Abstract
Estrogen receptor α (ERα) activity is regulated by phosphorylation at several sites. Recently several antibodies specific for individual phosphorylated sites within ERα have became available. Such antibodies potentially provide invaluable tools to gain insight into the relevance in vivo of phosphorylated ERα in human breast tumors. However, validation of these antibodies for immunohistochemistry in particular is necessary in the first instance. In this study we have investigated the usefulness of several antibodies generated to specific phosphorylated sites within ERα for immunohistochemistry of formalin-fixed, paraffin-embedded human breast cancer biopsy samples. As well, these data demonstrate for the first time, the detection of multiple phosphorylated ERα forms in breast cancer (P-S104/106-ERα, P-S118-ERα, P-S167-ERα, P-S282-ERα, P-S294-ERα, P-T311-ERα, and P-S559-ERα) suggesting the possibility that profiling of phosphorylated ERα isoforms might be useful in selecting subgroups of breast cancer patients that would benefit from endocrine therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Estrogen receptor (ER) activity can be regulated by several factors including post-translational modifications such as phosphorylation [1]. ERα is made up of five functional domains (A–E) and can be phosphorylated on multiple amino acid residues [2]. Serines 104 (S104), 106 (S106), 118 (S118), and 167 (S167), are found at the N-terminal domain of the ERα protein (A/B domain), where the ligand-independent activation function (AF-1) is located. Other identified phosphorylation sites include S236 (located in the C domain) [3], S305 [4], Threonine 311 (T311) [5] and Tyrosine 537 (Y537) [6], located in the C-terminal E domain, where the ligand dependent activation function (AF-2) is present. More recently novel phosphorylation sites in the ERα protein have been identified [7].
Little is known about the relevance of phosphorylated forms of ERα in vivo. With the recent availability of antibodies to some phosphorylated ERα epitopes a few studies have been published using human breast tumour sections and immunohistochemistry (IHC) [8–10] to establish correlations with histopathological parameters and clinical outcome. Results, while limited, are often contradictory. One reason for this may be the limited validation of the antibodies used. In this study we have analyzed several antibodies generated to phospho-specific epitopes within ERα for their usefulness for IHC of formalin-fixed, paraffin-embedded human breast cancer biopsy samples banked in the Manitoba Breast Tumor Bank (MBTB) [11, 12].
Methods
Tissue microarrays
All primary invasive breast cancers (all primary breast tumors) used in the present study were obtained from the MBTB (CancerCare Manitoba and University of Manitoba; [11]). The MBTB operates with approval from the Research Ethics Board of the Faculty of Medicine, University of Manitoba. Tissues are accrued to the bank from cases at multiple centers within Manitoba, which are collected and frozen at −70°C. A portion of the frozen tissue from each case is then processed to create matched formalin-fixed paraffin-embedded and frozen tissue blocks. The histopathology of all MBTB cases has been previously assessed and entered into a computerized database to enable selection based on composition of the tissue as well as clinical-pathological parameters. After selection, cases were re-reviewed on hematoxylin and eosin (H&E) sections by a breast pathologist (PHW). Tissue collection and selection of samples for constructing TMAs has been reported before [12, 13]. Briefly, ER positive (ER+) (defined by ligand binding assay (LBA) >3 fmol/mg protein) and PgR positive status was defined as >20 fmol/mg protein by LBA. Four hundred and fifty cases were represented on the original TMAs however due to exhaustion of tumor cores from previous use of the TMAs, or incomplete data for some cases, the number (N) of tumors analysed for some of the markers was <450.
Tissue collection times
The MBTB has a cohort of breast tumors for which the collection time has been recorded. Collection time is defined as the time of removal of the biospecimen from the operating table as documented in the operating room (OR) by an OR nurse to the time of freezing and storage at −70°C or in a liquid nitrogen freezer and/or formalin fixation and FFPE processing of the biospecimen. Queries of the database at MBTB were performed by the biobank’s informatics staff. These queries returned the excision time and freezing time for ER+ breast tumor biospecimens. This cohort also had associated PgR status information also determined by LBA. From these, after ranking them by increasing time from surgery to processing, a subgroup of 100 cases was chosen by selection from alternatively shortest and the longest time period in order to maximize any possible differences due to collection times. Total ERα and some phospho-epitopes (P-S118-ERα, P-S167-ERα) were then assessed by IHC in serial sections in order to determine if detection of the phospho-epitopes varied with time of biospecimen collection in an attempt to understand the stability of these phospho-epitopes due to biospecimen collection times. As noted above the final number of cases with interpretable data, for any one epitope, was <100.
Antibodies
Antibodies used for immunoblotting and IHC assays were as follows: the antibodies against P-S104/106-ERα, P-T311-ERα, P-S282-ERα, P-S294-ERα and P-S559-ERα were rabbit polyclonal affinity purified antibodies provided by Bethyl Laboratories, Montgomery, TX, USA [14]; P-S118-ERα (16J4, Cell Signaling, USA); P-S167-ERα (Abcam, Cambridge, MA, USA) and ERα (NCL-ER, clone 6F11, Novocastra Laboratories, Newcastle, UK) antibodies were used as previously described [13].
Immunohistochemistry
Immunohistochemistry for tissue microarrays (TMAs) was performed as described previously [13]. Serial sections (5 μm) of the TMAs were stained with anti-ERα, anti-P-S104/106-ERα, anti-P-S118-ERα, anti-P-S167-ERα, anti-P-T311-ERα, anti-P-S282-ERα, anti-P-S294-ERα and anti-P-S559-ERα antibodies (Table 1). Briefly, sections were submitted to heat-induced antigen retrieval in the presence of a citrate buffer (CC1, Ventana Medical Systems, AZ, USA) using an automated tissue immunostainer (Discovery Staining Module, Ventana Medical Systems, AZ, USA). Slides were viewed and scored using standard light microscopy. Specificity of the phospho-specific antibodies generally was determined in parallel using antibodies that had been immunoabsorbed (immunoneutralized) with ~30× excess phospho-specific peptide or non-phosphorylated peptide. Total ERα IHC was as previously described [13, 15].
Quantification and cut-off selection
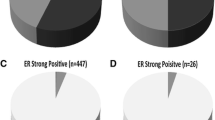
Positive nuclear immuno-staining for ERα, P-S104/106-ERα, P-S118-ERα, P-S167-ERα, P-T311-ERα, P-S282-ERα, P-S294-ERα and P-S559-ERα protein expression was assessed using semi-quantitative scoring (IHC-scores). IHC-scores derive from a semi-quantitative assessment of both staining intensity (scale 0–3) and the percentage of positive cells (0–100%), which when multiplied, generate a 0–300 score. Only nuclear staining was evaluated and scored. TMAs were evaluated independently by two investigators (GPS, PHW) and where discordance was found, cases were re-evaluated to reach consensus. Since no relevant clinical cut-off points are presently reported for any of the phosphorylated ERα sites in the literature, positivity results reported in this study were solely based on IHC-scores equivalent to the 25% percentile.
Results
Validation of phosphoantibodies for immunohistochemistry
P-S118-ERα antibody was validated for IHC previously and its specificity reported by different groups including our own [10, 16–18]. We have included P-S118-ERα staining for comparison with our previous studies. P-S118-ERα protein expression was determined in serial sections from the same TMAs, using previously described methods [10, 16]. Nuclear staining was scored and positivity for P-S118-ERα was defined as an IHC-score >0 (equivalent to 25% percentile). Three hundred and seventy cases provided interpretable IHC data and 48% of breast tumors were scored positive for P-S118-ERα (N = 177/370). P-S118-ERα was positively correlated with total ERα expression determined by IHC (r = 0.352, P < 0.0001, N = 355) and PgR LBA (r = 0.163, P = 0.0017, N = 369). Using the same cut-point (>0) median levels of PgR (LBA) expression were significantly higher in P-S118-ERα positive versus negative tumors (median PgR = 38 fmol/mg protein vs. median = 27.1 fmol/mg protein, P = 0.023, Mann–Whitney rank sum tests, two-sided). These data are consistent with previous studies [16] where a smaller number of node negative tumors only were assessed. The current cohort contains tumors from both node positive and negative patients.
The antibodies used in this study are listed in Table 1. Generally, these antibodies had been previously reported to be specific using western blotting of extracts from cells transfected separately with either wild type ERα or with the relevant site directed mutant ERα plasmids that could not be phosphorylated at the relevant residue [14] and using phosphatase treatment of the hyper-phosphorylated purified recombinant ERα (1 h incubation at 30°C resulted in loss of immuno-blotting signal) or following in vitro phosphorylation of purified baculoviral expressed ERα with specific kinases [14].
Initially we screened these antibodies for their ability to detect nuclear staining in ERα positive (determined by ligand binding of >3 fmol/mg protein and IHC) human breast tumor samples (examples shown in Fig. 1) that were formalin fixed and paraffin-embedded as previously described and stored in the MBTB [11]. IHC was carried out as described in Table 1 using the Ventana automated staining system. This approach was designed to determine antibodies that would be useful for high throughput screening of large cohorts of archived human breast tumors available as TMAs. Further, the antibodies were screened for lack of nuclear staining in a panel of ERα negative (determined by IHC and LBA) breast tumors. Examples are shown in Fig. 2.
Immunohistochemical validation of P-S167-ERα and P-S104/106-ERα phosphoantibodies in biopsies of representative human invasive breast cancers. IHC was performed as described in the “Methods”. A breast tumor section stained with the P-S167-ERα polyclonal antibody (Cat# BL1643, Montgomery, TX, USA) with strong, nuclear expression (a). An adjacent section of the same tumor using P-S167-ERα antibody pre-absorbed with a 30-fold excess of the phosphorylated peptide (b), or the non-phosphorylated ERα peptide (c) or peptide phosphorylated at T311 (d). A breast tumor section incubated with the P-S104/106-ERα polyclonal antibody (Cat# BL1636, Montgomery, TX, USA) showing specific nuclear expression (e). An adjacent section of the same tumor using pre-incubation of the P-S104/106-ERα antibody pre-absorbed with a 30-fold excess of the phosphorylated peptide (f), or non-phosphorylated ERα peptide (g) or a peptide phosphorylated at Ser 305 (h). All magnifications ×1,250
Examples of negative staining of phosphospecific ERα in ERα negative (LBA and IHC negative) breast tumor sections. a Tumor #12091 stained with P-S118-ERα antibody; b tumor #15933 stained with P-S118-ERα antibody; c tumor #11317 stained with P-S118-ERα antibody; d tumor #12091 stained with P-S167-ERα antibody; e tumor #15933 stained with P-S167-ERα antibody; f tumor #11317 stained with P-S167-ERα antibody; g tumor #12304 stained with P-T311-ERα antibody; h tumor #11317 stained with P-T311-ERα antibody; i tumor #12773 stained with P-S559-ERα antibody; j tumor #12304 stained with P-S282-ERα antibody; k tumor #12091 stained with P-S294-ERα antibody; l tumor #12304 stained with P-S559-ERα antibody. All magnifications ×1,250
Antibodies identified as potentially specific in the above screen were chosen for further analysis. Blocks from ER+ tumors showing good nuclear staining for any one antibody were then serially sectioned. One section was stained with the antibody, an adjacent section was stained with antibody that had been immunoabsorbed with ~30× excess of phosphorylated peptide (previously used to generate the antibody) and another adjacent section was stained with antibody that had been immunoabsorbed with ~30× excess of the relevant non-phosphorylated peptide. As well another serial section was stained with the antibody that had been immunoabsorbed with ~30× excess of a phosphorylated peptide representing a different site within ERα.
P-S167-ERα antibody
Figure 1a shows results of positive nuclear staining in a breast tumor section with P-S167-ERα antibody. Nuclear staining is lost in an adjacent section from the same tumor using the P-S167-ERα antibody pre-absorbed with a 30× molar excess of the peptide phosphorylated at S167 (Fig. 1b) while nuclear staining of an adjacent section was still obtained when 30× excess of the non-phosphorylated ERα peptide was used to pre-absorb the antibody (Fig. 1c). In addition, incubation of the P-S167-ERα antibody pre-absorbed with excess peptide phosphorylated at T311 had no effect on the positive nuclear P-S167-ERα antibody immunostaining (Fig. 1d). Together these data suggest that the P-S167-ERα antibody recognizes specifically ERα phosphorylated at S167 in human breast tumors using IHC.
We then assessed P-S167-ERα expression in ER+ breast cancer TMA serial sections using the above antibody. Interpretable data for P-S167-ERα expression were obtained in 400 breast cancer cases. Nuclear staining was scored and 43% of breast tumors were found positive for P-S167-ERα (N = 171/400), when P-S167-ERα positivity was defined as an IHC-score of >0 (equivalent to the 25% percentile). P-S167-ERα correlated positively with ERα expression defined by IHC (r = 0.267, P < 0.0001, N = 379), with P-S118-ERα (r = 0.463, P < 0.0001, N = 360), with P-S294-ERα (r = 0.163, P = 0.0012, N = 391), and with P-S559-ERα (r = 0.153, P = 0.0032, N = 367).
Stability of P-S118-ERα and P-S167-ERα due to collection times of biospecimens
One hundred and eighty-two cases were identified in the timed collection cohort which were ER+. Of these 160 and 161 had ER and PgR status determined by LBA, respectively. Consistent with previous data obtained by us [19] a statistically significant inverse correlation was found between collection time and ER expression as determined by LBA (Spearman r = −0.23, P = 0.0033, N = 160) but not PgR expression as determined by LBA (Spearman r = −0.11, P = 0.167, N = 161). In the subgroup chosen for IHC, no significant relationship between collection time and ERα (Spearman r = −0.07, P = 0.499, N = 99) or P-S118-ERα (Spearman r = −0.10, P = 0.35, N = 94) or P-S167-ERα (Spearman r = −0.13, P = 0.27, N = 79). Within the cohort chosen for IHC analysis the collection time ranged from 5 to 251 min (mean 66 min and median 55 min). ER protein by LBA ranged from 3.1 to 95 fmol/mg protein (mean 31 fmol/mg protein, median 31 fmol/mg protein, N = 98). PgR protein by LBA ranged from 0 to 145 fmol/mg protein (mean 29 fmol/mg protein, median 16 fmol/mg protein, N = 98). ER protein by IHC ranged from 0 to 270 (mean H-score 188, median 225 H-score, N = 99). P-S118-ERα by IHC ranged from 0 to 240 (mean H-score 60, median 30 H-score, N = 94). P-S167-ERα by IHC ranged from 0 to 270 (mean H-score 37, median 10 H-score, N = 79). Again within the IHC cohort, a statistically significant inverse correlation was found between collection time and ER expression as determined by LBA (Spearman r = −0.30, P = 0.0028, N = 98) but not PgR expression as determined by LBA (Spearman r = −0.15, P = 0.14, N = 98).
The tumors were then divided into groups based on collection times of <30 min versus ≥30 min. The results, when comparisons between time groupings were applied, are presented in Table 2. Significant decreased expression in relation to time was found for ER and PgR as determined by LBA. No significant difference was found in ER as determined by IHC and although there seemed to be a trend to decreased detection of the P-ERs in relation to increased time of collection these were not statistically significant. As well when using the 25% as a cut-off for detection or not of the P-ER, contingency analyses (Fisher’s exact test, two sided) did not find any significant differences in the frequency of detection of either phospho-epitope due to time of collection.
P-S104/106-ERα antibody
The P-S104/106-ERα antibody has not previously been validated for IHC. Good nuclear staining with this antibody was found in ERα positive breast tumor sections (Fig. 1e) but not ERα negative breast tumors (not shown). Pre-incubation of the P-S104/106-ERα antibody with a 30× excess of the appropriately phosphorylated peptide was found to abolish nuclear staining (Fig. 1f), while the non-phosphorylated ERα peptide or excess phosphorylated peptide at S305 had no effect on nuclear staining (Fig. 1g and h, respectively).
We then determined P-S104/6-ERα expression in serial sections of the breast cancer TMAs used above. Interpretable data were obtained in 301 breast cancer cases. Nuclear staining was scored and when P-S104/106-ERα positivity was defined as an IHC-score of >0 (equivalent to the 25% percentile) 67% of breast tumors were positive for P-S104/106-ERα expression (N = 201/301). P-S104/106-ERα was positively correlated with ERα (LBA) (r = 0.201, P = 0.0005, N = 301), ERα (IHC) (r = 0.21, P = 0.0004, N = 284), PgR (LBA) (r = 0.203, P = 0.0004, N = 301), P-T311-ERα, (r = 0.383, P < 0.0001, N = 293) and P-S559-ERα (r = 0.40, P < 0.0001, N = 280).
Other P-specific epitopes for ERα
Similar studies were done using antibodies to P-Threonine 311-ERα (Fig. 3a–c), P-Serine 559-ERα (Fig. 3d–f), P-Serine 294-ERα (Fig. 4a–c) and P-Serine 282-ERα (Fig. 4d–f). Good immunoneutralizable nuclear staining with these antibody was found in ERα positive breast tumor sections but not ERα negative breast tumors (Fig. 2).
Immunohistochemical validation of P-T311-ERα and P-S559-ERα phosphoantibodies in biopsies of representative human invasive breast cancers. IHC was performed as described in the “Methods”. An ER+ breast tumor section stained with the P-T311-ERα polyclonal antibody with strong, nuclear expression (a). An adjacent section of the same tumor using P-T311-ERα antibody pre-absorbed with a 30-fold excess of the phosphorylated peptide (b), or the non-phosphorylated ERα peptide (c). A breast tumor section incubated with the P-S559-ERα polyclonal antibody showing specific nuclear expression (d). An adjacent section of the same tumor using pre-incubation of the P-S559-ERα antibody pre-absorbed with a 30-fold excess of the phosphorylated peptide (e), or non-phosphorylated ERα peptide (f). All magnifications ×500
Immunohistochemical validation of P-S294-ERα and P-S282-ERα phosphoantibodies in biopsies of representative human invasive breast cancers. IHC was performed as described in the “Methods”. An ER+ breast tumor section stained with the P-S294-ERα polyclonal antibody with strong, nuclear expression (a). An adjacent section of the same tumor using P-S294-ERα antibody pre-absorbed with a 30-fold excess of the phosphorylated peptide (b), or the non-phosphorylated ERα peptide (c). A breast tumor section incubated with the P-S282-ERα polyclonal antibody showing specific nuclear expression (d). An adjacent section of the same tumor using pre-incubation of the P-S282-ERα antibody pre-absorbed with a 30-fold excess of the phosphorylated peptide (e), or non-phosphorylated ERα peptide (f). All magnifications ×500
Table 3 shows the frequency of positivity for each of the phospho-specific ERα epitopes when nuclear staining was scored and positivity was defined as an IHC-score of > equivalent to the 25% percentile. Correlations of one phospho-specific ERα epitope with another and other prognostic markers were often found and these are listed in Table 4.
Other antibodies
There were some antibodies that showed good nuclear staining such as that for P-Y537-ERα. However, the staining could not be immunoneutralized with excess phospho-peptide (up to 100× excess) and therefore was considered to be non-specific. Some antibodies such as pS305-ERα gave no nuclear staining in our hands.
Discussion
In this study we have validated several antibodies specific for phosphorylated residues within ERα in human breast tumor sections and TMA for IHC. P-S104/106-ERα, P-S118-ERα, P-S167-ERα, P-S282-ERα, P-S294-ERα, P-T311-ERα, and P-S559-ERα were measured in TMA consisting of up to 450 ERα positive invasive breast ductal carcinomas. In this cohort of ERα positive breast cancers, we found that at least 69% of all ERα positive breast tumors defined by both IHC and LBA were positive for at least one of the phospho-epitopes measured. Using cut-offs equivalent to the 25% percentile, any individual phospho-epitope was positively correlated with at least 2 other phospho-epitopes, and in the case of P-S559-ERα was positively correlated with all other phospho-ERα epitopes assessed. Therefore several ER+ breast tumors were found positive for multiple phospho-epitopes within ERα.
As might be expected the presence of any one phosphorylated form of ERα displayed an albeit weak but significant positive correlation with total ERα expression (IHC and/or LBA). However, P-S282 and P-S294 showed no correlation with any measure of total ERα expression. In the current study it was also observed that any one phosphorylated ERα was often positively correlated with the other forms of phosphorylated ERα expression. Since estrogen treatment can increase levels of ERα phosphorylated at S118, S167 and S104/106 as well as the novel phosphorylation sites [7] in human breast cancer cell lines and/or other model systems [2, 20, 21], it is possible that all or any phospho-ER of ERα represents the presence of an intact, estrogen dependent ER signalling pathway in primary human breast tumors. This conclusion is consistent with the association of most phosphorylated ERα’s often with increased PgR expression. Alternatively, it is possible that the phosphorylation of ERα at any one site may induce a conformational change which increases the likelihood of phosphorylation at the other sites [22].
Phospho-specific antibodies for ERα phosphorylated at S118 and S167 have been available for a few years now and some studies using these antibodies immunohistochemically in human breast tumor samples have been published [8–10, 16–18, 21, 23]. However, differences in association of these epitopes with established parameters in breast cancer and clinical outcome due to endocrine therapies have been found. This is not uncommon in retrospective studies of relatively small cohort sizes together with differences in IHC protocols, tissue processing and scoring, etc. But a common finding in many of these studies is that detection of phospho-ERα in breast tumors is associated with markers of an estrogen dependent ERα signalling pathway. This is quite important since it is not what would have been predicted from many laboratory results, which have shown quite clearly that kinases most often activated by growth factor receptor tyrosine kinases at the cell surface, which are often upregulated in invasive breast cancer, can directly phosphorylate ERα in particular at S118 and S167 and had been thought to be at least in part responsible for resistance to tamoxifen therapy (see references in [8, 10]). However, the currently available data in vivo do not support that hypothesis. This underscores the importance of using human breast tumor samples to test laboratory generated results as a first step in the translation of such data into clinical usefulness.
So while there are some consistencies within the available data, differences do occur. These may be due to multiple variables, however often in many but not all cases, adequate validation of antibody specificity and optimization analyses are not reported. This makes it difficult to reproduce such studies and also to interpret data and make conclusions. If a more consistent approach to validation and standardization of protocols was made, including more rigorous methods to validate the antibodies for IHC of formalin fixed paraffin embedded tissues sections, then sharing of and analyses of larger datasets on a collaborative basis could possibly be done in order to increase confidence in the results obtained and the conclusions made.
The main criteria that we have used to establish specificity of antibodies for phospho-ERα epitopes are peptide competition assays, where the nuclear signal is eliminated by pre-absorption with an excess of the phospho-peptide used to generate the antibody but little or no loss of signal when the antibody is pre-absorbed with an excess of the non-phosphorylated peptide or an excess of an irrelevant phospho-peptide. In some cases for example in Fig. 1, there appears to be a slight decrease in signal due to the excess non-phosphorylated peptide pre-absorption. This could be interpreted to mean that the antibodies are not entirely phosphospecific and have some cross-reaction with non-phosphorylated ERα. However, since the antibodies had been affinity purified and also previously tested for specificity using phosphatase and western blotting of mutant and wild-type ERα expression constructs [7], we would argue that the effects seen in our IHC study are due most likely to the heterogeneity of gene expression (staining intensity for any protein will vary amongst tumor cells within any biopsy from zero detection to highly intense, it is rare to have uniform intensity in sheets of tumor cells), orientation of the tumor cells and therefore the nuclei within any three dimensional tumor structure is not ordered or uniform therefore changing where exactly the nuclei are cut during sectioning (symmetrically through the centre or asymmetrically through another plane of the theoretical nucleus “sphere”). These variables as well as technical variables, we would argue, contribute most significantly to the differences perceived, and not due to the lack of phospho-epitope specificity, although we cannot completely eliminate this possibility, in staining intensities between adjacent sections.
In addition we have tried to assess the effects of biospecimen collection time on expression of proteins and phospho-epitopes within the ER. Previous analyses have suggested that tissue collection time can influence protein and mRNA gene expression levels [19]. In this study we have also found that ER and PgR as determined by LBA were decreased at collection times greater than 30 min. When we examined ER phosphorylated at either S118 or S167, while there was a trend to decreased expression as determined by H-score in the ≥30 min compared to the <30 min collection groups, the differences were not statistically significant. This latter result may however reflect the relatively small number of cases analyzed despite the significant finding in this same group for differences in ER and PgR measured by LBA. It still remains to be determined how the extent of the variability of epitope expression due to time of tissue collection, might be significant in comparison to the scale of the biological differences amongst biospecimens. We and others have previously found significant associations of phosphorylated ER with parameters that suggest a better clinical outcome in breast cancer and that phosphorylation is not increased in primary tumors coexpressing ER with overexpressed HER2 [8, 16, 21]. More recently, decreased expression of pS118-ERα was found to occur in surgical specimens from 80 postmenopausal patients obtained after endocrine therapy compared to the samples taken for diagnosis before surgery [24]. Together the data suggest that the presence of phosphorylated ER is functionally associated with and a marker of an intact estrogen dependent ER signalling pathway in vivo. We have therefore concluded that under the collection protocols of at least two breast tumorbanks the variability due to loss, if any, of phospho-epitopes on ER at least with respect to Ser118 and Ser167 is likely insignificant compared to the biological differences amongst the biospecimens. However, where possible this should be determined for other phospho-epitopes studied since intrinsic differences in terms of tissue type and stability/turn-over of different phospho-epitopes may occur as has been demonstrated for different mRNA previously [19]. This issue requires further investigation.
To conclude, we have extensively validated several antibodies to different phosphorylated epitopes in ERα for immunohistochemstry of FFPE sections of breast cancer biopsy samples. Our results suggest that multiple specific phosphorylated forms of ERα can be detected in primary human breast tumors in vivo. Although some decline in levels of expression of phospho-epitopes may occur due to time of collection, this was not statistically significant in the cohort studied. Often, detection of phosphorylated ER was found to be associated with another known marker of an intact estrogen dependent ER signalling pathway, i.e., PgR as determined by LBA. These data together with others in the literature therefore continue to support the idea that detection of phosphorylated forms of ERα in primary breast tumors is associated with a better response to endocrine therapy. These data raise the possibility that expanding ER status to incorporate post-translational profiling such as the phosphorylation status of ERα may provide additional useful information regarding clinical outcome and treatment response compared to ERα status alone, in breast cancer.
References
Weigel N, Moore N (2007) Steroid receptor phosphorylation: a key modulator of multiple receptor functions. Mol Endocrinol 21:2311–2319
Lannigan D (2003) Estrogen receptor phosphorylation. Steroids 68(1):1–9. doi:10.1016/S0039-128X(02)00110-1
Chen D, Pace P, Coombes R, Ali S (1999) Phosphorylation of human estrogen receptor alpha by protein kinase A regulates dimerization. Mol Cell Biol 19:1002–1015
Michalides R, Griekspoor A, Balkenende A, Verwoerd D, Janssen L, Jalink K, Floore A, Velds A, Veer LVT, Neefjes J (2004) Tamoxifen resistance by a conformational arrest of the estrogen receptor alpha after PKA activation in breast cancer. Cancer Cell 5:597–605. doi:10.1016/j.ccr.2004.05.016
Lee H, Bai W (2002) Regulation of estrogen receptor nuclear export by ligand-induced and p38-mediated receptor phosphorylation. Mol Cell Biol 22:5835–5845. doi:10.1128/MCB.22.16.5835-5845.2002
Arnold S, Vorojeikina D, Notides A (1995) Phosphorylation of tyrosine 537 on the human estrogen receptor is required for binding to an estrogen response element. J Biol Chem 270(50):30205–30212. doi:10.1074/jbc.270.50.30205
Williams C, Smith CL, Rowan BG (2007) Identification of four novel phosphorylation sites in estrogen receptor α: impact on receptor-dependent gene expression and phosphorylation by protein kinase CK2. In: The Endocrine Society’s 89th annual meeting, Toronto, Canada, 2007, pp 2–258
Jiang J, Sarwar N, Peston D, Kulinskaya E, Shousha S, Coombes R, Ali S (2007) Phosphorylation of estrogen receptor-alpha at Ser167 is indicative of longer disease-free and overall survival in breast cancer patients. Clin Cancer Res 13:5769–5776. doi:10.1158/1078-0432.CCR-07-0822
Gee J, Robertson J, Gutteridge E, Ellis I, Pinder S, Rubini M, Nicholson R (2005) Epidermal growth factor receptor/HER2/insulin-like growth factor receptor signalling and oestrogen receptor activity in clinical breast cancer. Endocr Relat Cancer 12(Suppl 1):S99–S111. doi:10.1677/erc.1.01005
Murphy LC, Cherlet T, Adeyinka A, Niu Y, Snell L, Watson P (2004) Phospho-Serine-118 estrogen receptor-alpha detection in human breast tumors in vivo. Clin Cancer Res 10:1354–1359. doi:10.1158/1078-0432.CCR-03-0112
Watson P, Snell L, Parisien M (1996) The NCIC-Manitoba Breast Tumor Bank: a resource for applied cancer research. CMAJ 155:281–283
Snell L, Watson P (2006) Breast tissue banking: collection, handling, storage, and release of tissue for breast cancer research. Methods Mol Med 120:3–24
Skliris G, Leygue E, Curtis-Snell L, Watson P, Murphy L (2006) Expression of oestrogen receptor-beta in oestrogen receptor-alpha negative human breast tumours. Br J Cancer 95:616–626. doi:10.1038/sj.bjc.6603295
Al-Dhaheri M, Rowan B (2006) Application of phosphorylation site-specific antibodies to measure nuclear receptor signaling: characterization of novel phosphoantibodies for estrogen receptor alpha. Nucl Recept Signal 4:e007
Emberley E, Niu Y, Curtis L, Troup S, Mandal S, Myers J, Gibson S, Murphy L, Watson P (2005) The S100A7-c-Jun activation domain binding protein 1 pathway enhances prosurvival pathways in breast cancer. Cancer Res 65(13):5696–5702. doi:10.1158/0008-5472.CAN-04-3927
Murphy L, Niu Y, Snell L, Watson P (2004) Phospho-Serine-118 estrogen receptor-alpha expression in primary human breast tumors in vivo is associated with better disease outcome in women treated with tamoxifen. Clin Cancer Res 10(17):5902–5906. doi:10.1158/1078-0432.CCR-04-0191
Yamashita H, Nishio M, Kobayashi S, Ando Y, Sugiura H, Zhang Z, Hamaguchi M, Mita K, Fujii Y, Iwase H (2005) Phosphorylation of estrogen receptor alpha serine 167 is predictive of response to endocrine therapy and increases post relapse survival in metastatic breast cancer. Breast Cancer Res 7:R753–R764. doi:10.1186/bcr1285
Sarwar N, Kim J, Jiang J, Peston D, Sinnett H, Madden P, Gee J, Nicholson R, Lykkesfeldt A, Shousha S et al (2006) Phosphorylation of ERalpha at serine 118 in primary breast cancer and in tamoxifen-resistant tumours is indicative of a complex role for ERalpha phosphorylation in breast cancer progression. Endocr Relat Cancer 13:851–861. doi:10.1677/erc.1.01123
Barnes R, Parisien M, Murphy L, Watson P (2008) Influence of evolution in tumor biobanking on the interpretation of translational research. Cancer Epidemiol Biomarkers Prev 17:3344–3350
Murphy L, Weitsman G, Skliris G, Teh E, LI L, Peng B, Davie J, Ung K, Niu Y, Troup S et al (2006) Potential role of estrogen receptor alpha phosphorylation at serine 118 in human breast cancer in vivo. J Steroid Biochem Mol Biol 102:139–146. doi:10.1016/j.jsbmb.2006.09.021
Weitsman G, Li L, Skliris G, Davie J, Ung K, Curtis-Snell L, Tomes L, Watson P, Murphy L (2006) Estrogen receptor-alpha phosphorylated at Serine 118 is present at the promoters of estrogen-regulated genes and is not altered due to Her2 over-expression. Cancer Res 66:10162–10170. doi:10.1158/0008-5472.CAN-05-4111
Yang C, Xin H, Kelley J, Spencer A, Brautigan D, Paschal B (2007) Ligand binding to the androgen receptor induces conformational changes that regulate phosphatase interactions. Mol Cell Biol 27:3390–3404. doi:10.1128/MCB.02411-06
Bergqvist J, Elmberger G, Ohd J, Linderholm B, Bjohle J, Hellborg H, Nordgren H, Borg A, Skoog L, Bergh J (2006) Activated ERK1/2 and phosphorylated oestrogen receptor alpha are associated with improved breast cancer survival in women treated with tamoxifen. Eur J Cancer 42:1104–1112. doi:10.1016/j.ejca.2006.01.028
Zoubir M, Mathieu M, Mazouni C, Liedtke C, Corley L, Geha S, Bouaziz J, Spielmann M, Drusche F, Symmans W et al (2008) Modulation of ER phosphorylation on serine 118 by endocrine therapy: a new surrogate marker for efficacy. Ann Oncol 19:1402–1406. doi:10.1093/annonc/mdn151
Acknowledgments
G.P.S. was funded by a Postdoctoral Fellowship from the Manitoba Health Research Council (MHRC) and previously from the CancerCare Manitoba Foundation (CCMF). S.B. is funded by an MHRC studentship. This work was supported by the Canadian Institute of Health Research (CIHR) and the Canadian Breast Cancer Research Alliance (CBCRA). We acknowledge the strong support of the CCMF for our facilities at MICB. The authors have no known conflicts of interests either financial or personal between themselves and others that might bias the work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skliris, G.P., Rowan, B.G., Al-Dhaheri, M. et al. Immunohistochemical validation of multiple phospho-specific epitopes for estrogen receptor α (ERα) in tissue microarrays of ERα positive human breast carcinomas. Breast Cancer Res Treat 118, 443–453 (2009). https://doi.org/10.1007/s10549-008-0267-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-008-0267-z