Abstract
The Breast Cancer Family Registry is a resource for interdisciplinary and translational studies of the genetic epidemiology of breast cancer. This resource is available to researchers worldwide for collaborative studies. Herein, we report the results of testing for germline mutations in BRCA1 and BRCA2. We have tested 4,531 probands for mutations in BRCA1 and 4,084 in BRCA2. Deleterious mutations in BRCA1 and BRCA2 were identified for 9.8% of probands tested [233/4,531 (5.1%) for BRCA1 and 193/4,084 (4.7%) for BRCA2]. Of 1,385 Ashkenazi Jewish women tested for only the three founder mutations, 17.4% carried a deleterious mutation. In total, from the proband and subsequent family testing, 1,360 female mutation carriers (788 in BRCA1, 566 in BRCA2, 6 in both BRCA1 and BRCA2) have been identified. The value of the resource has been greatly enhanced by determining the germline BRCA1 and BRCA2 mutation statuses of nearly 6,000 probands.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Breast Cancer Family Registry (Breast CFR), composed of six international registries and collaborating institutions, was established by the National Cancer Institute (USA) in 1995 to create a resource to facilitate collaborative interdisciplinary and translational studies of the genetic epidemiology of breast cancer [1]. The Breast CFR is available to researchers worldwide for collaborative studies (http://epi.grants.cancer.gov/CFR/). Over 40,000 participants from more than 13,000 families have been enrolled. These include incident breast cancer cases and their relatives ascertained through population-based cancer registries (population-based case families), families with strong cancer histories identified through cancer family clinics and community outreach (clinic-based families), and unaffected women and their relatives sampled from the populations (population-based control families). In addition, there was a specific recruitment of Ashkenazi Jewish women with a personal and/or family history of breast cancer. Population-based families were recruited from the San Francisco Bay area, California (California Breast CFR), the Province of Ontario, Canada (Ontario Breast CFR); and Melbourne and Sydney, Australia (Australian Breast CFR). Clinic-based families were recruited from Philadelphia (Philadelphia Breast CFR), New York City (New York Breast CFR), Utah (Utah Breast CFR), Ontario, Canada (Ontario Breast CFR), and Melbourne and Sydney, Australia (Australian Breast CFR). Specific recruitment of Ashkenazi-Jewish families was conducted by the New York, Philadelphia, Ontario and Australian Breast CFRs. All registries used the Breast CFR’s standardized questionnaires and protocols to collect family history information, epidemiological and clinical data, and biological specimens (blood and/or buccal samples and tumor tissue), with quality control measures throughout the collection, processing, and storing of data and samples. Families are continuing to be followed for new cancer diagnoses and treatment and disease-free survival for breast cancer cases.
Information on the germline BRCA1 and/or BRCA2 mutation status of individuals is needed for many research projects that use the Breast CFR. For example, some studies specifically require mutation carriers only, other studies exclude these carriers as far as is possible, while other studies compare specific characteristics of carriers with those of non-carriers. To facilitate these endeavors, we report the results of a collaborative study through the Breast CFR to identify BRCA1 and BRCA2 mutation carriers.
Materials and methods
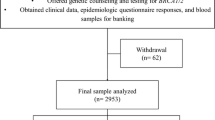
Subjects
Details of the enrollment criteria were previously described in detail [1]. In brief, the enrollment criteria were as follows:
-
(a)
Population-based families The California Breast CFR recruited population-based case probands younger than 65 years at diagnosis through the SEER cancer registry of the Greater San Francisco Bay area. A two-stage sampling scheme was used with an over-sampling based on age at diagnosis and cancer family history. More recently, recruitment has been limited to African-American and Hispanic breast cancer cases. The Ontario Breast CFR recruited population-based case probands diagnosed before the age of 70 years using a two-stage sampling scheme, with over-sampling based on age at diagnosis and cancer family history, through the Ontario Cancer Registry, a voluntary cancer registry that includes 98% of breast cancer cases diagnosed in Ontario. The Australian Breast CFR recruited case probands, stratified by age at diagnosis and unselected for family history, through the Victorian and New South Wales Cancer Registries, for which registration of all cases is mandated by law. Unaffected women were sampled from the population-based sites to be used as population-based control families. The Australian Breast CFR also enrolled family members of control probands. No mutation testing for control probands is described in this paper.
-
(b)
Clinic-based multiple-case families The Philadelphia Breast CFR recruited affected probands with a family history of breast and/or ovarian cancer from the Fox Chase Network of community hospitals, and Cooper Hospital/University Medical Center in Camden New Jersey, and unaffected probands with a family history of breast cancer from the Family Risk Assessment Programs (FRAP) at these institutions. The New York Breast CFR similarly recruited affected and unaffected probands with a family history of breast and/or ovarian cancer from hospitals and through community-based outreach to local organizations and breast cancer support groups. The Utah Breast CFR recruited families with three or more cases of breast or ovarian cancer, especially if at least one of the cancers occurred before the age of 45 years, from local clinicians, the Family Cancer Assessment Clinic at Huntsman Cancer Institute, and another ongoing research study. The Australian Breast CFR recruited affected and unaffected probands with at least two affected relatives through cancer family clinics in Victoria and New South Wales, and through physician referral.
-
(c)
Ashkenazi-Jewish families The New York, Philadelphia, Ontario and Australian Breast CFRs recruited Ashkenazi-Jewish women, predominantly those with a personal or family history of breast cancer, through clinics and the local communities [2].
BRCA1 and BRCA2 mutation testing
Testing for BRCA1 and BRCA2 mutations was not supported as part of the original Breast CFR funding beginning in 1995, and therefore mutation testing was performed through multiple funding sources including NCI (a supplement) using several methodologies. The majority of mutational analyses of BRCA1 and BRCA2 were undertaken by laboratories closely associated with the Breast CFRs and funded from local sources. A validation study was conducted for the methods used between 1997 and 2000, including two-dimensional gel (2-D gel) scanning, denaturing high performance liquid chromatography (DHPLC), enzymatic mutation detection (EMD) and protein truncation tests (PTT) [3]. Specificity and sensitivity of the methods for protein-truncating mutations were comparable to genomic sequencing of all the coding exons in BRCA1 and BRCA2. An additional method EGAN, based on Conformation Specific Gel Electrophoresis (CSGE) [4, 5] has been used for testing of the California samples. EGAN has been validated on a blinded patient set and compared favorably to full sequence analysis results in the same patients (sensitivity of 97.4% in detecting BRCA1 and BRCA2 sequence changes) (A. Miron, pers. comm.).
More recently, a substantial proportion of testing, funded by NIH, has been performed by Myriad Genetic Laboratories, Inc., using full sequence analysis (BRCAnalysis) (this was prior to their introduction of testing for large genomic re-arrangements, deletions, and insertions) [6]. The mutation detection method and number of probands tested at each registry are shown in Table 1, excluding those tested for only the three Ashkenazi Jewish mutations. Women recruited because of their Ashkenazi Jewish heritage were screened for the three founder mutations, 185delAG and 5382insC in BRCA1 and 6174delT in BRCA2, primarily funded through a supplement from the NIH. For the population-based families, the proband was tested. For the clinic-based families, the proband was tested if she was affected with breast cancer, else the youngest breast cancer case in the family from whom a blood sample was available was tested. For the purposes of this report, the affected individual tested will be referred to as the proband. In families in which a deleterious mutation was identified, participating family members for whom we had collected blood were tested when warranted for the same mutation. At the Philadelphia and Utah Breast CFRs, family members were only tested after consenting specifically to genetic testing and counseling. In the Australian Breast CFR, the process for and uptake to the offer of genetic test results has been reported previously [7].
Definition of deleterious mutations
The criteria for defining deleterious mutations were those used by the Breast Information Core (BIC; http://research.nhgri.nih.gov/bic/) and Myriad Genetic Laboratories, Inc. For BRCA1, any frameshift or nonsense mutation that occurs at or before codon 1,853 was classified as deleterious. For BRCA2, any frameshift or nonsense mutation that occurs at or before codon 3,309 was classified as deleterious. Missense changes at the cysteines and the histidine in the ring finger of BRCA1 were considered deleterious, as well as the R1699W and A1708E substitutions [8]. Missense changes at the first methionine for both genes were also classified as deleterious.
Results
Mutation testing results for non-Ashkenazi Jewish probands are shown in Table 1. For families tested for BRCA1, 5.1% (233/4,531) carried deleterious mutations. For families tested for BRCA2, 4.7% (193/4,084) carried deleterious mutations. Three probands were compound heterozygotes carrying deleterious mutations in both BRCA1 and BRCA2. The frequencies of mutations identified from clinic-based families were 9.9% for BRCA1 and 8.6% for BRCA2, and from the population-based families were 4.0% for BRCA1 and 3.7% for BRCA2. Differences across registries may reflect the differences in sampling and extent and type of testing across registries and between population-based and clinic-based sites. Testing of family members in carrier families identified an additional 259 BRCA1 and 242 BRCA2 carriers.
Of the 1,385 Ashkenazi Jewish probands tested for the three founder mutations, 241 (17.4%) carried a mutation (Table 2). Testing of DNA from available family members identified an additional 155 carriers, for a total of 430 female mutation carriers. Three women were found to be compound heterozygotes, carrying both a BRCA1 185delAG and BRCA2 6174delT mutation. These 1,385 probands were not included in Table 1 because they were tested only for the three Ashkenazi Jewish founder mutations.
The total number of female BRCA1 and BRCA2 mutation carriers, including probands and family members, was 1,360 (788 BRCA1, 566 BRCA2, and 6 with both BRCA1 and BRCA2 mutations) (Table 3). Of the total mutation carriers, 313 of the 788 (39.7%) of the BRCA1 carriers, 235 of the 566 (41.5%) BRCA2 carriers and 0 of 6 compound heterozygotes were unaffected with breast cancer at the time of testing. The age distribution of the female carriers by breast cancer status is shown in Table 4. In addition, 169 BRCA1 and 114 BRCA2 male mutation carriers have been identified.
The frequency of mutations was also examined by race/ethnicity, age at diagnosis of the proband, and family history of breast or ovarian cancer. The number of probands tested, defined by racial/ethnic group, is shown in Table 5. The majority of mutation carriers were non-Hispanic white (n = 310), reflecting the demographics of the Breast CFR as a whole. An additional 42 Latino and 31 African–American mutation carriers, as well as 47 carriers from other ethnic groups, have been identified. A detailed family history of breast and other cancers was collected for all families enrolled in the Breast CFR. The vast majority of mutations were identified in probands who had a first-or second-degree relative with breast or ovarian cancer (Table 6). Probands with at least one-first-degree relative diagnosed with breast cancer before age 50 years had the highest frequency of mutations at 12.7% for BRCA1 and 8.2% for BRCA2 (Table 6). For those without a family history of breast cancer, the frequency of mutations identified was 2.4% for BRCA1 and 2.2% for BRCA2. Of the mutations identified, there were 132 and 156 distinct mutations in BRCA1 and BRCA2, respectively.
The frequencies of each type of deleterious mutation were: 54.1% frameshift, 24.8% nonsense, 12.8% intervening sequence (IVS)/splice, and 7.5% missense for BRCA1; and 66.7% frameshift, 23.7% nonsense, 7.7% IVS/splice, 0.6% missense, and 1.3% in-frame insertions/deletions (in-frame indel) for BRCA2 (Fig 1). The 10 most frequently identified BRCA1 and BRCA2 mutations are shown in Fig 2. Reflecting the relatively high proportion of Ashkenazi Jewish families tested, the two Ashkenazi founder mutations were the most commonly found mutations in BRCA1. The distribution of distinct mutation types along the three coding segments of BRCA1 (Exons 1–10; 21.1%, Exon 11; 53.4% and Exons 12–24; 25.6%) and BRCA2 (Exons 1–10; 23.1%, Exon 11; 50.0% and Exons 12–27; 26.9%) were similar between the two genes.
Discussion
Overall, we have found deleterious mutations in approximately 10% of families screened to date for mutations in BRCA1 and BRCA2, with similar percentages for each gene. The frequency of deleterious mutations identified in clinic-based families was two-fold (18.5%) of that identified in the population-based families (9.4%). The higher frequency of mutations may be due to several possibilities. First, based on the nature of the recruitment, the clinic-based families have a stronger family history than the population-based families, and as such have a higher likelihood of carrying mutations. Second, a proportion of the clinic-based families were known to have a deleterious mutation at enrollment. In particular, approximately 41% of families from the Utah Breast CFR carry deleterious mutations, largely due to referral of families from a research study in which mutations had already been identified in the families. The frequency for the population-based families may be higher than for breast cancer cases in general due to the fact that that the three population-based sites of the Breast CFR over-sampled for younger ages at diagnosis, as well as for family history in Ontario and California.
Of the Breast CFR Ashkenazi families screened for only the three founder mutations, 17.9% carried one of the mutations. This is similar to what was observed by Myriad Genetic Laboratories Inc., who found 20.4% of tested individuals of Ashkenazi Jewish ancestry carried deleterious mutations [6]. In the same report, of 10,000 individuals screened for mutations, deleterious mutations were identified for 17.2% of those screened [6]. The frequency of mutations for individuals screened by Myriad Genetic Laboratories Inc. is higher than for our population-based families, likely reflecting that those screened were clinical samples sent for screening because they had a high prior probability of carrying deleterious mutations in BRCA1 and BRCA2.
The distributions of detected BRCA1 and BRCA2 mutations across the genes were similar to what has been reported in the Breast Information Core (BIC) database. For both genes, approximately half the mutations were detected in exon 11 (which constitutes approximately 60% of the coding regions of each gene). The most common type of clinically significant BRCA1 and BRCA2 mutations in the Breast CFR were frameshift mutations (54.9%) followed by nonsense alterations (24.8%). Missense and IVS/splice variants were found less frequently, whereas in-frame mutations were infrequent. For testing performed by cDNA based PTT and 5′ sequencing (as described in [3]), it is possible that some deleterious in-frame deletions that did not cause detectable protein shortening and some missense mutations that were not contained in the 5′ region would have been missed. Furthermore, none of the testing methods used detect large rearrangements/insertions/deletions that have been estimated to account for approximately 12% of mutations in BRCA1 and BRCA2 [9]. We had previously reported that in a population-based sample of multiple-case families from the Australian Breast CFR (n = 66), 2 of 10 BRCA1 mutations were large deletions that involved the promoter region of BRCA1 (large genomic alterations that lie outside the promoter region and BRCA2 were not studied) [10]. Therefore, it is likely that a small proportion of mutations have not yet been identified in these probands. There is an on-going study to test for large insertions/deletions in BRCA1 and BRCA2 in a set of cases selected for family history and breast cancer pathology.
Although the number of unclassified variants (UCVs), including missense and splice variants, identified in the Breast CFR sample is large (data not presented), only a small fraction have so far been shown to be functionally deleterious and thus potentially of clinical significance. Methods to evaluate BRCA1 and BRCA2 UCVs to classify them as deleterious or likely neutral have been published [8, 11–14]. These methods are being applied to the Breast CFR unclassified variants and classifications are being entered into the Breast CFR database.
Nearly 6,000 probands in the Breast CFR were tested for mutations in BRCA1 and BRCA2. More than 1,300 BRCA1 and BRCA2 mutation carriers have been identified in a total of 671 carrier families, including six compound heterozygotes. Mutation testing of probands for families not yet tested, and the application of new mutation testing strategies [e.g., multiplex ligation-dependent probe amplification (MLPA from MRC-Holland) and regulatory region screening) is ongoing. Once mutations are identified in probands, additional family members for whom DNA samples are available, are tested for the family mutation.
To date, the Breast CFR data on BRCA1 and BRCA2 mutation status have been used to estimate the population-based prevalence of BRCA1 mutations [15–18], the investigation of lifestyle factors [19–21]; and genetic factors [22, 23] that might modify the risk of breast cancer for BRCA1 and BRCA2 mutation carriers, and risk of breast and ovarian cancer for relatives of cancer patients with and without BRCA1 or BRCA2 mutations [24].
In conclusion, the value of the Breast CFR resource has been greatly enhanced by the testing for germline BRCA1 and BRCA2 mutations in probands and in many family members of identified carriers. These data, in combination with the family history, epidemiology, pathology, and follow-up data will facilitate studies of penetrance, genotype–phenotype correlations, gene–gene and gene–environment interactions, modifiers of risk in carriers, risks associated with unclassified variants or polymorphisms, and outcomes, as well as studies of characteristics of BRCA1- and BRCA2-associated tumors and assist in the efforts to discover novel breast cancer susceptibility genes. The Breast CFR resource is available to all researchers for collaborative, interdisciplinary, and translational studies of the genetic epidemiology of breast cancer. Detailed information on how to access the resource can be found at the URL: http://epi.grants.cancer.gov/CFR/, as well as citations of publications resulting from use of the Breast CFR. The resource will continue to be strengthened by additional knowledge of BRCA1 and BRCA2 mutation status and continual follow-up of all families.
References
John EM, Hopper JL, Beck JC et al (2004) The Breast Cancer Family Registry: an infrastructure for cooperative multinational, interdisciplinary and translational studies of the genetic epidemiology of breast cancer. Breast Cancer Res 6:R375–R389. doi:10.1186/bcr801
Apicella C, Peacock SJ, Andrews L et al (2006) Determinants of preferences for genetic counselling in Jewish women. Fam Cancer 5:159–167. doi:10.1007/s10689-005-3871-7
Andrulis IL, Anton-Culver H, Beck J et al (2002) Comparison of DNA- and RNA-based methods for detection of truncating BRCA1 mutations. Hum Mutat 20:65–73. doi:10.1002/humu.10097
Ganguly A, Rock MJ, Prockop DJ (1993) Conformation-sensitive gel electrophoresis for rapid detection of single-base differences in double-stranded PCR products and DNA fragments: evidence for solvent-induced bends in DNA heteroduplexes. Proc Natl Acad Sci USA 90:10325–10329. doi:10.1073/pnas.90.21.10325
Korkko J, Annunen S, Pihlajamaa T et al (1998) Conformation sensitive gel electrophoresis for simple and accurate detection of mutations: comparison with denaturing gradient gel electrophoresis and nucleotide sequencing. Proc Natl Acad Sci USA 95:1681–1685. doi:10.1073/pnas.95.4.1681
Frank TS, Deffenbaugh AM, Reid JE et al (2002) Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol 20:1480–1490. doi:10.1200/JCO.20.6.1480
Keogh LA, Southey MC, Maskiell J et al (2004) Uptake of offer to receive genetic information about BRCA1 and BRCA2 mutations in an Australian population-based study. Cancer Epidemiol Biomarkers Prev 13:2258–2263
Goldgar DE, Easton DF, Deffenbaugh AM et al (2004) Integrated evaluation of DNA sequence variants of unknown clinical significance: application to BRCA1 and BRCA2. Am J Hum Genet 75:535–544. doi:10.1086/424388
Walsh T, Casadei S, Coats KH et al (2006) Spectrum of mutations in BRCA1, BRCA2, CHEK2, and TP53 in families at high risk of breast cancer. JAMA 295:1379–1388. doi:10.1001/jama.295.12.1379
Smith LD, Tesoriero AA, Ramus SJ et al (2007) BRCA1 promoter deletions in young women with breast cancer and a strong family history: a population-based study. Eur J Cancer 43:823–827. doi:10.1016/j.ejca.2007.01.011
Tavtigian SV, Deffenbaugh AM, Yin L et al (2006) Comprehensive statistical study of 452 BRCA1 missense substitutions with classification of eight recurrent substitutions as neutral. J Med Genet 43:295–305. doi:10.1136/jmg.2005.033878
Chen X, Truong TT, Weaver J et al (2006) Intronic alterations in BRCA1 and BRCA2: effect on mRNA splicing fidelity and expression. Hum Mutat 27:427–435. doi:10.1002/humu.20319
Abkevich V, Zharkikh A, Deffenbaugh AM et al (2004) Analysis of missense variation in human BRCA1 in the context of interspecific sequence variation. J Med Genet 41:492–507. doi:10.1136/jmg.2003.015867
Easton DF, Deffenbaugh AM, Pruss D et al (2007) A systematic genetic assessment of 1,433 sequence variants of unknown clinical significance in the BRCA1 and BRCA2 breast cancer-predisposition genes. Am J Hum Genet 81:873–883. doi:10.1086/521032
Ozcelik H, Knight JA, Glendon G et al (2003) Individual and family characteristics associated with protein truncating BRCA1 and BRCA2 mutations in an Ontario population based series from the Cooperative Family Registry for Breast Cancer Studies. J Med Genet 40:e91. doi:10.1136/jmg.40.8.e91
Southey MC, Tesoriero AA, Andersen CR et al (1999) BRCA1 mutations and other sequence variants in a population-based sample of Australian women with breast cancer. Br J Cancer 79:34–39. doi:10.1038/sj.bjc.6690008
John EM, Miron A, Gong G et al (2007) Prevalence of pathogenic BRCA1 mutation carriers in 5 US racial/ethnic groups. JAMA 298:2869–2876. doi:10.1001/jama.298.24.2869
Whittemore AS, Gong G, John EM et al (2004) Prevalence of BRCA1 mutation carriers among U.S. non-Hispanic Whites. Cancer Epidemiol Biomarkers Prev 13:2078–2083
Haile RW, Thomas DC, McGuire V et al (2006) BRCA1 and BRCA2 mutation carriers, oral contraceptive use, and breast cancer before age 50. Cancer Epidemiol Biomarkers Prev 15:1863–1870. doi:10.1158/1055-9965.EPI-06-0258
McGuire V, John EM, Felberg A et al (2006) No increased risk of breast cancer associated with alcohol consumption among carriers of BRCA1 and BRCA2 mutations ages <50 years. Cancer Epidemiol Biomarkers Prev 15:1565–1567. doi:10.1158/1055-9965.EPI-06-0323
Breast Cancer Family Registry, Kathleen Cunningham Consortium for Research into Familial Breast Cancer (Australasia), Ontario Cancer Genetics Network (Canada) (2007) Smoking and risk of breast cancer in carriers of mutations in BRCA1 or BRCA2 aged less than 50 years. Breast Cancer Res Treat 109:67–75
Antoniou AC, Sinilnikova OM, Simard J et al (2007) RAD51 135G→C modifies breast cancer risk among BRCA2 mutation carriers: results from a combined analysis of 19 studies. Am J Hum Genet 81:1186–1200. doi:10.1086/522611
Couch FJ, Sinilnikova O, Vierkant RA et al (2007) AURKA F31I polymorphism and breast cancer risk in BRCA1 and BRCA2 mutation carriers: a consortium of investigators of modifiers of BRCA1/2 study. Cancer Epidemiol Biomarkers Prev 16:1416–1421. doi:10.1158/1055-9965.EPI-07-0129
Lee JS, John EM, McGuire V et al (2006) Breast and ovarian cancer in relatives of cancer patients, with and without BRCA mutations. Cancer Epidemiol Biomarkers Prev 15:359–363. doi:10.1158/1055-9965.EPI-05-0687
Acknowledgments
This work was supported by the National Cancer Institute, National Institutes of Health under RFA # CA-95-011 and through cooperative agreements with members of the Breast Cancer Family Registry and Principal Investigators, including Cancer Care Ontario (U01 CA69467), Columbia University (U01 CA69398), Fox Chase Cancer Center (U01 CA69631), Huntsman Cancer Institute (U01 CA69446), Huntsman Cancer Institute (U01 CA69446), Northern California Cancer Center (U01 CA69417), University of Melbourne (U01 CA69638), and Research Triangle Institute Informatics Support Center (RFP No. N02PC45022-46). Mutation testing in Australia was supported by grants from the National Health and Medical Research Council (NHMRC) and the Victorian Breast Cancer Research Consortium (VBCRC). Mutation testing at Fox Chase Cancer Center was in part supported by an Ovarian Cancer SPORE grant (P50 CA83638). Mutation testing in Ontario was supported in part by Cancer Care Ontario. We wish to thank members of the Ontario Cancer Genetics Network for their contributions to the study. MCS is a Senior Research Fellow of the NHMRC and JLH is an Australia Fellow and a VBCRC Group Leader. The content of this manuscript does not necessarily reflect the views or policies of the National Cancer Institute or any of the collaborating centers in the Breast CFR, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government or the Breast CFR.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Neuhausen, S.L., Ozcelik, H., Southey, M.C. et al. BRCA1 and BRCA2 mutation carriers in the Breast Cancer Family Registry: an open resource for collaborative research. Breast Cancer Res Treat 116, 379–386 (2009). https://doi.org/10.1007/s10549-008-0153-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-008-0153-8