Abstract
Work loss is a potential adverse consequence of cancer. There is limited research on patterns and correlates of paid work after diagnosis of breast cancer, especially among ethnic minorities. Women with non-metastatic breast cancer diagnosed from June 2005 to May 2006 who reported to the Los Angeles County SEER registry were identified and asked to complete the survey after initial treatment (median time from diagnosis = 8.9 months). Latina and African American women were over-sampled. Analyses were restricted to women working at the time of diagnosis, <65 years of age, and who had complete covariate information (N = 589). The outcome of the study was missed paid work (≤1 month, >1 month, stopped all together). Approximately 44, 24, and 32% of women missed ≤1 month, >1 month, or stopped working, respectively. African Americans and Latinas were more likely to stop working when compared with Whites [OR for stop working vs. missed ≤1 month: 3.0, 3.4, (P < 0.001), respectively]. Women receiving mastectomy and those receiving chemotherapy were also more likely to stop working, independent of sociodemographic and treatment factors [ORs for stopped working vs. missed ≤1 month: 4.2, P < 0.001; 7.9, P < 0.001, respectively]. Not having a flexible work schedule available through work was detrimental to working [ORs for stopped working 18.9, P < 0.001 after adjusting for sociodemographic and treatment factors]. Many women stop working altogether after a diagnosis of breast cancer, particularly if they are racial/ethnic minorities, receive chemotherapy, or those who are employed in an unsupportive work settings. Health care providers need to be aware of these adverse consequences of breast cancer diagnosis and initial treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ability of patients with breast cancer to return to work after diagnosis and treatment is an important survivorship issue because it may have adverse consequences on quality of life and family income [1–3]. While there is a growing body of literature that suggests that cancer may not limit a women’s ability to return to work, [4–8] less is known about the impact of disease and treatment on work performance [9, 10]. Additionally, there is limited research on these issues for African American women [4, 5, 8, 9], and Latinas have been largely omitted from prior research on the impact of cancer on work outcomes.
Work-related outcomes after a cancer diagnosis may be affected by the treatments patients receive, the presence of other comorbid medical conditions, and family and employment factors. Racial and ethnic minorities may be particularly vulnerable to poor work outcomes as a result of their cancer diagnosis, because, they are often diagnosed with more advanced disease [11, 12] that often requires more aggressive treatment [13–16], and have more co-morbidities [17]. Latinas may be at additional risk because of language barriers and other cultural factors like family role function [18, 19].
The impact of employment support on work outcomes is another area that remains under-explored in cancer survivorship research [5]. Federal and state laws address work place discrimination and mandate employers to provide reasonable accommodations [20, 21]. However, the types and the degree of accommodations can vary considerably by employer and work setting. Paid sick leave, flexible work schedule, or flexibility in job tasks are examples of the accommodations suggested by the American with Disabilities Act that may help buffer adverse consequences of breast cancer treatment on work disruption. However, minority women may have jobs that are less likely to afford these accommodations, therefore putting them at higher risk for an adverse effect of breast cancer on their employment situation. There is no research to address whether workplace support factors mediate associations between race/ethnicity and negative work outcomes related to breast cancer treatment.
In order to address potential disruption in paid work for patients with breast cancer, we studied patterns and correlates of missed work during the treatment period for a population-based sample of racially and ethnically diverse women recently diagnosed with breast cancer in Los Angeles County. We examined whether factors related to patients, their cancer treatments, and degree of workplace support were associated with missed work after breast cancer diagnosis.
Patients and methods
Study population
The parent study population consisted of women who were residents of the Los Angeles County from June 2005 to May 2006. Eligibility criteria included (1) 20–79 years of age, (2) a primary diagnosis of primary ductal carcinoma in situ (DCIS) or invasive breast cancer (Stage 0–III), and (3) were able to complete a questionnaire in English or Spanish. Asian women were excluded because they were already enrolled in other studies. Latina and African–American patients were over-sampled.
Sampling and data collection
Patients were selected shortly after diagnosis (mean time from diagnosis = 8.9 months), who were reported to the Los Angeles Cancer Surveillance Program (LA-CSP)—the Surveillance, Epidemiology, and End Results (SEER) Cancer Registry for Los Angeles County. We selected all African American women based on the information obtained from the treating hospitals. Since Latina ethnicity is not accurately collected by the treating hospital at time of diagnosis, we selected all women who were designated Hispanic by the hospital as well as all women whose surname indicated a high probability of being Latina based on a list generated from the 1980 US Census [22]. We then selected an approximately 11% random sample of the remaining white (non-Spanish Surnamed) patients.
Physicians notified our intention to contact patients through the mailing of an introductory letter followed by survey materials, and a $10 cash gift to subjects. The Dillman survey method was employed to encourage response [23] (a postcard reminder to non-respondents at 2 weeks, a second letter and survey at 6 weeks, and a follow-up phone call at 10 weeks). Those with a Spanish surname received all materials in English and Spanish. The SEER clinical and treatment data from hospital-based sources were merged with survey data for 98.2% of cases. The study protocol was approved both by the Institutional Review Boards of University of Michigan and University of Southern California.
Over the study period, 1,766 were initially accrued and 68 patients were excluded because: (1) a physician refused his permission to contact, (2) the patient did not speak English or Spanish, (3) the patient was too ill or incompetent to participate, or (4) the patient denied having cancer. Of the 1,698 patients included in the final accrued sample, 179 (10.5%) could not be contacted and 296 (17.5%) of patients contacted did not participate in the survey. Thus, a final sample of 1,224 (72.0%) completed the survey (97.8% of whom completed a written survey and 2.2% of whom completed a complete telephone survey). The median time from diagnosis to return of the completed surveys was 8.9 months (SD = 3.9 months). An analysis of non-respondents versus respondents showed that there were no significant differences by age at diagnosis, race, or Hispanic ethnicity. However, compared to respondents, non-respondents were less likely to have ever married (18.9 vs. 25.2%, P = 0.005) and to have received breast conserving surgery (56.0 vs. 64.4%, P < 0.001), and were more likely to have stage II/III disease (45.7 vs. 40.3%, P < 0.001.
Study measures
The dependent variable was missed work (missed ≤1 month, >1 month, stopped work all together) derived from the question “how many days of work have you missed because of breast cancer or its treatment?” Women also reported the average number of hours worked per week which was classified as full-time (≥35 h) versus part-time work (<35 h). To characterize the work place support, we asked women if they were paid sick leave or a flexible work schedule was available through their employer/work at the time of diagnosis.
Sociodemographic factors included age at the time of diagnosis, race/ethnicity, education, family income, number supported by family income, marital status, and time from breast cancer diagnosis to survey completion. An additional variable indicated low acculturation among Latinas based on responses to the Short Acculturation Scale for Hispanics (SASH) [24]. The scale is based on four questions regarding Spanish language preference for reading and speaking, speaking at home, thinking, and speaking with friends. Responses ranged from 1 to 5 (1 = only English to 5 = only Spanish). Latinas who had a score of 4 or higher on average across the four items were categorized as having low acculturation.
Clinical factors included breast cancer stage at diagnosis (0–III) using the American Joint Committee on Cancer Staging System (collected from the SEER registry) [25] and the number of co-morbidities (chronic bronchitis/emphysema, heart disease, other cancer, diabetes, high blood pressure, stroke, arthritis). Treatment factors included primary surgical procedure (lumpectomy, mastectomy), chemotherapy (yes/no), and radiation therapy (yes/no). More detailed measures of chemotherapy and radiation therapy were evaluated to incorporate the timing of treatment but yielded similar results. Thus, we reported the results obtained using the more simple chemotherapy and radiation therapy measures.
Statistical analysis
Descriptive statistics were used to characterize the distribution of the study variables overall and by amount of missed work. Point estimates were adjusted for design effects by using a sample population weight that accounted for differential selection by race, ethnicity, and non-response. Bivariate associations between missed work and each of the independent variables were tested using the Wald’s Chi-square test. Multinomial logistic regression models were used to calculate the adjusted odds ratio for missing more work or stopping work, by sociodemographic, treatment/clinical, and work support related factors. Second-order interactions between covariates were tested and retained in models, if P value is less than 0.05. All hypotheses were specified a priori and thus no adjustments were made for multiple comparisons. However, a P-value of <0.001 can be viewed as statistically significant by the most conservative methods of adjustments for multiple comparisons.
Results
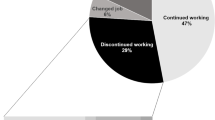
Of the 1,224 respondents, 860 were of working age (<65 years) of whom 589 (74.4%) were working at the time of breast cancer diagnosis (75.9% full-time, 24.1% part-time). African Americans were most likely to be working at the time of diagnosis (77.2%) followed by Whites and Latinas (75.7, 65.6%, respectively, P < 0.001). Among these women, 196, 160, and 235 women missed ≤1 month, >1 month, or stopped working, respectively, corresponding to 44.6, 23.9, and 31.5% using design weights (Fig. 1). Table 1 describes the characteristics of the analytic sample of women working at the time of breast cancer diagnosis, overall and by patterns of missed work. The mean age was 50.5 (SD = 8.2) and 21.9, 13.6, and 64.5% were Latina, African American, and White, respectively. The majority of women received a lumpectomy (72.7%), radiation therapy (69.7%), and chemotherapy (53.9%). More than half of women had paid sick leave (54.3%) or a flexible work schedule (60.0%) available at the time of diagnosis. Latinas were more likely to be foreign born (including Puerto Rico) (68.3 vs. 0.7 and 1.5% of African American and Whites, respectively). Most foreign-born Latinas were from Mexico (69.1%) followed by Central American countries (20.6%).
The amount of missed work varied by age, race/ethnicity, education, income, breast cancer stage, primary surgical treatment, receipt of chemotherapy, paid sick leave, and flexible work schedule (all P’s < 0.01) (Table 1). There were no statistically significant associations with number supported by family income, marital status, number of co-morbidities, radiation therapy, or full-time employment (all P’s > 0.450). A significantly higher proportion of women who stopped working received a lumpectomy (59.1%), radiation (70.1%), and chemotherapy (83.4%), and had unsupportive working environments (61.5% no paid sick leave, 75.0% no flexible work schedule). Stopping work was also prevalent in various sub-groups. For example, the prevalence of stopping work were 50.6% for Latinas, 46.1% for women receiving a lumpectomy, 48.7% for women receiving chemotherapy, 42.3% for women without a paid sick leave, and 58.9% for women without a flexible work schedule (not shown).
In multivariable analyses, the amount of missed work was significantly associated with age, race/ethnicity, education, number of co-morbidities, surgical treatment, receipt of chemotherapy, and flexible work schedule (all P’s < 0.01) (Table 2). Older women were more likely to stop working when compared with younger women (OR for 5 years increase [95% CI]: 0.6 [0.5–0.8]). Latinas and African Americans were more likely than Whites to stop working as opposed to missing ≤1 month (OR [95%CI]: 3.0 [1.2–7.4] for Latinas; 3.4 [1.3–8.6] for African American women). Women without co-morbidities were less likely to stop working compared with women with two or more co-morbidities (OR [95% CI]: 0.2 [0.1–0.5]). Additionally, women who received a mastectomy were more likely to stop working compared with women who received a lumpectomy (OR [95%CI]: 4.2 [1.8–10.0]), and women who did not receive chemotherapy were more likely to stop working compared with women who received chemotherapy (OR [95%CI]: 7.9 [3.1–20.2]). Finally, women who had no flexible work schedule available were more likely to stop working compared with women with more supportive working conditions (OR [95%CI]: 18.9 [9.1–39.4]). Similar patterns were observed for comparisons between missing >1 month vs. missing ≤1 month, however, associations were significantly less in magnitude for receipt of chemotherapy and flexible work schedule. For example, women without a flexible work schedule available were more likely to miss more than 1 month compared to women with a flexible work schedule (OR 2.2, 95% CI 1.1–4.1).
Figure 2 shows the adjusted odds ratios of missed work or stopping work by race/ethnicity and acculturation. Latinas with low acculturation were much more likely to miss >1 month or stop work compared with other groups even after controlling for all other factors. For example, the odds ratio for amount of missed work compared with Whites was 10.3 (95% CI 2.3–46.7) for stop working versus ≤1 month and 9.3 (95% CI 2.1–41.5) for >1 month versus ≤1 month. Compared to Latinas with high acculturation, Latinas with low acculturation were much more likely to be in unsupportive working environments (63.8 vs. 44.1% no paid sick leave; 79.1 vs. 46.3% no flexible work schedule).
Adjusted odds for missing more work or stopping work by race/ethnicity and acculturation (N = 589). Model adjusts for age, education, family income, number supported by family income, marital status, time from breast cancer diagnosis, number of co-morbidities, surgical procedure, receipt of radiation and chemotherapy, paid sick leave, and flexible work schedule, and full-time employment. P-value for test of overall significance 0.004
The amount of missed work was highly associated with potential adverse consequences. For example, 27.9% of women who stopped working altogether reported that they quit or lost their job versus 3.7% of women who missed ≤1 month (P < 0.001). Women who stopped working altogether were also more likely to report that they were worried about keeping their job (39.3 vs. 16.7% of women who missed ≤1 month, P < 0.001) or getting a new job in the future (58.8 vs. 21.4% of women who missed ≤1 month, P < 0.001).
Discussion
We examined patterns and correlates of missed paid work during the treatment period for a diverse sample of women recently diagnosed with breast cancer. Our results show that nearly 75% of women aged 65 and younger were working for pay at time of their breast cancer diagnosis. Many of these women reported missing work for substantial periods during the treatment period: 24% missed more than 1 month and 32% stopped working. Amount of missed work was associated with factors related to receipt of different treatments, the employment context, and patient sociodemographic factors. About one-third of patients received a mastectomy and these patients were more likely to miss work than those who received breast-conserving surgery. Over half of women in the sample received chemotherapy and half of these women stopped working altogether. The association between chemotherapy and amount of missed work persisted after controlling for sociodemographic, treatment, and work support factors. An explanation for this is that women receiving chemotherapy experience many side effects such as nausea and fatigue and that have been shown to be associated with adverse work outcomes [26, 27]. Our findings regarding associations between aggressive treatment and amount of missed work are generally uncorroborated in the literature [5, 10, 28, 29]. However, our sample is substantively different because of the multi-ethnic representation of women and a focus on the experiences during and shortly after the treatment period. Consistent with other studies, we found that women working in less supportive work settings were more vulnerable to missing more work [5]. Only about half of women in our study reported having had paid sick leave or a flexible work schedule available through work at the time of breast cancer diagnosis. Other research has found patients to report a higher level of workplace support than in our sample. For example, other investigators reported that 87% of women described their employer as accommodating their cancer treatment [5]. The lower rate found in our patients likely reflects our high proportion of Latina patients who were not represented in other studies.
Latinas and African Americans were more likely than Whites to miss more or have to stop working controlling for sociodemographic, treatment, and employment factors. While we could not find another study of work outcomes in breast cancer that included sufficient numbers of Latinas, a few studies have been examined differences in work outcomes (return to work and work absenteeism) between African Americans and Whites with mixed results [5, 8, 9]. Bouknight et al. found that African American women were less likely to return to work at 18 months from breast cancer diagnosis [5]. Conversely, in a study looking at return to work about 7 years from diagnosis, Bradley et al. found no differences in the number of missed days between African Americans and Whites [8]. The particular concern of our finding was that Latinas with low acculturation were much more vulnerable to missing more work during the treatment period than other groups. This may reflect differences in employment contexts (e.g., more isolated work settings, multiple employers, or more temporary employment) and language barriers in the work place.
Some limitations to our study merit comment. We do not know the consequences of missed work on patient and family life. Voluntary time off under favorable employment accommodations may buffer the adverse effects of arduous treatments. However, our findings suggest that in many cases missed work may have been involuntary because we observed a high frequency of prolonged work loss among patients who experienced aggressive treatment and were in an unsupportive employment settings. Furthermore, patients who stopped work altogether reported more work disruption and worried about current and future employment. However, the cross-sectional design limits inference in causal relationships. The omission of a control group of women without breast cancer obviates inference about the impact of the diagnosis on paid work experiences. Patient report of experiences of paid work, missed work, and work support may be subject to recall bias. In particular, Latinas may under-report paid work if they are in employment settings that are not fully registered with authorities. However, several lines of evidence suggest that this threat to measurement was not large. The response rate for Latinas was comparable to White non-Latinas. The majority of Latinas who reported not working for pay at diagnosis reported being homemakers. Any under-reporting of paid work status by Latinas would strengthen our findings since these women may be most vulnerable to work loss during treatment. Finally, we did not have objective measures of work conditions. Some women who had adverse work outcomes may have rated their work environments as unsupportive, irrespective of the actual conditions.
Our results have implications for clinical management of patients with breast cancer, particularly racial/ethnic minorities, and women receiving more aggressive treatments such as chemotherapy. In many cases, a modest amount of missed work may be welcomed by patients and facilitated by employers as women balance the challenges of work and family life with the burden of treatment. However, substantial periods of missed work after cancer diagnosis likely have adverse long-term financial and social consequences on patients and their families. Indeed, our results suggest that prolonged missed work even during the treatment period may put patients at risk for job loss. Clinicians and staff should be aware of potential racial/ethnic differences in employment situations and be prepared to assist patients by facilitating convenient scheduling and better management of treatment side effects. Employers need to be made similarly aware of the need for supportive environments and flexibility for patients diagnosed with cancer. Our findings motivate further research to examine the impact of different treatment experiences on paid work across the continuum of care—especially among racial/ethnic minorities and into the survivorship period—and the potential adverse effects on finances and quality of life of patients and their families.
References
Bowen DJ, Alfano CM, McGregor BA, Kuniyuki A, Bernstein L, Meeske K, Baumgartner KB, Fetherolf J, Reeve BB, Smith AW et al (2007) Possible socioeconomic and ethnic disparities in quality of life in a cohort of breast cancer survivors. Breast Cancer Res Treat 106(1):85–95. doi:10.1007/s10549-006-9479-2
Maunsell E, Brisson C, Dubois L, Lauzier S, Fraser A (1999) Work problems after breast cancer: an exploratory qualitative study. Psychooncology 8(6):467–473. doi:10.1002/(SICI)1099-1611(199911/12)8:6<467::AID-PON400>3.0.CO;2-P
Kennedy F, Haslam C, Munir F, Pryce J (2007) Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care (Engl) 16(1):17–25. doi:10.1111/j.1365-2354.2007.00729.x
Bradley CJ, Neumark D, Luo Z, Schenk M (2007) Employment and cancer: findings from a longitudinal study of breast and prostate cancer survivors. Cancer Invest 25(1):47–54. doi:10.1080/07357900601130664
Bouknight RR, Bradley CJ, Luo Z (2006) Correlates of return to work for breast cancer survivors. J Clin Oncol 24(3):345–353. doi:10.1200/JCO.2004.00.4929
Maunsell E, Drolet M, Brisson J, Brisson C, Masse B, Deschenes L (2004) Work situation after breast cancer: results from a population-based study. J Natl Cancer Inst 96(24):1813–1822
Spelten ER, Sprangers MA, Verbeek JH (2002) Factors reported to influence the return to work of cancer survivors: a literature review. Psychooncology 11(2):124–131. doi:10.1002/pon.585
Bradley CJ, Bednarek HL, Neumark D (2002) Breast cancer and women’s labor supply. Health Serv Res 37(5):1309–1328. doi:10.1111/1475-6773.01041
Bradley CJ, Oberst K, Schenk M (2006) Absenteeism from work: the experience of employed breast and prostate cancer patients in the months following diagnosis. Psychooncology 15(8):739–747. doi:10.1002/pon.1016
Drolet M, Maunsell E, Mondor M, Brisson C, Brisson J, Masse B, Deschenes L (2005) Work absence after breast cancer diagnosis: a population-based study. CMAJ 173(7):765–771. doi:10.1503/cmaj.050178
Sassi F, Luft HS, Guadagnoli E (2006) Reducing racial/ethnic disparities in female breast cancer: screening rates and stage at diagnosis. Am J Public Health 96(12):2165–2172. doi:10.2105/AJPH.2005.071761
Lantz PM, Mujahid M, Schwartz K, Janz NK, Fagerlin A, Salem B, Liu L, Deapen D, Katz SJ (2006) The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. Am J Public Health 96(12):2173–2178. doi:10.2105/AJPH.2005.072132
Hershman D, McBride R, Jacobson JS, Lamerato L, Roberts K, Grann VR, Neugut AI (2005) Racial disparities in treatment and survival among women with early-stage breast cancer. J Clin Oncol 23(27):6639–6646. doi:10.1200/JCO.2005.12.633
Katz SJ, Lantz PM, Paredes Y, Janz NK, Fagerlin A, Liu L, Deapen D (2005) Breast cancer treatment experiences of Latinas in Los Angeles County. Am J Public Health 95(12):2225–2230. doi:10.2105/AJPH.2004.057950
Du W, Simon MS (2005) Racial disparities in treatment and survival of women with stage I–III breast cancer at a large academic medical center in metropolitan Detroit. Breast Cancer Res Treat 91(3):243–248. doi:10.1007/s10549-005-0324-9
Bradley CJ, Given CW, Roberts C (2002) Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst 94(7):490–496
Adderley-Kelly B, Williams-Stephens E (2003) The relationship between obesity and breast cancer. ABNF J 14(3):61–65
Ashing-Giwa KT, Padilla GV, Bohorquez DE, Tejero JS, Garcia M (2006) Understanding the breast cancer experience of Latina women. J Psychosoc Oncol 24(3):19–52. doi:10.1300/J077v24n03_02
Ashing-Giwa KT, Padilla G, Tejero J, Kraemer J, Wright K, Coscarelli A, Clayton S, Williams I, Hills D (2004) Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psychooncology 13(6):408–428. doi:10.1002/pon.750
Short PF, Vargo MM (2006) Responding to employment concerns of cancer survivors. J Clin Oncol 24(32):5138–5141. doi:10.1200/JCO.2006.06.6316
Hoffman B (2005) Cancer survivors at work: a generation of progress. CA Cancer J Clin 55(5):271–280. doi:10.3322/canjclin.55.5.271
Word D, Perkins JR (2006) Building a Spanish surname list for the 1990s—a new approach to an old problem. US Census Bureau, Technical Working Paper No 13
Anema MG, Brown BE (1995) Increasing survey responses using the total design method. J Contin Educ Nurs 26:109–114
Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ (1987) Development of a short acculturation scale for Hispanics. Hisp J Behav Sci 9(2):183–205. doi:10.1177/07399863870092005
Benson JR, Weaver DL, Mittra I, Hayashi M (2003) The TNM staging system and breast cancer. Lancet Oncol 4(1):56–60. doi:10.1016/S1470-2045(03)00961-6
Spelten ER, Verbeek JH, Uitterhoeve AL, Ansink AC, van der Lelie J, de Reijke TM, Kammeijer M, de Haes JC, Sprangers MA (2003) Cancer, fatigue and the return of patients to work-a prospective cohort study. Eur J Cancer 39(11):1562–1567. doi:10.1016/S0959-8049(03)00364-2
Satariano WA, DeLorenze GN (1996) The likelihood of returning to work after breast cancer. Public Health Rep 111(3):236–241
Drolet M, Maunsell E, Brisson J, Brisson C, Masse B, Deschenes L (2005) Not working 3 years after breast cancer: predictors in a population-based study. J Clin Oncol 23(33):8305–8312. doi:10.1200/JCO.2005.09.500
Bushunow PW, Sun Y, Raubertas RF, Rosenthal S (1995) Adjuvant chemotherapy does not affect employment in patients with early-stage breast cancer. J Gen Intern Med 10(2):73–76. doi:10.1007/BF02600230
Acknowledgments
The study was supported by a grant from the National Cancer Institute (1R01CA109696) to the University of Michigan. Dr. Katz was supported by an Established Investigator Award in Cancer Prevention, Control, Behavioral and Population Sciences from the National Cancer Institute (K05 CA111340). The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Sect. 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract N01-PC-35139 awarded to the University of Southern California, contract N01-PC-54404 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement 1U58DP00807-01 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
The authors thank the Robert Wood Johnson Foundation Health & Society Scholars program for its financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mujahid, M.S., Janz, N.K., Hawley, S.T. et al. The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Res Treat 119, 213–220 (2010). https://doi.org/10.1007/s10549-009-0389-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-009-0389-y