Abstract
After primary surgery, patients diagnosed with early stage breast cancer undergo radiological investigations based on pathologic stage of disease to rule out distant metastases. Published guidelines can aid clinicians in determining which tests are appropriate based on stage of disease. We wished to assess the consistency of radiological staging in an academic community oncology setting with standard guidelines and to determine the overall impact of non-adherence to these guidelines. A retrospective cohort study was conducted for new breast cancer patients seen at a single institution between January 2009 and April 2010. Patients were included if initial diagnosis and primary surgery was at this institution. Pathologic stage and radiological tests completed were recorded. A literature review was performed and the results were compared with those from this study to determine overall adherence rates. Subsequently, a cost analysis was performed to determine the financial impact at this centre. 231 patients met eligibility criteria for inclusion in this study. A large proportion of patients were over-staged with 129 patients (55%) undergoing unnecessary investigations according to guidelines. Specifically, 59% of stage I patients and 58% of stage II patients were over-investigated. Distant metastases at the time of diagnosis were found in three patients, all of whom had stage III disease (1.3%). The literature reviewed revealed similar non-adherence rates in other centres. The estimated cost of such non-adherence is in the range of $78 (CDN) per new early stage breast cancer patient seen at this centre. This oncology centre has a low adherence to practice guidelines for staging investigations in breast cancer patients, with 55% of patients undergoing unnecessary tests. Very few patients had metastases at diagnosis, and all had pathological stage III disease. Efforts may need to focus on improving knowledge translation across clinical oncology settings to increase guideline adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the second leading cause of cancer mortality in women. In Canada, one in nine women are expected to develop breast cancer over the course of their lifetime [1, 2]. After initial diagnosis, and primary surgery, patients with more aggressive disease undergo extensive staging tests to rule out metastatic disease. Initial radiological and pathological staging of disease are important for adequate diagnosis and choice of therapeutic regimen [2, 3]. The likelihood of detecting metastases at initial diagnosis is fairly low in most stages of disease [2]. The Breast Cancer Disease Site Group of Cancer Care Ontario evaluated and reviewed evidence for routine testing in asymptomatic women who have undergone primary surgery for breast cancer [2]. This guideline, which was completed in 2003, gave indications for the appropriate use of bone scans, abdominal, and chest imaging in this group [2, 4].
The guideline included a systematic review of twenty-two studies published 1966–2003. From these studies, it was found that there was a very low likelihood of metastases in patients diagnosed with stage I disease, and very low likelihood of visceral metastases in patients with stage II disease [2]. The Cancer Care Ontario Practice Guidelines Initiative (CCOPGI) therefore concluded that patients with stage I disease require no further staging investigations, patients with stage II disease require bone scan, and that only for stage III disease is there a role for chest and abdominal imaging in addition to bone scan. This practice guideline by CCOPGI was of overall high quality, as determined by standardized criteria (the AGREE instrument), but did not include a specific plan for knowledge translation or implementation [5]. Over staging can be costly in terms of hospital resources and time, leading to unwarranted investigations. It can also cause unnecessary psychological distress in patients and erroneous staging results can lead to further investigations [6, 7].
Despite the publication of this guideline in 2003, variations in the frequency of investigations exist across hospitals for these newly early staged diagnosed cases who do not present with any symptoms, signs, or biochemical evidence of metastases [2]. The aim of this study was: to assess the consistency an academic oncology centre’s use of radiological staging with the recommendations of the CCOPGI and to determine the cost of over staging investigations in newly diagnosed early stage breast cancer patients across centres.
Patients and methods
A retrospective chart review of all newly diagnosed early stage (Stages I–III) breast cancer patients at a single, community oncology centre from January 2009 to April 2010 was conducted. Patients were identified through the Multidisciplinary Breast Cancer Clinic at St. Michael’s Hospital (SMH), Toronto, Canada, for all new referrals and newly diagnosed early stage breast cancer patients. Two hundred and fifty (250) cases of breast cancer cases were reviewed. Patients were included if they had histologically proven primary cancer of the breast and diagnosis of cancer at SMH. Nineteen files were excluded from analysis due to either recurrent breast cancer, primary surgery outside of the institution or referral to another oncology centre after primary surgery (see Fig. 1).
Breast cancer stage and TNM status were recorded in accordance with the American Joint Committee on Cancer classification system, Sixth Edition which was used in the pathology department during that time period [8]. Pathological and radiological data on all patients were collected and dated, ensuring they were subsequently performed after initial diagnosis and surgery. Bone scan (BS), abdominal ultrasound (AUS), and chest X-ray (CXR) assessments were documented. Initial consultations by surgical and medical oncologists were reviewed to determine if patient reported symptoms were the rationale for testing. This study was approved by the Research Ethics Board at SMH.
In order to assess more generally the extent of over staging in the breast cancer patient community, a literature review of the search engines, PubMed, Cochrane Library, and ERIC (Education Resources Information Center) was conducted. The period of January 1996 to April 2010 was reviewed with the key terms: “breast cancer, neoplasm, staging, guideline, post-operative and baseline”. This time period was chosen to include studies that utilized the most up-to-date guidelines on staging investigations in early breast cancer.
Studies were included given they met the criteria: a study population of early stage breast cancer patients, published in the English language, and included the utilization of at least two of the following: bone scan, chest X-ray, or abdominal/liver ultrasound. In addition, a cost assessment of avoidable investigations in breast cancer patients was conducted in reference to the costs of baseline staging tests set by the Ontario Health Insurance Plan fee schedule to determine the incremental cost-saving that would have been incurred if the guidelines were followed [4].
Results
Two hundred and thirty-one (231) patients, all of whom were female, met eligibility criteria for this study. Of this cohort: 138 (60%) had pathological stage I disease, 74 (32%) had stage II disease and 19 (8%) had stage III patients (see Table 1).
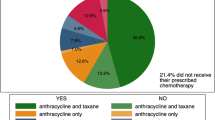
Of the 231 patients, 45% of patients were staged in accordance with Cancer Care Ontario’s (CCO) breast cancer clinical guideline on Staging and Follow up and 55% were not. Frequency of investigations across stages of breast cancer was collected and recorded (see Table 2). All patients with stage III disease were staged in accordance to CCO. The majority of patients with stage I as well as stage II breast cancer underwent unnecessary investigations. Chart review revealed that none of these patients had symptoms to explain the investigations ordered. Four patients (1.7%) were staged according to clinical trial assessment and eligibility criteria.
At diagnosis, one hundred and sixty-three patients underwent a bone scan. Bone scan investigations detected bone metastases in two patients (1.23%). One hundred and thirty-eight patients underwent a liver ultrasound and only one patient (0.72%) had distant metastases to the liver. X-rays completed at diagnosis did not find any lung metastases; in all one hundred and ninety-one cases assessed (0%) (see Table 3).
All distant metastases detected by bone scan or liver ultrasound were found in patients with stage III breast cancer. No distant metastases were found in patients with stage I/II breast cancer. For these patients who underwent testing, there were no documented symptoms on chart review to explain the need for the investigation.
Magnitude of issue
Literature review
An independent reviewer conducted the literature search which identified 225,575 articles of potential relevance by the previous mentioned search words (see Fig. 2). The search engines of Cochrane Library and ERIC did not identify potential articles of interest. Of these articles, six articles were included and summarized for their use of staging investigations in early breast cancer (see Table 4). Five studies included investigations of chest X-ray, liver/abdominal ultrasound, and bone scan [6, 7, 9–11]. The study conducted by Morris et al. [12] covered staging tests of abdominal ultrasound and bone scan.
Comparing levels of frequency of BS, CXR, LUS/AUS in newly diagnosed breast cancer patients, the cohort at SMH experienced higher levels of investigations than studies published by Morris et al. and McWhirter et al. [6, 7, 12], while lower levels of investigation compared to levels reported by Puglisi et al. (see Table 4). In order to determine an estimate of overall frequency level of investigations, results were pooled from the present study and the two studies, the first cohort of McWhirter et al. and patients from Puglisi et al. [6, 7], which specified the frequency of testing across each stage of disease. To determine overall estimates of frequency of testing, the number of patients examined by each baseline imaging was calculated by using the percentages of testing and number of patients according to stage. This was then summed and by dividing the total number of patients who had tests ordered by the total number of patients in the studies, an overall estimated frequency of testing can be established (see Table 5). This method is similar to that used by the CPOGI’s guideline update to determine an overall detection rate [2].
From this pooled data, there are high levels of investigations regardless of stage, ranging from 73 to 100% of patients. However, this pooled average of frequency of investigations and detection of distant metastases can only provide an approximation of staging investigations in early breast cancer across institutions and countries. Other centres encountered higher metastases detection rates in stage III patients than our centre per investigation (range = 5.66 to 14.0%), however, rates were relatively low in stages I and II patients across all institutions and studies (range = 0.0 to 5.6%) [6, 9, 10]. Owing to the nature of cohort studies, no correlation can be made between patient reported symptoms and the detection of metastases. Overall, the frequency of investigations varied across studies despite breast cancer staging guidelines set out by national organizations. This is in accordance with previous reported findings, with small differences depending on the population studied [12].
Cost-analysis
In terms of cost analysis, by using established costs of baseline staging tests in Ontario, we can determine direct cost-utilization in this cohort [4]. The technical fee for a bone scan is $103.80, ultrasound is $48.80 and chest radiograph $21.91 (CDN) [4] based on the Canadian dollar in 2003. Costs from the Ontario Health Insurance Plan fee schedule were available at time of analysis and can provide an approximation of cost incurred. The newly diagnosed breast cancer patients seen at SMH Multidisciplinary Breast Cancer Clinic between January 2009 and April 2010 who were not staged in accordance to CCO guidelines approximately cost $18, 090. This averages to an estimated unnecessary cost of $78 per new breast cancer patient seen at our centre. This does not include additional costs such as radiologist fee, however, provides an approximation of the annual cost saving that could have been appreciated with appropriate use of staging investigations.
Discussion
In this retrospective cohort study, 55% of newly diagnosed early stage breast cancer patients underwent unnecessary investigations, indicating that adherence to guidelines for post-operative staging of patients with breast cancer is poor. Unnecessary clinical investigation as defined by CCO guidelines cost $18, 090 (CDN) and detected no metastases. Detection of occult metastases by radiological investigations was done by appropriate utilization of the guidelines set out by CCO. Other published cohort studies yield similar results. These select studies were completed when the CCOPGI’s 2003 update on baseline staging tests in early stage breast cancer patients was present and available. This is an internationally recognized guideline which is consistent in key recommendations with the American Society of Clinical Oncology (ASCO) 2006 update of the breast cancer follow-up and management guidelines in the adjuvant setting and the National Institute for Health and Clinical Excellence (NICE)’s guideline on early and locally advanced breast cancer diagnosis and treatment [5]. An international physician survey showed that physicians are aware and accept international breast cancer practice guidelines but that barriers do exist in implementing standards of care [13].
Improving adherence to guidelines set out by national organizations may increase resources for urgent staging required for other patients, shorten delays to treatment and decrease anxiety for newly diagnosed breast cancer patients [6, 7, 9–12, 14, 15]. Indeed, it has been shown that there is an increase in psychological distress in cancer patients undergoing radiological investigations to assess the extent of disease [6, 7]. In early stage breast cancer patients, this distress may be completely avoidable. In addition, further secondary investigations required to verify benign findings may even lead to increase exposure to radiation and avoidable risks associated with biopsy of benign spots.
McWhirter et al. [7] demonstrated that following a directed educational intervention, a decrease in frequency of imaging investigations ordered by clinicians was observed for stage I breast cancer patients. Although this educational session is one approach, strategies and methods for knowledge translation of these guidelines have not been implemented to date. One of the more effective methods of knowledge translation is an iterative audit and feedback of guideline adherence directed at specific providers [16]. This has been implemented in other settings and has been applied to cancer settings such as pain management [17, 18]. A plan to adapt such an iterative audit and feedback approach may improve overall adherence.
Based on these results, a study to assess the barriers to guideline adherence has been developed and will be studied through a two-step initiative. First, focus groups with key stakeholders such as oncologists and nurses involved in the treatment of breast cancer will be held to discuss our findings and their insights on staging patients with early stage breast cancer. Specifically the rationale behind over staging patients will be addressed. Second, based on the results from our focus groups, the knowledge translation team at our centre will develop an implementation strategy based on feedback from stakeholders to insure effectiveness.
The cost of over staging in the breast cancer population can compromise access to radiological investigations for urgent staging in patients with symptoms or metastases. Through a review of the literature, it has been found that many centres have difficulties in guideline adherence of post operative staging investigations for early stage breast cancer. The estimated unnecessary imaging costs associated with a newly diagnosed breast cancer patient is $84 (CDN) per early stage breast cancer patient in our cohort. The overall cost-saving that could be incurred by following guideline care was estimated at $18, 090 (CDN) for the 231 patients seen at our centre.
Conclusion
This study confirmed data from previous similar studies completed on staging investigations and guideline adherence [3, 6, 7, 9–12, 14, 15]. An increase in positivity in distant metastases was observed as TNM stage increased, which is suggested by the guidelines set out by national organizations. Although it is necessary that newly diagnosed breast cancer patients be assessed and investigated; health care costs continue to increase. Staging examinations should be individualized according to tumor size, nodal status, and stage. Methods for improving knowledge translation of these guidelines need to be developed and evaluated in order to insure appropriate use of resources and avoid unnecessary psychological harms to the patients involved.
References
Canadian Cancer Society’s Steering Committee (2009) Canadian Cancer Statistics 2009. Canadian Cancer Society, Toronto
Myers RE, Johnston M, Pritchard K, Levine M, Oliver T, Breast Cancer Disease Site Group of the Cancer Care Ontario Practice Guidelines Initiative (2001) Baseline staging tests in primary breast cancer: a practice guideline. CMAJ 164(10):1439–1444
Ravaioli A, Pasini G, Polselli A, Papi M, Tassinari D, Arcangeli V, Milandri C, Amadori D, Bravi M, Rossi D, Fattori PP, Pasquini E, Panzini I (2002) Staging of breast cancer: new recommended standard procedure. Breast Cancer Res Treat 72(1):53–60. doi:10.1023/A:1014900600815
Members of the Breast Cancer Disease Site Group (2003) Baseline staging tests in primary breast cancer. Practice guideline report #1-14. Cancer Care Ontario
Simmons CE, Hogeveen S, Nichols J, Trudeau-Tavara S, Quan M (2010) Quality and consistency in breast cancer clinical guidelines internationally: are we globally consistent? J Clin Oncol 28:15s (abstr 6096)
Puglisi F, Follador A, Minisini AM, Cardellino GG, Russo S, Andreetta C, Di Terlizzi S, Piga A (2005) Baseline staging tests after a new diagnosis of breast cancer: further evidence of their limited indications. Ann Oncol 16(2):263–266. doi:10.1093/annonc/mdi063
McWhirter E, Yogendran G, Wright F, Dranitsaris G, Clemons M (2007) Baseline radiological staging in primary breast cancer: impact of educational intervention on adherence to published guidelines. J Eval Clin Pract 13(4):647–650. doi:10.1111/j.1365-2753.2007.00804.x
Singletary SA, Connolly JL (2006) Breast cancer staging: working with the sixth edition of the AJCC Cancer Staging Manual. CA Cancer J Clin 56(1):37–47. doi:10.3322/canjclin.56.1.37
Samur M, Bozcuk HS, Karaveli Ş, Pestereli E, Özdoğan M, Yildiz M, Artaç M, Savaş B (2003) Reevaluation of baseline staging tests in breast cancer; what should be the standard? Turkish J 33(3):150–153
Schneider C, Fehr MK, Steiner RA, Hagen D, Haller U, Fink D (2003) Frequency and distribution pattern of distant metastases in breast cancer patients at the time of primary presentation. Arch Gynecol Obstet 269(1):9–12. doi:10.1007/s00404-002-0445-x
Abuzallouf S, Motawy M, Thotathil Z (2007) Baseline staging of newly diagnosed breast cancer–Kuwait cancer control centre experience. Med Princ Pract 16:22–24. doi:10.1159/000096135
Morris PG, O’Connor M, O’Rafferty C, Sheikh R, Gray J, McDermott R, Boyle T, Kennedy MJ (2009) The excessive cost of baseline diagnostic imaging in early breast cancer. Ir Med J 102(5):149–152
Gandhi S, Alibhai S, Victor JC, Simmons C, Verma S (2010) The impact of resource setting and guidelines on global early breast cancer practice. 2010 Breast Cancer Symposium, Abstract 199. http://www.asco.org/ascov2/Meetings/Abstracts?&vmview=abst_detail_view&confID=100&abstractID=60376. Accessed 20 Aug 2011
Ravaioli A, Tassinari D, Pasini G, Polselli A, Fattori PP, Pasquini E, Masi A, Alessandrini F, Canuti D, Panzini I, Drudi G (1998) Staging of breast cancer: what standards should be used in research and clinical practice? Ann Oncol 9(11):1173–1177
Ma M, Bell J, Campbell S, Basnett I, Pollock A, Taylor I on behalf of the Clinical Advisory Panel (1997) Breast cancer management: is volume related to quality? Br J Cancer 75:1652–1659. doi:10.1038/bjc.1997.281
Davis DA, Taylor-Vaisey A (1997) Translating guidelines into practice. A systematic review of theoretical concepts, practical experience and research evidence in the adoption of clinical practice guidelines. Can Med Assoc J 157(4):408–416
Håkonsen GD, Strelec P, Campbell D, Hudson S, Loennechen T (2008) Adherence to medication guideline criteria in cancer pain management. J Pain Symptom Manage 37(6):1006–1018. doi:10.1016/j.jpainsymman.2008.06.006
Dulko D, Hertz E, Julien J, Beck S, Mooney K (2010) Implementation of cancer pain guidelines by acute care nurse practitioner using an audit and feedback strategy. J Am Acad Nurse Pract 22(1):45–55. doi:10.1111/j.1745-7599.2009.00469.x
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Han, D., Hogeveen, S., Sweet Goldstein, M. et al. Is knowledge translation adequate? A quality assurance study of staging investigations in early stage breast cancer patients. Breast Cancer Res Treat 132, 1–7 (2012). https://doi.org/10.1007/s10549-011-1786-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1786-6