the women (74.1%) were postmenopausal, and of these, 38.1% used HRT. Mean (SD) BMI was 25.4 (5.3) kg/m2. Most of the women (86.8%) were parous, and of these, 35.5% had their first live birth when they were 26 years of age or older. Mean (SD) percent mammographic density was 31.7 (17.7) in cases and 29.6 (18.9) in controls. Percent dense area and absolute dense area were highly correlated (r s = 0.74).
The association between parity and mammographic density was investigated among controls (Table 2). Percent dense area was lower among women with greater parity (P < 0.0001) and did not vary by age at first birth among parous women (P = 0.10). Results for dense area followed a similar pattern.
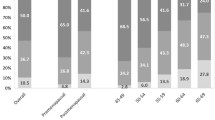
Percent dense area was associated with the risk of breast cancer in every subgroup defined by parity and age at first birth (Table 3). The magnitude of the effect was greater among nulliparous than parous women (OR per doubling of percent dense area = 1.39 vs. 1.24; P interaction = 0.054). The pattern of ORs across tertiles suggested that the dose–response relationship between percent dense area and breast cancer risk was different by parity. In nulliparous women, risks were elevated to a similar extent in the second tertile (OR = 2.83, 95% CI: 1.64–4.87) and the third tertile (OR = 2.63, 95% CI: 1.51–4.56) relative to the first. In parous women, a threshold was not apparent and risk increased with each tertile (OR = 1.51, 95% CI: 1.25–1.82, and OR = 1.90, 95% CI: 1.56–2.32). A post-hoc analysis to explore the shape of the relationship as modeled using restricted cubic splines (Fig. 1) reflects the pattern observed in Table 3.
Among parous women (Table 3), the association between percent dense area and breast cancer risk in women with one or two children was similar to that in women with three or more children (P interaction = 0.34). The magnitude of the effect among women with a first live birth at 26 years of age or older was nonsignificantly greater than the effect among women who were younger when they had their first child (OR per doubling = 1.33 vs. 1.20; P interaction = 0.16). Similar results were observed in models with dense area as the exposure with two distinctions. First, the magnitude of the association between dense area and breast cancer risk was very similar among nulliparous and parous women (OR per doubling = 1.35 vs. 1.31; P interaction = 0.63). Second, the heterogeneity of the effect by age at first birth was greater (first birth <26 years, OR per doubling = 1.25; first birth ≥26 years, OR = 1.47; P interaction = 0.03).
The modification of the association between percent dense area and breast cancer risk by parity appeared stronger in specific subgroups (Table 4). Although it was not significant in California (P interaction = 0.64) or Minnesota (P interaction = 0.20), it was very apparent in Hawaii (P interaction = 0.006). This pattern by location held when using the mammographic density measurements made by the original readers in the parent studies and when restricted to White participants (data not shown). When restricted to either postmenopausal participants or Asian participants, a stronger association among nulliparous than parous women was suggested, but was not statistically significant because of sparse data, not only in Hawaii but also in California (data not shown). Significant effect modification by parity was not observed in groups defined by ethnicity. Effect modification by parity was not significant in either normal weight (BMI 18.5–<25 kg/m2; P interaction = 0.65) or overweight/obese women (BMI ≥ 25 kg/m2; P interaction = 0.35) but was slightly stronger in the latter subgroup. It also was apparent in postmenopausal women (P interaction = 0.03), but not in premenopausal women (P interaction = 0.41).
Parity was associated with a lower risk of breast cancer (Table 5). Relative to nulliparous women, the risk of breast cancer was reduced by 24% (95% CI: 7–38) among women with one or two children and by 35% (95% CI: 20–47) among women with three or more children. Adjusting for either percent dense area or dense area attenuated these ORs, but never more than 16.4%, and they remained significant. Among parous women, age at first birth was not significantly related to an increased risk of breast cancer.
Discussion
In this analysis with 1,699 breast cancer cases and 2,422 controls from four studies, an association between mammographic density and breast cancer risk was evident in every subgroup defined by parity and age at first birth. The association appeared to be stronger among nulliparous than parous women with percent dense area (OR per doubling = 1.39 vs. 1.24; P interaction = 0.054), but not with dense area (OR per doubling = 1.35 vs. 1.31; P interaction = 0.63). However, when examined by study location, effect modification by parity was only observed in women from Hawaii, and when examined by menopausal status, it was observed only in postmenopausal women. Parous women had lower mammographic density than nulliparous women, but mammographic density seemed to explain only a small proportion of the reduction in breast cancer risk associated with parity.
Parity leads to changes in breast morphology (e.g., number and differentiation status of the lobular structures [28]), histology (e.g., amount of collagen [29]), and biochemistry (e.g., gene expression patterns [30, 31]). As suggested by correlations observed in this study and others [13–18, 32], some of the changes in breast composition induced by parity are reflected by a reduction in mammographic density. In the current article, however, although parity is associated with lower mammographic density and mammographic density is related to a reduction in breast cancer risk, we estimated using a standard calculation [27] that less than 17% of the association between parity and breast cancer risk is explained by mammographic density. Although the best method to validly quantify the proportion of an association that is explained by a putative mediator is currently under debate [33], the method we used should be sufficient to imply that the proportion mediated by mammographic density is slight. Thus, changes induced by pregnancy that are not reflected by mammographic density must also lead to a reduction in breast cancer risk. This suggestion is also supported by the observation in other studies that the association between parity and breast cancer risk remained significant after controlling for mammographic density in broad subjective qualitative categories [34–36]. The proportion mediated may be underestimated, however, by means of a single measure of mammographic density later in life that may not fully capture the cumulative reduction since the time of pregnancy. That the association between parity and breast cancer risk is not wholly mediated by a reduction in mammographic density is also supported by the observation that mammographic density affects the risk of both steroid receptor-positive and -negative subtypes of breast cancer [37], while parity appears to influence the risk of steroid receptor-positive cancers only [38, 39].
Most of the changes induced by pregnancy, which could lead to protection against breast carcinogenesis have been identified in the breast epithelial cells [31], although changes in circulating hormones or growth factors [40] or in the supporting stromal tissues [41] could also play a role. Variability in mammographic density, on the other hand, is largely determined by the amount of dense connective tissue and less so by the amount of epithelial tissue [29, 42]. The dense connective tissue, represented by mammographic density, could provide a growth-promoting environment that stimulates the proliferation of the epithelial cells [43, 44]. Owing to changes in the epithelial cells induced by pregnancy, it could be hypothesized that the epithelial cells in parous women are less susceptible to this stimulation than those in nulliparous women. Under such a scenario, the effect of mammographic density on breast cancer risk would be stronger among nulliparous than parous women, as observed in this study with percent dense area. Similarly, in an analysis among pre- and postmenopausal Caucasian women (129 cases and 517 controls) by van Gils et al. [9], the OR for breast cancer in women with >25% density relative to <5% density was 6.6 among nulliparous women, far greater than the OR of 3.6 among parous women [9]. Conversely, results from other small studies using broad subjective qualitative measures of mammographic density suggest a slightly stronger effect in parous women, but the interactions were not statistically significant [45, 46].
The pattern of ORs across categories of percent dense area observed in the present study suggests that risk in nulliparous women rises sharply and levels off or falls slightly, whereas in parous women, risk rises with each category of percent dense area but does not reach the levels observed in nulliparous women. Logistic modeling using restricted cubic splines in a post-hoc analysis illustrates this pattern, but will need to be confirmed in a larger population of nulliparous women.
Effect modification by parity in the present study was only observed in data from Hawaii and was not apparent in the other locations despite standardization of mammographic density assessment. This inconsistency could be introduced by instability in the estimates because of small numbers of nulliparous women, particularly in Minnesota and Japan, or by differences in the relative weighting of reasons for nulliparity (e.g., choice and infertility) from location to location. Owing to this inconsistency, if mammographic density is incorporated into individualized risk prediction models [47, 48], inclusion of the interaction with parity may not add to their performance.
Strengths of this study include the large sample size that provided the statistical power to detect modest yet meaningful degrees of effect modification; and the availability of information on potential confounders. Another considerable strength is the standardized assessment of mammographic density; it was done by a single observer using one type of interactive thresholding software. Other aspects of the measurement of mammographic density, however, could not be standardized including variation between and within studies arising from clinical mammography techniques (e.g., positioning and compression, and type of mammography unit) and the scanners used to digitize the films (e.g., range of optical density and pixel size). The Japanese mammograms, in particular, were different by virtue of being processed through digital versus film mammograms and of being the MLO versus CC view. We have previously reported that the association between mammographic density and breast cancer risk was heterogeneous between the studies and that this heterogeneity was largely driven by the data from Japan [3]; however, all analyses presented here were repeated excluding this study, and no substantive changes in the results were observed.
Limitations of the individual studies have been discussed in detail in their respective publications [21–24] and include the possibility of selection bias due to not limiting the cases to those enrolled in the screening program from which controls were derived in Japan and low response rates in Hawaii and California. Included women did not differ from women not included on the basis of parity, but in Hawaii, they had a slightly older age at first birth. Other limitations include the self-report of information about reproductive history and confounders, and the low number of nulliparous women (288 cases and 256 controls).
In conclusion, this study demonstrates that parity and mammographic density have independent effects on breast cancer risk. Although it suggests that the association between mammographic density and breast cancer risk may be stronger in nulliparous than parous women, this effect modification was only observed in the data from one of the four studies.
References
Boyd NF, Martin LJ, Bronskill M, Yaffe MJ, Duric N, Minkin S (2010) Breast tissue composition and susceptibility to breast cancer. J Natl Cancer Inst 102(16):1224–1237
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev 15(6):1159–1169
Conroy SM, Woolcott CG, Byrne C, Nagata C, Ursin G, Vachon CM, Yaffe MJ, Koga K, Pagano I, Maskarinec G (2011) Mammographic density and risk of breast cancer by adiposity: an analysis of four case–control studies. Int J Cancer. doi:10.1002/ijc.26205
Boyd NF, Martin LJ, Sun L, Guo H, Chiarelli A, Hislop G, Yaffe M, Minkin S (2006) Body size, mammographic density and breast cancer risk. Cancer Epidemiol Biomark Prev 15(11):2086–2092
Martin LJ, Minkin S, Boyd NF (2009) Hormone therapy, mammographic density, and breast cancer risk. Maturitas 64(1):20–26
Boyd NF, Martin LJ, Li Q, Sun L, Chiarelli AM, Hislop G, Yaffe MJ, Minkin S (2006) Mammographic density as a surrogate marker for the effects of hormone therapy on risk of breast cancer. Cancer Epidemiol Biomark Prev 15(5):961–966
Kerlikowske K, Cook AJ, Buist DS, Cummings SR, Vachon C, Vacek P, Miglioretti DL (2010) Breast cancer risk by breast density, menopause, and postmenopausal hormone therapy use. J Clin Oncol 28(24):3830–3837
Cuzick J, Warwick J, Pinney E, Duffy SW, Cawthorn S, Howell A, Forbes JF, Warren RM (2011) Tamoxifen-induced reduction in mammographic density and breast cancer risk reduction: a nested case–control study. J Natl Cancer Inst 103(9):744–752
van Gils CH, Hendriks JH, Otten JD, Holland R, Verbeek AL (2000) Parity and mammographic breast density in relation to breast cancer risk: indication of interaction. Eur J Cancer Prev 9(2):105–111
Nechuta S, Paneth N, Velie EM (2010) Pregnancy characteristics and maternal breast cancer risk: a review of the epidemiologic literature. Cancer Causes Control 21(7):967–989
Albrektsen G, Heuch I, Hansen S, Kvale G (2005) Breast cancer risk by age at birth, time since birth and time intervals between births: exploring interaction effects. Br J Cancer 92(1):167–175
Collaborative Group on Hormonal Factors in Breast Cancer (2002) Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet 360(9328):187–195
Wu AH, Ursin G, Koh WP, Wang R, Yuan JM, Khoo KS, Yu MC (2008) Green tea, soy, and mammographic density in Singapore Chinese women. Cancer Epidemiol Biomark Prev 17(12):3358–3365
Boyd N, Martin L, Gunasekara A, Melnichouk O, Maudsley G, Peressotti C, Yaffe M, Minkin S (2009) Mammographic density and breast cancer risk: evaluation of a novel method of measuring breast tissue volumes. Cancer Epidemiol Biomark Prev 18(6):1754–1762
Haars G, van Noord PA, van Gils CH, Grobbee DE, Peeters PH (2005) Measurements of breast density: no ratio for a ratio. Cancer Epidemiol Biomark Prev 14(11 Pt 1):2634–2640
Warren R, Skinner J, Sala E, Denton E, Dowsett M, Folkerd E, Healey CS, Dunning A, Doody D, Ponder B, Luben RN, Day NE, Easton D (2006) Associations among mammographic density, circulating sex hormones, and polymorphisms in sex hormone metabolism genes in postmenopausal women. Cancer Epidemiol Biomark Prev 15(8):1502–1508
Stone J, Warren RM, Pinney E, Warwick J, Cuzick J (2009) Determinants of percentage and area measures of mammographic density. Am J Epidemiol 170(12):1571–1578
Samimi G, Colditz GA, Baer HJ, Tamimi RM (2008) Measures of energy balance and mammographic density in the Nurses’ Health Study. Breast Cancer Res Treat 109(1):113–122
Mackinnon DP, Fairchild AJ, Fritz MS (2007) Mediation analysis. Annu Rev Psychol 58:593–614
Byng JW, Boyd NF, Fishell E, Jong RA, Yaffe MJ (1994) The quantitative analysis of mammographic densities. Phys Med Biol 39(10):1629–1638
Maskarinec G, Pagano I, Lurie G, Wilkens LR, Kolonel LN (2005) Mammographic density and breast cancer risk: the multiethnic cohort study. Am J Epidemiol 162(8):743–752
Ursin G, Ma H, Wu AH, Bernstein L, Salane M, Parisky YR, Astrahan M, Siozon CC, Pike MC (2003) Mammographic density and breast cancer in three ethnic groups. Cancer Epidemiol Biomark Prev 12(4):332–338
Vachon CM, Pankratz VS, Scott CG, Maloney SD, Ghosh K, Brandt KR, Milanese T, Carston MJ, Sellers TA (2007) Longitudinal trends in mammographic percent density and breast cancer risk. Cancer Epidemiol Biomark Prev 16(5):921–928
Nagata C, Matsubara T, Fujita H, Nagao Y, Shibuya C, Kashiki Y, Shimizu H (2005) Mammographic density and the risk of breast cancer in Japanese women. Br J Cancer 92(12):2102–2106
Byng JW, Boyd NF, Little L, Lockwood G, Fishell E, Jong RA, Yaffe MJ (1996) Symmetry of projection in the quantitative analysis of mammographic images. Eur J Cancer Prev 5(5):319–327
Desquilbet L, Mariotti F (2010) Dose–response analyses using restricted cubic spline functions in public health research. Stat Med 29(9):1037–1057
Szklo M, Nieto FJ (2000) Epidemiology: beyond the basics. Aspen Publishers, Gaithersburg
Russo J, Hu YF, Yang X, Russo IH (2000) Developmental, cellular, and molecular basis of human breast cancer. J Natl Cancer Inst Monogr 2000(27):17–37
Li T, Sun L, Miller N, Nicklee T, Woo J, Hulse-Smith L, Tsao MS, Khokha R, Martin L, Boyd N (2005) The association of measured breast tissue characteristics with mammographic density and other risk factors for breast cancer. Cancer Epidemiol Biomark Prev 14(2):343–349
Balogh GA, Heulings R, Mailo DA, Russo PA, Sheriff F, Russo IH, Moral R, Russo J (2006) Genomic signature induced by pregnancy in the human breast. Int J Oncol 28(2):399–410
Medina D (2005) Mammary developmental fate and breast cancer risk. Endocr Relat Cancer 12(3):483–495
Tamburrini AL, Woolcott CG, Boyd NF, Yaffe MJ, Terry T, Yasui Y, Jones CA, Patten SB, Courneya KS, Friedenreich CM (2010) Associations between mammographic density and serum and dietary cholesterol. Breast Cancer Res Treat 125(1):181–189
Hafeman D (2009) “Proportion explained”: a causal interpretation for standard measures of indirect effect. Am J Epidemiol 170(11):1443–1448
Vacek PM, Geller BM (2004) A prospective study of breast cancer risk using routine mammographic breast density measurements. Cancer Epidemiol Biomark Prev 13(5):715–722
Jakes RW, Duffy SW, Ng FC, Gao F, Ng EH (2000) Mammographic parenchymal patterns and risk of breast cancer at and after a prevalence screen in Singaporean women. Int J Epidemiol 29(1):11–19
Tice JA, Cummings SR, Ziv E, Kerlikowske K (2005) Mammographic breast density and the Gail model for breast cancer risk prediction in a screening population. Breast Cancer Res Treat 94(2):115–122
Ma H, Luo J, Press MF, Wang Y, Bernstein L, Ursin G (2009) Is there a difference in the association between percent mammographic density and subtypes of breast cancer? Luminal A and triple-negative breast cancer. Cancer Epidemiol Biomark Prev 18(2):479–485
Ma H, Bernstein L, Pike MC, Ursin G (2006) Reproductive factors and breast cancer risk according to joint estrogen and progesterone receptor status: a meta-analysis of epidemiological studies. Breast Cancer Res 8(4):R43
Yang XR, Chang-Claude J, Goode EL, Couch FJ, Nevanlinna H, Milne RL et al (2011) Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst 103(3):250–263
Dearth RK, Delgado DA, Hiney JK, Pathiraja T, Oesterreich S, Medina D, Dees WL, Lee AV (2010) Parity-induced decrease in systemic growth hormone alters mammary gland signaling: a potential role in pregnancy protection from breast cancer. Cancer Prev Res (Phila) 3(3):312–321
Schedin P (2006) Pregnancy-associated breast cancer and metastasis. Nat Rev Cancer 6(4):281–291
Ghosh K, Brandt KR, Reynolds CA (2009) Histologic markers of mammographic breast density: core-needle biopsy tissue from healthy volunteers. Cancer Res 69(Suppl 2):263S
Wiseman BS, Werb Z (2002) Stromal effects on mammary gland development and breast cancer. Science 296(5570):1046–1049
Passaperuma K, Warner E, Hill KA, Gunasekara A, Yaffe MJ (2010) Is mammographic breast density a breast cancer risk factor in women with BRCA mutations? J Clin Oncol 28(23):3779–3783
Kotsuma Y, Tamaki Y, Nishimura T, Tsubai M, Ueda S, Shimazu K, Jin Kim S, Miyoshi Y, Tanji Y, Taguchi T, Noguchi S (2007) Quantitative assessment of mammographic density and breast cancer risk for Japanese women. Breast 17(1):27–35
Duffy SW, Jakes RW, Ng FC, Gao F (2004) Interaction of dense breast patterns with other breast cancer risk factors in a case–control study. Br J Cancer 91(2):233–236
Tice JA, Cummings SR, Smith-Bindman R, Ichikawa L, Barlow WE, Kerlikowske K (2008) Using clinical factors and mammographic breast density to estimate breast cancer risk: development and validation of a new predictive model. Ann Intern Med 148(5):337–347
Chen J, Pee D, Ayyagari R, Graubard B, Schairer C, Byrne C, Benichou J, Gail MH (2006) Projecting absolute invasive breast cancer risk in white women with a model that includes mammographic density. J Natl Cancer Inst 98(17):1215–1226
Acknowledgments
This research was supported by the National Cancer Institute, the US Department of Health and Human Services, grant number R03 CA 135699. CGW and SMC were supported for the completion of the study on this project through postdoctoral fellowships on grant number R25 CA 90956.
Conflict of Interest
Dr. Martin Yaffe is one of the founders of Matakina Technology, a manufacturer of software for the assessment of mammographic density. However, the software was not used in the present research, and neither the results nor the way the research was conducted has been influenced by Dr. Yaffe’s involvement in Matakina Technology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Woolcott, C.G., Koga, K., Conroy, S.M. et al. Mammographic density, parity and age at first birth, and risk of breast cancer: an analysis of four case–control studies. Breast Cancer Res Treat 132, 1163–1171 (2012). https://doi.org/10.1007/s10549-011-1929-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1929-9