Abstract
In a previous study from our laboratory, high tumor levels of tissue inhibitor of metalloproteinases-1 (TIMP-1) have been associated with an adverse response to chemotherapy in metastatic breast cancer suggesting that TIMP-1, which is known to inhibit apoptosis, may be a new predictive marker in this disease. The purpose of this study was to investigate the association between TIMP-1 and objective response to chemotherapy in an independent patient population consisting of patients with metastatic breast cancer from Sweden and Denmark. TIMP-1 was measured using ELISA in 162 primary tumor extracts from patients who later developed metastatic breast cancer and these levels were related to the objective response to first-line chemotherapy. Increasing levels of TIMP-1 were associated with a decreasing probability of response to treatment, reaching borderline significance (OR = 1.59, 95% CI: 0.97–2.62, P = 0.07). This OR is very similar to the result from our previous study. Increasing levels of TIMP-1 were also associated with a shorter disease-free survival and overall survival, however, not statistically significant. The results from the present study support previous data that TIMP-1 is associated with objective response to chemotherapy for metastatic breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The majority of women diagnosed with breast cancer are offered adjuvant systemic treatment, i.e., chemotherapy and/or endocrine therapy, following surgical removal of the primary tumor. However, a large proportion of these women do not benefit from the treatment, but they may still suffer from the toxic side effects caused by the drugs. Especially, anthracyclines can cause irreversible cardiac toxicity. Today, only few predictive markers are available in breast cancer, including the presence of estrogen (ER) and progesterone receptors (PR) for predicting response to endocrine treatment and HER-2 expression for predicting the response to trastuzumab [1–3]. At present, no markers to predict the response to chemotherapy in general or to specific types of chemotherapy are in routine clinical use, although amplification/deletion of topoisomerase II alpha (topo IIα) seems promising in relation to treatment with anthracyclines [4–6]. Therefore, additional predictive markers need to be identified to enable individualized treatment of the patients.
Tissue inhibitor of metalloproteinases-1 (TIMP-1) has proven to be a promising marker in breast cancer carrying both prognostic [7–11] and, as shown more recently, predictive information [12–15]. For example, our laboratory has previously demonstrated that high primary tumor tissue levels of TIMP-1 were significantly associated with a poor response to the most frequently used chemotherapeutic drugs in metastatic breast cancer [14]. More recently, we have shown that TIMP-1 immunoreactivity in the cancer cells is significantly associated with benefit from adjuvant anthracycline treatment in patients with primary breast cancer [15]. These clinical findings have also been supported by in vitro cell studies [16, 17]. For example, murine fibrosarcoma cells deficient of the TIMP-1 gene were shown to be considerably more sensitive to chemotherapy compared with their genetically identical wild-type controls [16]. Likewise, transfected MCF10A cells over-expressing TIMP-1 were less sensitive to adriamycin compared with non-transfected cells [17].
The aim of the present study was to further investigate the association between tumor tissue TIMP-1 and the effect of chemotherapy in patients with metastatic breast cancer. Therefore, using ELISA, we measured TIMP-1 in primary tumor tissue extracts from 162 patients with metastatic breast cancer and related the measurements to the objective response to first-line chemotherapy (primarily anthracycline-containing regimens). Whenever applicable, the REMARK recommendations for reporting of tumor marker studies were followed [18].
Materials and methods
Patients and treatment. This study included two retrospective patient populations: (1) a patient population with available detergent-extracted tumor tissue extracts (n = 43) and (2) a patient population with available cytosolic tumor tissue extracts (n = 119). These two patient populations were pooled resulting in a total population of 162 patients. Patients were included in the present study provided that (1) tumor tissue extracts from the primary tumor were available, (2) they had had recurrence of disease (recurrence was defined as appearance of metastatic cancer lesions after primary surgery as determined by biopsy and/or other relevant diagnostic procedures), (3) they had received chemotherapy (≥3 cycles) for this recurrence, and (4) hospital medical records were available including data on objective response. The study was approved by the local ethical committees.
Patients with detergent-extracted tissues: This patient population consisted of a cohort of 43 Danish patients who underwent surgery for primary breast cancer from 1989 to 1993. Patient characteristics and pathological findings were registered by the Danish Breast Cancer Cooperative Group (DBCG). Clinicopathological characteristics of these patients have been described previously [9, 19] and are summarized in Table 1.
Patients with cytosolic extracts: This patient population consisted of both Swedish and Danish patients. The Swedish patients consisted of 110 women from the South Sweden Health Care Region, and they had all undergone surgery for primary breast cancer during the period 1987–2000. Nine Danish patients were operated during the period 1995–1999 and were enrolled in the Scandinavian Breast Group Trial, study 9403 [20]. Characteristics of these patients are also summarized in Table 1.
In general, surgical procedures consisted of modified radical mastectomy or breast conserving surgery and axillary lymph node dissection. Radiotherapy was offered to patients undergoing breast conserving surgery as well as patients with invasion of the deep resection margin after mastectomy and to patients with 4 or more positive lymph nodes. Median age at surgery was 53 years (range 33–74 years). Adjuvant therapy included cyclophosphamide, methotrexate, and 5-fluorouracil (CMF, 52 patients) or cyclophosphamide, epirubicin, and 5-fluorouracil (CEF, 4 patients), radiotherapy (77 patients), and/or endocrine treatment (60 patients). All patients received first-line chemotherapy for their metastatic disease: 146 received anthracycline-containing therapy, 9 patients received CMF, and 7 patients received other types of chemotherapy (vinorelbine, novantrone, cyclophosphamide, or 5-fluorouracil). Response to chemotherapy had been evaluated during treatment and was reassessed according to WHO response criteria [21] by thorough examinations of the patients’ hospital records.
Samples. At surgery, residual breast tumor tissue from biochemical ER analyses was frozen and stored in sealed containers at −80°C until tissue extraction. The tissue extraction procedure has previously been described in detail [19]. For preparation of the detergent-extracted tissue, proteins were extracted using an acetate-detergent low pH extraction buffer [19]. For the cytosolic extracts, proteins were extracted using a buffer containing Tris–HCl (10 mmol/L), EDTA (1.5 mmol/L), Na2MoO4 (5.0 mmol/L), and monothioglycerol (1.0 mmol/L), pH of 7.4.
TIMP-1 measurements. The total level of TIMP-1 was measured using a previously described validated in-house ELISA [9, 22]. For measurements, samples were diluted 1:101 in sample dilution buffer. As internal control, duplicates of a control plasma pool were included on every plate. All TIMP-1 measurements were normalized by relating the measurements to the total concentration of protein (as measured by the protein BCA Protein Assay kit (Pierce) according to the manufacturer’s instructions) in individual samples.
Statistical analyses. Descriptive statistics for TIMP-1 are presented by the median as well as minimum and maximum and stratified by population and response. Comparisons of categorical data were tested using a chi-square test for independence. The association between response and TIMP-1 was found using the logistic regression model. TIMP-1 was scored as a continuous variable on the log scale [ln (TIMP-1 + 1)]. For the cytosolic samples, TIMP-1 was also analyzed as a dichotomous variable. The cut-off chosen, 33.4 ngTIMP-1/mg protein, was the optimized cut-off derived from our previous publication [14]. Response was scored as complete response (CR) or partial response (PR) (response) versus stable disease (SD) or progressive disease (PD) (non-response). Pooled analyses were performed using a random effects model thereby taking into account the difference among populations. The effect of TIMP-1 on response is presented as odds ratios (OR) with 95% confidence intervals (CI). The relationship between TIMP-1 and progression-free survival (PFS) as well as overall survival (OS) has been analyzed using the Cox proportional hazards model. The effect is presented as hazard ratios (HR). Model assessment was accomplished using conventional techniques. All calculations were done using SAS (v9.1, SAS institute, Cary, NC, USA). P < 5% were considered significant.
Results
Patient characteristics. Differences between the characteristics of the patients in the cytosol and detergent group were tested using a chi-square test for independence. Significant differences between the groups were found for nodal status (P = 0.007), tumor size (P = 0.019), adjuvant therapy (P = 0.0004), and metastasis site (P = 0.025), whereas no difference was found for age at surgery (P = 0.68), menopausal status (P = 0.44), steroid receptor status (P = 0.15), or first-line chemotherapy (P = 0.15). Detailed characteristics of all patients are found in Table 1.
TIMP-1 levels and associations between TIMP-1 and clinicopathological parameters. For the patient population with detergent extracts, the median TIMP-1 level was 21.6 ng TIMP-1/mg protein (range 6.32–190 ng TIMP-1/mg protein) and for the patient population with cytosolic extracts, it was 14.3 ng TIMP-1/mg protein (range 0–75.8 ng TIMP-1/mg protein). Detailed characteristics of the patients are shown in Table 1. Associations between TIMP-1 and other clinicopathological parameters are shown in Table 1 for both populations separately. As can be seen, no associations between the TIMP-1 levels and the clinicopathological parameters were found except for tumor size, where a correlation was found for patients with cytosolic extracts (P = 0.04).
Response to chemotherapy
TIMP-1—univariate analysis. Median time between primary surgery and distant recurrence was 29 months (0–139 months). After primary surgery, median survival time of all patients was 47 months (5–166 months) and 16 months after initiation of chemotherapy. Median time to progression was 8 months (1–129 months). At the time of analysis, 153 patients (95%) had died.
For patients with detergent extracts, the median TIMP-1 level in responders (n = 22) was 19.8 ng TIMP-1/mg protein (6.32–52.1 ng TIMP-1/mg protein) and for non-responders (n = 21), it was 24.6 ng TIMP-1/mg protein (9.13–190 ng TIMP-1/mg protein), P = 0.27. For patients with cytosolic extracts, the median TIMP-1 level in responders (n = 54) was 13.9 ng TIMP-1/mg protein (2.95–75.8 ng TIMP-1/mg protein) and for non-responders (n = 65), it was 15.4 ng TIMP-1/mg protein (0–64.4 ng TIMP-1/mg protein), P = 0.07.
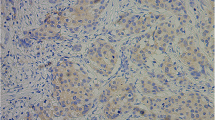
For analysis of the association between TIMP-1 and response, the two populations were pooled using a random effects model chosen in order to accommodate for the intrinsic heterogeneity between the studies. In the pooled present patient population, 14 (8.6%) patients had CR, 62 (38.3%) patients had PR, 46 (28.4%) patients had SD (27 patients had SD ≥6 months), and 40 (24. 7%) patients had PD. For analysis of association between the TIMP-1 levels, response was scored as CR or PR (response) versus SD or PD (no response). When analyzed as a continuous log-transformed variable, increasing tumor levels of TIMP-1, reaching borderline significance, were associated with a decreasing probability of response to CMF or anthracycline-containing chemotherapy (OR = 1.59, 95% CI: 0.97–2.62, P = 0.07, Fig. 1 top; Table 2). This means that when the TIMP-1 level increased 1 unit on the log scale, i.e., ~2.7 times, the risk of belonging to the group of non-responders increased 1.59 times. Although not significant, similar ORs were achieved when performing subgroup analyses for the detergent population (OR = 1.95, 95% CI: 0.59–6.44, P = 0.27) and the cytosol population (OR = 1.50 95% CI: 0.86–2.63, P = 0.15). We also grouped SD ≥6 months with CR and PR, i.e., “clinical benefit”, resulting in an OR of 1.43 (95% CI: 0.87–2.37, P = 0.16).
Forest plot illustrating the logistic regression analysis with TIMP-1 scored as a continuous variable on the log scale. OR with 95% CI as a measure of effect is presented representing the ratio of odds between two patients differing by 1 natural log (~2.7 times) in TIMP-1 levels. ORs are presented for the present study population (top), the Schrohl study population [14] (middle), and the Schrohl study population and present study population pooled together (bottom). Pooled analyses were performed using a random effects model
For comparison, we included the previous data from Schrohl et al. [14] (OR = 2.0, 95% CI: 1.1–3.3, P = 0.01, Fig. 1 middle). It can be seen that the odds ratio from the present study, although not reaching statistical significance at the 5% level, and the odds ratio from the Schrohl study are quite similar. We also performed a pooled analysis of the Schrohl patient population and the present patient population (n = 335) using the random effects model and found that the OR for response was 1.61 (95% CI: 1.14–2.29, P = 0.007, Fig. 1 bottom).
In the Schrohl study, an optimized cut-point for the cytosol samples of 33.4 ng TIMP-1/mg protein was identified, above which none of the patients responded to chemotherapy [14]. When applying this cut-point on the cytosol population in the current study, a significant difference in response rates was found between the patients with high TIMP-1 levels (n = 18), and low levels (n = 101), with corresponding response rates of 22% and 50%, respectively (P = 0.032, chi-square test, OR = 3.43, 95% CI: 1.06–11.1).
Other clinicopathological factors—univariate analysis. In univariate logistic regression analysis, dominant metastatic site (visceral or soft tissue vs. bone) as well as disease-free interval (>12 vs. ≤12 months) were associated with a better response to treatment. Lymph node status, age, tumor size, and steroid receptor status showed no significant association with response to chemotherapy (Table 2).
Multivariate analysis. In a multivariate analysis, only steroid receptor status and disease-free interval had a significant association with a better response to chemotherapy. For TIMP-1, an OR similar to the OR in the univariate analysis was found (Table 2).
Association between TIMP-1 and survival. We performed survival analyses with PFS and OS as endpoints. No statistically significant associations were found between increasing levels of TIMP-1 (continuous and log-transformed) and PFS (HR = 1.23, 95% CI: 0.94–1.61, P = 0.13) or OS (HR = 1.17, 95% CI: 0.92–1.48, P = 0.19).
Discussion
Predictive markers for the treatment of breast cancer are sparse. Especially, markers to predict whether the patients will respond to chemotherapy in general or to specific types of chemotherapy are required, since a significant number of the patients do not benefit from the treatment although they may suffer from treatment-induced adverse events. Thus, research concerning the identification of predictive markers is highly warranted. Recently, primary tumor tissue levels of TIMP-1 have been demonstrated to carry predictive information of the response to chemotherapy in patients with metastatic breast cancer, as patients with high levels of TIMP-1 benefit less from first-line chemotherapy compared with patients with low levels [14]. Interestingly, this association has also been demonstrated in metastatic colorectal cancer [23]. Furthermore, Lipton et al. [13] showed that high serum TIMP-1 levels were predictive of low objective response rate of endocrine therapy in metastatic breast cancer. Recently, we have also shown that TIMP-1 immunoreactivity in breast cancer is associated with benefit from adjuvant anthracycline treatment but not from adjuvant treatment with CMF [15]. The purpose of the present study was to further investigate the preliminary findings from metastatic breast cancer patients in an independent patient population.
An independent patient population was obtained by pooling metastatic breast cancer patients for whom detergent-extracted or cytosol-extracted samples from their primary tumors had been stored. The difference in the patient populations was circumvented in the statistical analysis by using a random effects model thereby taking into account the difference in sampling and extraction procedures. Next, we measured the primary tumor levels of TIMP-1 in the collected samples from the present patient population and related the TIMP-1 levels to the objective response to first-line anthracyclines or CMF treatment. When analyzing the present data in the same way as we have analyzed the original Schrohl data [14], i.e., responders versus non-responders in relation to the primary tumor TIMP-1 levels, we found that high TIMP-1 levels were associated with a poor response to treatment although not statistically significant. The odds ratio from the present study was very similar to the odds ratio from the Schrohl study [14]. Using the random effects model to perform a pooled analysis of the patients from the present patient population and the Schrohl patient population, we found an odds ratio for response of 1.61 (range 1.14–2.29, P = 0.007). Thus, even though the results in the present study did not reach statistical significance they support the results from the original Schrohl study. In the initial study on cytosolic extracts, an optimized cut-point of 33.4 ng TIMP-1/mg protein was identified, above which none of the patients responded to chemotherapy [14]. When applying this cut-point on the cytosolic extracts in the present study, a significant difference in response to chemotherapy was found between the patients with low TIMP-1 levels compared to those with high TIMP-1 levels. In the survival analyses, there was no statistically significant association between increasing levels of TIMP-1 and PFS and OS. The explanation for the lack of statistical significance could be an insufficient number of patients. It can also be noted that even though more patients had received first-line CMF in the Schrohl study (54 vs. 6% in the present study) [14], where a lower predictive value of TIMP-1 could be expected [15], a larger proportion of patients had received adjuvant therapy in the present study (35% adjuvant chemotherapy and 37% adjuvant endocrine treatment) compared to the Schrohl study [14] (21 and 14%, respectively). This could have obscured the “true” response to first-line chemotherapy thereby masking a possibly stronger predictive value of TIMP-1 in the present study.
If TIMP-1 could be used as a predictive marker in the metastatic setting, it would be of great importance since it could be used to ensure a tailored treatment for the individual patient. The biological explanation for the clinical findings mentioned earlier has been addressed in a number of studies. In this regard, TIMP-1 has been shown to inhibit apoptosis [16, 17], and since chemotherapy works by inducing apoptosis in the cancer cells, we have raised the hypothesis that TIMP-1 protects cells expressing high levels of TIMP-1 against chemotherapy by inhibiting apoptosis. In support of this hypothesis, our laboratory has recently shown that murine fibrosarcoma cells deficient of the TIMP-1 gene were significantly more sensitive to chemotherapy-induced apoptosis compared to their wild-type controls [16]. These results have recently been extended to a human breast carcinoma cell system [24]. In this study, it was shown that human breast carcinoma cells expressing high levels of TIMP-1 were significantly less sensitive to chemotherapy. Interestingly, the study suggested that TIMP-1 may selectively protect cancer cells against topo IIα inhibitors. It is interesting to note that of the patients included in the present study, ~90% had received anthracycline-containing chemotherapy, i.e., combinations containing epirubicin. Epirubicin is a topo IIα inhibitor, and thus our study supports the hypothesis that TIMP-1 may predict the response to this group of drugs. This hypothesis is now supported by our findings in patients receiving adjuvant chemotherapy [15]. In this context, it would be of interest to investigate whether TIMP-1 also associates with the effect of other groups of drugs, e.g., taxanes, or if the predictive value only applies to topo IIα inhibitors. Such studies would be of great interest since TIMP-1 as such could be used to discriminate between drugs being more effective than others in individual patients.
As a final remark, it should be mentioned, as emphasized in the introduction, that a number of previous studies have demonstrated that tumor tissue levels of TIMP-1 as well as TIMP-1 measured in blood carry prognostic information in primary breast cancer [7–11]. It is important to be aware of the various limitations in prognostic studies where endpoints such as recurrence-free survival and overall survival are used. These endpoints can be influenced by previously administered adjuvant and palliative treatments. In this regard, based on our previous study [14] and the present study on the association between TIMP-1 and response to chemotherapy, it seems that the prognostic value of TIMP-1 found in several previous studies could in part be the result of the TIMP-1 related effect on response to therapy. In order to investigate this issue further the prognostic value of TIMP-1 in patients who have not received adjuvant systemic therapy should be evaluated.
In conclusion, the data available on TIMP-1 and response to chemotherapy suggest that TIMP-1 carries predictive information in metastatic breast cancer that may enable a more tailored chemotherapy for the individual patient. Future studies should be aimed at converting the current ELISA technology with the need for frozen tumor tissue to methods that can be applied on paraffin sections [15] or serum or plasma [13, 22]. The latter would allow for direct measurement of TIMP-1 levels at the time of treatment for metastatic disease.
References
Goldhirsch A, Ingle JN, Gelber RD et al (2009) Thresholds for therapies: highlights of the St Gallen international expert consensus on the primary therapy of early breast cancer. Ann Oncol 16:1569–1583
Thomssen C, Janicke F (2000) Do we need better prognostic factors in node-negative breast cancer? Eur J Cancer 36:293–298
Goldhirsch A, Coates AS, Gelber RD et al (2006) First–select the target: better choice of adjuvant treatments for breast cancer patients. Ann Oncol 17:1772–1776
Knoop AS, Knudsen H, Balslev E et al (2005) Retrospective analysis of topoisomerase IIα amplifications and deletions as predictive markers in primary breast cancer patients randomly assigned to cyclophosphamide, methotrexate, and fluorouracil or cyclophosphamide, epirubicin, and fluorouracil: Danish Breast Cancer Cooperative Group. J Clin Oncol 23:7483–7490
Nielsen KV, Ejlertsen B, Jørgensen JT, Knoop A et al (2008) The value of TOP2A gene copy number variation as a biomarker in breast cancer: Update of DBCG trial 89D. Acta Oncol 47:725–734
Arriola E, Rodriguez-Pinilla SM, Lambros MBK et al (2007) Topoisomerase II alpha amplification may predict benefit from adjuvant anthracyclines in HER2 positive early breast cancer. Breast Cancer Res Treat 106:181–189
Ree AH, Florenes VA, Berg JP et al (1997) High levels of messenger RNAs for tissue inhibitors of metalloproteinases (TIMP-1 and TIMP-2) in primary breast carcinomas are associated with development of distant metastases. Clin Cancer Res 3:1623–1628
McCarthy K, Maguire T, McGreal G et al (1999) High levels of tissue inhibitor of metalloproteinase-1 predict poor outcome in patients with breast cancer. Int J Cancer 84:44–48
Schrohl AS, Christensen IJ, Pedersen AN et al (2003) Tumor tissue concentrations of the proteinase inhibitors tissue inhibitor of metalloproteinases-1 (TIMP-1) and plasminogen activator inhibitor type 1 (PAI-1) are complementary in determining prognosis in primary breast cancer. Mol Cell Proteomics 2:164–172
Schrohl AS, Holten-Andersen MN, Peters HA et al (2004) Tumor tissue levels of tissue inhibitor of metalloproteinase-1 as a prognostic marker in primary breast cancer. Clin Cancer Res 10:2289–2298
Würtz SØ, Møller S, Mouridsen H et al (2008) Plasma and serum levels of tissue inhibitor of metalloprrteinases-1 are associated with prognosis in node-negative breast cancer—a prospective study. Mol Cell Proteomics 7:424–430
Lipton A, Suhail MA, Leitzel K et al (2007) Elevated plasma tissue inhibitor of metalloproteinase-1 level predicts decreased response and survival in metastatic breast cancer. Cancer 109:1933–1939
Lipton A, Leitzel K, Chaudri-Ross HA et al (2008) Serum TIMP-1 and response to the aromatase inhibitor letrozole versus tamoxifen in metastatic breast cancer. J Clin Oncol 26(16):2653–2658
Schrohl AS, Meijer-van Gelder ME, Holten-Andersen MN et al (2006) Primary tumor levels of tissue inhibitor of metalloproteinases-1 are predictive of resistance to chemotherapy in patients with metastatic breast cancer. Clin Cancer Res 12:7054–7058
Willemoe GL, Hertel PB, Bartels A et al (2009) Lack of TIMP-1 tumor cell immunoreactivity predicts effect of adjuvant anthracycline based chemotherapy in patients (n = 647) with primary breast cancer. A Danish Breast Cancer Cooperative Group Study. Eur J Cancer. doi:10.1016/j.ejca.2009.05.029
Davidsen ML, Würtz SO, Romer MU et al (2006) TIMP-1 gene deficiency increases tumour cell sensitivity to chemotherapy-induced apoptosis. Br J Cancer 95:1114–1120
Li G, Fridman R, Kim HR (1999) Tissue inhibitor of metalloproteinase-1 inhibits apoptosis of human breast epithelial cells. Cancer Res 59:6267–6275
McShane LM, Altman DG, Sauerbrei W et al (2005) Reporting recommendations for tumor marker prognostic studies (REMARK). J Clin Oncol 23:9067–9072
Pedersen AN, Christensen IJ, Stephens RW (2000) The complex between urokinase and its inhibitor in primary breast cancer, relation to survival. Cancer Res 60:6927–6934
Ejlertsen B, Mouridsen HT, Langkjer ST et al (2004) Phase III study of intravenous vinorelbine in combination with epirubicin versus epirubicin alone in patients with advanced breast cancer: a Scandinavian Breast Group Trial (SBG9403). J Clin Oncol 22:2313–2320
World Health Organization (1979) WHO handbook for reporting results for cancer treatment. World Health Organization Offset Publications No. 48, Geneva
Holten-Andersen MN, Murphy G, Nielsen HJ et al (1999) Quantitation of TIMP-1 in plasma of healthy blood donors and patients with advanced cancer. Br J Cancer 80:495–503
Sørensen NM, Byström P, Christensen IJ et al (2007) TIMP-1 is significantly associated with objective response and survival in metastatic colorectal cancer patients receiving combination of irinotecan, 5-fluorouracil, and folinic acid. Clin Cancer Res 13:4117–4122
Würtz SO, Schrohl A, Brünner N, Lademann U (2009) Tissue inhibitor of metalloproteinases-1 protects the human breast carcinoma cell line MCF-7 S1 against anthracycline-induced cell death by activation of the akt survival pathway [abstract]. Cancer Res 69(Suppl):161s
Acknowledgments
The present study was supported financially by The Swedish Cancer Society, The Swedish Research Council, The Gunnar, Arvid, and Elisabeth Nilsson Foundation, The Mrs Berta Kamprad Foundation, The University Hospital of Lund Research Foundation, Governmental Funding of Clinical Research within the National Health Service, The Danish Cancer Society, Danish Center for Translational Breast Cancer Research, A Race Against Breast Cancer, The Ministry for Health and Prevention, and The Danish Strategic Research Council for Food and Health and the Sino-Danish Breast Cancer Research Centre.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors Marie Klintman and Sidse Ørnbjerg Würtz contributed equally to this work.
Per Malmström and Nils Brünner shared senior authorship.
Rights and permissions
About this article
Cite this article
Klintman, M., Ørnbjerg Würtz, S., Christensen, I.J. et al. Association between tumor tissue TIMP-1 levels and objective response to first-line chemotherapy in metastatic breast cancer. Breast Cancer Res Treat 121, 365–371 (2010). https://doi.org/10.1007/s10549-009-0483-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-009-0483-1