Abstract
We conducted a case–control study to evaluate the risk of breast cancer associated with adipose concentrations of polybrominated diphenyl ethers (PBDEs) among women undergoing surgical breast biopsies in the San Francisco Bay Area of California (n = 78 cases; 56 controls). Adipose tissue was analyzed for the five major congeners of PBDEs. Unconditional logistic regression was used to estimate age- and race-adjusted exposure-specific odds ratios (ORs) and 95% confidence intervals (95% CI). Adipose levels of PBDEs were among the highest ever reported. Adjusted ORs for the highest compared with lowest levels of exposures were as follows: 0.56 (95% CI 0.19–1.68) for BDE-47; 1.19 (95% CI 0.35–4.10) for BDE-99; 0.91 (95% CI 0.33–2.53) for BDE-100; 0.52 (95% CI 0.19–1.39) for BDE-153; 1.67 (95% CI 0.44–6.29) for BDE-154; 2.04 (95% CI 0.45–9.20) for total BDEs. These results provide no evidence of an association between PBDE adipose concentrations measured at or near the time of diagnosis and breast cancer risk. Our study was limited by a small sample size. Given the high levels of PBDEs found in this population of California women, future studies are warranted. Such studies would benefit from a larger sample size, a more representative control series, and/or a prospective design.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Variability in breast cancer rates by region and changing breast cancer rates with migration from one area to another led to speculation that environmental factors may play a role in this disease’s etiology. Polybrominated diphenyl ethers (PBDEs) are a class of more than 200 brominated compounds widely used as flame retardants in plastics, foams, textiles, electronic devices, and building materials [1, 2]. PBDEs are pervasive environmental contaminants and human exposures are widespread and well-documented [1, 3, 4]. The USA, and in particular, California, is home to some of the highest breast cancer rates in the world [5]. These regions have also reported high-PBDE body burden levels with Americans generally having levels tenfold those reported among European and Asian populations, and Californians having some of the highest body burden levels in the world [4, 6–9]. Health effects associated with PBDE exposures in humans are not well-characterized, but laboratory studies have demonstrated that PBDEs have endocrine-disrupting properties [2, 10–12], suggesting their potential role in hormonally related cancers such as breast cancer.
The results presented here are from a small hospital-based case–control study using measured levels of five major PBDE congeners in the breast adipose tissue of women who underwent surgical breast biopsies during 1995–1998 in the San Francisco Bay Area of California, USA.
Materials and methods
Study population
The current analysis is an extension of a previous case–control study designed to examine body burden levels of halogenated compounds and breast cancer risk [13, 14]. This study was initially conducted at two hospitals in the San Francisco Bay area of California. Cases were women with histologically confirmed invasive breast cancer, and controls were women with benign histological changes. Patients with a diagnosis of atypical hyperplasia or breast carcinoma in situ were excluded as were patients with prior cancer diagnoses or prior-reported treatments with radiation or Tamoxifen. Participants filled out a self-administered dietary questionnaire, completed an in-person interview, and allowed their surgeons to extract a small amount of breast adipose tissue during their diagnostic biopsy or surgical treatment. This project was reviewed and approved by the California Health and Human Services Agency Committee for the Protection of Human Subjects and by the Institutional Review Boards of the two participating hospitals and of the US Army Medical Research and Materiel Command.
The study population for this analysis is composed of 134 women (78 cases and 56 controls) who completed the study protocol and for whom concentrations of at least one PBDE congener was measured. Details of recruitment and characteristics of the study population are reported elsewhere [13].
Specimen collection and laboratory methods
For women undergoing surgical breast biopsy or local excision (lumpectomy), study surgeons obtained about 1 g of breast adipose tissue from beyond the edges of the biopsy or excision cavity. For women undergoing mastectomy, the surgeons obtained similar amounts of breast adipose tissue from a site distant from the tumor to avoid interference with pathologic analyses. The samples of adipose tissue were immediately placed in chemically clean glass jars with Teflon-lined screw caps and labeled with a number, with no identifiers. Samples were frozen to less than −20°C until analysis. Samples were extracted in dichloromethane/hexane in batches of six with a reagent blank and standard reference materials (SRM 1945). Gel permeation and Florisil column chromatography were used to remove lipids. Five BDEs (BDE-47, BDE-99, BDE-100, BDE-153, and BDE-154) were measured on a Varian 3800 Gas Chromatograph (GC) with a Varian 1200L Mass Spectrometer (MS). The column was a Varian VF-5 ms 30 m × 0.25 mm id × 0.25 μm film. Helium at 1.0 ml/min was used as the carrier gas. The MS was operated in extended dynamic range mode using electron impact ionization and MS/MS detection. A full description of laboratory methods and quality control efforts appears elsewhere [15].
Statistical analyses
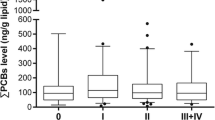
Questionnaire information was extracted, coded and entered in a computerized database, and merged with the chemical analysis results. Pearson’s chi-square statistics were used to compare the sociodemographic characteristics and risk factor distributions by case status. Where appropriate, we calculated P-values for trend from the Mantel–Haenszel chi-square. To examine the distribution of PBDEs by case status, we constructed box blots and calculated P-values from the Wilcoxon rank sum test. Unconditional logistic regression models were used to estimate exposure-specific odds ratios (OR) and 95% confidence intervals for each of the five PBDE congeners, adjusting for four categories of age (<40, 40–49, 50–59, and ≥60 years) and two categories of race/ethnicity (non-Hispanic white and “other”). Subsequent models also adjusted for lactation history and menopausal status (the only two breast cancer risk factors that differed by case status). In the logistic regression analyses, we alternately modeled the concentration for each PBDE congener as a continuous variable (on a log scale) and as an ordinal variable with three levels representing the tertiles of exposure among the controls. All analyses were performed in SAS [16] and R [17].
Results
Characteristics and risk factor distributions for the 78 cases and 56 controls included in this analysis are presented in Table 1. The study population was predominantly composed of highly educated (88% with a college degree or higher) high-income (39% with annual incomes of ≥$100,000) non-Hispanic white (72%) women. Despite efforts to frequency match on age, controls were more likely than cases to be premenopausal, reflecting their younger ages (approximately 70% of controls were younger than the age of 50 compared with 41% of cases). Generally, the reproductive risk factor profiles of cases and controls were remarkably similar. Other than shorter lactation histories among cases compared with controls, no differences were noted in the distribution of established breast cancer risk factors by case status.
Median PBDE adipose concentrations were modestly higher than those reported in 2003–2004 NHANES data [18] and varied substantially by congener with the highest levels observed for the lower-brominated congeners (in ng/g lipid): BDE-47 = 22, BDE-99 = 12, BDE-100 = 5, BDE-153 = 7, and BDE-154 = 1. Distributions of PBDE concentrations by case status are shown in Fig. 1. Although the median concentrations for all congeners were slightly higher in controls than in cases, no statistically significant differences in distributions between cases and controls were found (P-values for Wilcoxon rank sum tests ranged from 0.16 to 0.80).
Results for logistic regression analyses, adjusting for age and race/ethnicity, are presented in Table 2. Adjusted ORs did not significantly differ from 1.0, and there was no evidence for a trend of increasing risk associated with increasing concentrations for any of the PBDE congeners. Further adjustment for lactation history and menopausal status did not substantially change these results (data not shown). Models with PBDE levels expressed in a continuous fashion yielded similarly null results (data not shown).
Discussion
Our results provide no evidence of an association between PBDE adipose concentrations and breast cancer risk. Although the point estimates were suggestively elevated for BDE-154, they are based on a small number of cases and we cannot envision any biologic rationale for why this particular congener alone is related to breast cancer. A number of limitations of this study, however, are worth noting. First, the levels of PBDEs were measured at (or near) the time of diagnosis and therefore may not be representative of lifetime exposures or exposures during potentially critical windows of susceptibility during earlier life. Second, the lack of an association established between breast cancer risk factors and breast cancer risk in our study calls into question whether our controls may be overmatched to our cases. Although we excluded from our control group women diagnosed with atypical hyperplasia who carry an elevated risk of developing breast cancer, our control group did include women with other proliferative benign breast lesions for whom recent evidence now suggests are at increased risk for breast cancer, albeit to a lesser degree [19]. Thus, inclusion in our control group of some women with benign breast conditions that are on the causal pathway between exposure and the development of breast cancer may have limited our ability to detect a risk if one truly exists. Third, PBDE levels are known to inversely correlate with age [18]. Although we attempted to frequency match by age, difficulties encountered in recruitment resulted in a skewed age distribution such that controls were significantly younger than cases. Thus, it is possible that our results may be partially biased by residual confounding by age, although alternative models with age adjusted on a continuous scale yield similar results. Last, the study sample was small, limiting our power to detect risks.
Nevertheless, our study has a number of strengths. It was conducted among a population of women with high levels of exposures [20]. Despite being collected during an earlier time period, before the use of PBDEs began to be phased-out, median levels in our study population were higher than those reported in 2003–2004 national data. Also, our specimens were collected among women who had no prior history of treatment with radiation or tamoxifen and were predominantly collected as part of a diagnostic procedure, minimizing the degree to which breast cancer treatment might alter body burden measures of these compounds. Finally, our study relied on adipose levels of PBDEs, which is the preferred tissue to measure steady state concentrations of lipophilic contaminants as they are less influenced by surges in blood lipids than sera measurements [14].
This study is the first human health study to report on the risks of breast cancer associated with body burden levels of PBDEs. Overall, data on the carcinogenic effects of PBDEs in humans are extremely sparse. There have been reports of elevated cancer rates among populations living in the Zhejiang Province of China, an area of intense e-waste recycling, with documented high levels of PBDE environmental contamination [21, 22]. To date, only two small case–control studies have been published on PBDEs and cancer risk. A small population-based study conducted in Sweden found a modest, but statistically nonsignificant, increase in risk for non-Hodgkins lymphoma associated with adipose levels of Tetra-BDEs (found in the Penta commercial formulation), based on 19 cases [23]. Another small Swedish case–control study (31 cases) conducted by the same investigators reported significantly increased risks of testicular cancer among men associated with maternal serum levels of total PBDEs (OR = 2.9, 95% CI: 3.2 (1.1–8.9), although not associated with personal serum levels [24].
Despite the dearth of human health data, there is a strong biologic rationale for suspecting a link between PBDE exposures and breast cancer. The chemical structure and toxicological properties of PBDEs are very similar to the polychlorinated biphenyls and other dioxin-like compounds that are known carcinogens [25]. Limited data suggest the lower-brominated congeners have the ability to induce genetic recombination in mammalian cells and form macromolecular adducts in rodents [25]. Additionally, through their well-established endocrine-disrupting effects, PBDEs may exert a causal effect through a hormonal pathway for hormonally mediated cancers such as that of the breast [2, 10–12]. Given the growing chorus of public concern regarding the alarmingly high body burden levels of PBDEs among Americans [26], coupled with the efforts of policy makers to enact regulatory action to control these exposures in the face of virtually no human health data, more study is clearly warranted. Future studies would benefit from a larger sample size, a more representative control series, and/or a prospective study design.
References
Costa LG, Giordano G, Tagliaferri S, Caglieri A, Mutti A (2008) Polybrominated diphenyl ether (PBDE) flame retardants: environmental contamination, human body burden and potential adverse health effects. Acta Biomed 79(3):172–183
Darnerud PO (2008) Brominated flame retardants as possible endocrine disrupters. Int J Androl 31(2):152–160
Bradman A, Fenster L, Sjodin A, Jones RS, Patterson DG Jr., Eskenazi B (2007) Polybrominated diphenyl ether levels in the blood of pregnant women living in an agricultural community in California. Environ Health Perspect 115(1):71–74
Hites RA (2004) Polybrominated diphenyl ethers in the environment and in people: a meta-analysis of concentrations. Environ Sci Technol 38(4):945–956
Parkin DM, Whelan SL, Ferlay J, Raymond L, Young J (eds) (1997) Cancer incidence in five continents. International Agency for Research on Cancer (IARC), Lyon, France
Fischer D, Hooper K, Athanasiadou M, Athanassiadis I, Bergman A (2006) Children show highest levels of polybrominated diphenyl ethers in a California family of four: a case study. Environ Health Perspect 114(10):1581–1584
Petreas M, She J, Brown FR, Winkler J, Windham G, Rogers E, Zhao G, Bhatia R, Charles MJ (2003) High body burdens of 2, 2′,4,4′-tetrabromodiphenyl ether (BDE-47) in California women. Environ Health Perspect 111(9):1175–1179
Zota AR, Rudel RA, Morello-Frosch RA, Brody JG (2008) Elevated house dust and serum concentrations of PBDEs in California: unintended consequences of furniture flammability standards? Environ Sci Technol 42(21):8158–8164
Schecter A, Papke O, Tung KC, Joseph J, Harris TR, Dahlgren J (2005) Polybrominated diphenyl ether flame retardants in the U.S. population: current levels, temporal trends, and comparison with dioxins, dibenzofurans, and polychlorinated biphenyls. J Occup Environ Med 47(3):199–211
Legler J (2008) New insights into the endocrine disrupting effects of brominated flame retardants. Chemosphere 73(2):216–222
Meerts IA, Letcher RJ, Hoving S, Marsh G, Bergman A, Lemmen JG, van der Burg B, Brouwer A (2001) In vitro estrogenicity of polybrominated diphenyl ethers, hydroxylated PDBEs, and polybrominated bisphenol A compounds. Environ Health Perspect 109(4):399–407
Hamers T, Kamstra JH, Sonneveld E, Murk AJ, Kester MH, Andersson PL, Brouwer A (2006) In vitro profiling of the endocrine-disrupting potency of brominated flame retardants. Toxicol Sci 92(1):157–173
Reynolds P, Hurley SE, Petreas M, Goldberg DE, Smith D, Gilliss D, Mahoney ME, Jeffrey SS (2005) Adipose levels of dioxins and risk of breast cancer. Cancer Causes Control 16(5):525–535
Petreas M, Smith D, Hurley S, Jeffrey SS, Gilliss D, Reynolds P (2004) Distribution of persistent, lipid-soluble chemicals in breast and abdominal adipose tissues: lessons learned from a breast cancer study. Cancer Epidemiol Biomarkers Prev 13(3):416–424
Brown FR, Winkler J, Visita P, Park JS, Petreas M (2007) Simultaneous analysis of PCBs and polybrominated diphenyl ethers (PBDEs) in human adipose using GC/MS/MS. Organohalogen Compounds 69:1199–1202
SAS Institute I: SAS 9. In. 9 edn. Cary, NC: SAS Institute Inc.; 2007
R Development Core Team (2009) R: a language and environment for statistical computing, R foundation for statistical computing, Vienna, Austria
Sjodin A, Wong LY, Jones RS, Park A, Zhang Y, Hodge C, Dipietro E, McClure C, Turner W, Needham LL et al (2008) Serum concentrations of polybrominated diphenyl ethers (PBDEs) and polybrominated biphenyl (PBB) in the United States population: 2003–2004. Environ Sci Technol 42(4):1377–1384
Kabat GC, Jones JG, Olson N, Negassa A, Duggan C, Ginsberg M, Kandel RA, Glass AG, Rohan TE (2010) A multi-center prospective cohort study of benign breast disease and risk of subsequent breast cancer. Cancer Causes Control 21(6):821–828
Petreas M, Nelson D, Brown FR, Goldberg D, Hurley S, Reynolds P (2011) High concentrations of polybrominated diphenylethers (PBDEs) in breast adipose tissue of California women. Environ Int 37(1):190–197
Zhao G, Wang Z, Dong MH, Rao K, Luo J, Wang D, Zha J, Huang S, Xu Y, Ma M (2008) PBBs, PBDEs, and PCBs levels in hair of residents around e-waste disassembly sites in Zhejiang Province, China, and their potential sources. Sci Total Environ 397(1–3):46–57
Zhao G, Wang Z, Zhou H, Zhao Q (2009) Burdens of PBBs, PBDEs, and PCBs in tissues of the cancer patients in the e-waste disassembly sites in Zhejiang, China. Sci Total Environ 407(17):4831–4837
Hardell L, Lindstrom G, van Bavel B, Wingfors H, Sundelin E, Liljegren G (1998) Concentrations of the flame retardant 2,2′,4,4′-tetrabrominated diphenyl ether in human adipose tissue in Swedish persons and the risk for non-Hodgkin’s lymphoma. Oncol Res 10(8):429–432
Hardell L, Bavel B, Lindstrom G, Eriksson M, Carlberg M (2006) In utero exposure to persistent organic pollutants in relation to testicular cancer risk. Int J Androl 29(1):228–234
McDonald TA (2002) A perspective on the potential health risks of PBDEs. Chemosphere 46(5):745–755
Schmidt K (2004) Preventing fires, igniting questions. In: US News and World Report vol. 136, Washington; April 26: 70
Acknowledgments
This work was supported by the California Breast Cancer Research Program (Grants #2RB-0054 and 10IB-0061) and by the US Army Medical Research and Materiel Command (Grant #DAMD17-94-J-4429 P6003). The ideas and opinions expressed herein are those of the authors and endorsement by the Cancer Prevention Institute of California, Stanford University, or the California Department of Toxic Substances Control is not intended or should be inferred. The authors would like to thank all the women who participated in the study; Ms. M. Suzuki and Ms. A. Rothblatt who interviewed the women; Dr. Dawn LeManne who helped initiate the study; Drs. K. O’Neal, E. Mahoney, and L Bailey for assistance in recruiting patients; and Lynn Brissette and the other surgical staff who assisted in this effort.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hurley, S., Reynolds, P., Goldberg, D. et al. Adipose levels of polybrominated diphenyl ethers and risk of breast cancer. Breast Cancer Res Treat 129, 505–511 (2011). https://doi.org/10.1007/s10549-011-1481-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1481-7