Abstract
Breast cancer is the most commonly diagnosed type of cancer in reproductive aged women. Adjuvant systemic therapy is recommended in most women and has been demonstrated to reduce the risk of recurrence and increase survival. However, there may be a negative impact of adjuvant systemic therapy on fertility as well as on subsequent quality of life. There are a number of fertility preservation options currently available and relevant information regarding these options should be provided prior to commencing adjuvant treatment. The aim of the review is to identify the fertility-related needs, concerns and preferences of young women with early breast cancer. The databases MEDLINE and EMBASE were searched from 1988 onwards using keywords, and examining reference lists. Of the 499 articles identified, 20 met eligibility criteria and were reviewed. Multiple fertility-related information needs specific to this group regarding menstrual changes and potential infertility attitudes to, and actual decisions made regarding, pregnancy breastfeeding and contraception emerged. Information on fertility-related decisions was rated as important, and the preferred methods for obtaining this information was consultation with a specialist or a decision aid early in the treatment plan. There is limited research about fertility-related needs, and even less on contraceptive preferences and the attitudes of health care providers towards fertility-related issues. No studies describing the development of tools to assist with decisions about fertility-related choices were identified. Young women with early breast cancer have specific fertility- and menopause-related needs and concerns, which are commonly not adequately addressed or discussed prior to commencing adjuvant therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Approximately 10–15% of breast cancers are diagnosed in reproductive aged women. Young age at diagnosis has been reported to be an adverse prognostic factor and the majority of young women will be offered adjuvant chemo- and/or hormonal therapy, which significantly reduce the risk of recurrence and mortality. However, adjuvant therapies may negatively impact on ovarian function and fertility. Given that the age at first delivery has been steadily rising [1], and that increasing numbers of women have not yet started or completed their families when diagnosed, this raises additional concerns regarding subsequent fertility. These issues need to be discussed and addressed prior to commencing adjuvant chemotherapy.
Young age at breast cancer diagnosis is variably defined. Some studies report it as ≤50 years [2–6], ≤45 years [7], ≤40 years [8–11], allow self-definition of ‘young’ [12], or use menopausal status as an indicator [13]. In general the concept of ‘young’ is related to being premenopausal. The consequences of cancer treatment for pre- and postmenopausal women differ; younger breast cancer patients are at greater risk for emotional distress, fatigue, sexual dysfunction, and stress, which may persist for a number of years post-treatment [6]. Younger women appear to have a more negative and intense experience [14–16] and have more concerns about the side-effects of cancer treatment [17]. Given that the adjuvant chemotherapy regimens used for the treatment of breast cancer may adversely affect fertility, and may induce premature menopause [18–22] as well as sexual dysfunction, these therapies may lead to both emotional and physical symptoms [6, 13, 23–25]. Younger women tend to have relatively little knowledge about menopause or its symptoms and often find this to be particularly confronting [6]. Women with hormone receptor positive tumours are usually advised to delay pregnancy until they have completed up to 5 years of adjuvant hormonal treatment and during this time there will be a natural age-related decline in fertility. This delay may be particularly important for subsequent fertility in women who are over 30 years old when treatment commences. Thus it is unsurprising that this may significantly impact patients’ subsequent quality of life [24, 26, 27]; younger women wanting children at the time of a breast cancer diagnosis continue to be distressed for some time afterwards [2, 4, 10, 11].
Patients who receive more information tend to report greater satisfaction with their medical care [28] and experience less anxiety and depression [29] and younger women often prefer to play an active role in treatment decision-making [30]. There is evidence to suggest that adjustment in younger women is improved if they are involved in treatment choices [31]. Involving patients in treatment decisions and educating them on both the potential benefits and side-effects of different treatment options may improve long-term quality of life [32]. In order to meet these information needs, we require more data on the specific concerns and preferences of younger women with early breast cancer regarding fertility-related information.
Aim/purpose
The purpose of this review is to highlight the specific fertility-related psychosocial needs, concerns and preferences of younger women with breast cancer. This information contributes to patient decision-making about treatment options. A better understanding of these issues will assist the development of strategies to improve quality of care, quality of life and longer term psychosocial survival outcomes.
Method
Description of literature search strategy
A systematic review of studies was conducted on English language articles published between January 1988 and September 2008. MEDLINE, Medline in-Process or non-Indexed, and EMBASE databases were searched using the following keywords individually and in combination: “needs/concerns/preferences/education/decision/decision-making/quality of life/psychosocial” + “breast cancer/breast neoplasms” + “young/younger/pre-menopause/pre-menopausal” + “women/woman/female” + “fertility/infertility/reproduction/reproductive health/menopause/menopausal/chemotherapy/ovarian failure”. The reference lists accompanying all publications were examined. Studies were included if they described empirical research relating to the fertility-related needs, concerns or preferences of younger women with breast cancer. Articles that reported on women of all ages were included if they reported data on younger women separately. Qualitative studies were included in this review due to a limited number of quantitative studies measuring needs and concerns of younger women with breast cancer. Articles that did not explicitly relate to fertility were excluded. Publications were excluded from the review if they were review articles, lectures, single case reports, conference abstracts or commentaries. Studies pertaining only to advanced breast cancer were also excluded, because the issues and options for this group differ considerably from patients treated with curative intent.
Results
Excluded studies
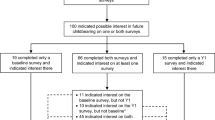
Figure 1 shows the number of included and excluded articles at different stages of the literature search. Amongst other articles, five review articles relating to psychosocial issues of younger women with breast cancer were excluded [24, 33–36]. They described quality of life broadly and discussed the distress associated with menopausal symptoms and fertility preservation techniques. Though the various psychosocial issues examined in these articles are important, these articles nevertheless do not discuss patients’ specific fertility-related needs and concerns but rather the vulnerability [33]; isolation [34]; support and coping [35, 36]; sexuality, body image and childbearing issues of younger women [24] and were excluded on this basis. The authors of these review articles suggest that the distress experienced by women may relate to interference with various aspects of women’s reproductive functioning, including the potential impact of treatment on fertility [24, 33–36].
Literature review strategy. Reasons for exclusion: *Publications on cancer, fertility and menopause treatments, cancer risk, other cancers, HRT, menopause, older patients and children, the development of measures, genetics, complimentary therapies, fertility, breast screening, epidemiology and aetiology, male breast cancer, decision-making, pregnancy, family perspectives, side-effects, predictors of disease free survival, clinician attitudes, oral contraceptive pill, participation in trials, and case reports. **Publications on treatments for breast cancer or menopause, side-effects of treatment, sexual dysfunction, coping, the development or use of measures, breast screening, quality of life (not referring to concerns, needs and preferences), assessment of an information intervention, role of nursing, and case studies or comments
The final sample includes 20 articles to be reviewed. Nine of the studies included in this review did not determine eligibility based on age; however, they reported on age-related differences in a sample of breast cancer survivors [5, 13, 37–42].
Identified fertility-related issues
Included in the final sample were interview studies (8 articles), survey studies (9 articles) or a combination of both (3 articles). Three themes emerged in relation to the fertility-related psychosocial needs and concerns of younger women with breast cancer. The diagnosis of cancer appears to highlight concerns regarding menstrual changes and potential infertility (Theme 1); attitudes to, and actual decisions made by women regarding, pregnancy, breastfeeding and contraception (Theme 2); and fertility-related information needs (Theme 3). Study and sample characteristics of the reviewed articles are presented in Tables 1, 2 and 3 under the thematic headings. Eight articles’ results fall under multiple headings, and these have been included in multiple tables or headings as appropriate [2, 5, 8, 10, 11, 13, 39, 41].
Concerns regarding menstrual changes and potential infertility
Thirteen studies were identified that described the concerns regarding menstrual changes and potential infertility identified by younger women with breast cancer (Table 1) [2, 5, 8, 10–12, 38, 39, 41, 43–46]. These studies show that substantial proportions of younger women are concerned about the impact of premature menopause, particularly the potential for infertility [2, 8, 10, 11, 38, 39, 45] and the inability to later fall pregnant should they want to [2, 10]. This concern is further supported by Ferrell et al.’s [41] survey which found that the worst outcome in physical well-being was in menstrual changes and fertility. Other studies have similarly identified the vulnerability of younger women with breast cancer to psychological morbidity [43, 44]. This may be related to women feeling worried about their future fertility [2], or the adverse impact on a woman’s role identities when cancer treatment forcibly removes fertility choices [5, 43–45].
Loss of fertility was of greater concern to women who had not yet completed their families and who had previous difficulty falling pregnant [10, 11, 38]. Being younger than 40 years was also associated with wanting to retain fertility [38]. Even for women who did not desire any, or any more, children the loss of menstrual function and the lack of choice about fertility was nevertheless reported as being emotionally stressful [5, 46]. Single women reported an additional concern about the delayed outcome of discovering their infertility until they had found a partner and decided to have a child [8]. Some women did not rate fertility as an important issue however [38], and in some cases, women simply assumed that cancer treatment had rendered them infertile [8].
Attitudes to, and actual decisions made by women regarding, pregnancy, breastfeeding, and contraception
Five studies described attitudes to, and actual decisions made by women regarding, pregnancy, breastfeeding and contraception (Table 2) [2, 5, 6, 8, 39, 44]. Pregnancy-related issues were identified as the second-highest concern amongst women who had not yet completed their families [2] and the breast cancer diagnosis reportedly caused women to examine their views on femininity and its relationship to motherhood [5]. For some women, pregnancy evoked positive emotions [8], for others, decisions relating to unplanned pregnancies and breastfeeding were described as particularly onerous [8].
Ganz et al. [6] investigated pregnancy incidence up to 12 months post-diagnosis amongst 577 women aged <50 years. About 5% of participants reported a pregnancy and live birth, with 11% considering pregnancy and 15% being undecided. About 12% of the women considering pregnancy had specific plans or fertility treatment underway, 7% were trying to get pregnant and 17% reported that they did fall pregnant. Reasons cited for avoiding pregnancy amongst women who were considering pregnancy included clinician recommendation (19%), concerns about risks of pregnancy (17%), and age or relationship status (29%).
Concerns about pregnancy after breast cancer often appear to be linked to fears about the impact of pregnancy on recurrence [2, 6, 8], and whether pregnancy and breastfeeding impacts on the detection of breast cancer [8], with up to 48% of women reporting a specific concern about the effects pregnancy may have on cancer [2]. Though not specifically reported as a reason to avoid pregnancy, some women surveyed reported not wanting more children, because they felt it was selfish to have a child when there was a potential that their lifespan was compromised [8]. Fear has been reported as a limitation in the ability to plan for the future or to have children in the future [39]. Interestingly Avis and colleagues [2] identified that the greater the time since diagnosis there were fewer pregnancy-related concerns.
All the women who were pregnant over the course of the interviews conducted by Connell et al. [8] wanted to breastfeed, but did not want lactation to occur in the affected breast. The majority of participants interviewed by Thewes et al. [39] said that they had sought information about their ability to breastfeed. Breastfeeding decisions were considered less of a stressor than potential termination of pregnancy following a breast cancer diagnosis [8].
Contraception was also mentioned as particularly concerning. Failed contraception was linked to fear and anxiety about recurrence [8]. For those who wished to avoid pregnancy, vasectomy was perceived to reduce their partners’ ability to father children in a future relationship, and hormonal contraception was considered unsafe and is not usually advised [8].
Fertility-related information needs
Twelve studies described fertility-related information needs of younger women with breast cancer (Table 3) [3–5, 7, 10, 11, 13, 37–41]. The findings of these studies either related to information needs about treatment options that impact on fertility or preferences for fertility-related information provision (see below).
Information needs about treatment options that impact on fertility
Many younger women investigated in these studies reported that the ability to retain fertility was an important factor in making treatment decisions. In one study, age was a significant factor in whether participants mentioned fertility as a reason for their treatment choice, with more women under 40 years citing the retention of fertility as a reason for choosing a particular cancer treatment [38]. The same study found that women with one or no children commented that fertility had been factored into treatment decision-making [38].
Similarly, Partridge and colleagues [10] found that the desire for (more) children, prior difficulty conceiving, and infertility, all influenced treatment decision-making, with 29% of the sample reporting that infertility concerns influenced treatment decisions. This retrospective survey of fertility issues in 657 premenopausal women found that 45% of participants questioned their treatment decisions (with 33% attributing this ‘questioning’ to concerns about fertility). As expected, concerns about infertility were also significantly correlated with concerns about menopause [10]. Similarly, in a study conducted by Bloom and colleagues [3], some women reported that they had regrets about the type of cancer treatment they had as a result of the lingering effects of treatment. Furthermore, in a longitudinal qualitative study of 13 women aged <40 years at diagnosis conducted by Connell et al. [8], the greatest regret stemmed from not having utilised fertility-preservation techniques at the time of early diagnosis. This could reflect that women are experiencing decisional regret. In terms of understanding the impact of cancer treatment on fertility, Dunn and Stegina [12] found that fertility issues were trivialised or not discussed by clinicians. Almost all women stressed the need for education about breast cancer treatment and the need for second opinions [3]. The majority of women with no children or very young children had sought information about the impact of their treatment on fertility [39]. Needs identified included education about breast cancer treatments and alternative options [3], as well as the need to revisit fertility-related information during the course of treatment [7]. Specific information that women wished to receive or to revisit included information about the impact of treatment on fertility, the management of menopausal symptoms and age-specific support [7].
Thewes et al. [11] found that receiving fertility-related information was considered more important than menopause-related information at the time of treatment decision-making [7, 11]. Fertility-related information was rated as most important by patients who had no children and those who planned to have children in the future [11]. Another study reported that younger women felt that their health providers did not listen to them or were insensitive to the psychological aspects of their cancer diagnosis [3]. The information about fertility and contraception was described as ambiguous and conflicting [13, 39]; the inaccessibility, inadequacy, and poor timing of fertility-related information appears to be a common experience[7, 13]. Concerns about symptoms and side-effects of treatment were mostly due to lack of information or poor recall of potential side-effects [4, 5, 7]. It is concerning that only 86% of participants in one study reported knowing that adjuvant chemotherapy might affect fertility [10]. Bloom et al. [3] have reported almost all of their participants stressed the need for education and Coyne and Borbasi [5] put forward that concerns about symptoms were mostly due to lack of information. In one study, some younger women particularly expressed a desire ‘to have one member of the hospital staff with whom you can talk to about all aspects of your condition, treatment and follow-up’ [37].
Preferences for fertility-related information provision
A common concern identified in younger women with breast cancer was their difficulty in communicating with their medical teams [3, 4]. The percentage of women who had discussed fertility-related issues with their clinicians varied across studies. Biglia et al. [40] found that more than 50% of concerned younger women had consulted with a physician about fertility. Most consulted gynaecologists (61%); oncologists (16%) and/or general practitioners (23%) were consulted less frequently [40]. Duffy et al. [4] found that 34% of participants discussed fertility with a clinician and 98% discussed the side-effects of treatment [4]. Partridge et al. [10] reported that only 51% of their participants had concerns addressed adequately, with only 71 and 72% of younger women in two retrospective surveys reporting discussing fertility issues with a clinician [10, 11]. Women also reported that it was difficult to know what questions to ask and expressed frustration with the uncertainty or lack of clarity in the answers they received [7].
The most preferred method of obtaining fertility- and menopause-related information in a retrospective study of 228 young women with breast cancer was consultation with a fertility or menopause specialist followed by a decision aid (an information booklet designed to assist with decision-making) [7, 11]. Many women believed that information about fertility should be given early in the treatment plan prior to commencement of adjuvant treatment, ideally at the time of treatment planning, and regularly reviewed throughout the treatment continuum [7, 12, 43]. Those who were dissatisfied with information from health care providers sought further information from other patients, government and community literature and help-line services, books, magazines, support groups, the internet, and mothers or older women who had been through menopause [7].
Discussion
A systematic review of the published literature demonstrates that younger breast cancer patients have significant fertility- and menopause-related needs and concerns, which are commonly not adequately addressed or discussed prior to commencing adjuvant therapy. Infertility is a very real possibility for many younger women with a diagnosis of breast cancer, and the options to potentially preserve or protect fertility are often not discussed in a timely manner. Women have reported regret at having not pursued fertility treatment [8], and the lack of uptake may be a consequence of feeling unprepared to make the major decisions required during breast cancer treatment without the availability of appropriate and timely information. The surprisingly low rate of discussions about fertility with health professionals highlights the importance of making oncologists aware of patient priorities regarding fertility. It is likely that addressing these unmet needs and informed involvement of patients in treatment decision-making will lead to improved psychosocial outcomes for patients. Knowing the risks of treatment on pregnancy, breastfeeding and contraception on recurrence also appears to be an important issue for breast cancer survivors; however high-quality information on these outcomes is currently lacking. With improved understanding of these issues, women may judge themselves ‘healthy’ enough to be a good parent, which in turn may lead to better emotional and mental health.
The importance of providing patient support throughout the breast cancer trajectory is also highlighted. These studies suggest that many concerns that cause distress and impair quality of life could be alleviated through greater emotional and informational support. A pathway for information provision and referral could be implemented (see Fig. 2) to ensure fertility-related needs and concerns are addressed effectively.
Limitations of studies reviewed and future directions for research
There is relatively little research available that identifies younger women’s fertility-related needs, and the results of many of the studies described are not definitive due to their methodological limitations. For example, most of the studies reviewed were qualitative interview studies, which describe the range of women’s attitudes about fertility-related issues, but do not allow for a determination of the degree of endorsement of such attitudes [5, 7, 8, 12, 13, 39, 41, 44, 46]. Many of the survey studies are cross-sectional in design [2, 4–7, 10, 11, 13, 37, 38, 40, 41, 44, 46], which means that changes of needs and concerns over time are not taken into account and causal relationships cannot be identified. Only one study assessed women shortly after diagnosis [4] as opposed to samples of women who were diagnosed more than 6 months ago, which may lead to recall bias. Moreover, several of the quantitative studies are based on small sample sizes, which does not allow for sub-group analyses. Clearly, there is a need for more prospective studies involving larger samples of women to achieve adequate statistical power.
Of those which were longitudinal [3, 8, 12, 43], none of these assessed women at the time of treatment decision-making. This may have led to bias as all participants would be considered to essentially have made their reproductive decisions. Also, most of the studies reviewed rely on patients’ self-reported experiences; audio- or video-recordings of actual consultations are needed to increase our understanding of patient-clinician interactions relating to the communication of fertility-related information. Such recordings would also provide the basis for audits of the current standard of care of younger women with breast cancer. Moreover, few studies included women from minority groups; future research should examine culturally and linguistically diverse samples of women.
Hormonal contraception is widely used, highly effective, reversible and popular amongst women but is contraindicated following breast cancer. Non-hormonal methods are available but these may be less reliable (such as barrier contraception) or irreversible (such as tubal ligation). Contraceptive choices are limited for breast cancer patients, who might be particularly motivated to avoid unplanned pregnancy [47]. There is little information available about patient needs and preferences regarding contraception following breast cancer.
Also, more research is needed into the attitudes of health care providers towards fertility-related issues; such research would help clarify cancer clinicians’ intentions and attitudes regarding the provision of fertility-related information, and perhaps explain the perceived inadequacy of such information currently being reported.
Finally, this review did not identify any studies that developed and evaluated information materials, such as decision aids, for younger women with early breast cancer considering their fertility-related options. Our review highlights the need to improve support, information, and education about fertility for younger women before they commence adjuvant therapies; we are currently in the process of developing and testing age- and fertility-specific materials in the clinic to meet this need.
References
Australian Bureau of Statistics (2000) Births, Australia 1999. Australian Bureau of Statistics, Canberra
Avis NE, Crawford S, Manuel J (2004) Psychosocial problems among younger women with breast cancer. Psychooncology 13:295–308. doi:10.1002/pon.744
Bloom JR, Stewart SL, Chang S et al (2004) Then and now: quality of life of young breast cancer survivors. Psychooncology 13:147–160. doi:10.1002/pon.794
Duffy CM, Allen SM, Clark MA (2005) Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J Clin Oncol 23:766–773. doi:10.1200/JCO.2005.01.134
Coyne E, Borbasi S (2006) Holding it all together: breast cancer and its impact on life for younger women. Contemp Nurse 23:157–169
Ganz PA, Greendale GA, Petersen L et al (2003) Breast cancer in younger women: reproductive and late health effects of treatment. J Clin Oncol 21:4184–4193. doi:10.1200/JCO.2003.04.196
Thewes B, Meiser B, Rickard J et al (2003) The fertility- and menopause-related information needs of younger women with a diagnosis of breast cancer: a qualitative study. Psychooncology 12:500–511. doi:10.1002/pon.685
Connell S, Patterson C, Newman B (2006) A qualitative analysis of reproductive issues raised by young Australian women with breast cancer. Health Care Women Int 27:94–110. doi:10.1080/07399330500377580
Singer D, Hunter M (1999) The experience of premature menopause: a thematic discourse analysis. J Reprod Infant Psychol 17:63–81. doi:10.1080/02646839908404585
Partridge AH, Gelber S, Peppercorn J et al (2004) Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol 22:4174–4183. doi:10.1200/JCO.2004.01.159
Thewes B, Meiser B, Taylor A et al (2005) Fertility- and menopause-related information needs of younger women with a diagnosis of early breast cancer. J Clin Oncol 23:5155–5165. doi:10.1200/JCO.2005.07.773
Dunn J, Steginga SK (2000) Young women’s experience of breast cancer: defining young and identifying concerns. Psychooncology 9:137–146. doi:10.1002/(SICI)1099-1611(200003/04)9:2<137::AID-PON442>3.0.CO;2-0
Knobf MT (2001) The menopausal symptom experience in young mid-life women with breast cancer. Cancer Nurs 24:201–210. doi:10.1097/00002820-200106000-00008 quiz 210-1
Mor V, Malin M, Allen S (1994) Age differences in the psychosocial problems encountered by breast cancer patients. J Natl Cancer Inst Monogr 16:191–197
Trief PM, Donohue-Smith M (1996) Counseling needs of women with breast cancer: what the women tell us. J Psychosoc Nurs Ment Health Serv 34:24–29
Baker F, Denniston M, Smith T et al (2005) Adult cancer survivors: how are they faring? Cancer 104:2565–2576. doi:10.1002/cncr.21488
Bakewell RT, Volker DL (2005) Sexual dysfunction related to the treatment of young women with breast cancer. Clin J Oncol Nurs 9:697–702. doi:10.1188/05.CJON.697-702
Shannon C, Smith IE (2003) Breast cancer in adolescents and young women. Eur J Cancer 39:2632–2642. doi:10.1016/S0959-8049(03)00669-5
Reichman BS, Green KB (1994) Breast cancer in young women: effect of chemotherapy on ovarian function, fertility, and birth defects. J Natl Cancer Inst Monogr 16:125–129
Sonmezer M, Oktay K (2006) Fertility preservation in young women undergoing breast cancer therapy. Oncologist 11:422–434. doi:10.1634/theoncologist.11-5-422
Dow KH, Kuhn D (2004) Fertility options in young breast cancer survivors: a review of the literature. Oncol Nurs Forum Online 31:E46–E53. doi:10.1188/04.ONF.E46-E53
Lee SJ, Schover LR, Partridge AH et al (2006) American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol 24:2917–2931. doi:10.1200/JCO.2006.06.5888
Berglund G, Nystedt M, Bolund C et al (2001) Effect of endocrine treatment on sexuality in premenopausal breast cancer patients: a prospective randomized study. J Clin Oncol 19:2788–2796
Schover LR (1994) Sexuality and body image in younger women with breast cancer. J Natl Cancer Inst Monogr 16:177–182
Rogers M, Kristjanson LJ (2002) The impact on sexual functioning of chemotherapy-induced menopause in women with breast cancer. Cancer Nurs 25:57–65. doi:10.1097/00002820-200202000-00011
Kunkel EJ, Chen EI, Kunkel EJS et al (2003) Psychiatric aspects of women with breast cancer. Psychiatr Clin North Am 26:713–724. doi:10.1016/S0193-953X(03)00038-8
Sammarco A (2001) Psychosocial stages and quality of life of women with breast cancer. Cancer Nurs 24:272–277. doi:10.1097/00002820-200108000-00005
Thompson SC, Nanni C, Schwankovsky L (1990) Patient-oriented interventions to improve communication in a medical office visit. Health Psychol 9:390–404. doi:10.1037/0278-6133.9.4.390
Fallowfield LJ, Baum M, Maguire GP (1986) Effects of breast conservation on psychological morbidity associated with diagnosis and treatment of early breast cancer. Br Med J (Clin Res Ed) 293:1331–1334
Bruera E, Willey JS, Palmer JL et al (2002) Treatment decisions for breast carcinoma: patient preferences and physician perceptions. Cancer 94:2076–2080. doi:10.1002/cncr.10393
Morris J, Ingham R (1988) Choice of surgery for early breast cancer: psychosocial considerations. Soc Sci Med 27:1257–1262. doi:10.1016/0277-9536(88)90355-3
Wang X, Cosby LG, Harris MG et al (1999) Major concerns and needs of breast cancer patients. Cancer Nurs 22:157–163. doi:10.1097/00002820-199904000-00008
Knobf MT (2006) The influence of endocrine effects of adjuvant therapy on quality of life outcomes in younger breast cancer survivors. Oncologist 11:96–110. doi:10.1634/theoncologist.11-2-96
Grosser L (2003) Meeting the needs of younger women with breast cancer. Nurs Times 99:20–22
Roche N (2006) Follow-up after treatment for breast cancer in young women. Breast 15:S71–S75. doi:10.1016/S0960-9776(07)70022-X
Schover LR (2008) Premature ovarian failure and its consequences: vasomotor symptoms, sexuality, and fertility. J Clin Oncol 26:753–758. doi:10.1200/JCO.2007.14.1655
Hwang SY, Park B-W (2006) The perceived care needs of breast cancer patients in Korea. Yonsei Med J 47:524–533
Fallowfield L, McGurk R, Dixon M (2004) Same gain, less pain: potential patient preferences for adjuvant treatment in premenopausal women with early breast cancer. Eur J Cancer 40:2403–2410. doi:10.1016/j.ejca.2004.07.013
Thewes B, Butow P, Girgis A et al (2004) The psychological needs of breast cancer survivors; a qualitative study of the shared and unique needs of younger versus older survivors. Psychooncology 13:177–189. doi:10.1002/pon.710
Biglia N, Cozzarella M, Cacciari F et al (2003) Menopause after breast cancer: a survey on breast cancer survivors. Maturitas 45:29–38. doi:10.1016/S0378-5122(03)00087-2
Ferrell BR, Grant M, Funk B et al (1996) Quality of life in breast cancer. Cancer Pract 4:331–340
Saini R, Mulcahy V (2006) Multidisciplinary approach to meeting the information needs of women with breast cancer. J Int Med Sci Acad 19:72–74
Bloom JR, Kessler L (1994) Risk and timing of counseling and support interventions for younger women with breast cancer. J Natl Cancer Inst Monogr 16:199–206
Knobf MT (2002) Carrying on: the experience of premature menopause in women with early stage breast cancer. Nurs Res 51:9–17. doi:10.1097/00006199-200201000-00003
Spencer SM, Lehman JM, Wynings C et al (1999) Concerns about breast cancer and relations to psychosocial well-being in a multiethnic sample of early-stage patients. Health Psychol 18:159–168. doi:10.1037/0278-6133.18.2.159
Wilmoth MC (2001) The aftermath of breast cancer: an altered sexual self. Cancer Nurs 24:278–286. doi:10.1097/00002820-200108000-00006
McNaught J, Reid RL, SGJAHCoB Cancer et al (2006) Progesterone-only and non-hormonal contraception in the breast cancer survivor: Joint Review and Committee Opinion of the Society of Obstetricians and Gynaecologists of Canada and the Society of Gynecologic Oncologists of Canada. J Obstet Gynaecol Can: JOGC 28:616–639
Acknowledgments
We would like to thank Ms Ursula Sansom-Daly for reviewing this manuscript. This study was funded by a Project Grant from the Cancer Council of New South Wales (ID RG 06-13). Bettina Meiser is supported by a Career Development Award from the National Health and Medical Research Council of Australia (ID 350989).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Peate, M., Meiser, B., Hickey, M. et al. The fertility-related concerns, needs and preferences of younger women with breast cancer: a systematic review. Breast Cancer Res Treat 116, 215–223 (2009). https://doi.org/10.1007/s10549-009-0401-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-009-0401-6