Abstract
We evaluated the contribution of an Alu insertion in BRCA2 exon 3 (c.156_157insAlu) to inherited predisposition to breast/ovarian cancer in 208 families originated mostly from northern/central Portugal. We identified the c.156_157insAlu BRCA2 mutation in 14 families and showed that it accounts for more that one-fourth of deleterious BRCA1/BRCA2 mutations in breast/ovarian cancer families originated from this part of the country. This mutation originates BRCA2 exon 3 skipping and we demonstrated its pathogenic effect by showing that the BRCA2 full length transcript is derived only from the wild type allele in carriers, that it is absent in 262 chromosomes from healthy blood donors, and that it co-segregates with the disease. Polymorphic microsatellite markers were used for haplotype analysis in three informative families. In two of the three families one haplotype was shared for all but two markers, whereas in the third family all markers telomeric to BRCA2 differed from that observed in the other two. Although the c.156_157insAlu BRCA2 mutation has so far only been identified in Portuguese breast/ovarian cancer families, screening of this rearrangement in other populations will allow evaluation of whether or not it is a population-specific founder mutation and a more accurate estimation of its distribution and age.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Molecular analyses of the BRCA1 and BRCA2 genes in families suspected to have hereditary predisposition to breast/ovarian cancer have shown that most populations exhibit a wide spectrum of mutations throughout both genes. However, several founder mutations have been identified in individuals of different ancestries, including those of Ashkenazi Jewish (185delAG and 53832insC) [1], French Canadian (C4446T and 2953del3+C) [2, 3], Norwegian (1675delA and 1135insA) [4], Dutch (2804delAA and Alu-mediated deletions encompassing exons 13 and 22) [5, 6], Polish (5382insC, C61G, and 4153delA) [7], Greek (5382insC and G1738R) [8, 9], Icelandic (999del5) [10], Spanish (330A>G, 6857_6858del, and 9254_9258del) [11, 12], and Swedish (3171ins5) [13] origins. We have previously reported several novel mutations in a first characterization of the mutational spectrum of the entire coding sequences and exon–intron boundaries of the BRCA1 and BRCA2 genes and large BRCA1 rearrangements in Portuguese breast/ovarian cancer families [14].
Recently, Teugels et al. [15] identified an Alu insertion in BRCA2 exon 3 (c.156_157insAlu) in a Portuguese breast cancer patient living in Belgium. This mutation was not detectable using the conventional mutation screening techniques and originates skipping of BRCA2 exon 3 [15]. A regional founder effect has recently been described for this rearrangement in hereditary breast/ovarian cancer families mostly originated from central/southern Portugal [16]. In an attempt to gain insight into the ancestral origin and population spread of the c.156_157insAlu BRCA2 mutation, we estimated its frequency in breast/ovarian cancer families originated mostly from northern/central Portugal and analyzed the chromosomal background upon which this mutation occurs using 10 microsatellite markers surrounding the BRCA2 gene. Furthermore, because some doubts have been raised about the pathogenic effect of BRCA2 exon 3 skipping [17], we have performed segregation studies and mRNA expression analysis of c.156_157insAlu carriers and disease-free controls.
Materials and methods
Patients
This study comprised the 78 Portuguese breast/ovarian cancer families in whom no clearly deleterious BRCA1/BRCA2 mutations were found in our previous study [14] and an additional 130 BRCA1/BRCA2 negative probands that had been selected using the following the criteria: (1) families with one or more breast cancers (one of them diagnosed before the age of 50 years) and one or more ovarian cancers (BC + OC); (2) families with two or more female breast cancers, one of them diagnosed before the age of 50 years (≥2BC); (3) families with at least one case of breast cancer or ovarian cancer in association with at least one case of male breast cancer (MBC); (4) patients without family history of breast/ovarian cancer, but showing early-onset breast cancer (1BC, diagnosed before the age of 35 years), breast (diagnosed before the age of 60 years) and ovarian cancer (1BC + OC), bilateral breast carcinomas (1BlC, one of them diagnosed before the age of 50 years), or male breast cancer (1MBC, at any age). BRCAPRO mutation probabilities were estimated for all probands [18].
DNA isolation and BRCA1/BRCA2 mutation screening
Genomic DNA was extracted from peripheral leucocytes according to standard procedures and subsequently amplified using primers described by van der Hout et al. [19]. Mutation screening of the entire coding regions of BRCA1 and BRCA2 was performed by Denaturing Gradient Gel Electrophoresis (DGGE), using the IngenyphorU system (Ingeny; Goes). Sequence analysis of genomic fragments with altered DGGE mobility pattern was carried out on an Applied Biosystems’ 310 automated DNA sequencer (Foster City), using the dye terminator method. Multiplex Ligation-dependent Probe Amplification (MLPA) (MRC-Holland, Amsterdam) was used to detect large exonic BRCA1 and BRCA2 rearrangements (only 23 probands were analyzed for the latter gene) in cases that were negative for pathogenic BRCA1/BRCA2 point mutations.
Screening for the c.156_157insAlu BRCA2 mutation
The c.156_157insAlu BRCA2 mutation was screened in 208 probands and in 262 control chromosomes (healthy blood donors). In the first PCR we used primers for BRCA2 exon 3 amplification (forward primer: GTCACTGGTTAAAACTAAGGTGGG and reverse primer: GAAGCCAGCTGATTATAAGATGGTT). The cycling conditions were 94°C for 1 min, 35 cycles of 94°C for 1 min, 52°C for 1 min, and 72°C for 4 min, and a final extension of 72°C for 10 min. In the second PCR we used primers specific for the c.156_157insAlu BRCA2 mutation (forward primer: GACACCATCCCGGCTGAAA and reverse primer: CCCCAGTCTACCATATTGCAT). The cycling conditions were 97°C for 15 min, 6 cycles of 97°C for 1 min, 68°C for 1 min, and 72°C for 1 min, 6 cycles of 97°C for 1 min, 66°C for 30 s, and 72°C for 1 min, 6 cycles of 97°C for 1 min, 64°C for 30 s, and 72°C for 1 min, 22 cycles of 97°C for 1 min, 60°C for 30 s, and 72°C for 1 min, and a final extension of 72°C for 10 min. Sequence analysis of genomic fragments with the insertion was carried out on an Applied Biosystems’ 310 automated DNA sequencer (FosterCity), using the dye terminator method.
RNA isolation and transcript analysis
Frozen cell pellets from nucleated cells of patients carrying the c.155_156insAlu BRCA2 variant and from control individuals (without known BRCA1 or BRCA2 mutations) were used to extract total RNA using 1 ml of Tripure isolation reagent (Roche Diagnostics, Indianapolis, USA), according to the manufacturer’s instructions. After quantification using a NanoDrop ND-1000 spetrophotometer, One-Step RT-PCR was performed in all cases using the Superscript One-Step RT-PCR System as suggested by the manufacturer (Invitrogen, Carlsbad, USA). We used primers spanning from exon 1 to exon 6 of BRCA2 (forward primer B2Ex1F: GCTTACTCCGGCCAAAAAAGA and reverse primer B2Ex6R: GGTGTCTGACGACCCTTCACA). The cycling conditions were 50°C for 30 min, 95°C for 15 min, 40 cycles of 94°C for 30 s, 55°C for 1 min, and 72°C for 1 min, and a final extension of 72°C for 10 min. RT-PCR products were separated on a 2% agarose gel (SeaKem LE Agarose, Rockland, USA) and visualized with ethidium bromide in an image analyser ImageMaster VDS (Amersham Biosciences, Little Chalfont, UK). Individual bands were excised from the gel, purified using GFXTM PCR DNA and Gel Band Purification Kit (GE HealthCare) and sequenced as indicated above.
Microsatellite typing and haplotype analysis
A total of 14 probands and 14 family members were genotyped for polymorphic microsatellite markers flanking BRCA2 and for the c.-25G>A polymorphism. The order of the markers, the consensus repeat, and the distances relative to each other and BRCA2 are shown in Table 1. The physical distances of the genetic markers were derived from the Human Genome Browser assembly hg18 from the UCSC Genome Bioinformatics (http://www.genome.ucsc.edu/). The consensus pattern was obtained with the software Tandem Repeats Finder (http://www.tandem.bu.edu/). The primer sequences for the amplification of the markers were derived from the Human Genome database (http://www.gdb.org). All 10 markers were assayed by PCR using fluorescently end-labeled primers. PCR products were run on an ABI PRISM 310 Genetic Analyser (Applied Biosystems) together with a fluorescence labeled DNA fragment size standard. Genotyping of the c.-25G>A polymorphism was performed by sequencing. Haplotypes were reconstructed manually in the three informative families. The geographic origin of the c.156_157insAlu BRCA2 positive families was inferred from the birthplace of the oldest carrier or of the oldest affected family member most likely to be a carrier.
Results
Detection of the c.156_157insAlu BRCA2 mutation
We identified eight probands with the c.156_157insAlu mutation in our initial series of 78 patients in whom no deleterious BRCA1/BRCA2 mutation had been found by DGGE and MLPA. This finding, together with the 22 pathogenic mutations previously reported [14], raised the deleterious mutation detection rate to 30% (30/100) of all cases studied and to 37% (29/79) of those probands with a family history of breast/ovarian cancer. The c.156_157insAlu BRCA2 mutation accounts for 27% of the 30 probands with BRCA1/BRCA2 pathogenic mutations and 53% of the 15 deleterious BRCA2 mutations identified in that series of 100 probands from breast/ovarian cancer families. Furthermore, screening of the c.156_157insAlu BRCA2 mutation in 130 additional probands in whom no germline BRCA1/BRCA2 mutations have been detected by DGGE and MLPA (data not shown) revealed six additional families with this mutation. Of the 14 probands with the c.156_157insAlu BRCA2 mutation, eight belonged to ≥2BC families, three to MBC families, two to BC + OC families, and one was a 1BC + OC patient. The mutation was also detected in six affected family members but neither in eight healthy relatives nor in the 262 chromosomes of the control population.
Analysis of RNA transcripts
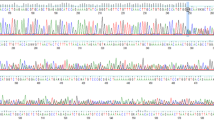
RNA splicing was evaluated by amplifying the BRCA2 coding region from exon 1 through exon 6. When the products from these reactions were visualized on agarose gels, besides a normal transcript two shorter bands were common to both the patients and controls: a transcript representing an in frame skip of exon 3 (BRCA2-Δex3) and a transcript with deletion of exon 3 plus 109 bp of exon 4 (Fig. 1). However, the band representing the BRCA2-Δex3 transcript had much higher intensity in the patients with the c.156_157insAlu BRCA2 mutation. When these fragments were excised from the gel, amplified, and sequenced, and because the PCR were designed to generate fragments that contained the c.-25G>A polymorphism, we could demonstrate that the controls heterozygous for the c.-25G>A polymorphism showed heterozygosity in the full length and the BRCA2-Δex3 transcripts, whereas the patients heterozygous for that polymorphism presented mainly one allele in the full length transcript and the other allele in the BRCA2-Δex3 transcript (Fig. 1). These findings indicate that the normal mRNA for BRCA2 is produced only from one chromosome in the patient.
RT-PCR analyses from exon 1 to exon 6 of the BRCA2 gene in c.156_157insAlu BRCA2 mutation carriers and controls. (a) Lane 1, 100 bp DNA standard. Lanes 2 and 3, patients with the c.156_157insAlu BRCA2 mutation. Lane 3, wild type control sample. A1 represents the full length transcript, A2 the BRCA2-Δex3 transcript and A3 the transcript with deletion of exon 3 plus 109 bp of exon 4 (data not shown). (b) Sequencing of the RT-PCR product (A1 band top and A2 band bottom) from a control individual with the c.-25G>A germline polymorphism (noted by an arrow), showing heterozygosity in the full length and the BRCA2-Δex3 transcripts. (c) Sequencing of the RT-PCR product (A1 band top and A2 band bottom) from a c.156_157insAlu BRCA2 mutation carrier with the c.-25G>A germline polymorphism (noted by an arrow), showing mainly one allele in the full length transcript and the other allele in the BRCA2-Δex3 transcript
Haplotype analysis
Haplotypes were phased for most of the markers for only three out of the 14 families. The results of the haplotype analyses for the three informative families are shown in Fig. 2. In one informative family, the haplotype associated with the mutation could be inferred accurately as five carriers were genotyped. In the other two families the haplotype was inferred in most instances as two carriers per family were genotyped. One haplotype was found to segregate within two families (11 and 13). The shared haplotype covered eight markers, but varied for the D13S1701 and D13S1700 alleles. In family 12 the disease associated alleles from the BRCA2 telomeric region were different from those associated with families 11 and 13. The genotypes found for the remaining probands are shown in Table 1 and the geographic origins of the c.156_157insAlu BRCA2 positive families are shown in Fig. 3.
Pedigrees of the three informative breast/ovarian cancer families and haplotype results (families 11, 12 and 13 in a, b and c, respectively). The order of the microsatellite markers is the same as in Table 1 and the alleles that segregate with the mutation are underlined. Unaffected individuals are indicated with open symbols, patients affected with breast cancer with black symbols. Bilateral breast disease is represented by striped circles and breast/ovarian cancer patients by dotted circles. Plus and minus signals represent family members with and without the c.156_157insAlu BRCA2 mutation, respectively
Map of Portugal showing the known geographical origin of the families with the c.156_157insAlu BRCA2 germline mutation. The open circles indicate the origin of the 14 families here reported and the black circles the families previously described by Machado et al. [16]
Discussion
Our findings show that the specific detection of the c.156_157insAlu BRCA2 mutation in Portuguese breast/ovarian cancer families allows a significant increase in the detection rate of BRCA1/BRCA2 mutations from 24.7% to 37% of those with a family history of cancer. This mutation rate is slightly above what has been reported in the majority of populations using similar criteria for referral to genetic counseling and testing [12, 20–22], something that might reflect the fact that we are now able to detect a mutation that escaped conventional mutation screening techniques. If we had used more strict selection criteria like those of the other major report on BRCA1/BRCA2 analysis of Portuguese breast/ovarian cancer families (BRCAPRO risk >25%, resulting in a mutation detection rate of 36%, one-sixth being the c.156_157insAlu BRCA2 mutation [16]), our mutation detection rate would have been 41%. Although this mutation rate can be seen as relatively high, it also indicates that other BRCA1/BRCA2 mutations undetectable by current-day screening methodologies may remain to be uncovered in high-risk breast/ovarian cancer families. On the other hand, five out of the 30 pathogenic mutations would have been missed had we used the generally recommended higher that 10% mutation probability criteria for genetic testing (8 of 30 if >25%). Careful selection of families after genetic counseling is therefore recommended to increase the chance of identifying all families that can benefit from genetic diagnosis of inherited predisposition to breast/ovarian cancer.
Teugels et al. [15] demonstrated that the c.156_157insAlu mutation originates an in-frame deletion of exon 3 from the BRCA2 mRNA encoding a transcriptional activation domain. On the other hand, Díez et al. [17] issued a word of caution when interpreting as pathogenic alterations causing BRCA2 exon 3 skipping, as exon 3 splicing can also be detected in normal tissues. In order to better characterize the pathological and clinical significance of this mutation, we have looked for this mutation in disease-free controls, analyzed in more detail the mRNA in carriers and noncarriers, and reconstructed haplotypes in informative families. Three separate findings corroborate the conclusion that the c.156_157insAlu BRCA2 mutation is indeed deleterious. First, BRCA2 full length transcript is derived only from the wild type allele in patients carrying the c.156_157insAlu BRCA2 mutation, whereas the BRCA2-Δex3 transcript was transcribed mostly from the mutated allele. This was demonstrated using a heterozygous polymorphism to evaluate the relative contribution of each allele to normal and BRCA2-Δex3 transcripts in patients and controls [23], the latter showing both alleles giving rise to a small proportion of the BRCA2-Δex3 transcript. Second, if the abnormal transcript with the in-frame deletion of exon 3 is fully functional, as it was suggested by Díez et al. [17], then this variant would have to be considered a polymorphism given its high frequency (8%) in families suspected to have hereditary predisposition to breast/ovarian cancer. However, we did not find the c.156_157insAlu in 262 chromosomes from healthy blood donors, allowing us to dismiss the hypothesis that it is a neutral polymorphism. Third, we could show co-segregation of this alteration and disease in six affected (but not in healthy) family members belonging to the informative families. These pieces of information allow us to confidently conclude that the c.156_157insAlu BRCA2 mutation is associated with the hereditary predisposition to breast/ovarian cancer in these families.
Alu elements are believed to insert randomly in the host genome, so the fact that this particular Alu is inserted at exactly the same position in BRCA2 exon 3 in all 14 families is by itself sufficient evidence that this represents a founder effect and not a recurrent mutation [24]. Additionally, in all c.156_157insAlu mutation carriers heterozygous for the c.-25G>A polymorphism there was a physical association between the mutation and the allele that did not contribute to wild type transcript. Nevertheless, analysis of the chromosomal background upon which a mutation occurs can be used to reconstruct its origin and age. We have performed haplotype reconstruction with ten microsatellite markers in three informative families. In two of the three families one haplotype was shared for all but two markers, whereas in the third family all markers telomeric to BRCA2 differed from that observed in the other two. A recombination event around BRCA2 could account for the latter haplotype difference, whereas the variance in allele size of one tetranucleotide repeat unit within the D13S1701 allele in two families may have been caused by slippage during DNA replication of this repeat sequence. It is not possible to determine if this marker exhibits a higher mutation rate than other markers in the BRCA2 region, as it was suggested by other studies [25], or if that mutation occurred early on during in the spreading of the population carrying the c.156_157insAlu BRCA2 mutation. If we compare the D13S1701 genotypes for all 14 c.156_157insAlu positive probands, it is tempting to say that all mutation carriers with unphased genotypes harbored the same 299 allele, but in two out of three informative families we observed that this allele did not segregate with the mutation. The possibility exists that this variation in D13S1701 is more frequent than that observed by Machado et al. [16], so care should be taken when constructing haplotypes from independent families. If that is so, estimation based on the closest recombinant markers could greatly underestimate mutation age. Although Machado et al. [16] claim that the c.156_157insAlu BRCA2 mutation has it origin 2,400–2,600 years ago in what is now central/southern Portugal, it is likely that it merely reflects their target population for genetic testing. In fact, we here show that the c.156_157insAlu BRCA2 mutation accounts for 27% of the BRCA1/BRCA2 deleterious mutations in northern/central Portugal (our main target population; Fig. 3), as compared to 16% in central/southern Portugal [16]. Although all known c.156_157insAlu BRCA2 mutations have so far been identified in Portuguese breast/ovarian cancer families, we cannot rule out that this mutation may be present in other populations and so it might have been introduced in Iberian Peninsula from somewhere else.
In summary, our study provides significantly new evidence to substantiate the pathogenicity of the c.156_157insAlu BRCA2 rearrangement and shows that this mutation is responsible for more that one-fourth of deleterious BRCA1/BRCA2 mutations in northern/central Portugal. To further evaluate whether or not it constitutes a population-specific founder mutation, one needs to perform the screening of the c.156_157insAlu BRCA2 rearrangement in other populations, which will allow for a more accurate estimation of its distribution and age.
References
Tonin P, Serova O, Lenoir G et al (1995) BRCA1 mutations in Ashkenazi Jewish women. Am J Hum Genet 57:189
Durocher F, Tonin P, Shattuck-Eidens D et al (1996) Mutation analysis of the BRCA1 gene in 23 families with cases of cancer of the breast, ovary, and multiple other sites. J Med Genet 33:814–819
Tonin PN, Mes-Masson AM, Futreal PA et al (1998) Founder BRCA1 and BRCA2 mutations in French Canadian breast and ovarian cancer families. Am J Hum Genet 63:1341–1351
Dørum A, Hovig E, Tropé C et al (1999) Three per cent of Norwegian ovarian cancers are caused by BRCA1 1675delA or1135insA. Eur J Cancer 35:779–781
Peelen T, Cornelis RS, van Vliet M et al (1996) The majority of 22 Dutch high-risk breast cancer families are due to either BRCA1or BRCA2. Eur J Hum Genet 4:225–230
Petrij-Bosch A, Peelen T, van Vliet M et al (1997) BRCA1 genomic deletions are major founder mutations in Dutch breast cancer patients. Nat Genet 17:341–345
Górski B, Jakubowska A, Huzarski T et al (2004) A high proportion of founder BRCA1 mutations in Polish breast cancer families. Int J Cancer 110:683–686
Konstantopoulou I, Rampias T, Ladopoulou A et al (2008) Greek BRCA1 and BRCA2 mutation spectrum: two BRCA1 mutations account for half the carriers found among high-risk breast/ovarian cancer patients. Breast Cancer Res Treat 107:431–441
Anagnostopoulos T, Pertesi M, Konstantopoulou I et al (2007) G1738R is a BRCA1 founder mutation in Greek breast/ovarian cancer patients: evaluation of its pathogenicity and inferences on its genealogical history. Breast Cancer Res Treat. doi:10.1007/s10549-007-9729-y
Rafnar T, Benediktsdottir KR, Eldon BJ et al (2004) BRCA2, but not BRCA1, mutations account for familial ovarian cancer in Iceland: a population-based study. Eur J Cancer 40:2788–2793
Campos B, Díez O, Odefrey F et al (2003) Haplotype analysis of the BRCA2 9254delATCAT recurrent mutation in breast/ovarian cancer families from Spain. Hum Mutat 21:452
Díez O, Osorio A, Durán M et al (2003) Analysis of BRCA1 and BRCA2 genes in Spanish breast/ovarian cancer patients: a high proportion of mutations unique to Spain and evidence of founder effects. Hum Mutat 22:301–312
Bergman A, Einbeigi Z, Olofsson U et al (2001) The western Swedish BRCA1 founder mutation 3171ins5; a 3.7 cM conserved haplotype of today is a reminiscence of a 1500-year-old mutation. Eur J Hum Genet 9:787–793
Peixoto A, Salgueiro N, Santos C et al (2006) BRCA1 and BRCA2 germline mutational spectrum and evidence for genetic anticipation in Portuguese breast/ovarian cancer families. Fam Cancer 5:379–387
Teugels E, De Brakeleer S, Goelen G et al (2005) De novo Alu element insertions targeted to a sequence common to the BRCA1 and BRCA2 genes. Hum Mutat 26:284
Machado PM, Brandão RD, Cavaco BM et al (2007) Screening for a BRCA2 rearrangement in high-risk breast/ovarian cancer families: evidence for a founder effect and analysis of the associated phenotypes. J Clin Oncol 25:2027–2034
Díez O, Gutiérrez-Enríquez S, Ramón y Cajal T et al (2007) Caution should be used when interpreting alterations affecting the exon 3 of the BRCA2 gene in breast/ovarian cancer families. J Clin Oncol 25:5035–5036
Parmigiani G, Berry D, Aguilar O (1998) Determining carrier probabilities for breast cancer-susceptibility genes BRCA1 and BRCA2. Am J Hum Genet 62:145–158
van der Hout AH, van den Ouweland AM, van der Luijt RB et al (2006) A DGGE system for comprehensive mutation screening of BRCA1 and BRCA2: application in a Dutch cancer clinic setting. Hum Mutat 27:654–666
Claes K, Poppe B, Coene I et al (2004) BRCA1 and BRCA2 germline mutation spectrum and frequencies in Belgian breast/ovarian cancer families. Br J Cancer 90:1244–1251
Perkowska M, BroZek I, Wysocka B et al (2003) BRCA1 and BRCA2 mutation analysis in breast-ovarian cancer families from northeastern Poland. Hum Mutat 21:553–554
Shih HA, Couch FJ, Nathanson KL et al (2002) BRCA1 and BRCA2 mutation frequency in women evaluated in a breast cancer risk evaluation clinic. J Clin Oncol 20:994–999
Judkins T, Hendrickson BC, Deffenbaugh AM et al (2005) Single nucleotide polymorphisms in clinical genetic testing: the characterization of the clinical significance of genetic variants and their application in clinical research for BRCA1. Mutat Res 573:168–179
Rowold DJ, Herrera RJ (2000) Alu elements and the human genome. Genetica 108:57–72
Oros KK, Leblanc G, Arcand SL et al (2006) Haplotype analysis suggest common founders in carriers of the recurrent BRCA2 mutation, 3398delAAAAG, in French Canadian hereditary breast and/ovarian cancer families. BMC Med Genet 7:23
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Peixoto, A., Santos, C., Rocha, P. et al. The c.156_157insAlu BRCA2 rearrangement accounts for more than one-fourth of deleterious BRCA mutations in northern/central Portugal. Breast Cancer Res Treat 114, 31–38 (2009). https://doi.org/10.1007/s10549-008-9978-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-008-9978-4