Abstract
The Faslodex Investigation of Dose evaluation in Estrogen Receptor-positive advanced breast cancer (FINDER)2 study evaluated the efficacy, safety, and pharmacokinetics (PK) of three fulvestrant dosing regimens. FINDER2 enrolled Western postmenopausal women recurring or progressing after prior endocrine therapy. Primary endpoint: objective response rate (ORR); secondary endpoints: time to progression (TTP), clinical benefit rate (CBR), tolerability, and PK parameters. Patients were randomized to receive fulvestrant: 250 mg/month (approved dose [AD]); 250 mg plus loading dose (loading dose [LD]; 500 mg on day 0, 250 mg on days 14, 28, and monthly thereafter); or 500 mg (high dose [HD]; 500 mg/month plus 500 mg on day 14 of Month 1). Treatment continued until disease progression or discontinuation. 144 patients were randomized: fulvestrant AD (n = 47); LD (n = 51); HD (n = 46). ORRs were: 8.5% (95% confidence interval [CI]: 2.4, 20.4%), 5.9% (1.2, 16.2%), and 15.2% (6.3, 28.9%) in the AD, LD, and HD arms, respectively. CBRs were: 31.9% (95% CI: 19.1, 47.1%), 47.1% (32.9, 61.5%), and 47.8% (32.9, 63.1%) for the AD, LD, and HD arms, respectively. Median TTP (months) was numerically longer for HD (6.0) and LD (6.1) versus AD (3.1). Tolerability was similar across dosing regimens. Steady-state plasma fulvestrant concentrations were predictable and achieved earlier with LD and HD. While there appeared to be a trend toward improved efficacy with HD and LD versus AD, no significant differences could be shown. A parallel study (FINDER1) has reported similar findings in Japanese patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fulvestrant is an estrogen receptor (ER) antagonist without known agonist activity that is able to reduce cellular levels of estrogen and progesterone receptors. Fulvestrant has a distinct mechanism of action, compared with other endocrine (anti-estrogen) therapies, thereby lacking cross-resistance with other anti-cancer agents such as tamoxifen [1, 2].
On the basis of data from two large, worldwide Phase III clinical trials [3, 4], fulvestrant is licensed at a dose of 250 mg/month (approved dose; AD) for the treatment of postmenopausal women with advanced breast cancer following progression or recurrence after prior endocrine therapy. Although fulvestrant AD has established efficacy in this setting, it has been hypothesized that alternative dosing regimens may improve efficacy even further [5].
To address this question, the Faslodex Investigation of Dose evaluation in Estrogen Receptor-positive (ER+) advanced breast cancer (FINDER) 1 and 2 studies have evaluated the efficacy, tolerability, and pharmacokinetic (PK) profiles of three different fulvestrant dose regimens in postmenopausal women with advanced breast cancer, as follows:
-
1.
AD (250 mg/month)
-
2.
250 mg loading dose (LD) regimen (500 mg on day 0 and 250 mg on days 14 and 28 of Month 1, and 250 mg every 28 days thereafter)
-
3.
High-dose (HD) regimen (500 mg/month plus 500 mg on day 14 of Month 1).
Here, we describe the results from FINDER2, which has been performed in a predominantly Western (i.e., non-Japanese) patient population.
Methods
Study design and treatment
FINDER2 (9238IL/0068; NCT00313170) was a randomized, double-blind, parallel-group, international, Phase II study conducted across 34 centers in eight countries: Belgium, Canada, Czech Republic, France, Hungary, Poland, Romania, and Turkey.
Patients were randomized 1:1:1 to one of the three fulvestrant dosing regimens (AD, LD, or HD). Treatment continued until patients experienced disease progression, or until any other criterion for discontinuation was met: voluntary discontinuation, safety concerns (according to the investigators’ judgment), non-compliance, or lost to follow-up.
Patients
FINDER2 enrolled postmenopausal women, all with measurable disease and documented ER+ (≥10% positive staining by immunohistochemistry), locally advanced/metastatic breast cancer. Eligible patients had: relapsed during or within 12 months of completion of adjuvant endocrine therapy; progressed after endocrine therapy started ≥12 months after the completion of adjuvant endocrine treatment; or progressed after first-line endocrine therapy for patients with de novo advanced breast cancer.
Patients were excluded if they had: life-threatening visceral metastases; received more than one previous regimen of systemic anti-cancer therapy (other than one regimen of endocrine treatment for advanced disease); extensive radiation therapy or systemic anti-cancer therapy within 4 weeks prior to randomization; abnormal laboratory values or a severe concomitant condition.
All patients provided written informed consent and the study was performed in accordance with the Declaration of Helsinki and was consistent with International Conference on Harmonization Good Clinical Practice.
Efficacy assessments
The primary study endpoint was the objective response rate (ORR) of patients treated with fulvestrant AD, LD, or HD, evaluated according to Response Evaluation Criteria In Solid Tumors (RECIST) criteria [6]. The best overall response for each patient was categorized as a response (complete response or partial response) or a non-response (stable disease, progressive disease, or not evaluable).
Secondary endpoints included time to progression (TTP), clinical benefit rate (CBR), and duration of response (DoR). All endpoints were evaluated according to RECIST criteria [6].
Pharmacokinetic parameters
Plasma samples for PK analysis were collected from patients who consented to PK measurement. Blood samples (4 ml) were drawn at baseline and prior to injection on days 14, 28, 56, and 84. Two additional samples were collected between days 5 and 10 and days 33 and 38. Drug concentration–time data were analyzed with NONMEM V5.0, using a non-linear mixed-effects model approach. The primary PK parameters were fulvestrant clearance and volume of distribution at steady state, and secondary parameters of maximum plasma concentration (C max), time to maximum plasma concentration (t max), minimum plasma concentration (C min), area under plasma concentration time curve from zero to the end of the dosing interval (AUC0−τ), and half life (t ½) were derived.
Safety assessments
The safety and tolerability of the three fulvestrant dosing regimens were assessed by continuous evaluation of adverse events (AEs), clinical laboratory tests, vital signs, electrocardiogram (ECG), and physical examinations. Safety assessments were performed at baseline, throughout the study period, and up to 8 weeks after the last injection of study medication.
Statistical analysis
Overall, 43 patients per group were required for 90% probability that the best dose regimen by response rate be correctly selected, assuming that the lowest response rate was 19.2% (based on results for AD in previous studies) and that the difference in response rate between the best and next-best dose regimen was 15%. To allow for drop-out, a total of 135 patients were to be recruited to this study (45 patients per group). No formal hypothesis tests were planned for the efficacy endpoints.
Results
Patients
Overall, 144 patients were randomized to treatment (intent-to-treat population); fulvestrant AD (n = 47), LD (n = 51), and HD (n = 46). One patient in the LD group did not receive treatment and was excluded from the safety population. Patient disposition throughout the study is shown in Fig. 1.
Baseline characteristics, including treatment history, were generally well balanced across the treatment groups, with no major discrepancies between arms. The majority of patients were Caucasian (98.6%) and median age across the groups was 67 (range 38–88) years (Table 1). All patients enrolled were ER+; approximately two-thirds of patients (65.3%) were progesterone receptor-positive as well as ER+. Despite all tumors being confirmed as ER+, some appeared to have the clinical behavior of a relatively endocrine-resistant tumor, with many patients relapsing either during adjuvant endocrine therapy (39.6%) or while receiving first-line endocrine treatment for de novo advanced breast cancer (37.5%) (Table 1). Only 18.1% of all tumors showed a late recurrence (i.e., >12 months after completion of adjuvant endocrine treatment).
Efficacy
Comparison of data across the three treatment arms shows that fulvestrant AD, LD, and HD had similar efficacy (Table 2). Although ORR was numerically lower with the fulvestrant AD (8.5%) and LD (5.9%) regimens compared with HD (15.2%), the 95% confidence intervals (CIs) for all three treatment arms were overlapping. Similarly, for the CBRs observed with fulvestrant AD (31.9%), LD (47.1%), and HD (47.8%) the 95% CIs for all three treatment arms also overlapped (Table 2).
While the estimated median TTP was numerically shorter with fulvestrant AD (3.1 months; Fig. 2), compared with the LD and HD arms (6.1 and 6.0 months, respectively), the incidence of progression events was similar between groups (AD: 35; LD: 31, and HD: 34 events, respectively).
The low number of responders in all treatment arms prevented meaningful assessment of DoR.
Pharmacokinetics
In this study, a two-compartment model with first-order absorption and first-order elimination was fitted to the concentration–time data from the 72 patients who consented to PK measurements. Plots of the observed versus population-predicted fulvestrant concentrations demonstrated a reasonable overall fit of the model to the PK data (Fig. 3).
The mean apparent clearance of fulvestrant was 31.0 l/h; inter-individual variability (IIV) was 39%. The mean apparent volume of distribution at steady state was 56300 l (IIV 40%), which was similar to values determined previously with fulvestrant AD [7]. Residual variability was estimated at 22%.
In the fulvestrant AD arm, steady-state concentrations were approached during the third month of dosing (Table 3; Fig. 3). The inclusion of an additional dose of fulvestrant at day 14 in the LD and HD regimens led to the achievement of steady-state fulvestrant concentrations in the first month of dosing. A higher C min for the LD regimen and a similar C min for the HD regimen demonstrate this in the first versus the third month of dosing for both the LD and HD regimens (Table 3; Fig. 3).
At month 3, C min and the AUC were similar for the AD and LD regimens, whereas these parameters were approximately doubled with the HD regimen. This indicates that the PK of fulvestrant is linear and predictable in this study (Table 3).
Safety
All three fulvestrant dose regimens were well tolerated, with no differences observed between the safety profiles. The incidence of AEs was generally similar across the three treatment regimens: 76.6, 72.0, and 69.6% in the AD, LD, and HD groups, respectively, and there was no evidence of a dose response for any of the AE categories.
Few patients experienced serious AEs (SAEs) with a non-fatal outcome (4, 9, and 4 patients in the AD, LD, and HD arms, respectively), with no clustering of event types. Of these, only pleural effusion and pulmonary embolism were reported in more than one patient (two patients each). One SAE (ischemic stroke) was judged by the investigator to be related to treatment (AD regimen). Overall, five patients died during the study; two patients due to progressive disease and three patients (2.1%) due to an AE (pulmonary embolism, squamous cell lung cancer, and general physical health deterioration). Of these, one death (pulmonary embolism) was considered by the investigator to be related to treatment (AD regimen).
The most frequently reported treatment-related AEs were injection-site pain, hot flash, and fatigue (Table 4). Overall, six patients (4.2%) discontinued from the study due to an AE (2, 3, and 1 patients in the AD, LD, and HD arms, respectively). Furthermore, there were no clinically important findings or abnormalities in hematology, clinical chemistry, ECG, vital signs, or physical examinations in any of the treatment groups.
Discussion
Data from this Phase II study showed that fulvestrant AD, LD, and HD have similar efficacy and tolerability in a population of Western postmenopausal women with ER+ locally advanced/metastatic breast cancer that had relapsed or progressed after prior endocrine (anti-estrogen) therapy. There appeared to be a trend toward improved efficacy with HD and LD compared with AD, but no clear differences could be proven, given that the 95% CIs for all three treatment arms overlapped.
A number of studies have previously investigated the efficacy and tolerability of fulvestrant LD and HD. Fulvestrant LD data have been reported in the Evaluation of Faslodex versus Exemestane Clinical Trial (EFECT) study involving postmenopausal women with advanced breast cancer who have experienced progression or recurrence during treatment with a non-steroidal aromatase inhibitor [8]. In this setting, fulvestrant LD and exemestane appeared to be efficacious and well tolerated.
The efficacy and safety of a higher-dose fulvestrant regimen has been examined in the Fulvestrant First-line Study Comparing Endocrine Treatments (FIRST) study, which evaluated fulvestrant HD versus anastrozole in the first-line advanced breast cancer setting. The FIRST study demonstrated that fulvestrant HD significantly prolongs TTP compared with anastrozole [9]. Furthermore, a recent, small Phase II study has reported that fulvestrant HD was efficacious and well tolerated in postmenopausal women who had not been previously treated with endocrine therapy [10]. In the neoadjuvant setting, results from the Neoadjuvant Endocrine Therapy for Women with Estrogen-Sensitive Tumors (NEWEST) trial demonstrated that fulvestrant HD reduced ER and the proliferation biomarker Ki67 to a significantly greater extent than AD, and that both doses were well tolerated [11]. The efficacy trends observed in the FINDER2 study appear to support the findings from NEWEST, but it is difficult to draw firm conclusions. However, the good tolerability of both HD and LD has been a consistent observation across all these studies, including FINDER2.
Recent data from the large Phase III Comparison of Faslodex in Recurrent or Metastatic breast cancer (CONFIRM) study, which compared the clinical benefit of fulvestrant HD versus AD in postmenopausal women with ER+ advanced breast cancer have shown that TTP was significantly longer for fulvestrant HD (n = 362) than AD (n = 374) (hazard ratio 0.80; 95% CI, 0.68, 0.94; P = 0.006), corresponding to a 20% reduction in the risk of progression. Fulvestrant HD also showed numerical advantages in other secondary efficacy endpoints while keeping a similar tolerability profile to fulvestrant AD. Overall, these results suggest that the risk:benefit profile for fulvestrant HD is better than that of AD [12].
In FINDER2, the PK profile of fulvestrant AD was comparable to that previously reported in Western populations [7], with steady-state concentrations approached during the third month of dosing. As expected, higher steady-state plasma levels of fulvestrant were reached with the HD regimen, and inclusion of a day 14 dose accelerated the achievement of steady-state concentrations, in agreement with PK results from the EFECT trial [13].
Despite notable PK differences between regimens in our study, and while there appeared to be a trend toward improved efficacy with HD and LD compared with AD, no clear differences in clinical efficacy could be proven, as indicated by the relatively low ORRs observed, which did not permit any differences between treatments to become apparent. These low ORRs were somewhat surprising since, according to baseline characteristics, all tumors were ER+. In spite of this, some tumors appeared to behave as if they were relatively resistant to endocrine therapy, i.e., baseline data indicated that only 60% of patients had not recurred during adjuvant endocrine therapy and 62% had not progressed while receiving endocrine therapy for de novo advanced breast cancer. Overall, only 18% of tumors showed a late recurrence (i.e., >12 months after completion of adjuvant endocrine treatment), which represents the patient subgroup with endocrine-sensitive tumors. Furthermore, during the study, 43.9% of patients showed disease progression. The lack of endocrine sensitivity in some patients may explain the relatively low response rates reported in this study. Nonetheless, these results are comparable to previous data from the EFECT trial, in which patients treated with fulvestrant LD achieved an ORR of 7.4% and a CBR of 32.2% (6.7 and 31.5% with exemestane, respectively) [8]. After 6 months, 70% of patients overall had experienced disease progression, implying that, similarly to FINDER2, the majority of enrolled patients had hormone-insensitive disease [8]. Overall, the findings from FINDER2 confirm the clinical feasibility, efficacy, and tolerability of the fulvestrant HD and LD regimens in this difficult-to-treat patient population.
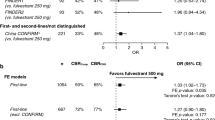
A parallel study (FINDER1) using the same fulvestrant dosing regimens in a Japanese patient population has also shown comparable efficacy results. In FINDER1, ORR was similar across the three dose regimens (11.1, 17.6, and 10.6% for fulvestrant AD, LD, and HD, respectively), with overlapping CIs. Median TTP was 6.0, 7.5, and 6.0 months and CBRs were 42.2, 54.9, and 46.8% for fulvestrant AD, LD, and HD, respectively [14]. The two studies also appeared to have similar PK and safety outcomes; in FINDER1, PK steady state was reached earlier with fulvestrant LD and HD and all three doses were well tolerated [14].
Taken together, the results from the two FINDER studies suggest that there were no major differences in the efficacy, tolerability, and PK of the three fulvestrant dosing regimens in either Japanese or non-Japanese patients. Therefore, ethnicity is unlikely to have an impact on the success of fulvestrant treatment. While fulvestrant HD did not show superior efficacy versus fulvestrant AD in these two small Phase II studies, the CONFIRM study, which was a much larger, Phase III trial has clearly demonstrated the clinical benefits of fulvestrant HD over AD in the management of postmenopausal women with advanced breast cancer.
References
Wakeling AE (2000) Similarities and distinctions in the mode of action of different classes of antioestrogens. Endocr Relat Cancer 7:17–28
Howell A (2006) Fulvestrant (‘Faslodex’): current and future role in breast cancer management. Crit Rev Oncol Hematol 57:265–273
Howell A, Robertson JFR, Quaresma Albano J et al (2002) Fulvestrant, formerly ICI 182, 780, is as effective as anastrozole in postmenopausal women with advanced breast cancer progressing after prior endocrine treatment. J Clin Oncol 20:3396–3403
Osborne CK, Pippen J, Jones SE et al (2002) Double-blind, randomized trial comparing the efficacy and tolerability of fulvestrant versus anastrozole in postmenopausal women with advanced breast cancer progressing on prior endocrine therapy: results of a North American trial. J Clin Oncol 20:3386–3395
Robertson JFR (2007) Fulvestrant (Faslodex)—how to make a good drug better. Oncologist 12:774–784
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Robertson JF, Erikstein B, Osborne KC et al (2004) Pharmacokinetic profile of intramuscular fulvestrant in advanced breast cancer. Clin Pharmacokinet 43:529–538
Chia S, Gradishar W, Mauriac L et al (2008) Double-blind, randomized placebo controlled trial of fulvestrant compared with exemestane after prior nonsteroidal aromatase inhibitor therapy in postmenopausal women with hormone receptor-positive, advanced breast cancer: results from EFECT. J Clin Oncol 26:1664–1670
Robertson JFR, Llombart A, Rolski J et al (2009) Activity of fulvestrant 500 mg versus anastrozole 1 mg as first-line treatment for advanced breast cancer: results from the FIRST study. J Clin Oncol 27:4530–4535
Come SE, Parker LM, wulf G et al (2009) Tolerability and efficacy of 500 mg fulvestrant in postmenopausal women with estrogen receptor (ER)+ advanced breast cancer. J Clin Oncol ASCO Annual Meeting Proceedings 27: (abstr 1050)
Kuter I, Hegg R, Singer CF et al (2007) Fulvestrant 500 mg vs 250 mg: first results from NEWEST, a randomized, phase II neoadjuvant trial in postmenopausal women with locally advanced, estrogen receptor-positive breast cancer. Breast Cancer Res Treat 106:S7 (abstr 23)
Di Leo A, Jerusalem G, Petruzelka L et al (2009) CONFIRM: a phase III, randomized, parallel-group trial comparing fulvestrant 250 mg vs. fulvestrant 500 mg in postmenopausal women with estrogen receptor-positive advanced breast cancer. Cancer Res 69:491s (abstr 25)
McCormack P, Sapunar F (2008) Pharmacokinetic profile of the fulvestrant loading dose regimen in postmenopausal women with hormone receptor-positive advanced breast cancer. Clin Breast Cancer 8:347–351
Sagara Y, Ohno S, Iwata H et al (2009) Three dose regimens of fulvestrant in advanced breast cancer: results from a double-blind, comparative study (FINDER1). In: ASCO breast cancer symposium, San Francisco, CA, USA, October 8–10 (abstr 241)
Acknowledgments
The authors would like to thank Katrina de Saram, PhD, formerly from Complete Medical Communications, who provided medical writing support funded by AstraZeneca. This study was funded by AstraZeneca Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pritchard, K.I., Rolski, J., Papai, Z. et al. Results of a phase II study comparing three dosing regimens of fulvestrant in postmenopausal women with advanced breast cancer (FINDER2). Breast Cancer Res Treat 123, 453–461 (2010). https://doi.org/10.1007/s10549-010-1022-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-010-1022-9