Abstract
There has been a 28% reduction in age-standardised breast cancer mortality in Australia since 1991 when the free national mammographic program (BreastScreen) began. Therefore, a comparative study between BreastScreen participation and breast cancer age specific mortality trends in Australia was undertaken for two time periods between 1991 and 2007, where women aged 50–59 and 60–69 years, who were invited to screen, were compared to women aged 40–49 and 70–79 years who were not invited, but who did have access to the program. There were mortality reductions in all four age groups between 1991–1992 and 2007, resulting in 5,849 (95% CI 4,979 to 6,718) fewer women dying of breast cancer than would have otherwise been the case. Women aged 40–49 years, who had the lowest BreastScreen participation (approximately 20%), had the largest mortality reduction: 44% (95% CI 34.8–51.2). Women aged 60–69 years, who had the highest BreastScreen participation (approximately 60%), had the smallest mortality reduction: 19% (95% CI 10.5–26.9). As BreastScreen participation by invited women aged 50–69 years only reached a maximum of about 55–60% in 1998–1999, a decline in mortality in Australian women cannot be attributed to BreastScreen prior to this time. Thus, almost 60% of the Australian decline in breast cancer mortality since 1991 cannot be attributed to BreastScreen. Therefore, mammographic screening cannot account for most of the reductions in breast cancer mortality that have occurred in Australian women since 1991 and may have contributed to over-diagnosis. Most, if not all, of the reductions can be attributed to the adjuvant hormonal and chemotherapy, which Australian women have increasingly received since 1986.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Australian Government launched a national free mammography screening program for women aged 40 or more years in 1991, the BreastScreen Australia program, following a review of the Swedish and other mammography screening trials [1] BreastScreen specifically targeted 50–69-year-old women by identifying them from the electoral roll and inviting them by letter to have a screening mammogram every 2 years [1–3]. Women aged 40–49 and 70 years or older could request and obtain a screening mammogram [1–3]. The Australian Institute of Health and Welfare (AIHW), which compiles and reports the national screening data [2], stated in 2006 that “A particularly important indication of the effectiveness of a screening program is the change in mortality rates over time in the target age group for screening” [4]. Therefore, our report analyses changes in breast cancer age specific mortality rates between 1991 and 2007 in women aged 40–79 years, during which period age-standardised (2001 Australian standard population) breast cancer mortality rates for all women fell from 31.1 to 22·1 per 100,000, a 28% reduction [2, 5].
Methods
The analyses presented in this report are based on comparisons of screening participation with crude cancer incidence and mortality rates between women in the screening target age range 50–69 years, and those in women aged 40–49 and 70–79 years, respectively, who are eligible for free screening but are not specifically invited. We have contrasted the total study period (1991–1992 through to 2007) with the latter half of the study period (1999–2000 to 2007). This comparison was done because in the long term follow up of five of the six the Swedish randomised controlled screening trials of invitation to mammography versus no invitation, a cumulative breast cancer mortality benefit for women invited to screen only began to emerge after 4 years (for women aged 60–69 years) and after 6 years (for women aged 40–59 years). This delay before the emergence of the breast cancer mortality benefit was seen despite first round participation in these 5 Swedish randomised controlled screening trials of 74–89% of invited women [6]. BreastScreen participation by invited women aged 50–69 years reached a maximum of about 55–60% in 1998–1999, well short of the first round participation in the Swedish trials. Since reductions in mortality in those Swedish trials occurred 4–6 years after screening began, we allowed for a longer period before any effect of BreastScreen on mortality might have been expected.
All the data used in the analysis was aggregated and is available in the public domain, so no ethical approval or patient consent was required.
Data sources
National BreastScreen participation rates have been available since 1994 when the BreastScreen Australia Statistical Report for 1994 and 1995 was published [7]. The AIHW BreastScreen Australia monitoring reports contain the remaining participation data in our analyses [2, 3]. The BreastScreen participation counts are published as aggregations into 2-year periods, reflecting the program’s recommended screening interval. The proportions of Australian women in each age group having screening mammography outside of the BreastScreen program were estimated by using survey data published by the Australian Bureau of Statistics (ABS), as well as data obtained from Australia’s universal health insurance program (http://www.medicareaustralia.gov.au/) [2, 4].
Data on the incidence of invasive breast cancer in Australia are provided by the National Cancer Statistics Clearing House at the AIHW, and are reported in the AIHW “Cancer in Australia” series of reports [8]. Cancer incidence data are provided to the AIHW by cancer registries in each Australian State and Territory, and registration of cancer with State cancer registries is required under State and Territory legislation.
Data on mortality from breast cancer in Australia are reported in AIHW’s “Cancer in Australia” series and the General Record of Incidence of Mortality books, which contain the mortality data used in this study [5, 8]. Because 2008 mortality rates were not yet available, the last mortality period comprises only 2007 data.
Statistical analyses
Each of the incidence and mortality counts was also aggregated into 2-year periods to reduce the variability in the rate estimates and for consistency with the participation rates, except for the most recent mortality data for which only 2007 data was available.
Rate estimates and associated 95% confidence intervals were then calculated by dividing the counts by the sum of the mid-year population estimates for each of the 2 years, as published by the ABS. The relative mortality reduction between any two periods was calculated as the difference in the mortality rate between the two periods divided by the mortality rate for the first period. The absolute mortality reductions, as the extra number of women who would have died of breast cancer in 2007 if the 1991–1992 and 1999–2000 mortality rates had applied, were estimated by multiplying the absolute fall in mortality rates between each of these periods and 2007 by the 2007 population. The cumulative absolute mortality reduction from 1991 to 2007 for all women aged 40–79 years was calculated by multiplying their mortality rate difference between each 2 year period by the their population in the second period and summing across the periods.
Results
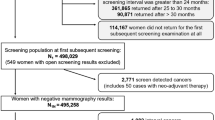
Population based mammographic screening began in two States (Western and South Australia) in 1989 and increased over the next 7 years as all States and Territories began participating in the national BreastScreen program, which began in 1991 [1, 3]. The national participation rates for the invited age group 50–69 years were first published for 1994–1995 (about 20%) and then reached a plateau of about 55–60% from 1998–1999 to 2006–2007; the full capacity BreastScreen program (Fig. 1). Participation rates for women aged 40–49 years reached a maximum of about one-third, and for women aged 70–79 years about one half, of those of the invited age group in this full capacity period.
Between 5 and 10% of Australian women aged 40–69 years are having mammographic screening outside Breast Screen [4, 9]. In 2001, 24% of women aged 40–49 years surveyed by the ABS reported that they had regular mammograms at least biennially, which is about 5% more than BreastScreen participation [4]. This survey also reported that 65 and 64% of 50–59 and 60–69-year-old women, respectively had regular mammograms at least biennially, which is 5–10% more than BreastScreen participation (Fig. 1). This is consistent with Medicare data, which shows that the rate of women having bilateral mammograms annually, which could be for diagnosis or screening, fell from about 43–33 per 1,000 women (4·3–3·3% of women) between 1993–1994 and 2007–2008, with most of the fall being between 1993–1994 and 1996–1997 when BreastScreen was increasing to full capacity [3].
The changes in breast cancer incidence in the four age groups over the same period, 1991–1992 to 2005–2006, are shown in Fig. 2. In 50–59-year-old women incidence rose significantly from 1991–1992 to a peak in 2001–2002 and then fell significantly to 2005–2006. In 70–79-year-old women incidence also rose significantly from 1991–1992 to a plateau from 1993–1994 to 2001–2001 and then fell significantly to 2005–2006. In contrast, whilst incidence rose significantly in 60–69-year-old women from 1991–1992 to peak in 2001–2002, it then remained on a plateau through 2005–2006. For the 40–49 year age group incidence was on a plateau from 1993–1994 through 2003–2004.
Significant and continuous falls in breast cancer mortality began in women aged 40–49 years in 1993–1994, and in women aged 50–59 and 70–79 years in 1995–1996. In contrast women aged 60–69 years had almost all of their mortality reduction between 1995–1996 and 1999–2000 (Fig. 3).
The corresponding relative reductions in mortality for women in these four age groups are shown in Fig. 4 for the complete study period (1991–1992 to 2007). The reduction in mortality for 40–49-year-old women, who were outside the targeted age range for screening mammography, 44% (95% CI 34.8–51.2), is significantly greater than that of 60–69-year-old women, 19% (95% CI 10.5–26.9), who were invited to screen (P < 0.05). The relative mortality reduction in each age group for the latter half of the study period (1999–2000 through to 2007) is also shown (Fig. 4). These data reveal that there was no significant relative mortality reduction in women aged 60–69 years in this period when BreastScreen could have had an effect. When the BreastScreen participation rates (Fig. 1) were correlated with either set of relative mortality reductions (Fig. 4), there was a no association between them.
The absolute mortality reductions in each age range are shown for both the full (1991–1992 to 2007) and latter half (1999–2000 to 2007) of the study period (Table 1), together with the population numbers in 2007. Based on the point estimates, 59% of the absolute reduction in mortality in women aged 40–79 years had occurred by 1999–2000. Furthermore, only one-third of the absolute reduction in mortality for the invited women aged 50–59 and 60–69 years combined occurred during the latter half of the study period when BreastScreen could have had an effect. Finally, as a consequence of the falls in breast cancer mortality rates over this 17 year period 5,849 (95% CI 4,979–6,718) fewer Australian women aged 40–70 years have died of breast cancer than would otherwise have been the case.
Discussion
Our analysis indicates that mammographic screening cannot account for most of the reduction in breast cancer mortality that has occurred in Australian women since 1991.
The significant increases in incidence of breast cancer in women aged 50–59, 60–69, and 70–79 years are evidence of screening mammography detecting asymptomatic (early) invasive breast cancers that may have subsequently presented when they became symptomatic. If a cancer screening program is functioning effectively, this rise in incidence is normally followed by a return to the previous incidence trend and also by a fall in mortality [10]. The failure of incidence to return to the previous trend in the 60–69-year-old age group is evidence of possible over-diagnosis of invasive breast cancer that would never have become symptomatic in these women [10]. The incidence trend in the 40–49 year age group is consistent with a level of screening that has not had any effect on the detection of breast cancer [10], and therefore would probably not have had an effect on mortality.
Mortality declines began in all age groups before 1999–2000 and most of the declines in the period 1991–1992 to 2007 occurred prior to 1999–2000, before BreastScreen would have been expected to affect mortality. Furthermore there has not been a greater reduction in relative or absolute mortality in the invited age groups: women 50–59 and 60–69 years, as compared with both younger and older women despite BreastScreen participation rates which are up to threefold greater in these invited age groups. In particular, there was no significant reduction in relative mortality in the invited women aged 60–69 years for the 8 years from 1999–2000 to 2007, when this age group had the highest BreastScreen participation rate (nearly 60%) and, on the basis of the long-term follow up of the Swedish randomised controlled screening trials [6], would have been expected to have had the greatest reduction.
These Swedish randomised controlled screening trials also provide the most relevant long term estimates of the possible effect on breast cancer mortality of an invitation to mammographic screening versus no invitation program and all but one had finished inviting and treating women by 1985 [6], before adjuvant hormonal and chemotherapy therapy was established practice [11]. In 1982–1987, 5-year survival from breast cancer in Australia for all women was 72.6% and 10-year survival was 60.7% and in 1988–1993, before BreastScreen could have had an impact, 5-year survival was 79.3% and 10-year survival was 70% [2]. By the time of the Australian national breast cancer treatment survey in 1995 [12], 5-year survival from breast cancer in Australia for all women had increased to 85.3% (1994–1999) and the 10-year survival to 77.8% [2] and most women diagnosed with early breast cancer were receiving appropriate adjuvant hormonal and chemotherapy as described by the Early Breast Cancer Trialists Collaborative Group (EBCTCG) [12, 13]. BreastScreen could have increased 5-year survival in this later period by producing lead time and length biases and by over-diagnosing cancers that would not have become symptomatic [10]. Nonetheless these improvements in 5-year survival are a useful indicator of the impact of improving treatment on women with breast cancer. In 1999–2000, when BreastScreen could have begun to affect mortality, 5-year survival from breast cancer in Australia for all women was 88.3% (5-year survival for women aged 40–69 years was 90–92%) and 9-year survival was 83.4% [2]. Therefore, by 1995 the window of opportunity for early diagnosis consequent upon mammographic screening alone to reduce breast cancer mortality had largely closed.
In contrast there is evidence that advances in breast cancer treatment could be responsible for the observed pattern of decline in breast cancer mortality in Australia. Based on a 10–15 year follow up of their quinquennial overviews (1985–2000) of randomised trials of adjuvant therapy in early breast cancer, the EBCTCG concluded in 2005 that for early breast cancer appropriate use of anthracycline based chemotherapy followed by tamoxifen for ER+ disease would result in annual breast cancer mortality reductions of 57% for ER+ women younger than 50 years of age and 45% for ER+ women aged 50–69 years [13].
Between 1986 and 1999 six Cancer-Registry-based treatment surveys were completed of all Australian women registered with invasive breast cancer in the States of Victoria and Western Australia and Nationally [12, 14–16]. In 1986, only 18% of women received adjuvant tamoxifen and 27% of premenopausal women received adjuvant chemotherapy [14]. The 1995 National survey reported that 85% of Australian women diagnosed with breast cancer had early disease, that 60% of them received adjuvant tamoxifen and that 57% of those who were premenopausal received adjuvant chemotherapy [12, 15]. In 1999, the Victorian State survey, which covered 25% of Australian women, found that 70% of women with early breast cancer received adjuvant tamoxifen and 72% of those who were premenopausal received adjuvant chemotherapy [15]. Our analysis of this Victorian data, using the EBCTG findings [13, 15], shows that breast cancer mortality reductions in Australia in 1999 from adjuvant therapy could have been up to 38% for women aged 40–49 years, and up to 24% for women aged 50 years and older (Appendix). Therefore, adjuvant therapy had the potential to produce most of the observed reductions in breast cancer mortality in Australia since 1991.
These observations are consistent with the findings in other countries where breast cancer mortality trends have been analysed. In the UK, where mortality from breast cancer fell by 22, 22 and 12% for women aged 20–49, 50–69 and 70–79 years, respectively between 1987 and 1997, the decreases in mortality were suggested to have mainly resulted from changes in the way that breast cancer was diagnosed and treated [17]. An examination of age specific falls in breast cancer mortality in the UK between 1989 and 2007 for women aged 40–49 years (41%), 50–64 years (41%) and 65–69 years (38%) lead to the conclusion that mammographic screening did not have a causal role in those falls [18, 19]. The annual percentage changes in breast cancer mortality in Denmark were examined for 1982–2006 and there was no demonstrable effect of the mammographic screening program on breast cancer mortality [19]. A recent study from Norway reported that mammographic screening could not account for at least two-thirds of the reduction in mortality observed in the first 9 years of the national mammographic screening program in women aged 50–69 years, the age group invited to screen [20].
Strengths of our study include the that the data were derived from complete state and national breast cancer incidence, mortality, mammography and treatment data sources and are available over the 17 year period during which BreastScreen was introduced and achieved stable penetration in the targeted age groups. A potential weakness includes the fact that women can have mammography outside of the BreastScreen program, although we have presented data to show that the extent of this would not affect mortality.
Finally, trends in incidence and mortality years since 1999–2000 in Australian women aged 60–69 indicate that over-diagnosis has probably occurred. This observation is consistent with the 2009 analysis of age specific incidence trends from 1972 until 2001 in the State of New South Wales, where 34% of Australian women resided, which estimated that 30–40% of invasive breast cancer in women aged 50–69 years in 2001–2002 was over-diagnosed because of mammographic screening [21]. The harms versus benefits of mammographic screening have now become a concern internationally [22], with a 2009 systematic review of incidence trends in six countries with organised mammographic screening programs finding that one in three breast cancers were over-diagnosed [23] and a 2010 analysis of mammographic randomised controlled screening trials finding that after 15 years of follow up a greater proportion of women screened by mammography had been over-diagnosed than had avoided death from breast cancer [24].
Conclusions
This age specific analysis of breast cancer mortality trends in Australia between when BreastScreen began in 1991 and 2007 has shown that significant reductions in mortality have occurred, but that the greatest relative reduction has been in women aged 40–49 years who are not invited by BreastScreen to participate. Adjuvant therapy probably accounts for most or all of the mortality reduction in these younger women, and at least two-thirds of the observed reduction in mortality for the 50–69 year old Australian women invited by BreastScreen. Therefore, any benefits of mammographic screening in this targeted population must now be weighed against the harms of over-diagnosis and unnecessary treatment. The benefits of adjuvant therapy for breast cancer have been profound and mortality rates should continue to fall as further improvements are translated from clinical trial outcomes into practice.
References
Australian Health Ministers’ Advisory Council (AHMAC) Breast Cancer Screening Evaluation Committee (1990) Breast cancer screening in Australia: future directions. Australian Institute of Health: Prevention Program Evaluation Series No 1. AGPS, Canberra
Australian Institute of Health and Welfare (AIHW) & National Breast and Ovarian Cancer Centre (NBOCC) (2009) Breast Cancer in Australia: an overview, 2009. Cancer series no. 50. Cat. no. CAN 46. AIHW, Canberra
Australian Institute of Health and Welfare (AIHW) (1998) Breast and Cervical Cancer Screening in Australia 1996–97. Cancer Series number 8. Cat. No. CAN 3. AIHW, Canberra
Australian Institute of Health and Welfare (AIHW) & National Breast Cancer Centre (NBCC) (2006) Breast Cancer in Australia: an overview, 2006. Cancer series no. 34. cat. no. CAN 29. AIHW, Canberra
Australian Institute of Health, Welfare (AIHW) (2010) GRIM (General Record of Incidence of Mortality) Books. AIHW, Canberra
Nyström L, Andersson I, Bjurstam N, Frisell J, Nordenskjöld B, Rutqvist LE (2002) Long-term effects of mammography screening: updated overview of the Swedish randomised trials. Lancet 359:909–919
National Cancer Prevention and Control Unit (1997) BreastScreen Australia Statistical Report 1994 and 1995. Department of Family Services, Commonwealth of Australia, Canberra
Australian Institute of Health, Welfare (AIHW), Australasian Association of Cancer Registries (AACR) (2010) Cancer in Australia: an overview, 2010. Cancer series no. 60. Cat. no. CAN 56. AIHW, Canberra
Roder D, Houssami N, Farshid G, Gill G, Luke C, Downey P, Beckmann K, Iosifidis P, Grieve L, Williamson L (2008) Population screening and intensity of screening are associated with reduced breast cancer mortality: evidence of efficacy of mammography screening in Australia. Breast Cancer Res Treat 108:409–416
Gann PH (1997) Interpreting recent trends in prostate cancer incidence and mortality. Epidemiology 8:117–120
Fisher B (1999) From Halsted to prevention and beyond: advances in the management of breast cancer during the twentieth century. Eur J Cancer 35:1963–1973
National Breast Cancer Centre (NBCC) (1999) Surgical management of breast cancer in Australia. NBCC, Sydney
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365:1687–1717
Hill DJ, Giles GG, Russell IS, Collins JP, Mapperson KJ (1990) Management of primary, operable breast cancer in Victoria. Med J Aust 152:67–72
White V, Pruden M, Giles G, Collins J, Jamrozik K, Inglis G, Boyages J, Hill D (2004) The management of early breast carcinoma before and after the introduction of clinical practice guidelines. Cancer 101:476–485
McEvoy S, Ingram D, Byrne M, Joseph D, Dewar J, Trotter J, Harper C, Haworth C, Harvey J, Sterret G, Jamrozik K, Fritschi L (2004) Breast cancer in Western Australia: clinical practice and clinical guidelines. Med J Aust 181:305–309
Peto R, Boreham J, Clarke M, Davies C, Beral V (2000) UK and USA breast cancer deaths down 25% in year 2000 at ages 20–69 years. Lancet 355:1822
Jorgensen KJ, Nielsen M, Gotzsche PC, Brodersen J, Hartling OJ (2009) Fall in breast cancer deaths: a cause for celebration, and caution. BMJ 338:b2126
Jorgensen KJ, Zahl P-H, Gotzsche PC (2010) Breast cancer mortality in organised mammography screening in Denmark: comparative study. BMJ 340:c1241. doi:10.1136/bmj.c1241
Kalager M, Zelen M, Langmark F, Adamai H (2010) Effect of screening mammography on breast cancer mortality in Norway. N Engl J Med 263:1203–1210
Morrell S, Barratt A, Irwig L, Howard L, Biesheuvel C, Armstrong B (2009) Estimates of overdiagnosis of invasive breast cancer associated with screening mammography. Cancer Causes Control 21:275–282
Quanstrum K, Hayward R (2010) Lessons from the mammography wars. N Engl J Med 363:1076–1079
Jorgensen KJ, Gotzsche PC (2009) Overdiagnosis in publicly organised mammography screening programmes: systematic review of incidence trends. BMJ 339:b2587. doi:10.1136/bmj.b2587
McPherson K (2010) Screening for breast cancer–balancing the debate. BMJ 340:c3106. doi:10.1136/bmj.c3106
Acknowledgments
The article was supported by National Health and Medical Research Council of Australia Grant number 465130. We thank Mark Elwood, M.D., D.Sc. of the British Columbia Cancer Agency, Vancouver, and Anthony Miller, M.D., Dalla Lana School of Public Health, University of Toronto, from Canada. for valuable help in reviewing the manuscript and Victoria White, Ph.D. of The Cancer Council Victoria, Melbourne, Australia, for providing the unpublished data used in Appendix.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Estimations of the annual mortality reductions which adjuvant tamoxifen and chemotherapy could have achieved in populations of Australian women diagnosed with breast cancer in 1999. Data from Ref. [15] unless otherwise shown, and proportions of ER+ women in Ref. [15] from Dr. Victoria White, Cancer Council Victoria, Australia; relevant ER data was not available for the 1995 National survey.
Women aged 40–49 years: tamoxifen
85% (proportion of all breast cancer that was early) × 73% (proportion of women with early breast cancer who were ER+ and aged less than 50 years) × 78% (proportion of women with early breast cancer less than 50 years of age who were ER+ and received Tamoxifen) × 31% (EBCTCG: adjuvant tamoxifen reduction in mortality for ER+ women of all ages with early breast cancer [13]) = 15.0%.
Women aged 50–69 years: tamoxifen
85% (proportion of all breast cancer that was early) × 78%(proportion of women with early breast cancer EBC more than 50 years of age who were ER+) × 92% (proportion of women with early breast cancer more than 50 years who were ER+ and received Tamoxifen) × 31% (EBCTCG: adjuvant tamoxifen reduction in mortality for ER+ women of all ages with EBC [13]) = 18.9%.
Women aged 40–59 years: Chemotherapy
72% (1999 Victorian treatment survey proportion of all women aged less than 50 years with early breast cancer who received adjuvant chemotherapy) × 85% (1995 National treatment survey proportion of all women with early breast cancer) × 38% (EBCTCG : adjuvant chemotherapy reduction in mortality for women aged less than 50 years [13]) = 23.3%.
Women aged 50–69 years: Chemotherapy
29% (Victorian treatment survey proportion of all women aged 50 or more years with early breast cancer who received adjuvant chemotherapy) × 85% (1995 National treatment survey proportion of all women with early breast cancer) × 20% (EBCTCG : adjuvant chemotherapy reduction in mortality for women aged more than 50 years [13]) = 4.9%.
Rights and permissions
About this article
Cite this article
Burton, R.C., Bell, R.J., Thiagarajah, G. et al. Adjuvant therapy, not mammographic screening, accounts for most of the observed breast cancer specific mortality reductions in Australian women since the national screening program began in 1991. Breast Cancer Res Treat 131, 949–955 (2012). https://doi.org/10.1007/s10549-011-1794-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1794-6