Abstract
Purpose An estimated 45–80% of breast cancer patients use antioxidant supplements after diagnosis, and use of antioxidant supplements during breast cancer treatment is common. Dietary supplements with antioxidant effects include vitamins, minerals, phytonutrients, and other natural products. We conducted a comprehensive review of literature on the associations between antioxidant supplement use during breast cancer treatment and patient outcomes. Methods Inclusion criteria were: two or more subjects; clinical trial or observational study design; use of antioxidant supplements (vitamin C, vitamin E, antioxidant combinations, multivitamins, glutamine, glutathione, melatonin, or soy isoflavones) during chemotherapy, radiation therapy, and/or hormonal therapy for breast cancer as exposures; treatment toxicities, tumor response, recurrence, or survival as outcomes. Results We identified 22 articles that met those criteria. Their findings did not support any conclusions regarding the effects of individual antioxidant supplements during conventional breast cancer treatment on toxicities, tumor response, recurrence, or survival. A few studies suggested that antioxidant supplements might decrease side effects associated with treatment, including vitamin E for hot flashes due to hormonal therapy and glutamine for oral mucositis during chemotherapy. Underpowered trials suggest that melatonin may enhance tumor response during treatment. Conclusion The evidence is currently insufficient to inform clinician and patient guidelines on the use of antioxidant supplements during breast cancer treatment. Thus, well designed clinical trials and observational studies are needed to determine the short- and long-term effects of such agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2008, approximately 180,000 women will be diagnosed with breast cancer [1], and an estimated 45–80% of these women will use antioxidant supplements after diagnosis, including during breast cancer treatment [2–12]. However, the effects of antioxidant supplements during radiation therapy, chemotherapy, and hormonal therapy on treatment toxicities, tumor response, recurrence, and survival are unknown [13–15], and guidelines regarding the use of antioxidant supplements during cancer treatment are inconsistent [16].
Many forms of chemotherapy and radiation therapy act primarily through oxidative stress pathways [17–19]. The purpose of these treatments is to induce the apoptotic cascade, through mechanisms such as altering DNA replication and disrupting mitochondrial membranes. However, these treatments may also damage healthy tissues, such as the oral mucosa and the heart. Some investigators have hypothesized that antioxidant supplements can provide protection against these treatment toxicities, which can be dose-limiting, can cause morbidity, and may contribute to mortality [20–24]. Others have expressed the concern that, like some treatment agents, antioxidant supplements may not differentiate between healthy tissue and tumors; if antioxidant supplements protect healthy tissue, they may simultaneously protect tumor tissue from treatment agents [14, 25]. Still other investigators have suggested that antioxidant supplements may actually potentiate chemotherapy and radiation therapy either by acting as pro-oxidants or by facilitating exposure of the tumor to reactive oxygen species [20, 21]. None of these theories is supported by solid clinical data. A recently published literature review on the use of antioxidants during radiation therapy and chemotherapy for any cancer type concluded that, despite insufficient evidence of harmful effects, antioxidant use should be discouraged due to the possibility that it might protect tumors and reduce survival [13].
An antioxidant supplement can be broadly defined as any dietary supplement that exerts antioxidant actions. Antioxidant supplements can be purchased over the counter individually or in combination with other antioxidants, vitamins, or vitamins and minerals as components of multivitamins. Many cancer patients believe that antioxidant supplements taken during treatment may counteract oxidative damage to healthy tissues, have direct anti-cancer activity, or confer general health benefits. Some supplements used primarily for specific purposes (e.g., soy isoflavones to counter hot flashes, melatonin to enhance immune function, and glutamine to prevent stomatitis) also have general antioxidant actions.
To our knowledge, there are no reviews of the literature on the effects of antioxidant supplementation specifically during breast cancer treatment. This review summarizes the findings of clinical trials and observational studies regarding the effects of antioxidant supplements during breast cancer treatment on treatment-related toxicities, tumor response, recurrence, and survival.
Methods
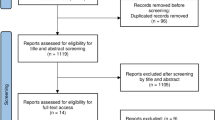
Observational studies and clinical trials included in this review were identified through repeated literature searches on PubMed conducted July 2006 through October 2007. Combinations of the following reference terms were used as both keywords and subject terms during the searches:
-
Cancer site—breast cancer, breast neoplasm;
-
Antioxidant supplements—antioxidants, supplements, vitamins, multivitamin, vitamin C, vitamin E, zinc, selenium, beta-carotene, coenzyme Q10, glutathione, N-acetyl cysteine, melatonin, soy isoflavones, green tea;
-
Treatment—chemotherapy, radiation therapy, hormonal therapy;
-
Outcomes—toxicity, oxidative stress, tumor marker, tumor response, recurrence, survival;
-
Study design—observational study, epidemiology, clinical trial.
The search was limited to human studies published in English, French, or German. Relevant references listed in primary-search manuscripts were collected and added to the review. In addition, we searched for review articles published on this topic and added relevant cited references to our review.
We included articles that met the following criteria:
-
Sample: including two or more breast cancer patients;
-
Design: clinical (controlled or uncontrolled) trial or observational study;
-
Exposure: documented use of antioxidant supplements during chemotherapy, radiation therapy, or hormonal therapy;
-
Outcome: toxicity, tumor response, recurrence, or survival in treated breast cancer patients.
The supplements that are most commonly considered to be antioxidants are vitamin C, vitamin E, selenium, and zinc. For the purposes of this review, we also included antioxidant combinations, multivitamins, glutamine, glutathione, melatonin, and soy isoflavones because they are also known to have antioxidant activity. Table 1 summarizes the properties and antioxidant actions of each of the dietary supplements that were eventually included in the review.
We limited our search to articles about antioxidant dietary supplements, that is, tablets, capsules, or powders, as opposed to foods or beverages, containing antioxidants. We excluded articles on antioxidant use during hematopoietic stem cell transplant therapy because this treatment has been proven to be no more effective than other less toxic treatment options and is no longer used in clinical practice [26]. We also excluded articles that reported on the prevalence of antioxidant use without reference to relevant clinical outcomes. Only breast cancer-specific outcomes were included for studies that reported outcomes for multiple tumor sites. Articles that provided outcomes for a mix of tumor sites were excluded if they did not provide results specific to subjects with breast cancer.
Results
Our search yielded 19 articles reporting the results of clinical trials and three articles reporting the results of observational studies that met our criteria for inclusion. The 19 articles from clinical trials represented nine randomized controlled trials, four non-randomized controlled trials, and six single-arm trials. The three observational studies were retrospective cohort studies. These studies were conducted in 13 countries and published in English between 1980 and 2007. Studies included one article on vitamin C [27], six articles on vitamin E [28–33], five articles on antioxidant combinations [34–38], one article on multivitamins [39], two articles on glutamine [40, 41], one article on glutathione [42], three articles on melatonin [43–45], and three articles on soy isoflavones [46–48]. Sample sizes ranged from 2 to 326 subjects. Table 2 summarizes the 22 articles.
We summarize our findings below by grouping studies with outcomes primarily related to (1) treatment toxicities, or (2) tumor response, recurrence, and survival.
Effects of antioxidant supplements on treatment toxicities
Our literature review yielded 13 studies examining the effects of antioxidant supplements on toxicities caused by chemotherapy, radiation therapy, and tamoxifen therapy. Chemotherapy toxicity studies included endpoints related to cardiotoxicity (n = 3), alopecia (n = 2), intestinal permeability (n = 1), oral mucositis (n = 1), and urotoxicity (n = 1). One study examined fatigue during radiation therapy, and four studies examined hot flashes during tamoxifen treatment. The antioxidant supplements in these studies included vitamin E (n = 6), multivitamins (n = 1), glutamine (n = 2), glutathione (n = 1), and soy isoflavones (n = 3).
Vitamin E
Six studies examined the use of vitamin E during breast cancer treatment. Two of the studies examined the use of vitamin E to prevent doxorubicin-induced alopecia, three examined the use of vitamin E to prevent doxorubicin-induced cardiotoxicity, and one study examined the use of vitamin E to treat hot flashes during tamoxifen therapy. The alopecia prevention trials included a non-randomized controlled trial (n = 25; 1,600 IU dl-α-tocopherol per day) [28] and a single-arm trial (n = 17 breast cancer patients, of 20 total patients; 1,600 IU α-tocopherol per day) [29]; neither trial showed any clinically beneficial effect. Similarly, no clinical benefit was suggested by any of the three cardiotoxicity prevention trials (a randomized controlled trial, n = 6 breast cancer patients of 16 total patients, of 1,800 IU dl-α-tocopherol per day; a single-arm trial, n = 21, of 2 g/m2 of α-tocopherol per day; and a non-randomized controlled trial, n = 12, of 200 mg IM tocopherol before chemotherapy) [30–32]. However, a randomized, placebo-controlled trial (n = 120) found that 800 IU per day of vitamin E reduced hot flashes among breast cancer patients, 60% of whom were receiving tamoxifen therapy [33]. The average magnitude of effect was one less hot flash per day (P ≤ 0.05).
Multivitamins
One randomized, placebo-controlled, double-blind cross-over trial (n = 40) examined the effect of supplementation with a Centrum Silver multivitamin during radiation therapy on fatigue [39]. Participants were randomized to take either a multivitamin or placebo when they began their radiation therapy, and were crossed over to the other arm midway through radiation therapy. The trial ended at the end of radiation therapy. At the crossover point, midway through treatment, patients taking the multivitamin reported higher rates of fatigue, compared to those on placebo (25% vs. 0%) (P = 0.035). Data on fatigue at completion of radiation therapy were not reported.
Glutamine
Two randomized, placebo-controlled trials examined the effect of glutamine supplementation on gastrointestinal epithelia during chemotherapy. One trial (n = 326, 2.5 g per day in a swish and swallow solution) found that glutamine reduced the incidence (38.7% vs. 49.7%; P = 0.026) and severity of oral mucositis (1.2% vs. 6.7%; P = 0.005) during anthracycline-based chemotherapy [41]. Another trial (n = 60, 30 g in water per day) found no effects of glutamine on stomatitis and diarrhea during neoadjuvant chemotherapy [40].
Glutathione
One single-arm trial (n = 2 breast cancer patients, of 13 total patients) examined the use of IV glutathione (2.5 g in 100 ml saline before and after cyclophosphamide infusions) to prevent urotoxicity during chemotherapy [42]. No urotoxicity was observed in the two breast cancer patients. The small number of breast cancer patients in this study makes results difficult to interpret.
Soy isoflavones
Three randomized, placebo-controlled trials examined the effect of soy isoflavones on hot flashes in postmenopausal women with a history of breast cancer, some of whom were taking hormonal therapy (tamoxifen or raloxifene) [46–48]. Daily doses used in these three studies varied widely (150 mg of soy isoflavones, n = 177; 90 mg of soy isoflavones, n = 123; 35 mg of soy isoflavones, n = 72). The studies were well designed and none showed an effect of soy intake on the frequency or intensity of hot flashes (all P > 0.05).
Effects of antioxidant supplements on tumor response, recurrence, and survival
Nine studies examined the effects of antioxidant supplements on tumor markers (n = 1), tumor response (n = 2), and recurrence/survival (n = 6). The antioxidant supplements in these studies included vitamin C (n = 1), combination antioxidants (n = 5), and melatonin (n = 3).
Vitamin C
We identified only a single study of vitamin C, a non-randomized controlled trial that examined 5-year survival in women who began 3 g per day of ascorbic acid after surgical resection of primary breast cancer and before 6 weeks of radiation therapy (n = 27) [27]. Women who had similar clinical histories and did not supplement with ascorbic acid were used as the comparison group (n = 25). The duration of treatment with ascorbic acid was not clearly indicated by the report (in different places in the article, overall treatment duration was noted as 9 months and as 5 years). Blood and urine biomarkers collected at regular intervals up to 9 months suggested that women were adherent to vitamin C. The 5-year disease-free survival rates were 48% in ascorbic acid group versus 50% in control group (no statistical tests were reported). The study had significant limitations. The sample size was small; the allocation methods were not described; no information was provided on chemotherapy or hormonal therapy; no adherence information was reported; and no statistical tests were performed to compare the 5-year survival rates.
Combination antioxidants
Five studies examined the effects of antioxidant combinations on recurrence and survival. Lockwood et al. published a single-arm trial (n = 32) on the use of high-dose combination antioxidants and other supplements during routine surgery, chemotherapy, radiation therapy, and tamoxifen therapy for breast cancer treatment [36]. The authors reported partial tumor response in 19% of patients, no signs of recurrence in any patients, and no deaths at 24 months. They did not use a concurrently followed control group or compare the observed outcomes to those that would be expected if patients used only conventional treatment. Based on an incompletely described statistical rationale, the authors reported that they had expected four deaths.
Three studies of megadose vitamins were reported from the practice of Abram Hoffer, MD, an orthomolecular physician. Two papers compared observed survival times of cancer patients who did and did not follow a suggested clinical protocol of mega-dose vitamins [34, 35]. The authors concluded that their data showed better survival for the patients who followed the vitamin protocol than for the control group of patients who did not. However, the appropriateness of this conclusion is unclear given the small control group (five breast cancer patients) and statistical methods. A subsequent well designed study by Lesperance et al. used a retrospective cohort study design with matched controls to examine the effects of Dr. Hoffer’s clinical protocol of megadose vitamins on recurrence and survival in women with unilateral non-metastatic breast cancer [37]. Ninety of Dr. Hoffer’s patients were matched to 180 control women with breast cancer using multiple clinical criteria; all 270 women received conventional cancer care at the same facility. The study results suggested that the group following Dr. Hoffer’s protocol fared worse than the control group, but the differences were not statistically significant (breast cancer-specific mortality hazard ratio: 1.75, 95% CI 0.83–2.69; disease-free mortality hazard radio: 1.55, 95% CI 0.94–2.54). However, the group treated with megadose vitamins was self-selected and may have had a worse prognosis at study entry.
One study examined the effects of combination antioxidants on tumor markers. Premkumar reported the effects of an antioxidant combination (100 mg coenzyme Q10, 10 mg riboflavin, and 50 mg niacin) on tumor markers in breast cancer patients taking tamoxifen therapy (n = 84) [38]. After 3 months, CEA and CA 15-3 (P < 0.05) were lower than at baseline.
Melatonin
A series of three trials by Lissoni et al. examined the use of 20 g per day of melatonin on thrombocytopenia, tumor response, and survival during chemotherapy [43, 44], and on tumor response during tamoxifen therapy [45]. A randomized controlled trial (n = 77) of melatonin supplementation during chemotherapy found that patients on doxorubicin treatment who took melatonin had a better clinical response than those on doxorubicin alone (48% vs. 32%, P < 0.05) (no differences for those on mitoxantrone or paclitaxel) [44]. Patients taking melatonin with doxorubicin or paclitaxel had better survival than those taking doxorubicin or paclitaxel alone (P < 0.05) (no difference for mitoxantrone). This group also reported two other single-arm trials. A single-arm trial (n = 14) of melatonin supplementation during epirubicin treatment showed normalization of platelet function in 9/12 patients (75%) and tumor response in 41% of patients [43]. A phase II single-arm trial (n = 14) in metastatic breast cancer patients taking tamoxifen showed a partial response in 4/14 patients [45].
Discussion
Data on the effects of antioxidant supplements during conventional breast cancer treatment are scarce. Overall, the 22 articles we identified provided insufficient evidence to support conclusions regarding the effects of individual antioxidant supplementation during conventional breast treatment on toxicities, tumor response, recurrence, or survival. However, for several antioxidant supplements, studies suggested possible beneficial, null, or harmful effects and require further investigation. A few studies indicated that specific supplements may decrease side effects associated with treatment, including vitamin E for hot flashes due to hormonal therapy and glutamine for oral mucositis during various chemotherapy regimens. Underpowered trials suggested that melatonin supplementation may enhance tumor response during epirubicin and doxorubicin treatment, and prolong survival after doxorubicin treatment. Trials indicated that vitamin E was not useful in preventing alopecia or cardiotoxicity due to chemotherapy. One study showed that taking multivitamins during radiation treatment increased fatigue. An observational study suggested that megadose supplements did not improve, and may have decreased, 5-year survival rates.
All of the studies suffered from methodological limitations. None of the studies adequately measured both the short- and long-term effects of antioxidant supplementation during breast cancer treatment. Many studies had other limitations including not having a well matched control population, using small sample sizes that lacked sufficient power to make definitive conclusions, including populations heterogeneous in their conventional treatments, and/or not following patients long enough to make conclusions on recurrence and survival rates. Another limitation of the studies presented here is that none accounted for other behaviors or exposures that may alter the effects of antioxidant supplements, such as intake of other dietary supplements, dietary antioxidant intake via fruits and vegetables, host nutritional status, and physical activity patterns.
Caution is nonetheless warranted on the use of antioxidant use during breast cancer treatment. The only large-scale observational study of breast cancer patients using high-dose antioxidants during treatment showed a trend towards decreased survival [37]. No large-scale clinical trials of antioxidants during any form of breast cancer treatment have been conducted with recurrence or survival as the outcome. A recent review of the evidence regarding early and late effects of the use of antioxidants during chemotherapy and radiation therapy for multiple tumor sites concluded that antioxidant supplementation may cause harm during radiation therapy, but may possibly reduce dose-limiting toxicities during chemotherapy [49]. Because breast cancer patients may receive different forms and doses of chemotherapy and radiation therapy than patients with other cancers, these conclusions may not be specifically applicable to breast cancer patients even if they are valid for patients with other cancers. Unfortunately, few of the studies presented long-term survival data. To date, the strongest evidence suggesting the possibility of harm comes from a study of antioxidant supplements during radiation therapy for head and neck cancers. A well designed and well powered randomized, clinical trial examined the use of α-tocopherol supplementation (400 IU/day for 3 years, beginning at the initiation of radiation therapy) during radiation therapy on treatment related side effects and overall survival [50, 51]. The investigators found that the treated patients had both fewer adverse side effects and poorer overall survival than the controls at 8 years. However, head and neck cancer patients differ from breast cancer patients in risk factors, treatment, and prognosis. Hence these study results may or may not be generalizable to breast cancer patients. Finally, no studies have examined the effects of antioxidant supplementation during hormonal therapy on breast cancer survival.
Observational studies now in progress will be better able to address questions on the effects of using antioxidant supplements during breast cancer treatment. A review of NIH-funded studies (http://crisp.cit.nih.gov/) identified two well designed, prospective observational studies currently collecting data on these outcomes and CAM use and lifestyle factors; their results will significantly contribute to the knowledge base in this area. One study (SWOG S0221A-ICSC, PI: Ambrosone) is examining the effects of supplemental antioxidants on treatment outcomes among patients (n = 3,250) in a therapeutic trial of adjuvant doxorubicin, cyclophosphamide and paclitaxel for breast cancer. Another, the Pathways Study (R01CA105274, PI: Kushi), is using rapid case ascertainment to identify women within Kaiser Permanente Northern California who are diagnosed with invasive breast cancer (n = 3,000) [52]. The study will follow women over time to investigate effects of lifestyle and molecular factors, including diet, supplement use, and genetic polymorphisms, in addition to treatment, on long-term outcomes. Women with breast cancer are not using antioxidant supplements in isolation; women who use antioxidants are more likely to use other dietary supplements, other forms of complementary and alternative medicine, and modify their diets and physical activity [53, 54]. Observational studies can collect data on multiple exposures in real-life contexts. If powered sufficiently, these studies can provide us with information on the combined effects of multiple simultaneous exposures.
Well designed clinical trials offer the best opportunities to draw definitive conclusions on single agents or agent combinations because they can control for dose, duration of use, and timing of use. A review of NIH’s clinical trials database (http://www.clinicaltrials.gov) yielded four trials examining the effects of antioxidant supplements specifically during breast cancer treatment on treatment-related toxicities (four trials during chemotherapy, and one trial during tamoxifen therapy). Two trials are examining the effects of antioxidant supplements on chemotherapy-related treatment toxicities; CoQ10 for fatigue during chemotherapy and radiation therapy (phase of trial unspecified, PI: Lesser) and a phase III trial of glutamine for peripheral neuropathy during paclitaxel chemotherapy (PI: Vahdat). A phase II trial is examining the effects of glutathione during doxorubicin and cyclophosphamide treatment on tumor response (PI: Monterea), and another phase II trial is examining the use of soy isoflavones during tamoxifen therapy to alleviate hot flashes (Chair: Fleming).
Currently, the evidence is insufficient to provide clear guidelines on the use of antioxidant supplement during breast cancer treatment, including radiation therapy, chemotherapy, and hormonal therapy. It is important for patients and clinicians to know if antioxidant interventions during conventional breast cancer treatment can decrease dose-limiting toxicities and long-term side effects. If so, supplementation could enable patients to receive higher doses and to be more adherent to treatment. It is also important to know if antioxidant supplementation is beneficial or detrimental to breast cancer recurrence and survival. This review suggests that well designed clinical trials and observational studies are needed to provide this information.
Priority in trial development should be given to agents that show the most promise of either reducing treatment toxicities (e.g., glutamine to reduce oral mucositis) or enhancing treatment effects (e.g., melatonin to enhance tumor response). Trials should follow the standard three-phase sequence and evaluate magnitude of effect, short-term adverse effects, and interactions with conventional treatments. Phase III trials should follow enough study participants long enough to assess effects on recurrence and survival.
The purpose of conducting trials is to determine whether an intervention that is thought to be beneficial really is beneficial. The medical community has repeatedly made mistakes by adopting treatments prior to rigorous evaluation. Trials of antioxidant supplements are needed because many people believe that such supplements are beneficial and are using them in the absence of evidence for benefit or harm. Given the prevalence of such use, the absence of clear evidence for harm justifies trials, but we and others must strive to maintain clinical equipoise and rigor in conducting them.
Meanwhile, in the absence of clear evidence, clinicians should discuss the potential risks and benefits of using antioxidant supplements during treatment with their breast cancer patients.
References
American Cancer Society (2008) Breast cancer facts & figures 2007–2008. Atlanta, American Cancer Society, Inc
Velicer CM, Ulrich CM (2008) Vitamin and mineral supplement use among US adults after cancer diagnosis: a systematic review. J Clin Oncol 26:665–673
Boon HS, Olatunde F, Zick SM (2007) Trends in complementary/alternative medicine use by breast cancer survivors: comparing survey data from 1998 and 2005. BMC Womens Health 7:4
Buettner C, Kroenke CH, Phillips RS et al (2006) Correlates of use of different types of complementary and alternative medicine by breast cancer survivors in the nurses’ health study. Breast Cancer Res Treat 100:219–227
Henderson JW, Donatelle RJ (2004) Complementary and alternative medicine use by women after completion of allopathic treatment for breast cancer. Altern Ther Health Med 10:52–57
Navo MA, Phan J, Vaughan C et al (2004) An assessment of the utilization of complementary and alternative medication in women with gynecologic or breast malignancies. J Clin Oncol 22:671–677
Ashikaga T, Bosompra K, O’Brien P et al (2002) Use of complimentary and alternative medicine by breast cancer patients: prevalence, patterns and communication with physicians. Support Care Cancer 10:542–548
Lengacher CA, Bennett MP, Kip KE et al (2002) Frequency of use of complementary and alternative medicine in women with breast cancer. Oncol Nurs Forum 29:1445–1452
Patterson RE, Neuhouser ML, Hedderson MM et al (2002) Types of alternative medicine used by patients with breast, colon, or prostate cancer: predictors, motives, and costs. J Altern Complement Med 8:477–485
Demark-Wahnefried W, Peterson B, McBride C et al (2000) Current health behaviors and readiness to pursue lifestyle changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer 88:674–684
VandeCreek L, Rogers E, Lester J (1999) Use of alternative therapies among breast cancer outpatients compared with the general population. Altern Ther Health Med 5:71–76
Newman V, Rock CL, Faerber S et al (1998) Dietary supplement use by women at risk for breast cancer recurrence. The Women’s Healthy Eating and Living Study Group. J Am Diet Assoc 98:285–292
Lawenda BD, Kelly KM, Ladas EJ et al (2008) Should supplemental antioxidant administration be avoided during chemotherapy and radiation therapy? J Natl Cancer Inst 100:773–783. doi:10.1093/jnci/djn148
D’Andrea GM (2005) Use of antioxidants during chemotherapy and radiotherapy should be avoided. CA Cancer J Clin 55:319–321
Ladas EJ, Jacobson JS, Kennedy DD et al (2004) Antioxidants and cancer therapy: a systematic review. J Clin Oncol 22:517–528. doi:10.1200/JCO.2004.03.086
Velicer CM, Ulrich CM (2008) Vitamin and mineral supplement use among US adults after cancer diagnosis: a systematic review. J Clin Oncol 26:665–673. doi:10.1200/JCO.2007.13.5905
Weijl NI, Cleton FJ, Osanto S (1997) Free radicals and antioxidants in chemotherapy-induced toxicity. Cancer Treat Rev 23:209–240. doi:10.1016/S0305-7372(97)90012-8
Hellman S (1993) Principles of radiation therapy. In: DeVita VT, Hellman S, Rosenberg SA (eds) Cancer: principles and practice of oncology, 4th edn. J. B. Lippincott Co, Philadelphia
Sangeetha P, Das UN, Koratkar R et al (1990) Increase in free radical generation and lipid peroxidation following chemotherapy in patients with cancer. Free Radic Biol Med 8:15–19. doi:10.1016/0891-5849(90)90139-A
Conklin KA (2000) Dietary antioxidants during cancer chemotherapy: impact on chemotherapeutic effectiveness and development of side effects. Nutr Cancer 37:1–18. doi:10.1207/S15327914NC3701_1
Conklin KA (2004) Cancer chemotherapy and antioxidants. J Nutr 134:S3201–S3204
Borek C (2004) Dietary antioxidants and human cancer. Integr Cancer Ther 3:333–341. doi:10.1177/1534735404270578
Simone CB II, Simone NL, Simone V et al (2007) Antioxidants and other nutrients do not interfere with chemotherapy or radiation therapy and can increase kill and increase survival, part 2. Altern Ther Health Med 13:40–47
Simone CB II, Simone NL, Simone V et al (2007) Antioxidants and other nutrients do not interfere with chemotherapy or radiation therapy and can increase kill and increase survival, part 1. Altern Ther Health Med 13:22–28
Labriola D, Livingston R (1999) Possible interactions between dietary antioxidants and chemotherapy. Oncology (Williston Park) 13:1003–1008 (discussion 1008, 1011-1002)
Moore HC, Green SJ, Gralow JR et al (2007) Intensive dose-dense compared with high-dose adjuvant chemotherapy for high-risk operable breast cancer: Southwest Oncology Group/Intergroup Study 9623. J Clin Oncol 25:1677–1682. doi:10.1200/JCO.2006.08.9383
Poulter JM, White WF, Dickerson JW (1984) Ascorbic acid supplementation and five year survival rates in women with early breast cancer. Acta Vitaminol Enzymol 6:175–182
Martin-Jimenez M, Diaz-Rubio E, Gonzalez Larriba JL et al (1986) Failure of high-dose tocopherol to prevent alopecia induced by doxorubicin. N Engl J Med 315:894–895
Perez JE, Macchiavelli M, Leone BA et al (1986) High-dose alpha-tocopherol as a preventive of doxorubicin-induced alopecia. Cancer Treat Rep 70:1213–1214
Weitzman SA, Lorell B, Carey RW et al (1980) Prospective study of tocopherol prophylaxis for anthracycline cardiac toxicity. Curr Ther Res 28:682–686
Legha SS, Wang YM, Mackay B et al (1982) Clinical and pharmacologic investigation of the effects of alpha-tocopherol on adriamycin cardiotoxicity. Ann N Y Acad Sci 393:411–418. doi:10.1111/j.1749-6632.1982.tb31279.x
Lenzhofer R, Ganzinger U, Rameis H et al (1983) Acute cardiac toxicity in patients after doxorubicin treatment and the effect of combined tocopherol and nifedipine pretreatment. J Cancer Res Clin Oncol 106:143–147. doi:10.1007/BF00395393
Barton DL, Loprinzi CL, Quella SK et al (1998) Prospective evaluation of vitamin E for hot flashes in breast cancer survivors. J Clin Oncol 16:495–500
Hoffer A, Pauling L (1990) Hardin Jones biostatistical analysis of mortality data for cohorts of cancer patients with a large fraction surviving at the termination of the study and a comparison of survival times of cancer patients receiving large regular oral doses of vitamin C and other nutrients with similar patients not receiving these doses. J Orthomol Med 5:143–154
Hoffer A, Pauling L (1993) Hardin Jones biostatistical analysis of mortality data for a second set of cohorts of cancer patients with a large fraction surviving at the termination of the study and a comparison of survival times of cancer patients receiving large regular oral doses of vitamin C and other nutrients with similar patients not receiving these doses. J Orthomol Med 8:157–167
Lockwood K, Moesgaard S, Hanioka T et al (1994) Apparent partial remission of breast cancer in ‘high risk’ patients supplemented with nutritional antioxidants, essential fatty acids and coenzyme Q10. Mol Aspects Med 15:S231–S240. doi:10.1016/0098-2997(94)90033-7
Lesperance ML, Olivotto IA, Forde N et al (2002) Mega-dose vitamins and minerals in the treatment of non-metastatic breast cancer: an historical cohort study. Breast Cancer Res Treat 76:137–143. doi:10.1023/A:1020552501345
Premkumar VG, Yuvaraj S, Vijayasarathy K et al (2007) Effect of coenzyme Q10, riboflavin and niacin on serum CEA and CA 15-3 levels in breast cancer patients undergoing tamoxifen therapy. Biol Pharm Bull 30:367–370. doi:10.1248/bpb.30.367
de Souza Fede AB, Bensi CG, Trufelli DC et al (2007) Multivitamins do not improve radiation therapy-related fatigue: results of a double-blind randomized crossover trial. Am J Clin Oncol 30:432–436. doi:10.1097/COC.0b013e31804b40d9
Li Y, Yu Z, Liu F et al (2006) Oral glutamine ameliorates chemotherapy-induced changes of intestinal permeability and does not interfere with the antitumor effect of chemotherapy in patients with breast cancer: a prospective randomized trial. Tumori 92:396–401
Peterson DE, Jones JB, Petit RGII (2007) Randomized, placebo-controlled trial of Saforis for prevention and treatment of oral mucositis in breast cancer patients receiving anthracycline-based chemotherapy. Cancer 109:322–331. doi:10.1002/cncr.22384
Nobile MT, Vidili MG, Benasso M et al (1989) A preliminary clinical study of cyclophosphamide with reduced glutathione as uroprotector. Tumori 75:257–258
Lissoni P, Tancini G, Paolorossi F et al (1999) Chemoneuroendocrine therapy of metastatic breast cancer with persistent thrombocytopenia with weekly low-dose epirubicin plus melatonin: a phase II study. J Pineal Res 26:169–173. doi:10.1111/j.1600-079X.1999.tb00579.x
Lissoni P, Barni S, Mandala M et al (1999) Decreased toxicity and increased efficacy of cancer chemotherapy using the pineal hormone melatonin in metastatic solid tumour patients with poor clinical status. Eur J Cancer 35:1688–1692. doi:10.1016/S0959-8049(99)00159-8
Lissoni P, Barni S, Meregalli S et al (1995) Modulation of cancer endocrine therapy by melatonin: a phase II study of tamoxifen plus melatonin in metastatic breast cancer patients progressing under tamoxifen alone. Br J Cancer 71:854–856
Quella SK, Loprinzi CL, Barton DL et al (2000) Evaluation of soy phytoestrogens for the treatment of hot flashes in breast cancer survivors: A North Central Cancer Treatment Group Trial. J Clin Oncol 18:1068–1074
Van Patten CL, Olivotto IA, Chambers GK et al (2002) Effect of soy phytoestrogens on hot flashes in postmenopausal women with breast cancer: a randomized, controlled clinical trial. J Clin Oncol 20:1449–1455. doi:10.1200/JCO.20.6.1449
MacGregor CA, Canney PA, Patterson G et al (2005) A randomised double-blind controlled trial of oral soy supplements versus placebo for treatment of menopausal symptoms in patients with early breast cancer. Eur J Cancer 41:708–714. doi:10.1016/j.ejca.2005.01.005
Block KI, Koch AC, Mead MN et al (2008) Impact of antioxidant supplementation on chemotherapeutic toxicity: a systematic review of the evidence from randomized controlled trials. Int J Cancer 123:1227–1239. doi:10.1002/ijc.23754
Bairati I, Meyer F, Gelinas M et al (2005) Randomized trial of antioxidant vitamins to prevent acute adverse effects of radiation therapy in head and neck cancer patients. J Clin Oncol 23:5805–5813. doi:10.1200/JCO.2005.05.514
Bairati I, Meyer F, Gelinas M et al (2005) A randomized trial of antioxidant vitamins to prevent second primary cancers in head and neck cancer patients. J Natl Cancer Inst 97:481–488
Kwan ML, Ambrosone CB, Lee MM et al (2008) The Pathways Study: a prospective study of breast cancer survivorship within Kaiser Permanente Northern California. Cancer Causes Control. doi:10.1007/s10552-008-9170-5
Greenlee H, Kwan ML, Krathwohl SE et al (2008) History of CAM use in a prospective breast cancer cohort study. In: Presented at 4th biennial cancer survivorship research conference, 18–20 June 2008, Atlanta, GA (abstr 1794)
Greenlee H, Gammon MD, Abrahamson PE et al (2007) Use of supplemental antioxidants after breast cancer diagnosis and during breast cancer treatment among women with breast cancer in the Long Island Breast Cancer Study Project. In: Presented at society for integrative oncology 4th international conference, 15–17 November 2007, San Francisco CA (abstr 18157)
Albanes D, Heinonen OP, Huttunen JK et al (1995) Effects of alpha-tocopherol and beta-carotene supplements on cancer incidence in the Alpha-Tocopherol Beta-Carotene Cancer Prevention Study. Am J Clin Nutr 62:1427S–1430S
Omenn GS, Goodman GE, Thornquist MD et al (1996) Risk factors for lung cancer and for intervention effects in CARET, the Beta-Carotene and Retinol Efficacy Trial. J Natl Cancer Inst 88:1550–1559. doi:10.1093/jnci/88.21.1550
van Dalen EC, Caron HN, Dickinson HO et al (2008) Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev 2:CD003917
Savarese DM, Savy G, Vahdat L et al (2003) Prevention of chemotherapy and radiation toxicity with glutamine. Cancer Treat Rev 29:501–513. doi:10.1016/S0305-7372(03)00133-6
Lissoni P (2007) Biochemotherapy with standard chemotherapies plus the pineal hormone melatonin in the treatment of advanced solid neoplasms. Pathol Biol (Paris) 55:201–204. doi:10.1016/j.patbio.2006.12.025
Acknowledgements
This work was supported by NCI Grant R25 CA09406 and the Lance Armstrong Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Greenlee, H., Hershman, D.L. & Jacobson, J.S. Use of antioxidant supplements during breast cancer treatment: a comprehensive review. Breast Cancer Res Treat 115, 437–452 (2009). https://doi.org/10.1007/s10549-008-0193-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-008-0193-0