Abstract
Cisplatin and carboplatin have antitumor activity in breast cancer. Satraplatin, an orally bioavailable platinum analog, offers a potential alternative to intravenous chemotherapy. We conducted a multicenter phase II study of this agent as first- or second-line treatment of metastatic breast cancer. Satraplatin 80 mg/m2 was taken PO Days 1–5 q 21 days in cycles 1 and 2, and if tolerated, increased to 100 mg/m2 for subsequent cycles. Restaging studies to assess response were performed after every 2 cycles. Between November 2005 and March 2006, 40 patients were enrolled. Baseline characteristics: 48% prior adjuvant chemotherapy, 60% prior chemotherapy for MBC; median age, 62 years (ranges 43–83), 58% ER+/PR+, 23% ER+/PR−, 18% ER−/PR−/HER2−, and 5% HER2+. In 31 patients with measurable disease, there were two partial responses (PR; 6%; 95% CI 0, 15.2); and four patients (13%) had SD ≥6 months for a clinical benefit rate of 19%. Among the subanalysis of seven triple-negative patients with measurable disease, there were 2 SD and 2 PD. Median survival was 15 months and median progression-free survival was 2.7 months. The most common grade 3–4 toxicities were neutropenia (28%) and thrombocytopenia (25%). AEs leading to treatment discontinuation were nausea (n = 3), thrombocytopenia (n = 3), fever (n = 2), and vomiting (n = 2). This phase II study demonstrates oral satraplatin has limited activity as a single agent for MBC. Satraplatin, at a lower dose used in this study, could be combined with other chemotherapy agents in future trials in breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In minimally treated MBC, platinum-based chemotherapeutic agents (i.e., cisplatin and carboplatin) exhibit antitumor activity as single agents, with mean response rates of 50 and 32%, respectively. However, in patients previously treated with chemotherapy, the response rates drop significantly to <10% [1]. The use of platinum-based chemotherapeutic agents is of special interest in breast cancer patients whose tumors are ER− (negative), PR−, and HER2− (“triple-negative”) due to preclinical and early clinical evidence suggesting sensitivity to platinums [2, 3]. Garber et al. [4] have previously reported an ORR of 63% using single-agent cisplatin as a neo-adjuvant therapy in triple-negative patients.
Satraplatin (also known as JM-216) or bis (acetato) ammine dichloro (cyclohexylamine) platinum (IV) is the first platinum analog that is bioactive with oral administration. Satraplatin exhibits a slightly higher cytotoxic activity in vitro when compared to cisplatin, and also exhibits activity against some cisplatin-resistant human tumor lines [5, 6]. Like other platinum-based drugs, satraplatin exerts its biological activity by means of reactive biotransformation products that bind to DNA, causing the inhibition of DNA replication, cell cycle arrest, and induction of apoptosis. In addition, it has recently been reported that satraplatin inhibits Stat3 activity [7, 8]. In studies using both murine tumors and human ovarian carcinoma xenografts, oral administration of satraplatin resulted in meaningful antitumor activity, and was comparable to intravenous (IV) administration of cisplatin or carboplatin [7].
Results from early Phase I clinical trials with satraplatin have shown that the compound is extensively metabolized in vivo following oral administration. Urinary recovery of platinum is less than 10% in the first 24 h following satraplatin administration. This suggests a relatively minor role for the kidney in the elimination of parent satraplatin or its platinum-containing metabolites. Satraplatin offers a potentially more convenient alternative to platinum agents administered intravenously. In addition, satraplatin may lower treatment costs by eliminating time spent in the clinic receiving infusions. Phase II trials of single-agent satraplatin have demonstrated activity in patients with small-cell lung cancer (SCLC), relapsed ovarian cancer, and prostate cancer [9, 10]. Phase III trials in hormone refractory prostate cancer have shown the comparability of satraplatin in combination with prednisone to single-agent prednisone with regards to toxicity and progression-free survival (PFS) [11].
This multicenter Phase II study was undertaken to determine the efficacy and safety of satraplatin in minimally pretreated MBC patients. The primary objective in this study was to determine the objective response rate (ORR) of satraplatin in MBC patients. The secondary objectives were to determine duration of response, PFS, and 1-year survival and to evaluate the toxicities of satraplatin in MBC patients.
Materials and methods
Study design
This was a Phase II, open-label, nonrandomized study for MBC patients with measurable and nonmeasurable disease. The protocol was approved by a central institutional review board (IRB) with jurisdiction over the specific sites that registered patients on study. All patients signed the IRB-approved informed consent at study entry. Further details regarding the overall study design will be discussed in the statistical analysis section.
Patients
Female patients age ≥18 years with cytologically or pathologically confirmed breast cancer that had metastasized who had either measurable disease as per response evaluation criteria in solid tumors (RECIST) [12] or nonmeasurable disease (including lytic bone disease) if there was also an elevated serum CA27.29 (or CA15.3) were registered. HER2-positive BC patients were required to have been treated previously with trastuzumab. Patients were required to have an Eastern Cooperative Oncology Group (ECOG) performance status of 0–2 as well as white blood cell counts (WBC) ≥3,500 × 106/L; absolute neutrophil count (ANC) ≥1,500 × 106/L; platelet count ≥100,000 × 106/L; hemoglobin ≥9 g/dL; total bilirubin ≤1.5 mg/dL; alkaline phosphatase, AST, and ALT ≤3× upper limit of normal (ULN; unless liver metastases present, then ≤5× ULN allowed); and serum creatinine ≤1.5 mg/dL. In addition, patients could have received no more than one prior chemotherapy regimen for MBC, had no prior platinum-based therapy, were able to swallow capsules, have integrity of the upper gastrointestinal (GI) tract, and have no active GI disease or history of malabsorptive disorder that could affect the bioavailability of oral medications. Patients with brain metastases that were not progressive, and that did not require steroid therapy (off steroids for at least 2 months), were eligible.
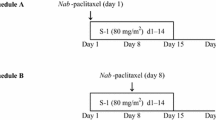
Treatment
Starting on Day 1, patients received a starting dose of 80 mg/m2 oral satraplatin per day for five consecutive days of every 21 day cycle. Patients were observed by clinical personnel for at least 1 h following the first-dose. Patients took satraplatin on an empty stomach (no food for 1 h before or 2 h after dosing) with 4–8 oz. of water.
A dose escalation to 100 mg/m2/day for five consecutive days was allowed starting with Cycle 3 if patients had completed at least 2 (21-day) cycles of satraplatin with no incidence of ≥grade 2 hematologic toxicities; ≥grade 2 GI toxicities (while receiving antidiarrheal treatment); grade 4 febrile neutropenia; dosing interruption or delay due to toxicities. In addition, patients must have had no evidence of disease progression. All patients were allowed only one dose escalation. After dose escalation, a complete blood count (CBC) with differential and platelet count was performed weekly for that cycle. Any dose reductions that occurred were permanent.
Patients received 1 mg of prophylactic granisetron administered orally twice a day as follows: 1 h prior to study drug dose and approximately 12 h after study drug dose each of the 5 days of study drug administration. If required, antidiarrheal medication (e.g, loperamide) was prescribed at the discretion of the treating physician and administered as per the clinic’s standard practice.
Assessments
Prestudy (baseline) assessments included the following: medical history; complete physical examination; pregnancy test (if applicable); assessment of PS on the ECOG scale; physical and radiological examination of the tumor; and CBC and complete metabolic profile; CA27.29 (CA15.3) was assessed in patients with nonmeasurable disease; hormone (ER/PR) and HER2 receptor status were performed locally. During treatment, these assessments were performed in the same manner at the start (Day 1) of each cycle, except: CBC was performed on Days 1 and 14 of each cycle; dose escalations required additional assessment Day 7; radiologic examination of the tumor (after Cycle 2 and 4, and every 3 cycles thereafter); toxicity and treatment compliance assessment within each cycle. When patients came off treatment, all previous assessments were repeated.
Response criteria and toxicity
Response was assessed using RECIST criteria [12]. Patients with nonmeasurable disease were not assessed for ORR, but rather for time-to-disease progression (TTP) and 1-year survival. Toxicities and adverse events were graded using the National Cancer Institute’s Common Terminology Criteria for Adverse Events (NCI CTCAE) Version 3.0 [13].
Statistical analysis
The primary objective of this study was to determine the ORR of oral satraplatin in MBC based on the patients with measurable disease. Secondary objectives for this study included evaluating toxicities, duration of response, PFS, and 1-year survival. The safety of satraplatin was also assessed.
The two-stage MiniMax method of Simon [14] was used to estimate the sample size. The results specified a sample size of 47 patients with measurable disease (including 10% for early dropouts) distributed in two stages. The hypothesis (H1) assumed a response rate of 21%, while the null hypothesis (H0) predicted the ORR to be not greater than 8%, with a significance level of 0.05 and statistical power at 80%. In the first-stage, a minimum of 28 patients with measurable tumors needed to be treated with at least three responses to continue to the second stage. In parallel, 33 patients with nonmeasurable disease were to be registered for the possibility of assessing the clinical utility of serum CA27.29 (or CA15.3) and circulating tumor cells as predictors of time to disease progression. Patients were stratified by measurable versus nonmeasurable disease and each group was further stratified by ER−, PR−, and HER2− (triple-negative) versus nontriple-negative patients. The intent-to-treat (ITT) population was defined as all eligible patients enrolled in the study that had no major violations of protocol inclusion and/or exclusion criteria. The evaluable population was defined as those with a confirmed response of CR, PR, SD, PD, or NE.
Responses were tabulated in a frequency table of all evaluable patients with measurable disease. The response rate was calculated as the number of responders (best study response recorded as CR or PR) divided by the number of patients qualified for measurable tumor response analysis. Among tumor responders, the duration of tumor response was measured from the first date that measurement criteria were met for CR/PR (whichever status was recorded first), until the first date that progressive disease was objectively documented, or until the last date of contact for patients who did not progress. PFS was calculated as the time start of treatment to either the date the patient was first recorded as having disease progression (even if the patient went off treatment because of toxicity), or the date of death if the patient died due to any causes before progression.
One-year survival was defined as the proportion of patients alive at 1-year following the first-dose of study drug. The toxicity profile of satraplatin was evaluated on the safety population, which was defined as all patients who received at least one dose of study drug.
Results
Patient characteristics
Between November 2005 and March 2006, 40 women were enrolled on study and comprised both the ITT and safety population. Thirty-eight patients were evaluable for response (31 patients with measurable tumors and 7 with nonmeasurable tumors); two patients were ineligible (both failed the inclusion criteria of having more than 1 prior chemotherapy); however, both had received 1 cycle of study drug, therefore are included in the safety analysis. Patient characteristics are summarized in Table 1. This patient population was notable for its older age (median age 62 years), predominant hormone receptor positive status (80%), and minimal prior chemotherapy (35% of patients had no prior chemotherapy for adjuvant or metastatic disease; and 48% of patients had prior adjuvant therapy).
Of the 40 patients enrolled in the study, 27 (68%) came off treatment for disease progression, 8 (20%) for adverse events, 2 (5%) withdrew consent, 2 (5%) were ineligible, and 1 (2.5%) by Investigator request. The top metastatic sites in the ITT population were bone (68%), lung (45%) liver (40%), and lymph nodes (30%). Brain metastases were present in 5% of patients.
Treatment outcomes
Responses for the evaluable population are summarized in Table 2. The ORR in patients with measurable disease was 6% (CR 0%, PR 6%; 95% CI, 0, 15.2). About 18 patients had as their best response SD (58%): nine patients (26%) had SD ≥ 3 months and four patients (13%) had SD ≥ 6 months. One patient with nonmeasurable disease achieved SD. The clinical benefit rate (CR+PR+SD ≥ 6 months) was 19%. The two responders and 33% of patients with SD had not received prior chemotherapy. Metastatic sites in patients that achieved PR and SD ≥ 6 months were at the bone, liver, lung, and lymph node. Neither of the two patients with brain metastasis achieved an objective response. All seven patients who achieved PD progressed after at least 2 cycles of treatment.
The durations of response in the two responders were 4 and 9.5 months. Median PFS in the ITT population was 2.7 months (95% CI, 1.8–5.4 (Fig. 1)). The median survival for all patients was 15 months [95% CI, 12.2–18.3 (Fig. 2)] similar to patients with nonmeasurable tumors. Median follow-up for all patients was 15 months (range, 0.4–22.5). The 1-year survival was 67% for all patients and 83% for patients with nonmeasurable tumors. The receptor statuses of the responders were ER+/PR+/HER2− and ER+/PR−/HER2−, and the status of the four patients with SD ≥6 months was ER+/PR+/HER2−.
In the subanalysis of seven patients with triple-negative hormone receptors, all had measurable disease; there were 2 SD, 2 PD, and 3 NE, no CR or PR was observed. The length of SD for each of the 2 SD patients was 2.7 months. Median PFS in this population was 2.7 months (95% CI, 1.1—Not Reached [NR]). Survival at 1-year for triple-negative patients was 40%, with a median overall survival of triple-negative patients of 10 months (95% CI, 6.8—NR).
Drug delivery
The median number of cycles of satraplatin that were given to the safety population (N = 40) was 2 (range, 1–19). Five patients had doses escalated to 100 mg/m2 at day 1 of cycle 3. Dose reductions occurred in 17 (43%) of patients; 11 of these patients required both a dose reduction and delay (28%). Three patients had delayed doses (8%). Reasons for dose modifications included weight loss, thrombocytopenia, neutropenia, and diarrhea. The median dose intensity for satraplatin, defined as actual dose/planned dose, was 99.7% (range, 92–100%), while the mean was 99%; 57% of patient receive all doses as planned.
Toxicity
Treatment-related toxicities are summarized in Table 3. The two most common grade 3–4 toxicities were neutropenia (28%) and thrombocytopenia (25%). Other grade 3–4 toxicities that occurred in ≤3 patients were anemia, fatigue, and leukopenia. Eight patients (20%) discontinued study treatment attributed to adverse events, summarized in Table 4.
Discussion
Anthracyclines and taxanes are classic chemotherapy agents in MBC; however, since the 1980s, platinum agents such as cisplatin and carboplatin have gained popularity. Cisplatin was originally tested in preclinical studies in mice where tumor regression was observed [15]; in clinical studies, cisplatin produced a remarkable ORR of 54% when used as a single-agent in patients with previously untreated MBC [16]. Another study verified these results, reporting an ORR of 47% [17]. These results indicated that cisplatin had significant impact for use as a first-line treatment in MBC.
Carboplatin, developed to be a less toxic analogue of cisplatin but still preserve its antitumor activity [18], also has shown moderate activity in MBC patients without prior therapy. In two studies where carboplatin was given at 400 mg/m2 IV once every 4 weeks as a single-agent, first-line treatment in MBC, Kolarić and colleagues [19] reported an ORR of 20% (2 complete responses and 2 partial responses in 20 total patients), whereas, Martin and colleagues reported an ORR of 35% (1 complete response and 11 partial responses in 34 total patients) [20]. In both reports, toxicity was reported as ranging from mild to moderate with myelotoxicities being the primary events. These studies suggested that like cisplatin, carboplatin was an active drug in previously untreated MBC.
Satraplatin, originally developed to be an orally active platinum agent with tolerability similar to carboplatin, displayed meaningful antitumor activity in mice with ovarian cancer xenografts in preclinical studies [5, 15]. Furthermore, satraplatin also had activity in human ovarian cancer cells that were considered to be cisplatin-resistant [6]. In several Phase II and III studies, satraplatin showed promise in a variety of cancers. Two prior studies suggested satraplatin’s potential in breast cancer. In a Japanese Phase I study of satraplatin in patients with solid tumors, antitumor activity was observed in two patients with MBC, who had previously been treated with doxorubicin [21], warranting a Phase II investigation of satraplatin in MBC.
This is the first reported clinical trial of oral satraplatin in MBC patients. With an ORR of 6%, clinical benefit rate (CR+PR+SD ≥ 6 months) of 19%, and a median survival of 15 months, single-agent satraplatin had limited activity as the first- or the second-line chemotherapy in this population. In the evaluable population, 26% of patients achieved SD ≥3 months, while 13% of patients achieved SD ≥6 months. Because, only two objective responses were noted in the first-cohort of patients enrolled, accrual was stopped and did not proceed to stage 2.
The results seen in the current study are in accordance with previous reports where single-agent cisplatin or carboplatin showed minimal antitumor activity in chemotherapy pretreated patients [15, 22]. Using cisplatin as a single-agent in pretreated MBC, no ORR have been reported greater than 11% [23]. Similarly, carboplatin also has minimal activity in patients who had prior chemotherapy, with ORR ranging from 0 to 8% [23–25] Interestingly, the two objective responses produced by satraplatin in the present study were both in patients who had no prior chemotherapy.
While satraplatin was fairly well tolerated and toxicities were manageable in the current study, 20% of patients went off treatment because of toxicity, and dose reductions were required in 38% of patients. Therefore, slightly lower doses of satraplatin would be necessary to combine it with other chemotherapy agents in future trials in breast cancer. In the triple-negative patients, median PFS and OS were unremarkable with satraplatin treatment; however, the population was too small to make any conclusive statement.
References
Decatris MP, Sundar S, O’Byrne KJ (2004) Platinum-based chemotherapy in metastatic breast cancer: current status. Cancer Treat Rev 30:53–81. doi:10.1016/S0305-7372(03)00139-7
Bhattacharyya A, Ear US, Koller BH et al (2000) The breast cancer susceptibility gene BRCA1 is required for subnuclear assembly of Rad51 and survival following treatment with the DNA cross-linking agent cisplatin. J Biol Chem 275:23899–23903. doi:10.1074/jbc.C000276200
Quinn JE, Kennedy RD, Mullan PB, Gilmore PM et al (2003) BRCA1 functions as a differential modulator of chemotherapy-induced apoptosis. Cancer Res 63:6221–6228
Garber JE, Richardson A, Harris LN, et al. (2006) Neo-adjuvent cisplatin (CDDP) in “triple-negative” breast cancer (BC). San Antonio Breast Cancer Symposium, abstr 3074
Kelland LR, Abel G, McKeage MJ et al (1993) Preclinical antitumor evaluation of bis-acetato-ammine-dichloro-cyclohexylamine platinum (IV): an orally active platinum drug. Cancer Res 53:2581–2586
Sharp SY, Rogers PM, Kelland LR (1995) Transport of cisplatin and bis-acetato-ammine-dichlorocyclohexylamine platinum(IV) (JM216) in human ovarian carcinoma cell lines: identification of a plasma membrane protein associated with cisplatin resistance. Clin Cancer Res 1(9):981–989
Rose WC, Crosswell AR, Schurig JE et al (1994) Preclinical antitumor activity of orally administered platinum (IV) complexes. Cancer Chemother Pharmacol 32:197–203. doi:10.1007/BF00685835
Gariboldi MB, Ravizza R, Molteni R et al (2007) Inhibition of Stat3 increases doxorubicin sensitivity in a human metastatic breast cancer cell line. Cancer Lett 258(2):181–188. doi:10.1016/j.canlet.2007.08.019
GPC Biotech Inc. April 2004. Satraplatin (JM-216) Bis (acetato) ammine dichloro (cyclohexylamine) platinum (IV). Clinical Investigator’s Brochure Version 1
Choy H (2006) Satraplatin: an orally available platinum analog for the treatment of cancer. Expert Rev Anticancer Ther 6(7):973–982. doi:10.1586/14737140.6.7.973
Sternberg CN, Whelan P, Hetherington J et al (2005) Phase III trial of satraplatin, an oral platinum plus prednisone vs. prednisone alone in patients with hormone-refractory prostate cancer. Oncology 68(1):2–9. doi:10.1159/000084201
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European organization for research and treatment of cancer, national cancer institute of the United States, national cancer institute of Canada. J Natl Cancer Inst 92:205–216. doi:10.1093/jnci/92.3.205
Cancer Therapy Evaluation Program Common Terminology Criteria for Adverse Events v3.0 (CTCAE). URL: http://ctep.cancer.gov/reporting/ctc_v30.html. Accessed 30 Sep 2008
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10:1–10. doi:10.1016/0197-2456(89)90015-9
Kelland L (2007) The resurgence of platinum-based cancer chemotherapy. Nat Rev Cancer 7(8):573–584. doi:10.1038/nrc2167
Kolarić K, Roth A (1983) Phase II clinical trial of cis-dichlorodiammine platinum (cis-DDP) for antitumorigenic activity in previously untreated patients with metastatic breast cancer. Cancer Chemother Pharmacol 11(2):108–112. doi:10.1007/BF00254257
Sledge GW Jr, Loehrer PJ Sr, Roth BJ, Einhorn LH (1988) Cisplatin as first-line therapy for metastatic breast cancer. J Clin Oncol 6(12):1811–1814
Harrap KR (1985) Preclinical studies identifying carboplatin as a viable cisplatin alternative. Cancer Treat Rev 12(Suppl A):21–33
Kolarić K, Vukas D (1991) Carboplatin activity in untreated metastatic breast cancer patients–results of a phase II study. Cancer Chemother Pharmacol 27(5):409–412. doi:10.1007/BF00688868
Martín M, Díaz-Rubio E, Casado A et al (1992) Carboplatin: an active drug in metastatic breast cancer. J Clin Oncol 10(3):433–437
Kurata T, Tamura T, Sasaki Y et al (2000) Pharmacokinetic and pharmacodynamic analysis of bis-acetato-ammine-dichloro-cyclohexylamine-platinum(IV) (JM216) administered once a day for five consecutive days: a phase I study. Jpn J Clin Oncol 30(9):377–384. doi:10.1093/jjco/hyd102
Martín M (2001) Platinum compounds in the treatment of advanced breast cancer. Clin Breast Cancer 2(3):190–208. doi:10.3816/CBC.2001.n.022
Ott I, Gust R (2007) Preclinical and clinical studies on the use of platinum complexes for breast cancer treatment. Anticancer Agents Med Chem 7(1):95–110. doi:10.2174/187152007779314071
Martín M, Díaz-Rubio E, Casado A et al (1991) Phase II study of carboplatin in advanced breast cancer: preliminary results. Semin Oncol 18(suppl 2):23–27
O’Brien ME, Talbot DC, Smith IE (1993) Carboplatin in the treatment of advanced breast cancer: a phase II study using a pharmacokinetically guided dose schedule. J Clin Oncol 11(11):2112–2117
Acknowledgments
We thank the patients who participated in this clinical trial, US Oncology physicians, the site coordinators, project manager Karla Burgos, BS; data reviewer Delia Estrada, BS; and, Jean Kochis, MBA, Kristi A. Boehm, MS, and Maren K. Levin, MS, for their writing contributions. The research support was provided by GPC Biotech Inc., Princeton, NJ, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smith, J.W., McIntyre, K.J., Acevedo, P.V. et al. Results of a phase II open-label, nonrandomized trial of oral satraplatin in patients with metastatic breast cancer. Breast Cancer Res Treat 118, 361–367 (2009). https://doi.org/10.1007/s10549-009-0410-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-009-0410-5