Abstract
Previous studies showing the presence of antibodies against tumor-associated antigens in healthy individuals suggest that antibody-dependent cell cytotoxicity (ADCC) might play a role in the development of breast cancer. We hypothesized that functional polymorphisms in fragment c gamma receptor (FcgR) genes were associated with breast cancer risk. We conducted hospital-based case–control studies of patients aged 20–74 years with invasive breast cancer, and matched controls from medical checkup examinees in Nagano, Japan and from cancer-free patients in São Paulo, Brazil. A total of 869 pairs (403 Japanese, 80 Japanese Brazilians and 386 non-Japanese Brazilians) were genotyped for two single nucleotide polymorphisms (SNPs): a histidine (H)/arginine (R) polymorphism at position 131 of FcgRIIa (FcgRIIa H131R) and a valine (V)/phenylalanine (F) polymorphism at position 158 of FcgRIIIa (FcgRIIIa F158V). We found no statistically significant association between either of the two SNPs and breast cancer risk regardless of population. In analyses of the three populations combined, adjusted odds ratio (OR) was 0.93 [95% confidence interval (CI) 0.66–1.32] for women with the R/R versus H/H genotype of the FcgRIIa H131R polymorphism and 1.04 (95% CI 0.69–1.57) for the V/V versus F/F genotype of the FcgRIIIa F158V polymorphism. On combination of the two SNPs, compared to women with both the R/R genotype of the FcgRIIa H131R polymorphism and F/F genotype of the FcgRIIIa F158V polymorphism, the adjusted OR for women with both the H/H and V/V genotype was 0.68 (95% CI 0.37–1.27). In conclusion, our findings suggest that ADCC might not play a major role in the etiology of breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common malignancy in women in Japan and many other parts of the world [1, 2]. Although sex hormones, particularly estrogens, play an important role in the etiology of breast cancer [3], present knowledge has proved insufficient to allow the disease to be overcome, and the identification of other important etiological factors thus requires further study.
It has been hypothesized that the immune system recognizes malignant cells as foreign agents and eliminates them. Although several epidemiological studies have supported this hypothesis, only a few studies have investigated the role of the immune system in the etiology of breast cancer [4–6]. Natural killer (NK) cells are large granular lymphocytes that mediate innate immunity against pathogens and tumors. Natural cytotoxicity is believed to play an important role in host anti-cancer defense mechanisms. In their cohort study of 3,625 participants in Japan with 11-year follow-up, e.g., Imai and colleagues [5] showed that high cytotoxic activity of peripheral blood lymphocytes was associated with a decreased risk of total cancer, while Dewan et al. [6] recently reported that NK activities of peripheral blood mononuclear cells from breast cancer patients were significantly lower than those of healthy individuals.
NK cells are also capable of mediating antibody-dependent cell cytotoxicity (ADCC) against antibody-coated targets via the expression of a low-affinity receptor for IgG [fragment c gamma receptor (FcgR) III]. Many kinds of autoantibodies against tumor-associated antigens have been investigated, some of which are also detected in healthy control sera [7]. Anti-epithelial mucin (MUC1) antibodies, e.g., are frequently detected in healthy individuals, particularly in women during pregnancy and lactation [8, 9]. Notably, Forsman and colleagues [10] reported that serum from multiparous women, but not nulliparous women or men, contained antibodies which selectively mediated ADCC against established mammary carcinoma cell lines. Given that breast cancer risk is higher in nulliparous than multiparous women, this finding suggests that ADCC might play a role in the development of breast cancer.
Immune effector cells, including NK cells, recognize antibodies bound to target cells through FcgRs and elicit ADCC activity, which can be modulated by FcgR gene polymorphisms. At least two functional FcgR gene polymorphisms that may affect the killing function of immune effector cells have been identified: a histidine (H)/arginine (R) polymorphism at position 131 of FcgRIIa (FcgRIIa H131R) and a valine (V)/phenylalanine (F) polymorphism at position 158 of FcgRIIIa (FcgRIIIa F158V) [11–14]. The H allele of the FcgRIIa H131R polymorphism has higher binding efficiency to human IgG2 than the R allele, and confers enhanced phagocytic activity [13, 14]. The V allele of the FcgRIIIa F158V polymorphism has higher affinity for human IgG than the F allele and cells bearing this allele mediate ADCC more effectively than those with the F allele [11, 12]. In fact, ADCC is a potential anti-tumor mechanism behind targeted therapy with the humanized monoclonal antibody trastuzumab for human epidermal growth factor receptor 2 (HER2)-positive breast cancer [15]. FcgR gene polymorphisms have, therefore, been suggested to modulate the clinical efficacy of trastuzumab-based therapy in patients with metastatic HER2-positive breast cancer [16].
In addition to this putative effect of polymorphisms in the FcgR gene in modulating ADCC activity, roles in several other mechanisms in the immune system have been suggested, with FcgRs on leukocytes also modulating phagocytosis, clearance of immune complexes, superoxide generation, degranulation, cytokine production, and regulation of antibody production [17].
To better understand the role of the immune system in the etiology of breast cancer, we tested the hypothesis that polymorphisms in the FcgR gene are associated with the risk of breast cancer using data from hospital-based case–control studies in Nagano, Japan and São Paulo, Brazil.
Materials and methods
Study subjects
We conducted multicenter, hospital-based case–control studies of breast cancer in Japan and Brazil. In addition to determining lifestyle factors and genetic susceptibility to the risk of breast cancer, the protocols of these studies were also designed to compare potential risk factors among Japanese living in Nagano, Japan, and Japanese Brazilians and non-Japanese Brazilians living in São Paulo, Brazil [18, 19]. Eligible case patients were a consecutive series of female patients aged 20–74 years with newly diagnosed and histologically confirmed invasive breast cancer. Case patients were recruited between 2001 and 2005 at four hospitals in Nagano, and between 2001 and 2006 at eight hospitals in São Paulo. A total of 405 case patients (98%) participated in Nagano, and 83 Japanese Brazilian (91%) and 389 non-Japanese Brazilian case patients (99%) in São Paulo. In the Nagano study, eligible control subjects were selected from medical checkup examinees in two of the four hospitals who were confirmed not to have cancer. One control subject was matched for each case patient by age (within 3 years) and residential area during the study period. Among potential controls, one examinee declined participation and two declined the provision of blood samples. Consequently, we obtained written informed consent from 405 matched pairs. In the São Paulo study, eligible control subjects were preferentially selected from cancer-free patients who visited the same hospital as the index patients. One control was matched with each case by age (within 5 years) and ethnicity during the study period. Among potential control subjects, 22 patients declined participation (participation rate = 96%). Consequently, we obtained written informed consent from 472 matched pairs (83 for Japanese Brazilians and 389 for non-Japanese Brazilians). The study protocol was approved by CONEP (Comissão Nacional de Ética em Pesquisa), Brasília, Brazil and by the institutional review board of the National Cancer Center, Tokyo, Japan.
Data collection
Participants in Nagano were asked to complete a self-administered questionnaire, while those in São Paulo were given in-person interviews conducted by trained interviewers using a structured questionnaire. The two questionnaires contained closely similar questions concerning demographic characteristics, medical history, family history of cancer, menstrual and reproductive history, anthropometric factors, physical activity, and smoking habits.
Information on estrogen receptor (ER) and progesterone receptor (PR) status was obtained from medical records. Hormone receptor status was determined by either enzyme-linked immunoassay or immunohistochemical assay. Hormone receptor positivity values were determined either as specified by the laboratory that performed the assay or in accordance with the laboratory’s written interpretation thereof, or both.
Participants in Nagano provided blood at the time they returned their self-administered questionnaire, and those in São Paulo at the time of interview. Blood samples were divided into serum aliquots in Nagano and into plasma aliquots and buffy layers in São Paulo. All blood samples were shipped to the Epidemiology and Prevention Division, Research Center for Cancer Prevention and Screening, National Cancer Center, Tokyo, Japan and stored at −80°C until analysis.
Genotyping
Genomic DNA samples were extracted from peripheral blood using Qiagen FlexiGene® DNA Kits (Qiagen K.K., Tokyo, Japan) according to the manufacturer’s protocol. We genotyped two single nucleotide polymorphisms (SNPs), namely FcgRIIa H131R (rs1801274) and FcgRIIIa F158V (rs396991) by TaqMan® SNP Genotyping Assays (Applied Biosystems, Foster City, CA, USA). Cases and matched controls were analyzed in the same well by laboratory personnel who did not know the case–control status. The quality of genotyping was assessed by duplicate quality control samples (n = 140), with concordance rates of 100% for FcgRIIa H131R and 99% for FcgRIIIa F158V.
Statistical analysis
We excluded subjects whose DNA samples were not available, leaving a total of 869 pairs (403 Japanese, 80 Japanese Brazilians and 386 non-Japanese Brazilians). Comparison of baseline characteristics between cases and controls was evaluated by the Mantel–Haenszel test using matched-pair strata in each population. Genotype frequencies were tested for deviation from the Hardy–Weinberg equilibrium with the Chi-square test. Odds ratios (ORs) and 95% confidence intervals (CIs) of breast cancer for SNPs and their combination were calculated using a conditional logistic regression model. Stratified analyses according to menopausal status and parity were calculated using an unconditional logistic regression model. Tests for interaction were performed based on the difference between two likelihood ratios of the models with and without the interaction terms. Associations between SNPs and hormone receptor-defined breast cancer were assessed by an unconditional polytomous logistic regression model. The Wald test was used to test the null hypothesis that estimates were equal across hormone receptor-defined breast cancer subtypes. In addition to matching factors, the following variables were adjusted for as potential confounders: family history of breast cancer (yes, no), history of benign breast disease (yes, no), age at menarche (continuous), menopausal status and age at menopause [premenopausal women, age at menopause for postmenopausal women (<45, 46–49, 50–51, >52) for the three populations combined, (<47, 48–49, 50–51, >52) for Japanese, (<47, 48–49, 50–52, >53) for Japanese Brazilians, and (<43, 44–47, 48–50, >51) for non-Japanese Brazilians], number of births (0, 1, 2, 3, >4), age at first birth (<21, 22–24, 25–26, >27, nulliparous for the three populations combined; <23, 24–25, 26–27, >28, nulliparous for Japanese; <24, 25–26, 27–28, >29, nulliparous for Japanese Brazilians; and <18, 19–21, 22–24, >25, nulliparous for non-Japanese Brazilians), breast feeding (yes, no, nulliparous), body mass index (BMI) (continuous), alcohol drinking (no, occasional, regular drinkers), smoking status (never, past, current smokers), moderate physical activity in the past 5 years (no, less than 3 days/month, 1–4 days/week, more than 5 days/week) and vitamin supplement use (yes, no). All reported P values are two-sided, and significance level was set at P < 0.05. All statistical analyses were performed with SAS software version 9.1 (SAS Institute, Inc., Cary, NC).
Results
Characteristics of case patients and control subjects have been described elsewhere [18, 19]. For Japanese, the proportion of premenopausal women, current smokers, and vitamin supplement users was higher in cases than in controls; and cases tended to have a family history of breast cancer and history of benign breast disease. Cases were less likely than controls to breast-feed and be physically active. For Japanese Brazilians, cases were less likely than controls to give birth and be physically active. For non-Japanese Brazilians, the proportion of premenopausal women and current smokers was higher in cases than in controls, whereas the proportion of physically active women and vitamin supplement users was lower (data not shown).
Allele frequencies of the SNPs among controls in each population are presented in Table 1. Genotype frequencies of each SNP were consistent with the Hardy–Weinberg equilibrium. The prevalence of the minor allele in the FcgRIIa H131R polymorphism was lower in the Japanese and Japanese Brazilian controls than in the non-Japanese Brazilian controls, while that of the minor allele in the FcgRIIIa F158V polymorphism was similar among the three populations.
ORs for breast cancer by SNP are shown in Table 2. We found no statistically significant association between either of the two SNPs and breast cancer risk regardless of population. Further, no statistically significant association was observed in analyses of the three populations combined: adjusted ORs were 0.93 (95% CI 0.66–1.32) for women with the R/R versus H/H genotype of the FcgRIIa H131R polymorphism and 1.04 (95% CI 0.69–1.57) for the V/V versus F/F genotype of the FcgRIIIa F158V polymorphism.
We next calculated adjusted ORs according to the combination of the two SNPs (Table 3). Overall, we found no significant association. However, compared to women with both the R/R genotype of the FcgRIIa H131R polymorphism and the F/F genotype of the FcgRIIIa F158V polymorphism, the adjusted OR for women with both the H/H and V/V genotype was 0.68 (95% CI 0.37–1.27). In contrast, adjusted ORs were 1.90 (95% CI 0.42–8.69) for women with both the R/R and V/V genotype and 1.63 (95% CI 0.73–3.66) for women with both the H/R and V/V genotype.
We performed further stratified analyses by menopausal status. The association between the two SNPs and risk did not substantially differ between two strata regardless of population (data not shown). Moreover, stratified analyses by parity (nulliparous and parous) to determine whether parity modified the association between the two SNPs and risk showed no remarkable difference for either of the two SNPs (data not shown).
The association between these two SNPs in the FcgR gene and the risk of hormone receptor-defined breast cancer is shown in Table 4. Information on the combined ER and PR status of the breast tumor was available for 730 cases (84%). The following subtypes were used for modeling in an unconditional polytomous logistic regression model: positive for both receptors (ER+/PR+), ER-positive and PR-negative (ER+/PR−), negative for both receptors (ER−/PR−), and unknown. Overall, we found no remarkable difference in risk by hormone receptor-defined subtype.
Discussion
In these case–control studies, we found no statistically significant association between either of the two SNPs examined and breast cancer risk. Although we expected that women harboring the favorable H/H genotype of the FcgRIIa H131R polymorphism and V/V genotype of the FcgRIIIa F158V polymorphism would show more potent ADCC activity, as mentioned in “Introduction” [11–14], no statistically significant decrease in risk was seen, albeit that the adjusted OR was 0.68. To our knowledge, this is the first study to test the hypothesis that functional SNPs in the FcgR gene are associated with the risk of breast cancer. Our findings do not support this hypothesis and suggest that ADCC might not play a major role in the etiology of breast cancer.
We observed that the prevalence of the minor allele in the FcgRIIa H131R polymorphism was lower in the Japanese and Japanese Brazilian controls than in the non-Japanese Brazilian controls, while that of the minor allele in the FcgRIIIa F158V polymorphism was similar among the three populations, which is in general agreement with previous studies [16, 20, 21]. Although prevalence differed between the populations, no association was found for FcgRIIa H131R polymorphism regardless of population.
Several possible explanations for the observed absence of associations with breast cancer risk can be considered. First, we examined two SNPs, namely the FcgRIIa H131R and FcgRIIIa F158V polymorphisms. Although differences in the level of phagocytic or cytotoxic activities among genotypes of FcgRIIa H131R and FcgRIIIa F158V have been suggested [11–14], the absence of associations indicates that they might not be large enough to contribute to a difference in breast cancer risk among genotypes.
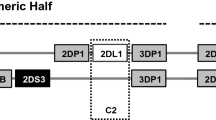
Second, FcgRs are expressed on leukocytes and are composed of three distinct classes: FcgRI, FcgRII, and FcgRIII. The latter two are further divided into FcgRIIa, FcgRIIb, and FcgRIIc, and FcgRIIIa and FcgRIIIb. FcgRI exhibits high affinity for IgG and can bind to monomeric IgG, whereas FcgRII and FcgRIII show weaker affinity for monomeric and hence can only interact effectively with multimeric immune complexes. FcgRIIa and FcgRIIIa activate FcgRs expressed on monocytes/macrophages and on both monocytes/macrophages and NK cells, respectively. Given that FcgRI exhibits high affinity for IgG, and that FcgRIIc on NK cells also induced ADCC [17, 22], the two SNPs in the FcgR gene we examined might not necessarily be the major determinants of inter-individual variation in ADCC or phagocytosis.
Third, although our study included a total of 869 pairs, it may not have had sufficient statistical power to detect a small increase or decrease in the risk of breast cancer. In fact, this study had approximately 80% statistical power, with a two-sided α error level of 5% and a proportion in the ‘heterozygous and minor homozygous’ group of 35% to detect a true OR of 1.32 or 0.74 for breast cancer among the ‘heterozygous and minor homozygous’ versus ‘major homozygous’ groups. While our findings, therefore, suggest that the two SNPs examined are not associated with an approximately 30% or greater increase or decrease in the risk of breast cancer, they cannot deny the possibility of a smaller increase or decrease in risk. In addition, analyses for the combination of FcgRIIa H131R and FcgRIIIa F158V polymorphisms showed a lower risk of breast cancer among women with the two favorable genotypes (H/H and V/V), albeit without statistical significance. This is partly because of the small proportion of women with these two favorable genotypes (5%), mandating a larger sample size.
Fourth, as a methodological issue, analyses for the three population combined might be subject to misclassification due to the difference in study methods between Japan and Brazil, albeit that the two studies were conducted under a similar protocol. For example, the control group in Japan was selected from medical checkup examinees with matching for age (within 3 years) and residential area, whereas that in Brazil was selected from cancer-free patients with matching for age (within 5 years) and ethnicity. If such difference leads to misclassification, this might also explain the observed absence of associations.
Although we found no overall association between these two SNPs in the FcgR gene and breast cancer risk, they might nevertheless be associated with breast cancer risk among specific subgroups. Analyses for the combination of the two SNPs showed a lower risk of breast cancer among women with the two favorable genotypes (H/H and V/V), which might be explained by the difference in ADCC. However, the reason for the higher risk of breast cancer among women with the R allele of the FcgRIIa H131R polymorphism and V/V genotype of the FcgRIIIa F158V polymorphism compared to those with both the R/R and F/F genotype is unclear. The adjusted ORs were not statistically significant, and these findings might merely be due to chance given the small number of subjects in these groups.
Hormonal milieu substantially differs between premenopausal and postmenopausal women, and previous studies have suggested differences in several risk factors between premenopausal and postmenopausal breast cancer [23, 24]. In addition, the age-specific breast cancer incidence rate in Japan shows a unique pattern: while rates in Western countries continue to increase after menopause, those in Japan increase before age 50 years but decrease or flatten after 50 years [25]. In this regard, although we were particularly interested in stratified analysis by menopausal status in this study, we found no remarkable difference for either of the two SNPs examined regardless of population.
Given that the presence of antibodies against tumor-associated antigens is essential for the induction of ADCC, the association between polymorphisms in the FcgR gene and breast cancer risk might be more prominent among women with antibodies against tumor-associated antigens than in those without these antibodies. Although antibodies against most tumor-associated antigens are found in only 0–3% of healthy individuals, anti-MUC1 antibodies are found in 23.3% for IgG (weighted average of five studies) and 53% for IgM (weighted average of two studies) [7]. It is known that women develop MUC1 and anti-MUC1 antibodies during pregnancy and breast-feeding, presumably due to changes within the breast or uterus that alter MUC1 expression, glycosylation, or shedding [8]. Moreover, serum from multiparous women contained antibodies which selectively mediated ADCC against established mammary carcinoma cell lines [10]. In this regard, however, our stratified analyses showed no association between the two SNPs in the FcgR gene and risk of breast cancer regardless of parity. Further studies using information on the presence of antibodies against tumor-associated antigens will clarify the association between polymorphisms in the FcgR gene and breast cancer risk.
Previous studies have shown that risk factors such as parity and BMI differ among breast cancer subtypes defined by ER or PR status [23, 26]. We, therefore, examined whether the association of the two SNPs in the FcgR gene differed across subtypes, but found no significant difference in risk. On the other hand, given that ADCC is a potential anti-tumor mechanism behind targeted therapy with the humanized monoclonal antibody trastuzumab for HER2-positive breast cancer [15], the two SNPs in the FcgR gene might be more closely associated with the risk of HER2-positive breast cancer. Moreover, gene expression profiling in tumor tissues suggests that breast cancers may be divided into molecular subtypes consisting of two ER+ types (luminal A and B) and three ER− types [HER2-expressing, basal-like, and unclassified (normal-like)], with distinctive clinical outcomes [27, 28]. It is, therefore, of particular interest to test the hypothesis that the association of the two SNPs in the FcgR gene might differ by HER2 status or molecular subtype. However, the present study was not designed to collect tumor tissues or information on HER2 status at the start of recruitment. Further large studies are required to test this hypothesis.
In conclusion, we found no statistically significant association between two SNPs in the FcgR gene and breast cancer risk. Our findings suggest that ADCC might not play a major role in the etiology of breast cancer. Further studies are needed to clarify the role of the immune system in the etiology of breast cancer.
Abbreviations
- ADCC:
-
Antibody-dependent cell cytotoxicity
- CI:
-
Confidence interval
- FcgR:
-
Fragment c gamma receptor
- HER2:
-
Human epidermal growth factor receptor 2
- MUC1:
-
Epithelial mucin
- NK:
-
Natural killer
- OR:
-
Odds ratio
- SNP:
-
Single nucleotide polymorphism
References
Ferlay J, Bray F, Pisani P et al (2004) GLOBOCAN 2002 cancer incidence, mortality and prevalence worldwide. IARC CancerBase No. 5, version 2.0. IARC Press, Lyon
Matsuda T, Marugame T, Kamo K et al (2009) Cancer incidence and incidence rates in Japan in 2003: based on data from 13 population-based cancer registries in the Monitoring of Cancer Incidence in Japan (MCIJ) Project. Jpn J Clin Oncol 39:850–858
Key T, Appleby P, Barnes I et al (2002) Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst 94:606–616
Finn OJ (2008) Cancer immunology. N Engl J Med 358:2704–2715
Imai K, Matsuyama S, Miyake S et al (2000) Natural cytotoxic activity of peripheral-blood lymphocytes and cancer incidence: an 11-year follow-up study of a general population. Lancet 356:1795–1799
Dewan MZ, Takada M, Terunuma H et al (2009) Natural killer activity of peripheral-blood mononuclear cells in breast cancer patients. Biomed Pharmacother 63:703–706
Reuschenbach M, von Knebel Doeberitz M, Wentzensen N (2009) A systematic review of humoral immune responses against tumor antigens. Cancer Immunol Immunother 58:1535–1544
Croce MV, Isla Larrain MT, Price MR et al (2001) Detection of circulating mammary mucin (Muc1) and MUC1 immune complexes (Muc1-CIC) in healthy women. Int J Biol Markers 16:112–120
Croce MV, Isla Larrain MT, Capafons A et al (2001) Humoral immune response induced by the protein core of MUC1 mucin in pregnant and healthy women. Breast Cancer Res Treat 69:1–11
Forsman LM, Jouppila PI, Andersson LC (1984) Sera from multiparous women contain antibodies mediating cytotoxicity against breast carcinoma cells. Scand J Immunol 19:135–139
Koene HR, Kleijer M, Algra J et al (1997) Fc gammaRIIIa-158V/F polymorphism influences the binding of IgG by natural killer cell Fc gammaRIIIa, independently of the Fc gammaRIIIa-48L/R/H phenotype. Blood 90:1109–1114
Dall’Ozzo S, Tartas S, Paintaud G et al (2004) Rituximab-dependent cytotoxicity by natural killer cells: influence of FCGR3A polymorphism on the concentration–effect relationship. Cancer Res 64:4664–4669
Salmon JE, Edberg JC, Brogle NL et al (1992) Allelic polymorphisms of human Fc gamma receptor IIA and Fc gamma receptor IIIB. Independent mechanisms for differences in human phagocyte function. J Clin Invest 89:1274–1281
Warmerdam PA, van de Winkel JG, Vlug A et al (1991) A single amino acid in the second Ig-like domain of the human Fc gamma receptor II is critical for human IgG2 binding. J Immunol 147:1338–1343
Spector NL, Blackwell KL (2009) Understanding the mechanisms behind trastuzumab therapy for human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol 27:5838–5847
Musolino A, Naldi N, Bortesi B et al (2008) Immunoglobulin G fragment C receptor polymorphisms and clinical efficacy of trastuzumab-based therapy in patients with HER-2/neu-positive metastatic breast cancer. J Clin Oncol 26:1789–1796
van Sorge NM, van der Pol WL, van de Winkel JG (2003) FcgammaR polymorphisms: implications for function, disease susceptibility and immunotherapy. Tissue Antigens 61:189–202
Iwasaki M, Hamada GS, Nishimoto IN et al (2009) Dietary isoflavone intake and breast cancer risk in case–control studies in Japanese, Japanese Brazilians, and non-Japanese Brazilians. Breast Cancer Res Treat 116:401–411
Shimada N, Iwasaki M, Kasuga Y et al (2009) Genetic polymorphisms in estrogen metabolism and breast cancer risk in case–control studies in Japanese, Japanese Brazilians and non-Japanese Brazilians. J Hum Genet 54:209–215
Wang SS, Cerhan JR, Hartge P et al (2006) Common genetic variants in proinflammatory and other immunoregulatory genes and risk for non-Hodgkin lymphoma. Cancer Res 66:9771–9780
Kyogoku C, Dijstelbloem HM, Tsuchiya N et al (2002) Fcgamma receptor gene polymorphisms in Japanese patients with systemic lupus erythematosus: contribution of FCGR2B to genetic susceptibility. Arthritis Rheum 46:1242–1254
Metes D, Ernst LK, Chambers WH et al (1998) Expression of functional CD32 molecules on human NK cells is determined by an allelic polymorphism of the FcgammaRIIC gene. Blood 91:2369–2380
Suzuki R, Orsini N, Saji S et al (2009) Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status—a meta-analysis. Int J Cancer 124:698–712
World Cancer Research Fund and American Institute for Cancer Research (2007) Food, nutrition, physical activity and the prevention of cancer: a global perspective. American Institute, Washington, DC
Curado MP, Edwards B, Shin HR et al (2007) cancer incidence in five continents, vol IX. IARC Scientific Publications No. 160. IARC, Lyon
Althuis MD, Fergenbaum JH, Garcia Closas M et al (2004) Etiology of hormone receptor-defined breast cancer: a systematic review of the literature. Cancer Epidemiol Biomark Prev 13:1558–1568
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874
Carey LA, Perou CM, Livasy CA et al (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295:2492–2502
Acknowledgments
This study was supported by a Grant-in-Aid for Research on Risk of Chemical Substances from the Ministry of Health, Labour and Welfare of Japan, and Grants-in-Aid for Scientific Research on Priority Areas (17015049) and for Young Scientists (B) (22700934) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan and the Japan Society for the Promotion of Science, and Foundation for Promotion of Cancer Research in Japan. We are grateful to the participants of the “São Paulo-Japan Breast Cancer Study Group”: T. Hanaoka, M. Kobayashi, J. Ishihara, S. Ikeda, and C. Nishimoto (Research Center for Cancer Prevention and Screening, National Cancer Center, Tokyo); C. I. Yamaguchi, C. M. Kunieda, and S. S. Sugama (Nikkei Disease Prevention Center, São Paulo); C. K. Taniguchi and J. A. Marques (Departamento de Ginecologia, Hospital Pérola Byington, São Paulo); M. R. Eichhorn (Departamento de Nutrição, Hospital Pérola Byington, São Paulo); M. M. Netto, M. S. Maciel, S. M. T. Carvalho, J. B. D. Collins, and C. E. M. Fontes (Departamento de Mastologia, Hospital A.C. Camargo, São Paulo); L. P. Kowalski and J. M. F. Toyota (Departamento de Cirurgia de Cabeça e Pescoço e Otorrinolaringologia, A. C. Camargo Hospital, São Paulo); E. M. Barbosa (Departamento de Mastologia, Instituto Brasileiro de Controle ao Câncer, São Paulo); O. Ferraro (Departamento de Mastologia, Hospital do Servidor Público Estadual Francisco Morato de Oliveira, São Paulo); E. H. Hotta and D. A. Petti (Instituto de Ginecologia e Mastologia, Hospital Beneficencia Portuguesa); and S. Mendes (Instituto Brasileiro de Mastologia e Ginecologia, Hospital Beneficencia Portuguesa).
Conflict of interest
All authors declare that we have no conflict of interest in connection with this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Iwasaki and N. Shimada contributed equally to this work.
Rights and permissions
About this article
Cite this article
Iwasaki, M., Shimada, N., Kasuga, Y. et al. Fragment c gamma receptor gene polymorphisms and breast cancer risk in case–control studies in Japanese, Japanese Brazilians, and non-Japanese Brazilians. Breast Cancer Res Treat 126, 497–505 (2011). https://doi.org/10.1007/s10549-010-1109-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-010-1109-3