Abstract
Animal models have demonstrated the critical role of bone marrow-derived VEGFR1+ hematopoietic progenitor cells (HPCs) and VEGFR2+ endothelial progenitor cells (EPCs) in metastatic progression. We explored whether these cells could predict relapse and response in breast cancer (BC) patients. One hundred and thirty-two patients with stages 1–4 BC were enrolled on 2 studies. Circulating CD45+/CD34+/VEGFR1+ HPCs and CD45dim/CD133+/VEGFR2+ EPCs were assessed from peripheral blood mononuclear cells using flow cytometry. Changes in HPCs and EPCs were analyzed in (1) patients without overt disease that relapsed and (2) metastatic patients according to response by RECIST. At study entry, 102 patients were without evidence of disease and 30 patients had metastatic BC. Seven patients without evidence of BC by exam, labs, and imaging developed recurrence while on study. Median HPC/ml (range) increased from 645.8 (23.5–1,914) to 2,899 (1,176–37,336), P = 0.016, followed by an increase in median EPC/ml from 21.3 (4.7–42.5) to 94.7 (28.2–201.3), P = 0.016, prior to clinical relapse. In metastatic patients with progressive disease, median HPC/ml increased from 1,696 (10–16,470) to 5,124 (374–77,605), P = 0.0009, and median EPC/ml increased from 26 (0–560) to 71 (0–615) prior to progression, P = 0.10. In patients with responding disease, median HPC/ml decreased from 6,147 (912–85,070) to 633 (47–18,065), P = 0.05, and EPC/ml decreased from 46 (0–197) to 23 (0–105), P = 0.41, at response. There were no significant changes in these cells over time in patients with stable disease. Circulating bone marrow-derived HPCs and EPCs predict relapse and disease progression in BC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer remains the most commonly diagnosed cancer among women and the second leading cause of cancer mortality in the United States [1]. Despite major advances in adjuvant therapy for early stage breast cancer, patients still have a 20–50% chance of relapse over 10 years [2]. Metastasis, the final step of cancer progression, is responsible for most cancer-related deaths and may occur after an extraordinarily long period of time after initial diagnosis and treatment [3, 4]. Traditionally, probability of metastases has been correlated with tumor size and nodal status in breast cancer, but recent data suggest that molecular subtype may ultimately trump all traditional prognostic factors with the basal and HER2/neu intrinsic subtypes having the worst prognosis [5–8]. Though great strides have been made in delineating risk factors associated with recurrence, a reliable test to herald a clinical relapse does not exist. Several serum-based tumor markers are available in clinical practice for breast cancer; however, a clinical intervention when a tumor marker becomes newly abnormal is usually too late to prevent an impending relapse. Therefore, American Society of Clinical Oncology (ASCO) guidelines do not recommend routine screening with tumor markers in adjuvant breast cancer patients [9].
It is well established that tumor angiogenesis, the process of new blood vessel formation from preexisting vasculature, as well as differentiation and migration of endothelial cells, plays a crucial role in the growth and metastasis of tumors [10, 11]. However, less is known regarding the mechanisms that allow the transition from dormant, or occult, cancer cells to overt clinical relapse in cancer patients. Emerging evidence from preclinical models suggests that tumor-derived signals stimulate the quiescent bone marrow compartment, resulting in the expansion and mobilization of bone marrow-derived (BMD) VEGFR1+ hematopoietic progenitor cells (HPCs) and VEGFR2+ endothelial progenitor cells (EPCs), among others. HPCs home to the target organ and form clusters, or premetastatic niches, providing a permissive local microenvironment for the recruitment of incoming tumor cells and the establishment of micrometastases. EPCs are then recruited to the periphery of the micrometastatic lesions where they modulate the angiogenic switch, the transition from avascular micrometastatic lesions to vascularized macrometastatic disease. In these murine models, inhibition of VEGFR1+ significantly reduces HPC localization to the premetastatic niche and development of metastasis. Similarly, blocking EPC mobilization strongly inhibits vasculogenesis and impairs the formation of macrometastases [12–14].
The contribution of HPCs and EPCs to human cancer progression and pathogenesis is less well understood. HPCs have been implicated in defining the premetastatic niche in axillary lymph nodes of breast cancer patients and pelvic lymph nodes of prostate cancer patients [13, 15]. Elevated EPCs have been observed in cancer patients versus healthy controls [16]. EPCs have been also associated with advanced stage and worse prognosis in several hematologic and solid malignancies, and some but not all breast cancer studies [17–23].
Based on the preclinical data characterizing the angiogenic switch in murine model systems, we designed a study to characterize the angiogenic switch in a breast cancer population. We analyzed the temporal relationship of HPCs and EPCs in a series of breast cancer patients at high risk of recurrence based on traditional clinicopathologic factors. Furthermore, we explored whether quantitative changes in these cells could predict response to therapy in a well-annotated cohort of breast cancer patients receiving systemic therapy for advanced disease.
Materials and methods
Patients with breast cancer were enrolled on one of the two Institutional Review Board approved studies at Weill Cornell Medical College (WCMC) Iris Cantor Breast Cancer Center. Written informed consent was obtained in accordance with the Declaration of Helsinki.
Study population and design
Study 1
Patients with pathologically confirmed stage 1–4 invasive breast cancer were recruited from WCMC Iris Cantor Breast Cancer Center from March 2005 to July 2009 and divided into 2 cohorts:
Cohort 1: Patients with stage 1–3 breast cancer were enrolled following definitive surgery (lumpectomy and axillary evaluation or mastectomy) and prior to the initiation of adjuvant systemic therapy. Adjuvant systemic therapy was based on physician’s choice and could consist of the following: chemotherapy, hormonal therapy, biologic and/or radiation therapy. Clinical specimens were obtained at the initiation of systemic therapy, halfway through systemic chemotherapy and every 3 months at routine follow-up thereafter.
Cohort 2: Patients with stage 4 breast cancer with established metastasis or with presentation of newly diagnosed stage 4 disease (de novo stage 4 breast cancer) were enrolled upon starting a new systemic therapy. Clinical specimens were obtained monthly and coincident with an imaging scan to assess response to therapy.
Study 2
Patients without evidence of breast cancer but at high risk of relapse with pathologically confirmed stage 2 or greater triple-negative breast cancer and any subtype of stage 3 or stage 4 breast cancer with no evidence of disease (stage 4 NED) were enrolled on a phase II trial of tetrathiomolybdate, a copper depletion compound at WCMC Iris Cantor Breast Cancer Center (NCT00195091, 0903-882) from July 2007 to June 2010. In this trial, clinical specimens were obtained on a monthly basis for up to 2 years.
Clinical response
Response was based on Response Evaluation Criteria in Solid Tumors (RECIST) [24]. Patients with progressive disease (PD) comprised the “progression of disease” group. Patients with complete response (CR) or partial response (PR) comprised the “responding disease” group. Patients with stable disease (SD) comprised the “stable disease” group.
HPC and EPC quantitation
Blood samples were obtained prior to chemotherapy administration. Ten to 20 ml of venous blood was collected in EDTA-containing tubes and processed within 12 h. Laboratory evaluation of specimens in both studies was identical. Peripheral blood mononuclear cells were isolated by Ficoll density-gradient centrifugation. To quantitate circulating EPCs, cells were stained with CD133-PE (Miltenyi Biotec, Auburn, CA), VEGFR2-APC (R&D Systems, Minneapolis, MN), and CD45-PerCP (BD Biosciences, Franklin Lakes, NJ). To quantitate HPCs, cells were stained with CD34-FITC (BD Biosciences), VEGFR1-APC (R&D Systems), and CD45-PerCP (BD Biosciences). An aliquot of cells was also stained with the appropriate isotype controls (mouse anti-human IgG1k). Samples were analyzed using a FACSCalibur flow cytometer (Bectin Dickinson, San Jose, CA). Three hundred thousand events were collected in the nucleated cell gate (excludes debris and platelets). Data analysis was done using FlowJo software (FlowJo, Ashland, OR). A series of consecutive gates were made to include and exclude acquired events to quantitate specific populations such as CD45+, CD34+, VEGFR1+. The number of EPCs and HPCs per ml of blood was calculated as follows: HPC/ml = (# HPC events/# lymphocyte events) X absolute lymphocyte count (lymphocytes/ml). EPC/ml = (# EPC events/# lymphocyte events) X absolute lymphocyte count (lymphocytes/ml). See supplemental data for detailed gating strategy.
Definition of HPCs and EPCs
The definition of HPCs and EPCs was based on the phenotypes used by Bertolini et al. [25, 26]. HPCs were defined as CD45+, CD34+, VEGFR1+. EPCs were defined as CD45dim, CD133+, VEGFR2+.
Statistical analysis
All analyses were performed in GraphPad Prism version 5.0 (GraphPad Software, La Jolla, CA). Since the methods and endpoint of both studies were identical, the results of the studies were combined to test the following hypotheses: (1) circulating bone marrow-derived progenitor cells predict progression of disease or responding disease in metastatic breast cancer patients receiving systemic chemotherapy and (2) circulating bone marrow-derived progenitor cells predict relapse in breast cancer patients with stage 4 NED (no evidence of disease). Results were expressed as medians and range. In metastatic patients, baseline was defined as initiation of a new systemic therapy, and comparisons between baseline and postresponse HPC and EPC values were made with the Wilcoxon signed-rank test. Comparisons between baseline and postresponse absolute lymphocyte values were made with standard paired t test. In the patients who relapsed from a prior no evidence of disease state, baseline was defined as median of EPC and HPC values prior to EPC or HPC surge, and comparisons between baseline and “prior to relapse” were made with the Wilcoxon signed-rank test. All P values were two sided with statistical significance evaluated at the 0.05 alpha level.
Results
One hundred and thirty-two patients were enrolled on two studies (Fig. 1). Data from both studies were combined to analyze patients who entered the study without overt breast cancer and developed recurrence while on study (“relapsed group”: Study 1 [observational study]/Cohort 1 and Study 2 [TM trial]). Patients with stage 4 breast cancer were grouped according to response by RECIST (Study 1/Cohort 2). Demographic variables are shown in Table 1.
This schema represents the 2 studies from which the observations are pooled. Study 1 contained 2 cohorts of breast cancer patients (stages 1–3 and metastatic patients), while Study 2 represents stage 2–4 breast cancer patients without evidence of disease but at high risk of relapse. Abbreviations: BC breast cancer, NED no evidence of disease, n number of patients, t number of treatment cycles, TM tetrathiomolybdate, aPatients may have had more than 1 response throughout study, b1 patient rendered NED with therapy then relapsed, thereafter comprising the “relapsed” group, c4 pts evaluable
Of the 102 patients, who at study entry were without evidence of disease by physical examination, laboratory data, tumor markers, or imaging, 10 patients developed overt breast cancer recurrence while on study. Three patients relapsed 1–2 months after study entry and were not included in the analysis. Of the seven evaluable patients, 3 were from Study 1 and 4 from Study 2. Four patients had stage 4 breast cancer without any evidence of disease (2 were estrogen receptor [ER] positive, 1 was HER2/neu positive, and 1 was triple-negative), 2 patients had a prior diagnosis of stage 3C breast cancer (ER-positive and triple-negative), and 1 patient had a prior diagnosis of stage 2 breast cancer (triple-negative). The median primary tumor size was 3 cm (range 1.7–4.3 cm), and number of positive lymph nodes involved was 1 (range 1–42).
Incremental rise in VEGFR1+ HPCs and VEGFR2+ EPCs predicts relapse in patients with breast cancer who have no evidence of disease
In the 7 patients who developed relapse without prior evidence of disease, the median HPC/ml increased from baseline of 645.8 (range 23.5–1,914) to 2,899 (range 1,176–37,336) prior to relapse, P = 0.016 (Fig. 2a). Similarly, median EPC/ml increased from baseline of 21.3 (range 4.7–42.5) to 94.7 (range 28.2–201.3) immediately prior to relapse P = 0.016 (Fig. 2b).
In the 4 patients on Study 2, 3 patients had monthly specimens enabling a look at the temporal relation of HPCs and EPCs prior to relapse. In all 3 patients, an identical pattern in the progenitor cells emerged which heralded a relapse of breast cancer. An initial surge followed by a decline in HPCs and subsequent increase in EPCs preceded an overt recurrence (Fig. 3). In these patients, the median time between a surge in HPCs and EPCs prior to overt relapse was 6 months (range 4–8) and 1 month (range 1–2), respectively. Because the surge antedating relapse is between 4 and 8 months, the 3 patients who relapsed within 2 months of study entry were actively relapsing at that time, hence were excluded from this analysis.
Characteristic pattern of VEGFR1+ and VEGFR2+ hemangiogenic progenitor cells is observed prior to relapse of breast cancer who are without evidence of disease at study entry, that is, an initial surge of the VEGFR1+ HPCs is followed by a surge of the VEGFR2+ EPCs prior to overt relapse. Median values of baseline, HPC surge, EPC surge, and at relapse of relapsed patients (n = 3) are shown here. Parenthesis, range in months prior to overt relapse
Incremental rise in VEGFR1+ HPCs and VEGFR2+ EPCs predicts clinical progression of disease in patients with breast cancer who are undergoing systemic therapy
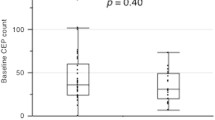
Thirty patients with stage 4 breast cancer were enrolled into Cohort 2 of Study 1 and underwent evaluation at the initiation of therapy and at 3, 4, or 6-week intervals over the course of 3 years and 40 treatment cycles. Eight patients were not included in the final analysis due to death prior to subsequent sample collection (4 patients) and loss to follow-up (4 patients). Since a normal range does not exist for bone marrow-derived progenitor cells, subsequent time points are required for comparison to baseline. Of the 22 evaluable patients, systemic treatment included chemotherapy alone (19 cycles), hormonal therapy (6 patients), and combinations of both with biologics (trastuzumab and/or lapatinib [11 patients], bevacizumab [2 patients], and dasatinib [2 patients]). HPCs and EPCs were analyzed in patients stratified by response as per RECIST (Table 2). Patients with progressive disease representing 20 treatment cycles had a significant increase in HPCs preceding overt progression compared to the baseline values at the start of a new treatment (Fig. 4a, b). Median HPC/ml increased from baseline of 1,696 (range 10–16,470) to 5,124 (range 374–77,605) prior to progression, P = 0.0009. Median EPC/ml increased from baseline of 26 (range 0–560) to 71 (range 0–615) prior to progression, P = 0.10. The median time between baseline and the increase in HPCs and EPCs was 7.5 weeks (range 4–88). There were no significant changes in these patients’ median absolute lymphocyte count (ALC)/μl after receiving chemotherapy, 1,255 (range 500–2,800) at baseline and 1,450 (range 470–3,460) after chemotherapy, P = 0.08.
Change in VEGFR1+ HPCs and VEGFR2+ EPCs from baseline to a subsequent time point stratified by response to therapy, as defined by a, b progression of disease, c, d responding disease, and e, f stable disease. 1 data point is outside the axis limits in (a, b) graphs and 2 in ( c, d ) graphs. Horizontal line, median values
Decrease in VEGFR1+ HPCs and VEGFR2+ EPCs predicts clinical response to systemic therapy
Eleven patients with breast cancer metastases representing 12 treatment cycles that were responding to systemic therapy had a reduction in median HPC and EPC values (Fig. 4c, d). Median HPC/ml decreased from baseline of 6,147 (range 912–85,070) to 633 (range 47–18,065) at response, P = 0.05. A trend was seen for decreased median EPC/ml; 46 (range 0–197) at baseline decreased to 23 (range 0–105) at response, P = 0.41. The median time between baseline and the decrease in HPCs and EPCs was 6 weeks (range 4–23). Median ALC/μl did not significantly change after chemotherapy in this group, 1,150 (range 600–3,400) at baseline and 1,250 (range 260–2,800) after chemotherapy, P = 0.53.
Five patients with clinically stable disease after 8 treatment cycles did not have a significant change in either progenitor cells from baseline to a posttreatment time point, (median 9 weeks, range 8.5–32.5) (Fig. 4e, f). HPC/ml remained stable at 1,309 (range 390–55,377) at baseline compared to 1,188 (range 135–20,690) at a posttreatment time point, P = 0.31. EPC/ml decreased from 78 (range 11–484) at baseline to 29 (range 9–331) at a posttreatment time point, though this did not reach statistical significance, P = 0.15. Similarly, median ALC/μl did not significantly change: 1,235 (range 1,000–2,300) to 1,450 (720–2,300), P = 0.7.
Discussion
Understanding the metastatic process is critical in eradicating cancer deaths. In this prospective study, we begin to gather insight into the terminal events leading to the development of overt metastases in well-defined cohorts of breast cancer patients. We have demonstrated a substantial increase in the VEGFR1+ HPCs months before relapse followed by a surge in the VEGFR2+ EPCs immediately preceding an overt relapse of cancer. We postulate that the surge of HPCs in advance of the arrival of circulating EPCs represents initiation of the premetastatic niche, and an overt relapse occurs after EPCs “turn on” the angiogenic switch. This characteristic pattern was observed in patients without objective evidence of disease that relapsed as well as patients with established metastasis who progressed on therapy. In the 92 patients without evidence of disease who remained relapse-free throughout the study, this pattern in HPCs and EPCs was not observed. We believe these observations confirm the preclinical models of metastases in breast cancer patients.
Furthermore, levels of circulating HPCs in patients with overt clinical metastases predicted therapeutic response. The change in HPCs was most significant in treatment-refractory tumors (progression of disease group) suggesting that active tumor neoangiogenesis is being driven by these cells. In fact, immediately prior to a patient’s death, the levels of HPCs in addition to EPCs were several-fold higher than at any time earlier in their treatment course. In treatment-sensitive tumors (responding disease group), a significant reduction in HPCs was observed with therapy. The absolute lymphocyte count in these patients remained stable during treatment; therefore, it is unlikely that the marrow suppressive effects of the chemotherapy contributed to the decrease in HPCs observed. A significant change in EPCs did not occur in either group, although there was a trend for increased EPCs in the progression of disease group and decreased EPCs in the responding group. This could be due to timing of the specimen as the angiogenic switch is a dynamic process, and a subsequent examination of EPCs even a week later may have revealed a further change that reached statistical significance. It is unclear whether chemotherapy-induced EPC mobilization, described in mouse models and human patients, may have contributed [27, 28]. Taken together, we postulate that the change in HPCs might be the more robust marker to monitor for therapeutic response. Finally, as expected with the current model, in patients with disease that remained stable on therapy, there were no significant changes in either HPCs or EPCs.
It is important to acknowledge the difficulties in analyzing these progenitor cells. The lack of a consensus in defining the HPC and EPC phenotype or the optimal method to assay these cells may impact accurate quantification. The rarity of these cells in the peripheral circulation, constituting less than 0.0001–0.01% of peripheral circulating mononuclear cells, further underscores this difficulty [29]. EPC levels may be affected by several factors including medications, growth factors, and common comorbidities such as cardiovascular disease [30, 31]. Our data set is heavily annotated and controlled for these variables. Moreover, our study (and data from an ongoing unpublished study) suggests that the relationship between these two distinct populations of BMD progenitor cells might be more important than the absolute values.
There is a potential advantage for the use of HPCs and EPCs as a clinical biomarker over the use of existing serum-based biomarkers (e.g., CEA and CA15-3), as the latter probably does not predict relapse early in the metastatic process and is a relatively late-stage event. In our study, 9 of 14 patients in both the progression of disease and relapsed cohorts had an elevation of a tumor marker at least 2 months after the surge in HPCs. Conceivably, this change in BMD progenitor cells might represent a sufficiently early step in metastatic progression that allows for the opportunity to intervene with targeted therapy to promote the maintenance of tumor dormancy and prevention of relapse or progression.
Several novel agents targeting BMD cells have been introduced into the clinical arena with promising data including cediranib, (pan-VEGFR inhibitor), ramucirumab (IMC-1121B, anti-VEGFR2 antibody) and IMC-18F1 (anti-VEGFR1 antibody) [32–34]. Finally, Study 2 described here is an ongoing phase II clinical trial of an anti-angiogenic copper depletion compound, which is attempting to modulate the angiogenic switch through copper-dependent mechanisms, in high risk for relapse breast cancer patients. We observed that patients who became adequately copper-depleted had a significant reduction in EPCs from baseline [35]. A clinical trial investigating ramucirumab and IMC-18F1 in combination with capecitabine in women with metastatic breast cancer is underway and is expected to shed much insight into the role of these BMD progenitor cells and the effect of targeted therapy on outcome (ClinicalTrials.gov identifier: NCT01234402).
This is the first study to offer insight into the angiogenic switch in vivo, specifically in de novo relapse and progression of breast cancer metastases. Circulating HPCs and EPCs may serve as a biomarker to predict relapse or disease progression, as well as serve as a promising therapeutic target in those at high risk of relapse. We acknowledge that the sample size was small, and the data are an aggregate of two studies. Future avenues of research include a larger study to further define the temporal relationship and effect of different therapies on these cells.
References
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60:277–300
Brewster AM, Hortobagyi GN, Broglio KR et al (2008) Residual risk of breast cancer recurrence 5 years after adjuvant therapy. J Natl Cancer Inst 100:1179–1183
Chiang AC, Massague J (2008) Molecular basis of metastasis. N Engl J Med 359:2814–2823
Saphner T, Tormey DC, Gray R (1996) Annual hazard rates of recurrence for breast cancer after primary therapy. J Clin Oncol 14:2738–2746
Perou CM, Sorlie T, Eisen MB et al (2000) Molecular portraits of human breast tumours. Nature 406:747–752
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874
Sorlie T, Tibshirani R, Parker J et al (2003) Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 100:8418–8423
Cheang MC, van de Rijn M, Nielsen TO (2008) Gene expression profiling of breast cancer. Annu Rev Pathol 3:67–97
Harris L, Fritsche H, Mennel R et al (2007) American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol 25:5287–5312
Folkman J (1971) Tumor angiogenesis: therapeutic implications. N Engl J Med 285:1182–1186
Carmeliet P, Jain RK (2000) Angiogenesis in cancer and other diseases. Nature 407:249–257
Lyden D, Hattori K, Dias S et al (2001) Impaired recruitment of bone marrow derived endothelial and a hematopoietic precursor cells blocks tumor angiogenesis and growth. Nat Med 7:1194–1201
Kaplan RN, Riba RD, Zacharoulis S et al (2005) VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature 438:820–827
Gao D, Nolan DJ, Mellick AS, Bambino K, McDonnell K, Mittal V (2008) Endothelial progenitor cells control the angiogenic switch in mouse lung metastasis. Science 319:195–198
Fujita K, Nakayama M, Nakai Y et al (2009) Vascular endothelial growth factor receptor 1 expression in pelvic lymph nodes predicts the risk of cancer progression after radical prostatectomy. Cancer Sci 100:1047–1050
Taylor M, Rossler J, Geoerger B et al (2009) High levels of circulating VEGFR2+ Bone marrow-derived progenitor cells correlate with metastatic disease in patients with pediatric solid malignancies. Clin Cancer Res 15:4561–4571
Gao D, Mittal V (2009) The role of bone-marrow-derived cells in tumor growth, metastasis initiation and progression. Trends Mol Med 15:333–343
Roodhart JM, Langenberg MH, Daenen LG, Voest EE (2009) Translating preclinical findings of (endothelial) progenitor cell mobilization into the clinic; from bedside to bench and back. Biochim Biophys Acta 1796:41–49
Dome B, Timar J, Dobos J et al (2006) Identification and clinical significance of circulating endothelial progenitor cells in human non-small cell lung cancer. Cancer Res 66:7341–7347
Furstenberger G, von Moos R, Lucas R et al (2006) Circulating endothelial cells and angiogenic serum factors during neoadjuvant chemotherapy of primary breast cancer. Br J Cancer 94:524–531
Massa M, Rosti V, Ramajoli I et al (2005) Circulating CD34+, CD133+, and vascular endothelial growth factor receptor 2-positive endothelial progenitor cells in myelofibrosis with myeloid metaplasia. J Clin Oncol 23:5688–5695
Richter-Ehrenstein C, Rentzsch J, Runkel S, Schneider A, Schonfelder G (2007) Endothelial progenitor cells in breast cancer patients. Breast Cancer Res Treat 106:343–349
Naik RP, Jin D, Chuang E et al (2008) Circulating endothelial progenitor cells correlate to stage in patients with invasive breast cancer. Breast Cancer Res Treat 107:133–138
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Bertolini F, Shaked Y, Mancuso P, Kerbel RS (2006) The multifaceted circulating endothelial cell in cancer: towards marker and target identification. Nat Rev Cancer 6:835–845
Mancuso P, Antoniotti P, Quarna J et al (2009) Validation of a standardized method for enumerating circulating endothelial cells and progenitors: flow cytometry and molecular and ultrastructural analyses. Clin Cancer Res 15:267–273
Shaked Y, Henke E, Roodhart JM et al (2008) Rapid chemotherapy-induced acute endothelial progenitor cell mobilization: implications for antiangiogenic drugs as chemosensitizing agents. Cancer Cell 14:263–273
Farace F, Massard C, Borghi E, Bidart JM, Soria JC (2007) Vascular disrupting therapy-induced mobilization of circulating endothelial progenitor cells. Ann Oncol 18:1421–1422
Khan SS, Solomon MA, McCoy JP Jr (2005) Detection of circulating endothelial cells and endothelial progenitor cells by flow cytometry. Cytometry B Clin Cytom 64:1–8
Bahlmann FH, De Groot K, Spandau JM et al (2004) Erythropoietin regulates endothelial progenitor cells. Blood 103:921–926
Friedrich EB, Werner C, Walenta K, Bohm M, Scheller B (2009) Role of extracellular signal-regulated kinase for endothelial progenitor cell dysfunction in coronary artery disease. Basic Res Cardiol 104:613–620
Goss GD, Arnold A, Shepherd FA et al (2010) Randomized, double-blind trial of carboplatin and paclitaxel with either daily oral cediranib or placebo in advanced non-small-cell lung cancer: NCIC clinical trials group BR24 study. J Clin Oncol 28:49–55
Spratlin JL, Cohen RB, Eadens M et al (2010) Phase I pharmacologic and biologic study of ramucirumab (IMC-1121B), a fully human immunoglobulin G1 monoclonal antibody targeting the vascular endothelial growth factor receptor-2. J Clin Oncol 28:780–787
Schwartz JD, Rowinsky EK, Youssoufian H, Pytowski B, Wu Y (2010) Vascular endothelial growth factor receptor-1 in human cancer: concise review and rationale for development of IMC-18F1 (Human antibody targeting vascular endothelial growth factor receptor-1). Cancer 116:1027–1032
Jain S, Ward M, Chuang E, Cigler T, Moore A, Donovan D et al (2010) The effect of tetrathiomolybdate (TM) on circulating endothelial progenitor cells in women at moderate to high risk of breast cancer recurrence. Proc Breast Cancer Symp; abstr 297
Acknowledgments
We greatly appreciate the generous support from the following: Anne Moore Breast Cancer Research Fund, Stephen and Madeline Anbinder Foundation, Rozaliya Kosmandel Research Fund, Susan G Komen for the Cure, New York Community Trust, and Cancer Research and Treatment Fund. We would also like to thank the Weill Cornell Translational Core Laboratory, Rakhi Naik, MD for her initial contribution to the design of Study 1, and Dingchen Gao and Raul Catena for their valuable comments on this manuscript. Dr. Paul Christos was partially supported by the following grant: Clinical Translational Science Center (CTSC) (UL1-RR024996).
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jain, S., Ward, M.M., O’Loughlin, J. et al. Incremental increase in VEGFR1+ hematopoietic progenitor cells and VEGFR2+ endothelial progenitor cells predicts relapse and lack of tumor response in breast cancer patients. Breast Cancer Res Treat 132, 235–242 (2012). https://doi.org/10.1007/s10549-011-1906-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1906-3