Abstract
The aim of this study was to investigate the association of two genetic polymorphisms, MDM2 SNP309 and TP53 R72P, with incidence of neutropenia in breast cancer patients treated with 5-FU/epirubicin/cyclophosphamide (FEC). Primary breast cancer patients (n = 216) treated with adjuvant FEC (60, 75 or 100 mg/m2) were included in this study. The association of genotypes of MDM2 SNP309 and TP53 R72P, determined by TaqMan SNP Genotyping Assays, with febrile neutropenia (FN) was investigated. In the patients treated with FEC100, G/G genotype for MDM2 SNP309 (G/G genotypeMDM2) was significantly (P < 0.01) associated with a lower incidence (5.3 vs. 39.2%) of severe neutropenia (<100/mm3) than with T/T + T/G genotypesMDM2, and C/C genotype for TP53 R72P (C/C genotypeTP53) was significantly (P = 0.03) associated with a higher incidence (58.3 vs. 27.3%) of FN than with G/G + G/C genotypesTP53. The combination of C/C genotypeTP53 and T/T + T/G genotypeMDM2 showed the highest risk for developing severe neutropenia (83.3%) and FN (62.5%) than any other combinations. In the patients treated with FEC60 or FEC75, there was no significant association of MDM2 SNP309 and TP53 R72P with severe neutropenia and FN. MDM2 SNP309 and TP53 R72P are significantly associated with severe neutropenia and FN, respectively, in breast cancer patients treated with FEC100, and especially their combination may be a useful predictor of severe neutropenia and FN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination chemotherapy consisting of 5-FU, epirubicin, and cyclophosphamide (FEC) is often used for active treatment of breast cancer in neoadjuvant, adjuvant, and metastatic settings. The prescribed dose of epirubicin in FEC used to be 50–75 mg/m2 every 3 weeks but recently a higher dose of 100 mg/m2 every 3 weeks is used more often since this higher dose was clearly demonstrated to be more effective. However, one of the clinically most important and frequently observed adverse effects of FEC is bone marrow suppression. For Caucasian patients treated with FEC100, incidence of febrile neutropenia (FN) is reportedly 0–8% [1–3] while for Japanese patients it seems to be slightly higher (14–20%) [4, 5]. The ASCO guideline (2006 update) recommends the primary prophylactic use of colony stimulating factor (CSF) when the risk of FN is in the range of 20% or higher. Thus, the incidence of FN for Japanese patients treated with FEC100 can be considered to be close to the threshold for prophylactic use of CSF. For the adequate and safe administration of chemotherapy, it is therefore very important to predict who is more likely to develop FN since they can be candidates for prophylactic use of CSF.
Several factors such as higher age (>65 years), small body surface area (BSA), and pretreatment absolute neutrophile count (ANC) are reported to be associated with FN. But prediction of FN occurrence using these risk factors is not accurate enough, so that more accurate predictors need to be developed. Nayak et al. [6] recently reported that MDM2 SNP309 is associated with resistance to chemotherapy in vitro, i.e., G/G homozygotes up-regulate MDM2, which in turn down-regulates topoisomerase 2A (TOPO2A), rendering tumor cells less sensitive to anti-TOPO2A chemotherapy such as epirubicin-based regimens. Since this effect of MDM2 SNP309 on tumor cells is speculated to be also operational in normal bone marrow hematopoietic cells, their sensitivity to epirubicin-based regimens may be influenced by MDM2 SNP309 and such an association, if proved, might then be applicable to the prediction of FN occurrence.
TP53 R72P is one of the most thoroughly studied single nucleotide polymorphisms (SNPs) in breast cancer in terms of its association with resistance to chemotherapy [7–10]. 72P-allele has been shown to induce apoptosis less effectively than does R72-allele in vitro [11]. In fact, 72P-allele has been demonstrated to be associated with resistance to chemotherapy in vitro [12] and also in the neoadjuvant setting [8]. If this impact of TP53 R72P on chemo-sensitivity is also operational in normal bone marrow hematopoietic cells, this polymorphism may well be associated with FN.
Although the association of MDM2 SNP309 or TP53 R72P with resistance to chemotherapy in breast tumors has been investigated by several investigators, conflicting results have been reported [7–10, 13, 14]. Since mechanisms of chemo-resistance are complicated and differ among tumors, it is very difficult to demonstrate in the clinical setting whether these SNPs, even though they have a certain impact, are associated with chemo-resistance. On the other hand, bone marrow hematopoietic cells are normal cells without any genetic changes such as somatic mutations and gene amplification/deletion, and thus, the influence of these SNPs on response to chemotherapy can be evaluated in a less complicated manner in normal bone marrow hematopoietic cells than in tumor cells. In the present study, we investigated whether MDM2 SNP309 and TP53 R72P are associated with the incidence of leucopenia and FN in breast cancer patients treated with FEC in the adjuvant setting.
Materials and methods
Patients
Primary breast cancer patients (n = 216), who underwent mastectomy or breast-conserving surgery and were treated with adjuvant FEC therapy (5FU 500 mg/m2, epirubicin 60, 75 or 100 mg/m2, and cyclophosphamide 500 mg/m2, q3w× 6 cycles) at Osaka University Hospital between July 2001 and April 2010, were consecutively recruited for this study. Before FEC treatment, all the patients showed satisfactory organ (bone marrow, liver, and kidneys) function. After chemotherapy, the patients who underwent breast-conserving surgery received radiotherapy for the breast and patients with hormone-receptor-positive tumors received adjuvant hormonal therapy. The median follow–up was 55 months (range, 4–114 months). Characteristics of the patients are shown in Table 1. Informed consent was obtained from each patient.
Genotype analysis
Genomic DNA was extracted from peripheral whole blood mononuclear cells obtained before surgery, and TaqMan SNP Genotyping Assays (Applied Biosystems, Foster City, CA, USA) were used for genotyping MDM2 SNP309 (genotypeMDM2) and TP53 R72P (genotypeTP53).
Detection of neutropenia
All the patients had to have neutrophile counts >1,500/mm3 before FEC was administered. For the first cycle, a complete blood count test was performed both before and about 7 days after FEC. When grade 4 (G4) neutropenia was found, the complete blood count test was repeated a few days later. A patient who developed FN was treated with G-CSF (lenograstim) until the neutrophile count improved to over 5,000/mm3 and received a reduced dose (20–25% reduction) of FEC from the next cycle or the same dose combined with a prophylactic dose of G-CSF. For most patients, a complete blood count test was performed once before FEC from the second cycle thereafter.
Grades of neutropenia, infection, and FN were assessed according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events (version 4) and G4 neutropenia with a neutrophile count <100/mm3 was defined as severe neutropenia for the purposes of this study since severe neutropenia is considered to be a risk factor for the development of FN [15].
Estrogen receptor, progesterone receptor, HER2 and histological grade
Estrogen receptor and progesterone receptor were classified as positive when 10% or more of the tumor cells immunohistochemically stained positive (ER: Clone 6F11, Ventana, Tokyo, Japan; PR: Clone16, SRL Inc., Tokyo, Japan). The HER2 amplification was determined with FISH using the PathVysion HER-2 DNA Probe Kit (Abbott Molecular, Chicago, IL, USA and SRL) or immunohistochemically using anti-human c-erbB-2 polyclonal antibody (Nichirei Biosciences, Tokyo, Japan) as previously described [16]. FISH scores were obtained by counting fluorescence signals in at least 60 malignant cell nuclei per case, and for each specimen, the ratio of HER2 gene signals to chromosome 17 centromere signals was calculated. A tumor was considered to be HER2-amplified if the FISH ratio was ≥2.0. When a tumor showed +3 immunostaining, it was considered HER2 positive. The histological grade was determined with the Scarff-Bloom-Richardson grading system [17].
Statistical analysis
Associations between the clinicopathological parameters and genotypes were assessed with the χ2 test or Fisher’s exact test. A logistic regression model was used for univariate and multivariate analysis of the relationship between the MDM2 SNP309 or TP53 R72P and FN. All test results with a P-value of less than 0.05 were considered significant. All statistical analyses were performed with StatView software (Version 5.0 for Windows; SAS Institute, Cary, NC, USA).
Results
MDM2 SNP309 and neutropenia
Patients treated with FEC60 or FEC75 showed no significant differences in the incidence of any type of neutropenia among T/T, T/G, and G/G genotypesMDM2 or between G/G and T/T + T/G genotypesMDM2 (Table 2). For patients treated with FEC100, no significant differences were detected either in the incidence of any type of neutropenia among T/T, T/G, and G/G genotypesMDM2. However, a comparison of G/G genotypeMDM2 with T/T + T/G genotypesMDM2 found that the former showed a tendency (P = 0.07) toward a lower incidence (73.7 vs. 90.2%) of G4 neutropenia as well as a significantly (P < 0.01) lower incidence (5.3 vs. 39.2%) of severe neutropenia than did T/T + T/G genotypes MDM2.
TP53 R72P and neutropenia
Patients treated with FEC60 or FEC75 showed no significant differences in the incidence of any type of neutropenia among G/G, G/C, and C/C genotypesTP53 or between C/C and G/G + G/C genotypesTP53 (Table 3). For patients treated with FEC100, no significant differences were detected either in the incidence of any type of neutropenia among G/G, G/C, and C/C genotypesTP53. However, a comparison of C/C genotypeTP53 with G/G + G/C genotypesTP53, found that the former showed a tendency (P = 0.07) toward a higher incidence (55.6 vs. 26.2%) of severe neutropenia as well as a significantly (P = 0.03) higher incidence (58.3 vs. 27.3%) of FN than did G/G + G/C genotypesTP53.
Association of MDM2 SNP309 and TP53 R72P with neutropenia after adjustment for conventional risk factors
For the patients treated with FEC100, the associations of MDM2 SNP309 and TP53 R72P with severe neutropenia and FN after adjustment for conventional risk factors such as age, BSA, and pretreatment ANC were investigated (Table 4). After these adjustments, G/G genotypeMDM2 still showed a significantly lower incidence of severe neutropenia, and C/C genotypeTP53 a significantly higher incidence of FN.
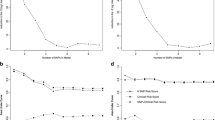
The percentage of patients who developed FN according to the treatment cycle at which FN was first seen is shown in Fig. 1. When FN occurred, it did so in the first cycle for almost all patients regardless of MDM2 SNP309 or TP53 R72P genotypes, so that there was no significant difference in the cycle at which FN occurred between the T/T + T/G genotypeMDM2 and G/G genotypeMDM2 or between the G/G + G/C genotypeTP53 and C/C genotypeTP53.
Incidence of FN according to the cycle of FEC100 MDM2 SNP309: Among the patients treated with FEC100, 22 (35.5%) of 62 patients with T/T + T/G genotypesMDM2 and 5 (21.7%) of 23 patients with G/G genotypeMDM2 developed febrile neutropenia (FN). The graph shows distribution of the patients with FN according to the treatment cycle where FN first occurred. Frequency (vertical axis) means number of patients with FN as a percentage of the total number of patients in each genotype group (G/G genotypeMDM2 or T/T + T/G genotypesMDM2). TP53 R72P: Among the patients treated with FEC100, 20 (27.3%) of 73 patients with G/G + G/C genotypesTP53 and 7 (58.3%) of 12 patients with C/C genotypeTP53 developed FN. The graph shows distribution of the patients with FN according to the treatment cycle where FN first occurred. Frequency (vertical axis) means number of patients with FN as a percentage of the total number of patients in each genotype group (C/C genotypesTP53 or G/G + G/C genotypesTP53)
Combination of MDM2 SNP309 and TP53 R72P as predictor of neutropenia
The combination of MDM2 SNP309 and TP53 R72P genotypes was subjected to analysis in terms of their association with neutropneia in FEC100 treated patients (Table 5). The combination of T/T + T/G genotypeMDM2 and C/C genotypeTP53 was associated with a significantly higher incidence of severe neutropenia (83.3%) (P < 0.01) and FN (62.5%) (P = 0.02) than the combination of G/G genotypeMDM2 and G/G + G/C genotypeTP53 (6.3 and 15.8%, respectively). Interestingly, the combination of G/G genotypeMDM2 and C/C genotypeTP53 and of T/T + T/G genotypeMDM2 and G/G + G/C genotypeTP53 were associated with an intermediate incidence of severe neutropenia and FN (31.3 and 32.3%, respectively).
Discussion
It has been reported that G/G genotypeMDM2 is associated with an elevated expression of MDM2, which results in the down-regulation of TOPO2A, thus rendering tumor cells with G/G genotypeMDM2 resistant to chemotherapeutic agents against TOPO2A [6]. Moreover, the elevated expression of MDM2 down-regulates TP53, which leads to chemoresistance because of the inhibition of the TP53-induced apoptotic pathway. Since bone marrow hematopoietic cells are thought to be similarly affected by MDM2 SNP309, it is speculated that G/G genotypeMDM2 would show resistance to anthracycline-based regimens such as FEC in terms of bone marrow suppression. In the study presented in this article, we could in fact demonstrate that G/G genotypeMDM2 treated with FEC100 showed a significantly (P < 0.01) lower incidence (5.3%) of severe neutropnenia than did T/T + T/G genotypesMDM2 (39.2%). Although the difference was statistically not significant, the incidence of FN was also lower for G/G genotypesMDM2 (21.7%) than for T/T + T/G genotypesMDM2 (35.5%). However, such associations were not detected for patients treated with FEC60 or FEC75, probably because the incidence of severe neutropenia and FN was much lower in those patients, so that the impact of MDM2 SNP309 on neutropenia, if any, is probably not detectable.
Since the apoptotic function of tumor cells with C/C genotypeTP53 has been found to have diminished in association with an increased resistance to DNA-damaging agents in vitro [11, 12], it was expected that C/C genotypeTP53 would show a lower incidence of severe neutropenia and FN. Unexpectedly, however, we obtained the opposite results. C/C genotypeTP53 showed a significantly (P = 0.03) higher incidence (58.3 vs. 27.3%) of FN and a tendency (P = 0.07) toward an increase in the incidence (55.6 vs. 26.2%) of severe neutropenia than G/G + G/C genotypesTP53 when treated with FEC100. Recently, Khrunin et al. have reported a significant association of severe neutropenia with C/C genotypeTP53 in ovarian cancer patients treated with cisplatin-based chemotherapy [18]. These results put together suggest that C/C genotypeTP53 is more sensitive to FEC100 than G/G + G/C genotypesTP53.
The association between the TP53 mutation and response to an anthracycline-based regimen is not straightforward. Although early studies reported on an association between the TP53 mutation and resistance to an anthracycline-based regimen in various types of tumors in vitro [19] and several clinical studies also reported comparable findings [20–22], the opposite finding, namely that TP53 mutation was associated with a better response to an anthracycline-based regimen was also reported both in vitro [23] and clinically [24]. The reason for these discrepant effects of TP53 mutation on response to an anthracycline-based regimen is currently unknown. In tumor cells with TP53 mutation, the apoptosis inducing function is impaired but so is the DNA repair function. It might thus be possible that tumor cells with DNA damage escape apoptosis and proceed to the G2/M phase where they meet with catastrophic cell death, resulting in a higher sensitivity to chemotherapy. Since the TP53 function of bone marrow hematopoietic cells with C/C genotypeTP53 is thought to be diminished, such cells may also show a high sensitivity to FEC through a mechanism analogous to the one described above. However, the precise mechanism through which C/C genotypeTP53 acquires a high sensitivity to FEC in terms of bone marrow suppression will need to be investigated in a future study.
Since age, BSA, and pretreatment ANC are well-established risk factors for neutropenia, we examined the association of MDM2 SNP309 and TP53 R72P with neutropenia after adjustment for these risk factors (Table 4), but still the associations between MDM2 SNP309 and severe neutropenia (P = 0.02) and between TP53 R72P and FN (P = 0.03) remained significant. The combination of these two genetic polymorphisms was also investigated. For MDM2 SNP309, T/T + T/G genotypeMDM2 was found to be a high-risk genotype and G/G genotypeMDM2 a low-risk genotype for neutropenia. For TP53 R72P, C/C genotypeTP53 was found to be a high-risk genotype and G/G + G/C genotypeTP53 a low-risk genotype. In treatment with FEC100, we found that the combination of high-risk genotypeMDM2 and high-risk genotypeTP53 was associated with the highest incidence of severe neutropenia and FN and that of low-risk genotypeMDM2 and low-risk genotypeTP53 with the lowest incidence. Interestingly, the combination of high-risk genotypeMDM2 and low-risk genotypeTP53 and of low-risk genotypeMDM2 and high-risk genotypeTP53 was associated with an intermediate incidence of severe neutropenia and FN, suggesting that the combination of these two SNPs has an additive effect on their capability to predict severe neutropenia and FN.
In conclusion, we were able to show that the presence of MDM2 SNP309 and TP53 R72P is significantly associated with, respectively, the frequency of severe neutropenia and FN in breast cancer patients treated with FEC100 but not with FEC60 or FEC75. These SNPs, especially in their combination, may be useful as predictors of risk for developing severe neutropenia and FN in patients treated with FEC100. However, our observations presented in this article need to be validated in a future study covering a larger number of patients.
References
Roche H, Fumoleau P, Spielmann M et al (2006) Sequential adjuvant epirubicin-based and docetaxel chemotherapy for node-positive breast cancer patients: the FNCLCC PACS 01 trial. J Clin Oncol 24:5664–5671
Mouret-Reynier MA, Abrial CJ, Ferrière JP et al (2004) Neoadjuvant FEC 100 for operable breast cancer: eight-year experience at Centre Jean Perrin. Clin Breast Cancer 5:303–307
French Adjuvant Study Group (2001) Benefit of a high-dose epirubicin regimen in adjuvant chemotherapy for node-positive breast cancer patients with poor prognostic factors: 5 year follow-up results of French Adjuvant Study Group 05 randomized trial. J Clin Oncol 19:602–611
Abe H, Umeda T, Tanaka M et al (2010) Feasibility of FEC 100 followed by DOC 100 as adjuvant chemotherapy for breast cancer. Gan To Kagaku Ryoho 37:1483–1487
Toi M, Nakamura S, Kuroi K et al (2008) Phase II study of preoperative sequential FEC and docetaxel predicts of pathological response and disease free survival. Breast Cancer Res Treat 110:531–539
Nayak MS, Yang JM, Hait WN (2007) Effect of a single nucleotide polymorphism in the murine double minute 2 promoter (SNP309) on the sensitivity to topoisomerase II-targeting drugs. Cancer Res 67:5831–5839
Tommiska J, Eerola H, Heinonen M et al (2005) Breast cancer patients with p53 Pro72 homozygous genotype have a poorer survival. Clin Cancer Res 11:5098–5103
Xu Y, Yao L, Ouyang T et al (2005) p53 codon 72 polymorphism predicts the pathologic response to neoadjuvant chemotherapy in patients with breast cancer. Clin Cancer Res 11:7328–7333
Xu Y, Yao L, Zhao A et al (2008) Effect of p53 codon 72 genotype on breast cancer survival depends on p53 gene status. Int J Cancer 122:2761–2766
Toyama T, Zhang Z, Nishio M et al (2007) Association of TP53 codon 72 polymorphism and the outcome of adjuvant therapy in breast cancer patients. Breast Cancer Res 9:R34
Dumont P, Leu JI, Della Pietra AC 3rd, George D, Murphy M (2003) The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet 33:357–365
Sullivan A, Syed N, Gasco M et al (2004) Polymorphism in wild-type p53 modulates response to chemotherapy in vitro and in vivo. Oncogene 23:3328–3337
Schmidt MK, Tommiska J, Broeks et al (2009) Combined effects of single nucleotide polymorphisms TP53 R72P and MDM2 SNP309, and p53 expression on survival of breast cancer patients. Breast Cancer Res 11:R89
Boersma BJ, Howe TM, Goodman JE et al (2006) Association of breast cancer outcome with status of p53 and MDM2 SNP309. J Natl Cancer Inst 98:911–919
Smith TJ, Khatcheressian J, Lyman GH et al (2006) 2006 update of recommendations for the use of white blood cell growth factors: an evidence-based clinical practice guideline. J Clin Oncol 24:3187–3205
Tsuda H, Sasano H, Akiyama F et al (2002) Evaluation of interobserver agreement in scoring immunohistochemical results of HER-2/neu (c-erbB-2) expression detected by herceptest, nichirei polyclonal antibody, CB11 and TAB 250 in breast carcinoma. Pathol Int 52:126–134
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19:403–410
Khrunin AV, Moisseev A, Gorbunova V, Limborska S (2010) Genetic polymorphisms and the efficacy and toxicity of cisplatin-based chemotherapy in ovarian cancer patients. Pharmacogenomics J 10:54–61
O’Connor PM, Jackman J, Bae I et al (1997) Characterization of the p53 tumor suppressor pathway in cell lines of the National Cancer Institute anticancer drug screen and correlations with the growth-inhibitory potency of 123 anticancer agents. Cancer Res 57:4285–4300
Kandioler-Eckersberger D, Ludwig C, Rudas M et al (2000) TP53 mutation and p53 overexpression for prediction of response to neoadjuvant treatment in breast cancer patients. Clin Cancer Res 6:50–56
Chrisanthar R, Knappskog S, Løkkevik E et al (2008) CHEK2 mutations affecting kinase activity together with mutations in TP53 indicate a functional pathway associated with resistance to epirubicin in primary breast cancer. PLoS One 26:e3062
Geisler S, Lønning PE, Aas T et al (2001) Influence of TP53 gene alterations and c-erbB-2 expression on the response to treatment with doxorubicin in locally advanced breast cancer. Cancer Res 6:2505–2512
Bunz F, Hwang PM, Torrance C et al (1999) Disruption of p53 in human cancer cells alters the responses to therapeutic agents. J Clin Invest 104:263–269
Bertheau P, Turpin E, Rickman DS et al (2007) Exquisite sensitivity of TP53 mutant and basal breast cancers to a dose-dense epirubicin-cyclophosphamide regimen. PLoS Med 4:e90
Acknowledgments
This study was supported in part by a Grant-in-Aid for Cancer Research from the Ministry of Health, Labour and Welfare of Japan.
Conflict of interest
S. Noguchi has received research grants and honoraria from Pfizer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Okishiro, M., Kim, S.J., Tsunashima, R. et al. MDM2 SNP309 and TP53 R72P associated with severe and febrile neutropenia in breast cancer patients treated with 5-FU/epirubicin/cyclophosphamide. Breast Cancer Res Treat 132, 947–953 (2012). https://doi.org/10.1007/s10549-011-1637-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1637-5