Abstract
To investigate the therapeutic effect of methylselenocysteine (MSC) combined with tamoxifen in MCF-7 breast cancer xenograft and the underlying mechanisms. MCF-7 breast cancer xenograft was established in ovariectomized female athymic nude mice and treated with tamoxifen and/or MSC. Tumor size was measured twice a week. Immunohistochemistry and TUNEL assays were used to measure ERα expression, ERα target genes (progesterone receptor (PR) and cyclin D1 expression), Ki-67 index, apoptosis and microvessel density. Combined treatment with tamoxifen and MSC synergistically inhibited tumor growth compared to MSC alone and tamoxifen alone. MSC alone or MSC + tamoxifen significantly reduced ERα, PR and cyclin D1, Ki67 index and microvessel density while increasing apoptosis in tumor tissues. These findings demonstrate synergistic growth inhibition of ERα positive breast cancer xenografts by combination of tamoxifen with organic selenium compounds. Organic selenium may provide added benefit when combined with tamoxifen in adjuvant therapy or prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Selenium is a very important micronutrient and exhibits antioxidant and anti-cancer effects in the human body. Although it is well known that organic selenium compounds are effective chemopreventatives for a number of cancers [1–3], recent studies demonstrate that selenium may also be effective as a cancer therapeutic for overt disease either alone or in combination with well-established chemotherapeutic and hormonal therapy drugs. Studies have demonstrated that organic selenium compounds, methylselenocysteine (MSC) and seleno-l-methionine (SLM), are stable, water-soluble compounds that are non-toxic in mice at 0.2 mg/mouse/day. At this dose, MSC and SLM were effective at reducing anticancer drug induced toxicity in mice and permitted increased anticancer drug dosing above the maximal tolerated dose (MTD) [4–7]. In mice, MSC is readily hydrolyzed by β-lyase to methylselenol, the presumed selenium active metabolite responsible for the anti-cancer activity of selenium. The anticancer effects of selenium are mediated through several mechanisms including decrease in cell proliferation via changes in activity of cell cycle proteins, and through induction of apoptosis in part due to increased phosphorylation of p53 and mitogen-activated protein kinase, via dephosphorylation of Akt and extracellular signal-regulated kinase 1/2, and via PARP cleavage [1, 8–11].
To date, few studies have examined the potential therapeutic efficacy of selenium in preclinical tumor models and no studies have examined selenium effects in breast tumors in combination with chemotherapy or hormonal therapy. A recent study by Gao et al. [12] demonstrated that a pharmacological dose of MSC inhibited the growth of LNCaP human prostate cancer xenografts in mice, and this growth inhibition was accompanied by downregulation of androgen receptor (AR) and prostate specific antigen (PSA). Another study by Bhattacharya et al. [13] demonstrated that MSC synergized with anticancer agents to inhibit tumor growth through both antiangiogenesis and improved drug delivery.
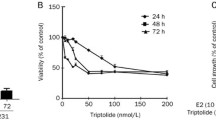
Tamoxifen (TAM), a nonsteroidal selective estrogen receptor modulator (SERM), has been widely used as a first-line therapy for estrogen receptor-α (ER-α)-positive breast cancer and also as a chemopreventative agent [14, 15]. But there are some serious side effects caused by the prolonged use of high-dose TAM, most notably in the uterus, that manifests in undesirable proliferation and increase in the risk for endometrial cancer [16–19]. Therefore new therapeutic strategies are needed that could increase TAM sensitivity so that lower doses may be used without compromising efficacy. One potential strategy is combinations of tamoxifen with other agents that will increase efficacy and decrease toxicity. Our previous in vitro studies demonstrated synergy between tamoxifen and organic selenium compounds for growth inhibition and apoptosis induction in breast cancer cell lines [20]. The present study extends the finding of synergy between selenium and tamoxifen in vitro, to demonstrate similar synergy in vivo through measurement of breast tumor xenograft growth, apoptosis, angiogenesis and ER signaling.
Materials and methods
Reagents
MSC, an organic selenium compound, was purchased from Sigma Chemicals Co. (St Louis, MO). TAM pellets (5 mg/pellet, 60-day release) and 17-β-estradiol-sustained release pellets (0.72 mg, 60-day release) were purchased from Innovative Research of America (Sarasota, FL). Matrigel Reduced Factors was purchased from BD Biosciences (Bedford, MA).
Cell culture
MCF-7 cells (tamoxifen-sensitive, ER-positive human breast cancer cell line) were purchased from the American Type Culture Collection (Rockville, MD) and cultured as previously described [21]. For inoculation into nude mice, cells were washed with PBS, incubated in PBS-EDTA for 10 min, and then resuspended in PBS prior to injection.
Animals and implantation of estradiol pellets and tumor cells
NU/NU immune-compromised female ovariectomized mice (4 weeks old) were obtained from Charles River Laboratories (Wilmington, MA) and maintained under specific pathogen-free conditions with phytoestrogen-free food and water ad libitum. Then the protocol was performed as described before [22]. Briefly, mice were used when 5 weeks old and anesthetized with a mixture of isofluorane and oxygen. Estradiol pellets were implanted subcutaneously into the right back between the ear and shoulder. For negative control mice, no estradiol pellets were administrated. MCF-7 cells were harvested from subconfluent cultures by treatment with PBS/EDTA solution and washed with PBS. About 5 × 106 cells suspension in 50 μl sterile PBS were mixed with 100 μl Matrigel and administered within both sides of the inguinal mammary fat pad through a 5 mm incision at the hypogastrium area. The wound was closed in one layer with metal wound clips.
Therapy of MCF-7 tumor xenografts
Three independent studies were conducted to examine the effects of MSC and/or TAM on MCF-7 xenograft tumors. Mice with palpable (~100 mm3) tumors were randomized into four treatment groups (five animals/group): estradiol only (E2), E2 + TAM, E2 + MSC, and E2 + TAM + MSC. MSC was suspended in PBS (1 mg/ml) and was administered via intraperitoneal injection at 100 μg/mouse/day for the E2 + MSC and the E2 + TAM + MSC groups. For TAM treatment, TAM pellets were implanted subcutaneously into the left back between the ear and shoulder. In the first set of experiments, tumor was measured twice a week for 4 weeks using a digital caliper and tumor volume was determined as 4/3π LM 2, where L is the larger radius and M is the smaller radius. In the second set of experiments, animals were euthanized by exposure to a CO2 chamber on day 3, 7, and 14 separately. In both sets of experiments, tumors were excised and either frozen in liquid Nitrogen or fixed in 10% formalin for further immunohistochemistry or TUNEL analysis. All experiments involving these animals were conducted in accordance with State and Federal laws, and the institutional guidelines for the welfare of animals in experiments. The Tulane University Animal Care and Use Committee (ACUC) reviewed the protocol for the animal experiments and gave full approval.
Immunohistochemistry
Paraffin-embedded 4-μM-thick tumor sections were analyzed by immunohistochemistry using primary monoclonal antibodies against human ERα (D-12, Santa Cruz Biotechnology), human PR (SP2, Abcam, Cambridge, MA), cyclin D1 (SP4, Abcam, Cambridge, MA), human Ki-67 (SP6, Thermo Scientific, Fremont, CA) and mouse CD34 (Santa Cruz Biotechnology). The standard ABC staining kit (sc-2017, Santa Cruz) was applied to perform immunohistochemistry. Briefly, the sections were deparaffinized, and hydrated in a graded series of ethanol solutions with a decreasing concentration. Then, 0.3% H2O2 was applied to inactivate the endogenous peroxide. For antigen retrieval, sections were heated for 20 min in Sodium Citrate buffer at 95°C, and then cooled for 20 min at room temperature. Slides were incubated with 2% goat serum in PBS for 30 min at room temperature and then with primary antibodies (1:50) in 2% goat serum or 2% goat serum alone overnight at 4°. In negative controls, the primary antibody was replaced with PBS. Biotinylated secondary antibody was added to the sections for an incubation period of 30 min. After rinsing, two to four drops of AB complex was added to the sections and incubated for 30 min. DAB solution was applied and incubated for 3 min at room temperature and sections were counterstained with hematoxylin.
Sections were viewed and digitally photographed using an Olympus U-SPT light microscope with an attached charge coupled device camera. At least four images at ×400 were taken of each tumor section with care to avoid areas of necrosis. Images were saved as JPEG files for further processing in Adobe Photoshop (Adobe Systems, Inc.). For ERα staining quantification, positive staining was quantified using NIH image analysis software, Image J, and is reported as the mean number of positive pixels/tumor section. For Ki-67 index, numbers of positively stained cells were expressed as a percentage of the total number examined. Intratumoral microvessel density (MVD) represented the mean number of CD34-positive vessels in the most vascularized area in four ×200 fields as described [23]. Any CD34 positive endothelial cell clusters clearly separated from each other were considered as single countable micro vessels. A lumen was not required to identify a vessel. All measurements were made blinded to the treatment group.
TUNEL assay
Terminal DNA transferase-mediated dUTP nick end labeling (TUNEL) assay was employed to determine in situ apoptotic DNA breaks by using the DeadEnd Colorimetric TUNEL System (Promega Inc, Madison, WI) following manufacturer’s instructions. Formalin-fixed, paraffin-embedded 4-μm-thick tumor sections were subjected to the assay. Results are reported as the percentage of positive cells, with at least 2,000 nuclei being counted per section, with care being taken to avoid areas of necrosis.
Statistics
Linear mixed-effects models were used to estimate average tumor volume across the treatment group. Each experiment was analyzed separately. The model allowed the estimation of mean effect of treatment in each group and random effects for each mouse within a group. All data on tumor volume were longitudinal and unbalanced. The differences between estimated means for all treatments averaged over days and at each day were compared. Results are expressed as means ± SEM and compared using two-sided Student’s t test. A value of P < 0.05 was considered significant.
The immunohistochemical data of ER, PR and, cyclin D1 were expressed as the arithmetic mean ± SE and each evaluated with an unpaired t test. Data of Ki-67, apoptosis and MVD were expressed as the mean number ± SE in each tumor areas. Then nonparametric comparisons (χ2) were made for each treatment group compared with their respective E2 control. A value of P < 0.05 was considered statistically significant.
Results
Synergistic MCF-7 tumor growth inhibition by combination of MSC with TAM
MCF-7 tumor xenografts do not grow in the absence of estradiol pellets (data not shown). Treatments with MSC and TAM were postponed ~10 days post-injection of MCF-7 tumor cells into mammary fat pads and implantation of estrogen pellets to permit palpable tumors to form (~100 mm3). The delay in selenium and TAM treatment was necessary to both limit drug effects on tumor prevention, and also to maximize the synergistic effects of combined TAM + MSC. The delay in TAM treatment therefore resulted in only modest tumor growth inhibition that did not reach significance. Implantation of TAM pellets prior to formation of 100 mm3 palpable tumors resulted in significant tumor growth inhibition (data not shown). The estrogen alone group exhibited rapidly growing MCF-7 tumors (Fig. 1a). For tumor size data spanning treatment days 7–28, the E2 + TAM + MSC group exhibited markedly reduced palpable tumor that differed significantly from all other treatment groups (all comparisons, P < 0.01). E2 + MSC exhibited modest tumor growth inhibition compared to the E2 group that approached significance on treatment days 23, and 28 (P = 0.095 and 0.054, respectively).
a TAM and MSC effects on MCF-7 tumor xenograft growth in nude mice. Ovariectomized nude mice supplemented with estradiol and bearing MCF-7 xenografts were grouped randomly into four groups. Five animals/group (two tumors/animal) were used for each treatment group (n = 10). Tumors were treated and tumor volumes were monitored twice a week and calculated as described in the “Materials and methods”. Results shown are from one experiment that was representative of three independent experiments. Data is represented as mean ± SEM. *P < 0.05; **P < 0.01 (Student’s t-test). b Immunohistochemical detection of ERα in MCF-7 xenograft tumor samples. Treatment groups: estrogen (E2); E2 + TAM; E2 + MSC; E2 + TAM + MSC. Two animals (two tumors/animal) were used for each treatment group (n = 4) (Paraffin section; ABC stain; ×400). c Quantification of ERα expression in MCF-7 tumor xenograft. Significant differences (Student’s t-test) are indicated with asterisks. *P < 0.05; **P < 0.01
ERα, PR, and cyclin D1 expression are downregulated by MSC and TAM
Our previous study demonstrated that selenium reduced ERα protein and ERα signaling in MCF-7 breast cancer cells in vitro [24]. In the present in vivo study, at the end of the treatment period (28 days) there was less ERα protein for all three treatment groups compared to control (Fig. 1b, c). However, the presence of MSC in treatments (MSC alone or MSC + TAM) resulted in reduced ERα at a much earlier time (within 3-days treatment). TAM alone initially increased ERα protein at day 3 and then reduced ERα protein only at the 28 day treatment. PR and cyclin D1 are ERα regulated genes and surrogate markers of functional ERα signaling. PR expression was reduced by MSC and MSC + TAM by day 7 (P < 0.01) and was further reduced by the end of the treatment period (day 28) (Fig. 2a, b). TAM alone had no effect on PR expression at day 7 but PR levels began to decrease after 14-days treatment. A different pattern of regulation was observed for cyclin D1 expression. Cyclin D1, was rapidly down-regulated after 3 days by MSC + TAM but by day 7 all treatment groups resulted in reduced cyclin D1 expression (Fig. 2c, d).
Immunohistochemical detection of PR (a) and cyclin D1 (c) in MCF-7 xenograft tumor samples. Treatment groups: estrogen (E2); E2 + TAM; E2 + MSC; E2 + TAM + MSC. Two animals (two tumors/animal) were used for each treatment group (n = 4) (Paraffin section; ABC stain; ×400). b Quantification of expression of ERα (b) and cyclin D1 (d) in MCF-7 tumor xenograft. Significant differences (Student’s t-test) are indicated with asterisks. *P < 0.05; **P < 0.01
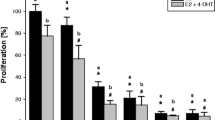
Inhibition of cell proliferation and induction of apoptosis by MSC
Tumor cell proliferation was determined by immunohistochemistry with anti-Ki-67 antibody. As shown in Fig. 3, the Ki-67 labeling index for the E2 group was ~80% during the treatment period. Of particular note was the finding that the addition of MSC resulted in a more rapid inhibition of tumor proliferation compared to TAM alone. After 7-days treatment with MSC or MSC + TAM, the Ki-67 proliferation index was significantly decreased compared to the E2 group (62.5% and 65.5% vs. 81.4%, respectively P < 0.01), whereas TAM alone had no effect. An additional 7-days treatment was needed before TAM alone resulted in decreased tumor proliferation. At 14-days treatment, TAM alone and TAM + MSC reduced the proliferation index to 41.4 and 41.6%, respectively (vs. 79.6%, E2 group, P < 0.01) whereas MSC alone had a more modest effect on inhibition of proliferation (54.2%). All treatments maintained the reduced proliferation index through the end of the treatment period.
Ki-67 expression by immunohistochemistry in MCF-7 xenograft tumor samples. a Treatment groups: estrogen (E2); E2 + TAM; E2 + MSC; E2 + TAM + MSC. Two animals (two tumors/animal) were used for each treatment group (n = 4) (Paraffin section; ABC stain; ×400). b Quantification of Ki-67 index (% of positive cells). Significant differences are indicated with asterisks. *P < 0.05; **P < 0.01; §P < 0.01 (vs. E2 + MSC)
MSC and MSC plus TAM rapidly induced apoptosis by 3-days treatment and this apoptosis was maintained for the entire treatment period (Fig. 4). TAM alone did not induce apoptosis at any timepoint. After 7-days treatment, MSC + TAM induced significantly more apoptosis than MSC alone (20.08% vs. 14.17%, P = 0.046) although no significant difference in apoptosis induction was detected between these two groups at 14 and 28 days.
TUNEL (terminal deoxynucleotidyl transferase biotin-dUTP nick end labeling) assay of MCF-7 xenograft tumor samples. a Treatment groups: estrogen (E2); E2 + TAM; E2 + MSC; E2 + TAM + MSC. Two animals (two tumors/animal) were used for each treatment group (n = 4) (Paraffin section; ABC stain; ×400). b Quantification of apoptosis (% of positive cells). Significant differences are indicated with asterisks. *P < 0.05; **P < 0.01
Inhibition of angiogenesis by MSC
Staining of mouse endothelial cells for CD34 was used to evaluate angiogenesis in terms of MVD. MVD was expressed as mean number of CD34-positive vessels as described in the “Materials and methods” section. The data demonstrated that TAM alone had no effect on MVD for the duration of the treatment period (Fig. 5). Remarkably, MSC alone but not MSC + TAM resulted in reduced MVD by 3 days compared to E2 (35.3% vs. 45.3%, P = 0.04). By 7-days treatment, both MSC and MSC + TAM decreased MVD to about 30% of control, and this reduced MVD was maintained for the entire treatment period.
CD34 immunohistochemistry in MCF-7 xenograft tumor samples. a Treatment groups: estrogen (E2); E2 + TAM; E2 + MSC; E2 + TAM + MSC. Two animals (two tumors/animal) were used for each treatment group (n = 4) (Paraffin section; ABC stain; ×400). b MVD assay of MCF-7 xenograft tumor samples as described in “Materials and methods” and MVD represents the mean number of CD34 positive vessels per field. Significant differences are indicated with asterisks. *P < 0.05; **P < 0.01
Discussion
TAM, as a nonsteroidal anti-breast cancer drug, has been widely used as both chemoprevention agent for women at risk of developing breast cancer, and as hormonal therapy for ERα positive breast cancer patients. Selenium, a well-known chemopreventative micronutrient, has recently been shown to have potential as a therapeutic for overt cancer through combination with well-established drugs, such as with the topoisomerase 1 poison irinotecan or doxorubicin [7, 11]. Our previous in vitro study demonstrated synergy with TAM and selenium for inhibition of MCF-7 cells growth and induction of apoptosis. This raises the possibility that combination of TAM with selenium may have use for treatment of breast cancer patients. To extend our previous work, the present study investigated in vivo efficacy of TAM combined with selenium using an ERα positive breast cancer xenograft model in mice. The tumor size data demonstrated that co-treatment of TAM with MSC resulted in synergistic tumor growth inhibition compared to either agent alone. Tumor growth inhibition was accompanied by decreases in ERα protein, ERα signaling, proliferation and angiogenesis, and increases in tumor cell apoptosis. Importantly, all treatments were well tolerated by mice as there was no abnormal appearance or behavior (ruffled fur/lethargy) in mice.
It should be noted that clinically, MSC is given orally and a preclinical study has used oral gavage to administer MSC to mice and have defined an oral MTD for MSC in mice [7]. In the present study, ovariectomized mice were implanted with pellets of estradiol and tamoxifen on each side of the neck. Administration of MSC by IP injection was used for ease of administration and to limit any disturbance of the pellets due to daily gavage, MSC dose was chosen based on a previous study that used 100 μg/day MSC administered IP in which no toxicity was observed [12]. This dose was based on ½ the oral MTD for MSC in mice [7]. Although a MTD for IP injection was not defined in the previous study, it is likely that 100 μg/day IP approaches the MTD for MSC since IP administration would likely deliver more bioactive drug than the oral route. We did not observe any overt toxicity nor change in body weight of the animals for the duration of the treatment (data not shown).
Treatment with MSC was started concurrent with, and not prior to TAM treatment and MSC was administered daily for the entire 28 day treatment period. Synergy between MSC and other anticancer drugs was greatest when mice were pre-treated with MSC prior to administration of anticancer drugs [7, 13]. Although the present study did not use pretreatment with MSC, it should be noted that MSC alone demonstrated rapid inhibition of MVD (3 days) much earlier than the anti-proliferative effects of TAM alone that first occurred on day 14 (Figs. 3, 5). These findings are in accordance with the previous study by Bhattacharya et al. [13] that indicated that selenium effects on the tumor vasculature were required for synergy through facilitation of drug delivery to the tumor (see below).
Our previous in vitro study with MCF-7 breast cancer cells showed that selenium could down-regulate ERα mRNA and protein [21]. In the present study, we also found that MSC alone reduced ERα protein within 3 days and low levels were maintained throughout the treatment period. These data indicate that tumor growth inhibition may be due, at least in part, to down regulation of ERα. It is well known that there is a significant positive correlation between ER and its regulated target genes PR and cyclin D1 in breast cancer cells [25, 26]. Consistent with these earlier studies, we also demonstrated that the reduction of ERα protein by MSA or MSA + TAM either preceded or coincided with reduction in ERα signaling (PR and cyclin D1) suggesting that the loss of ERα protein was the major contributing factor to loss of ERα signaling. In stark contrast to MSC, TAM also reduced ERα protein but only after 28-days treatment. Nevertheless, TAM also reduced ERα signaling at times well before TAM-induced loss of ERα protein. These findings indicate that in contrast to MSC, TAM effects on reduction in ERα signaling in MCF-7 tumor xenograft are the result of inhibition of ERα function and not loss of ERα protein.
The most significant difference between effects of TAM and MSC on tumor growth inhibition was at the level of apoptosis. TAM did not induce apoptosis whereas MSC and MSC + TAM significantly increased apoptosis throughout the treatment period. These results were similar to in vitro data from our lab [21, 24] and an accepted manuscript to Mol. Cancer Ther. [20] and others [11]. With the exception that MSC + TAM induced more apoptosis at day 7 treatment compared to MSC alone, there were no other differences in apoptosis induction by MSC compared to MSC + TAM.
While this difference in apoptosis induction at day 7 for the MSC and MSC + TAM treatment groups was indeed significant, differences in apoptosis alone could not likely explain the synergistic tumor growth inhibition that was observed with MSC + TAM compared to MSC alone or TAM alone. Differences in tumor cell proliferation were likely a contributing factor to the different anti-tumor efficacy among the treatment groups. MSC and MSC + TAM inhibited proliferation by 7 days whereas TAM required 14-days treatment before significant inhibition of proliferation was observed. However, during the later treatment periods (days 14–28), TAM and TAM + MSC resulted in significantly greater inhibition of proliferation than MSC alone.
Selenium has been reported to interrupt tumor angiogenesis through inhibiting endothelial cell growth. The mechanisms involved are apoptosis induction and cell cycle inhibition of vascular endothelial cells [27–29]. Bhattacharya et al. [13] recently demonstrated that the antiangiogenesis effect of selenium resulted in vascular maturation in tumors. The vascular maturation was proposed to underlie the synergy of selenium with anticancer drugs through improved anticancer drug delivery. In the present study, TAM had no effect on reducing angiogenesis whereas MSC significantly attenuated angiogenesis within 3 and 7 days, respectively. Taken together, these data demonstrate significant differences in the anti-tumor effects of TAM compared to MSC that may reveal potential intersections for the synergistic growth inhibition by MSC + TAM. In general, TAM resulted in a cytostatic, anti-proliferative effect on MCF-7 tumor xenografts without induction of apoptosis nor effects on angiogenesis. The decreased proliferation in response to TAM was likely due, in part, to decreased ER signaling and suppression of critical cell cycle regulatory genes such as cyclin D1. Similar to TAM, MSC also exhibited anti-proliferative effects on MCF-7 tumors. However more importantly, at very early times (day 3) MSC exhibited the additional benefits of inducing a very robust apoptosis and reducing angiogenesis in MCF-7 tumors. It is very likely that antiangiogenesis and tumor vessel stabilization induced by MSC could result in more delivery of TAM to the tumor supporting a more robust cytostatic action. In this regard, there is a strong rationale to test whether pretreatment with selenium prior to TAM would increase antitumor efficacy [7, 13, 30].
Although differences in mechanisms for tumor growth inhibition by TAM compared to MSC were clear, mechanistic differences that could explain the synergistic growth inhibition of MSC + TAM compared to MSC alone were not readily apparent. Although there was no difference in apoptosis induction, anti-angiogenesis effects, nor loss of ERα protein between the two treatment groups, a closer examination of timepoints revealed significant time dependent differences in two potentially critical events that could have contributed to the synergistic tumor growth inhibition by MSC + TAM. MSC + TAM resulted in significant reduction in cyclin D1 protein by day 3 whereas MSC alone did not reduce cyclin D1 levels until day 7 (Fig. 2c, d). Furthermore, at days 14 and 28, MSC + TAM resulted in quantitatively greater reduction in proliferation than MSC alone and this inhibition was comparable to TAM alone. These findings suggest that the cytostatic, antiproliferative effects contributed by TAM greatly enhanced the anti-tumor effect of MSC with the combination of both agents resulting in synergistic tumor growth inhibition.
The present study provides the preclinical ‘proof of principle’ evidence that selenium synergizes with TAM for inhibition of ERα positive breast cancer xenografts. A recent phase I study reported for the first time that high dose selenium (SLM at 7,200 mg/day) can be given to humans without toxicity demonstrating the feasibility of clinical trials using organic selenium compounds [31]. Taken together, these findings provide a strong rationale to verify the therapeutic approach of high dose selenium combined with TAM in breast cancer patients with ERα positive breast cancer either the neoadjuvant, adjuvant or metastatic settings.
Abbreviations
- MSC:
-
Methylselenocysteine
- ERα:
-
Estrogen receptor α
- PR:
-
Progesterone receptor
- TAM:
-
Tamoxifen
- MVD:
-
Microvessel density
- E2:
-
Estradiol
- AR:
-
Androgen receptor
- PSA:
-
Prostate specific antigen
- PARP:
-
Poly ADP-ribose polymerase
- TUNEL:
-
Terminal DNA transferase-mediated dUTP nick end labeling
References
Dong Y, Ganther HE, Stewart C et al (2002) Identification of molecular targets associated with selenium-induced growth inhibition in human breast cells using cDNA microarrays. Cancer Res 62:708–714
Wang Z, Jiang C, Lu J (2002) Induction of caspase-mediated apoptosis and cell-cycle G1 arrest by selenium metabolite methylselenol. Mol Carcinog 34:113–120. doi:10.1002/mc.10056
Sinha R, Medina D (1997) Inhibition of cdk2 kinase activity by methylselenocysteine in synchronized mouse mammary epithelial tumor cells. Carcinogenesis 18:1541–1547. doi:10.1093/carcin/18.8.1541
Ip C, Zhu Z, Thompson HJ et al (1999) Chemoprevention of mammary cancer with Se-allylselenocysteine and other selenoamino acids in the rat. Anticancer Res 19:2875–2880
Ip C (1998) Lessons from basic research in selenium and cancer prevention. J Nutr 128:1845–1854
Clark LC, Combs GF Jr, Turnbull BW et al (1996) Effects of selenium supplementation for cancer prevention in patients with carcinoma of the skin. A randomized controlled trial. Nutritional prevention of cancer study group. JAMA 276:1957–1963. doi:10.1001/jama.276.24.1957
Cao S, Durrani FA, Rustum YM (2004) Selective modulation of the therapeutic efficacy of anticancer drugs by selenium containing compounds against human tumor xenografts. Clin Cancer Res 10:2561–2569. doi:10.1158/1078-0432.CCR-03-0268
Ip C, Dong Y (2001) Methylselenocysteine modulates proliferation and apoptosis biomarkers in premalignant lesions of the rat mammary gland. Anticancer Res 21:863–867
Lu J, Jiang C, Kaeck M et al (1995) Dissociation of the genotoxic and growth inhibitory effects of selenium. Biochem Pharmacol 50:213–219. doi:10.1016/0006-2952(95)00119-K
Dong Y, Zhang H, Hawthorn L et al (2003) Delineation of the molecular basis for selenium-induced growth arrest in human prostate cancer cells by oligonucleotide array. Cancer Res 63:52–59
Li S, Zhou Y, Wang R et al (2007) Selenium sensitizes MCF-7 breast cancer cells to doxorubicin-induced apoptosis through modulation of phospho-Akt and its downstream substrates. Mol Cancer Ther 6:1031–1038. doi:10.1158/1535-7163.MCT-06-0643
Lee SO, Yeon Chun J, Nadiminty N et al (2006) Monomethylated selenium inhibits growth of LNCaP human prostate cancer xenograft accompanied by a decrease in the expression of androgen receptor and prostate-specific antigen (PSA). Prostate 66:1070–1075. doi:10.1002/pros.20329
Bhattacharya A, Seshadri M, Oven SD et al (2008) Tumor vascular maturation and improved drug delivery induced by methylselenocysteine leads to therapeutic synergy with anticancer drugs. Clin Cancer Res 14:3926–3932. doi:10.1158/1078-0432.CCR-08-0212
Love RR (1989) Tamoxifen therapy in primary breast cancer: biology, efficacy, and side effects. J Clin Oncol 7:803–815
Jordan VC (1992) The strategic use of antiestrogens to control the development and growth of breast cancer. Cancer 70:977–982
Fisher B, Costantino JP, Wickerham DL et al (1998) Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 90:1371–1388. doi:10.1093/jnci/90.18.1371
Fornander T, Rutqvist LE, Cedermark B et al (1989) Adjuvant tamoxifen in early breast cancer: occurrence of new primary cancers. Lancet 1:117–120. doi:10.1016/S0140-6736(89)91141-0
Johnston SR, Dowsett M, Smith IE (1992) Towards a molecular basis for tamoxifen resistance in breast cancer. Ann Oncol 3:503–511
Osborne CK (1998) Tamoxifen in the treatment of breast cancer. N Engl J Med 339:1609–1618. doi:10.1056/NEJM199811263392207
Li Z, Carrier L, Rowan BG (2008) Methylseleninic acid synergizes with tamoxifen to induce caspase-mediated apoptosis in breast cancer cells. Mol Cancer Ther 7:3056–3063. doi:10.1158/1535-7163.MCT-07-2142
Shah YM, Kaul A, Dong Y et al (2005) Attenuation of estrogen receptor alpha (ERalpha) signaling by selenium in breast cancer cells via downregulation of ERalpha gene expression. Breast Cancer Res Treat 92:239–250. doi:10.1007/s10549-005-3203-5
Salvo VA, Boue SM, Fonseca JP et al (2006) Antiestrogenic glyceollins suppress human breast and ovarian carcinoma tumorigenesis. Clin Cancer Res 12:7159–7164. doi:10.1158/1078-0432.CCR-06-1426
Hansen S, Grabau DA, Rose C et al (1998) Angiogenesis in breast cancer: a comparative study of the observer variability of methods for determining microvessel density. Lab Invest 78:1563–1573
Shah YM, Al Dhaheri M, Dong Y et al (2005) Selenium disrupts estrogen receptor (alpha) signaling and potentiates tamoxifen antagonism in endometrial cancer cells and tamoxifen-resistant breast cancer cells. Mol Cancer Ther 4:1239–1249. doi:10.1158/1535-7163.MCT-05-0046
Hui R, Cornish AL, McClelland RA et al (1996) Cyclin D1 and estrogen receptor messenger RNA levels are positively correlated in primary breast cancer. Clin Cancer Res 2:923–928
Moy B, Goss PE (2006) Estrogen receptor pathway: resistance to endocrine therapy and new therapeutic approaches. Clin Cancer Res 12:4790–4793. doi:10.1158/1078-0432.CCR-06-1535
Jiang C, Jiang W, Ip C et al (1999) Selenium-induced inhibition of angiogenesis in mammary cancer at chemopreventive levels of intake. Mol Carcinog 26:213–225. doi:10.1002/(SICI)1098-2744(199912)26:4<213::AID-MC1>3.0.CO;2-Z
Jiang C, Kim KH, Wang Z et al (2004) Methyl selenium-induced vascular endothelial apoptosis is executed by caspases and principally mediated by p38 MAPK pathway. Nutr Cancer 49:174–183. doi:10.1207/s15327914nc4902_9
Wang Z, Hu H, Li G et al (2008) Methylseleninic acid inhibits microvascular endothelial cell cycle progression and decreases tumor microvessel density. Int J Cancer 122:15–24. doi:10.1002/ijc.23077
Rustum Y, Cao S, Durrani F et al (2004) Se-(methyl)selenocysteine (MSC) potentiates the antitumor activity of irinotecan against human tumor xenografts and protects against drug induced toxicity. J Clin Oncol 22:2068 (meeting abstracts)
Fakih MG, Pendyala L, Brady W et al (2008) A phase I and pharmacokinetic study of selenomethionine in combination with a fixed dose of irinotecan in solid tumors. Cancer Chemother Pharmacol 62:499–508. doi:10.1007/s00280-007-0631-4
Acknowledgment
This project was supported, in part, by grants from the Louisiana Cancer Research Consortium to BGR.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Z., Carrier, L., Belame, A. et al. Combination of methylselenocysteine with tamoxifen inhibits MCF-7 breast cancer xenografts in nude mice through elevated apoptosis and reduced angiogenesis. Breast Cancer Res Treat 118, 33–43 (2009). https://doi.org/10.1007/s10549-008-0216-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-008-0216-x