Abstract
Purpose To characterize diarrhea events in patients with cancer treated with lapatinib as monotherapy or in combination with capecitabine or taxanes. Patients and methods Eleven clinical trials (phase I, II, or III) in patients with metastatic cancer were analyzed. Lapatinib was administered at doses ranging from 1,000 to 1,500 mg/day as monotherapy (n = 926) or in combination with capecitabine (n = 198) or taxanes (n = 687). Diarrhea events were characterized based on severity, time to onset, duration, required interventions, and clinical outcomes. Results In the pooled analysis of nine studies, diarrhea occurred in 55% of lapatinib-treated patients and 24% of patients not receiving lapatinib. All grade diarrhea occurred in 51% of patients treated with lapatinib monotherapy and 65% treated with lapatinib plus capecitabine. In a separate analysis, 48% of patients treated with lapatinib plus a taxane experienced diarrhea. Overall, most diarrhea events were grade 1/2. Grade 3 events occurred in <10% of patients and grade 4 events were rare (≤1%). Most diarrhea events resolved with conventional approaches and without dose modification. Approximately 40% of patients treated with lapatinib monotherapy or combination therapy experienced a first diarrhea event within 6 days of treatment initiation, with a median duration of 7–9 days. Lapatinib-containing chemotherapy regimens do not cause severe diarrhea when proactive monitoring and intervention is introduced. Conclusion Most diarrhea events in lapatinib-treated patients are low grade, requiring infrequent lapatinib dose modification or interruption. Proactive management of diarrhea is crucial to prevent more serious complications in lapatinib-treated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diarrhea is one of the most common side effects of cancer treatment [1]. Approximately 10% of patients with advanced cancer experience acute or persistent chemotherapy-induced diarrhea, ranging from mild to fatal in severity. Certain chemotherapeutic agents, including fluoropyrimidines and irinotecan, are associated with a significantly higher risk for chemotherapy-induced diarrhea. As many as 80% of patients treated with these agents, either alone or in combination, experience diarrhea, and ≥30% of patients experience serious diarrhea, which can be life-threatening [2]. Diarrhea may delay treatment or reduce patient compliance with oral medications, thus reducing the efficacy of anticancer therapy. The management of diarrhea events also increases the cost of cancer treatment [3, 4]. Consequently, early recognition and timely implementation of appropriate intervention strategies are crucial for the successful control of chemotherapy-induced diarrhea in patients with cancer [5, 6].
Lapatinib (Tykerb®/Tyverb®; GlaxoSmithKline, Philadelphia, PA) is an oral, dual tyrosine kinase inhibitor targeting both EGFR (ErbB1) and HER2 (ErbB2) receptors. Lapatinib is approved in the United States, Switzerland, Australia, and several other international markets for the treatment of advanced or metastatic breast cancer in patients with HER2-positive tumors who have progressed on treatment regimens containing an anthracycline, a taxane, and trastuzumab [7]. Lapatinib is clinically active as a single agent or in combination with various chemotherapy agents in patients with HER2-positive breast cancer and other solid tumors [8–11].
Commonly reported side effects of lapatinib in clinical trials include diarrhea, rash, nausea, and vomiting. Diarrhea was the most frequently reported adverse event in phase I studies of lapatinib-treated patients with advanced or metastatic solid tumors [12]. In addition, diarrhea occurred more frequently in patients with breast cancer who were treated with lapatinib in combination with capecitabine compared with capecitabine alone [9]. Gastrointestinal toxicity is a known side effect of EGFR receptor inhibition; hence, diarrhea events are expected in lapatinib-treated patients. Diarrhea may affect patients’ well-being, the likelihood of continuing therapy, and treatment outcomes more than other side effects of lapatinib.
This article reviews only diarrhea-related safety and tolerability data from 11 clinical studies; patients with breast cancers or other solid tumors were administered lapatinib either as monotherapy (seven studies) or in combination with paclitaxel, docetaxel, or capecitabine (four studies).
Patients and methods
Lapatinib clinical studies
To characterize diarrhea events, two analyses were performed on 11 completed lapatinib clinical studies in patients with locally advanced or metastatic cancer (Table 1). Five studies enrolled patients with breast cancer, and six studies enrolled patients with other solid tumors. Lapatinib was administered as monotherapy in seven studies and as combination therapy with paclitaxel in two studies, docetaxel in one study, and capecitabine in one study. Lapatinib was administered as a once-daily oral medication at doses ranging from 1,000 to 1,500 mg/day. Paclitaxel was administered intravenously at doses ranging from 80 mg/m2 every week to 135 to 225 mg/m2 every 3 weeks. Docetaxel was administered intravenously at a dose of 50–75 mg/m2 every 3 weeks. Capecitabine was administered as an oral medication at a dose of 2,000–2,500 mg/m2 from day 1 to 14 of a 21-day cycle.
Diarrhea events were characterized in a pooled analysis of nine studies (seven monotherapy studies: EGF20001, EGF20002, EGF20003, EGF20004, EGF20008, EGF20009, and EGF20014; a lapatinib plus paclitaxel study: EGF30001; and a lapatinib plus capecitabine study: EGF100151). An additional analysis of study EGF30001 combined with two additional phase I taxane studies (EGF10009 and EGF10021) was conducted to further assess diarrhea events in patients treated with lapatinib–taxane combination therapy.
Monitoring of diarrhea events
Diarrhea events included the following MedDRA terms: diarrhea, diarrhea hemorrhagic, frequent bowel movements, and loose stools. Diarrhea severity was graded on a scale from 1 to 5 using the National Cancer Institute Common Toxicity Criteria (CTC, versions 2.0 and 3.0; Table 2) [13, 14]. Diarrhea events were assigned possible causality to the study medication by the investigators and were characterized based on severity, time to onset, duration, required interventions (lapatinib dose adjustment, interruption, or discontinuation), and clinical outcomes. Patients’ ages and events associated with diarrhea, including nausea, vomiting, and dehydration, were also reviewed. Patients who were not treated with lapatinib but received paclitaxel, docetaxel, capecitabine, or hormonal therapy in the same studies served as comparators.
Results
Patient population
The pooled analysis of nine completed phase II and III studies included 2,093 patients with locally advanced or metastatic cancer—1,413 patients with breast cancer and 680 with other solid tumors. An additional analysis of patients treated with a combination of lapatinib and taxanes included 687 patients from three studies—two phase I studies, EGF10009 (56 patients) and EGF10021 (52 patients), and a phase III study, EGF30001 (579 patients; Table 1). Patients were treated with lapatinib 1,000–1,500 mg once daily (QD) either as monotherapy (n = 926) or in combination with capecitabine (n = 198), paclitaxel (EGF30001, n = 293; EGF10009, n = 56), or docetaxel (EGF10021; n = 52). Patients who were not exposed to lapatinib but received paclitaxel, docetaxel, capecitabine, hormones, or placebo in the same studies served as comparators (n = 676).
Patient disposition
In the pooled analysis of nine studies, the median age of patients was 55 years (range from 19 to 87 years; Table 3). Elderly (≥70 years) patients accounted for 13% of lapatinib-treated patients and 11% of patients not treated with lapatinib. All patients in the breast cancer studies were female, whereas only 35% of patients in the non-breast cancer studies were female. About 78% of patients were white. A higher percentage of non-white patients participated in breast cancer (2–13%) versus non-breast cancer studies (<3%). Most (96%) patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0–1, and 63% of patients had a Karnofsky performance status score of 90–100 at study entry. In the analysis of lapatinib–taxane combination therapy, the median age of patients was 52 years (range, 19–88 years), 91% of patients were female, and 68% of patients were white.
Diarrhea events
In the pooled analysis (n = 2,093), all grade diarrhea events occurred more frequently in lapatinib-treated patients compared with patients treated with comparator agents (all grades, 55% vs. 24%, respectively; Table 4). Diarrhea events in both the lapatinib and comparator groups were predominantly grade 1/2 in severity. Grade 3 events occurred in 9% of lapatinib-treated patients versus 4% of no lapatinib-treated patients. Grade 4 events occurred in <1% of patients in both treatment groups, and the mean number of diarrhea events per patient was similar in both groups (two events). Almost half (42%) of lapatinib-treated patients had a first diarrhea event within 6 days of treatment initiation, whereas the largest proportion of patients not treated with lapatinib (36%) had a first event after 28 days. Forty-one patients in the lapatinib group and four patients in the comparator group had grade 3/4 diarrhea at first presentation. Diarrhea rarely worsened from grade 1/2 to 3/4 in the lapatinib (13 patients) or comparator (three patients) groups. The median duration in patients treated with lapatinib was 5 days compared to 4 days in patients not treated with lapatinib (Table 5).
The majority of diarrhea events resolved (lapatinib 92%; no lapatinib 96%). Outcomes were similar in breast and non-breast cancer studies. Diarrhea events rarely led to treatment discontinuation (2%), and most diarrhea events did not require dose reductions or interruptions in study drug (lapatinib 85%; no lapatinib 78%). Patients who required intervention responded to standard antidiarrheal medications (e.g., loperamide and diphenoxylate hydrochloride/atropine sulfate) and, in more severe cases, to hydration, octreotide, and antibiotics.
Four percent of patients treated with lapatinib experienced diarrhea as a serious adverse event (SAE; lapatinib 4%; no lapatinib 2%). Most diarrhea SAEs were considered treatment-related (lapatinib, 82%; no lapatinib, 81%). However, most diarrhea SAEs resolved (lapatinib, 97%; no lapatinib, 94%), and there were no fatal lapatinib-related diarrhea SAEs.
Seven percent of elderly patients (≥70 years) treated with lapatinib experienced diarrhea events. Diarrhea events in elderly patients had similar severity, onset, and resolution compared with diarrhea events in patients <70 years, although some minor differences existed. Elderly patients with breast cancer experienced more grade 3 events (33% vs. 19% in patients <70 years), and the median duration of diarrhea events was longer in elderly patients with other solid tumors, including colon and renal cancer (28 days), compared with patients <70-year-old (10 days).
Nausea (12%), vomiting (8%), or nausea and vomiting (4%) occurred within 3 days of onset of diarrhea in lapatinib-treated patients. Nausea and vomiting occurred more frequently in patients treated with lapatinib in combination with paclitaxel or capecitabine. Mucositis was associated with diarrhea in <1% of patients.
Lapatinib monotherapy (n = 926)
Fifty-one percent of patients treated with lapatinib monotherapy experienced diarrhea events (Table 4). Forty-five percent of patients reported grade 1/2 events, 6% of patients reported grade 3 events, and <1% of patients reported grade 4 events. Forty-five percent of patients who received lapatinib monotherapy had a first diarrhea event within 6 days of treatment initiation. The median duration of diarrhea events was similar by grade in lapatinib monotherapy studies (5–6 days; Table 5). Two percent of patients treated with lapatinib monotherapy experienced diarrhea as an SAE. Most (87%) diarrhea events did not require changes to lapatinib treatment. The lapatinib dose was adjusted in 3% of events, treatment was interrupted in 8% of events, and treatment was discontinued in 2% of events. Most diarrhea events resolved with conventional approaches in patients receiving lapatinib monotherapy (89%).
Lapatinib in combination with capecitabine (n = 198)
Diarrhea events were reported in 65% of patients treated with lapatinib in combination with capecitabine (EGF100151; Table 4). Most (89%) diarrhea events were deemed to be treatment-related. The majority of patients experienced grade 1/2 events, grade 3 events occurred in 13% of patients, and grade 4 events occurred in 1% of patients. Forty-one percent of patients had a first diarrhea event within 6 days of treatment initiation, and the median duration of diarrhea events was longer in patients with severe events (8.5 days vs. 4–5 days for mild to moderate events; Table 5). There were no fatal diarrhea events, and diarrhea was reported as an SAE in 7% of patients. Ninety-one percent of events resolved, and 2% of events led to discontinuation of treatment.
In contrast, diarrhea events were reported in 40% of patients treated with capecitabine monotherapy. Grade 1/2 events occurred in 30% of patients, and grade 3 events occurred in 10% of patients. There were no grade 4 events. Diarrhea events in patients treated with capecitabine monotherapy had a median onset of 16 days and a median duration of 6 days. Diarrhea as an SAE was reported in 6% of patients. Most (94%) diarrhea events resolved, and only 3% of events resulted in withdrawal.
Lapatinib in combination with taxanes (n = 687)
Forty-eight percent of patients treated with lapatinib combined with paclitaxel or docetaxel (EGF10009, EGF10021, and EGF30001) experienced diarrhea events (Table 4). Distribution of diarrhea events by grade was similar to that reported for the lapatinib monotherapy studies; most diarrhea events were grade 1/2, and 3 and four events occurred in <10% of patients. Notably, a higher incidence of diarrhea events was reported in the two phase I studies that enrolled patients with refractory tumors, EGF10009 (82%) and EGF10021 (71%). An average of two diarrhea events occurred in patients who received lapatinib–taxane combination therapy. The median time to onset of diarrhea was 8 days; 37% of patients had a diarrhea event within 6 days of treatment initiation and diarrhea events lasted <10 days in 71% of patients. The median duration of diarrhea was similar by grade (3–4 days; Table 5). Four percent of patients treated with lapatinib–taxane combination therapy experienced diarrhea as an SAE; there were no fatal diarrhea SAEs. Overall, 84% of diarrhea AEs were considered treatment-related. Most diarrhea events were managed without recorded medical intervention (Table 6). Diarrhea events rarely led to treatment discontinuation (2%), and almost all events resolved.
Twenty-six percent of patients treated with taxane monotherapy experienced diarrhea events, 81% of which were deemed treatment-related. Grade 1/2 events occurred in 24% of patients, and grade 3 events occurred in 1% of patients. There were no grade 4 events. Diarrhea events in patients treated with taxane monotherapy had a median onset of 22 days and a median duration of 3 days. Diarrhea as an SAE was reported in <1% of patients. Ninety-eight percent of events resolved, and there were no treatment withdrawals.
Management of diarrhea events
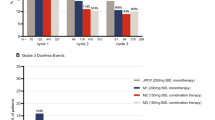
Several SAEs, including death, as a result of septic shock and diarrhea occurred early in the lapatinib–paclitaxel combination study (EGF30001; Fig. 1). However, introduction of supportive measures as outlined in the American Society of Clinical Oncology (ASCO) treatment guidelines for cancer therapy-induced diarrhea (Table 7) [2] significantly decreased the frequency and severity of gastrointestinal complications. As a result, GlaxoSmithKline recommended that diarrhea events that occurred in other lapatinib clinical studies should be managed using the ASCO guidelines. As outlined in these guidelines, most uncomplicated cases of diarrhea (grade 1/2) were treated in an outpatient setting. In addition to dietary modification, lapatinib and cytotoxic chemotherapy were withheld in patients with grade 2 diarrhea until symptoms resolved. High-dose loperamide at an initial dose of 4 mg followed by 2 mg every 4 h was administered until 12 h elapsed without loose motions. In patients who were refractory to loperamide, octreotide therapy was initiated. Oral antibiotics were also added as needed. Patients with more complicated diarrhea (grade 3/4 diarrhea, grade 1/2 diarrhea with complicating features, or progression of grade 1/2 to grade 3/4 diarrhea) were hospitalized and received octreotide, intravenous fluids, and/or antibiotics. If necessary, a brief (up to 14 days) interruption or reduction in the dose of lapatinib or chemotherapy was implemented until symptoms of diarrhea resolved.
Discussion
These analyses of 2,201 patients enrolled in seven lapatinib monotherapy studies and four lapatinib combination studies (three studies with taxanes and one study with capecitabine) demonstrated that lapatinib-induced diarrhea is usually low-grade, self-limiting, and manageable. Severe (grade 3) diarrhea occurs in <10% of patients, and grade 4 diarrhea occurs rarely. Notably, the addition of chemotherapy (either taxanes or capecitabine) does not substantially increase the overall incidence or severity of diarrhea, particularly when proactive management guidelines are in place. Diarrhea generally occurs early in the course of treatment (<1 week) and is usually of limited duration (median of 4–5 days). Most diarrhea events resolve and do not require lapatinib dose reduction, interruption, or discontinuation. Although the elderly (>70 years) patient population was small, the incidence of diarrhea events was comparable to that observed in younger patients and does not represent a particular concern in the elderly.
A small group of patients (10–15%) developed clinically significant diarrhea that was of concern, especially in those receiving concomitant myelosuppressive chemotherapy. Several diarrhea events that culminated in serious consequences, including death, as a result of septic shock, were reported early in a lapatinib–paclitaxel combination study in patients who were experiencing diarrhea and severe myelosuppression [15]. Further experience with lapatinib, a better understanding of the side effect profile of lapatinib, and early introduction of supportive care significantly decreased the frequency and severity of gastrointestinal complications. Consequently, most recent lapatinib clinical studies incorporate proactive diarrhea management, and lapatinib dose adjustments, interruptions, or discontinuations should only be necessary in patients with persistent diarrhea.
The mechanism underlying EGFR-related diarrhea has not been completely elucidated. Several important observations resulted from phase I studies that evaluated the relationship between pharmacokinetic parameters and side effects in patients with metastatic solid tumors who were treated with lapatinib, either as monotherapy or in combination with taxanes and capecitabine [12]. It was shown that the frequency of diarrhea was related to the dose but not the serum concentration of lapatinib, suggesting that lapatinib toxicity evolves from a local effect on the gut epithelium [12]. Pharmacokinetic interactions were reported when lapatinib was combined with paclitaxel [16]. Coadministration of lapatinib and paclitaxel in patients with metastatic solid tumors resulted in an approximately 20% increase in systemic exposure (area under the concentration–time curve) to both drugs [16, 17]. In contrast, lapatinib combined with either docetaxel or capecitabine did not result in detectable pharmacokinetic interactions [15].
Some chemotherapy agents exert cytotoxic effects on the rapidly dividing crypt cells in the intestinal epithelium, which may lead to a relative loss of intestinal-absorptive capacity compared with secretory capacity [18, 19]. Furthermore, cytotoxic destruction or augmentation of enzymes involved in the digestion of proteins and carbohydrates may also alter osmotic gradients in the gut and contribute to decreased reabsorption and increased secretion of fluid and electrolytes in the stool, resulting in diarrhea [20]. The addition of paclitaxel, docetaxel, or capecitabine to lapatinib treatment may increase the incidence of diarrhea events; however, diarrhea events are manageable in patients who receive combination therapy.
Diarrhea is a recognized side effect of EGFR inhibitors [21]. The incidence and severity of diarrhea in lapatinib-treated patients is similar to results reported for other EGFR inhibitors. Diarrhea of any grade was noted in 48% of patients with non-small cell lung cancer (NSCLC) treated with gefitinib 250 mg/day (1% had grade 3/4) [22]. Any grade diarrhea was observed in 54% of patients with NSCLC treated with erlotinib 150 mg; 6% of patients developed severe (grade 3/4) diarrhea [23]. Similar to the current analysis, other EGFR therapies are also associated with higher incidences and severities of diarrhea when administered as combination therapy. Any grade diarrhea was reported in 25% of patients with colorectal cancer treated with cetuximab monotherapy (2% had grade 3/4) [24]. However, 72% of patients treated with cetuximab combination therapy experienced diarrhea (22% had grade 3/4). Similarly, diarrhea developed in 25% of patients with metastatic breast cancer treated with trastuzumab monotherapy and in 45% of patients treated with trastuzumab combined with paclitaxel or anthracyclines [25]. Paclitaxel monotherapy is associated with a diarrhea incidence rate of 38% [26]. In addition, diarrhea developed in 39% of patients treated with docetaxel monotherapy (5% had grade 3/4) [26]. Fifty-seven percent of patients with metastatic breast cancer who received capecitabine monotherapy reported all grade diarrhea (15% had grade 3/4) [27]. The incidence of diarrhea in patients treated with lapatinib–capecitabine combination therapy was similar in the current analysis (65%). Diarrhea has also been reported to occur in placebo-treated patients who participate in clinical studies (all grade, 13–27%; <1% had grade 3/4) [23, 28, 29].
The onset of diarrhea events in lapatinib-treated patients is similar to that reported for other EGFR tyrosine kinase inhibitors. Diarrhea events occurred in gefitinib-treated patients within the first month of therapy, and only 2% of patients discontinued therapy because of diarrhea [22]. Similarly, the median time to onset of diarrhea in erlotinib-treated patients was 12 days and dose reduction and treatment discontinuation occurred in 1% of patients [23].
Consistent with EGFR-related mechanism-based toxicity, most diarrhea events in lapatinib-treated patients were mild to moderate in severity, had an early onset, and were of short duration. The majority of events resolved and did not require lapatinib dose adjustment or treatment interruption. Serious cases of diarrhea occurred rarely; however, these events may pose a clinical problem, especially in patients treated with lapatinib in combination with chemotherapy. Consequently, proactive diarrhea management is strongly recommended when lapatinib is administered in combination with chemotherapy.
References
Arnold RJ, Gabrail N, Raut M et al (2005) Clinical implications of chemotherapy-induced diarrhea in patients with cancer. J Support Oncol 3:227–232
Benson AB III, Ajani JA, Catalano RB et al (2004) Recommended guidelines for the treatment of cancer treatment-induced diarrhea. J Clin Oncol 22:2918–2926
Viele CS (2003) Overview of chemotherapy-induced diarrhea. Semin Oncol Nurs 19:2–5
Wadler S, Benson AB III, Engelking C et al (1998) Recommended guidelines for the treatment of chemotherapy-induced diarrhea. J Clin Oncol 16:3169–3178
Saltz LB (2003) Understanding and managing chemotherapy-induced diarrhea. J Support Oncol 1:35–46. discussion 38–41, 45–46
Sharma R, Tobin P, Clarke SJ (2005) Management of chemotherapy-induced nausea, vomiting, oral mucositis, and diarrhoea. Lancet Oncol 6:93–102
Tykerb [package insert] (2007) GlaxoSmithKline, Research Triangle Park, NC
Gomez HL, Chavez MA, Doval DC et al (2006) Results from a phase II randomized study of lapatinib as first-line treatment for patients with ErbB2-amplified advanced or metastatic breast cancer [abstract]. Breast Cancer Res Treat 100:S68. Abstract 1090
Geyer CE, Forster J, Lindquist D et al (2006) Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med 355:2733–2743
Ravaud A, Gardner J, Hawkins R et al (2006) Efficacy of lapatinib in patients with high tumor EGFR expression: results of a phase III trial in advanced renal cell carcinoma (RCC) [abstract]. J Clin Oncol 24(suppl):217s. Abstract4502
Bourhis J, Harrington K, Rosine D et al (2006) A phase I, open-label study (EGF100262) of lapatinib plus chemoradiation in patients with locally advanced squamous cell carcinoma of the head and neck (SCCHN). Ann Oncol 17:ix180. Abstract 576PD
Burris HA III, Hurwitz HI, Dees EC et al (2005) Phase I safety, pharmacokinetics, and clinical activity study of lapatinib (GW572016), a reversible dual inhibitor of epidermal growth factor receptor tyrosine kinases, in heavily pretreated patients with metastatic carcinomas. J Clin Oncol 23:5305–5313
Cancer Therapy Evaluation Program (2006) Common terminology criteria for adverse events, version 3.0 (CTCAE). Available via http://www.ctep.cancer.gov/forms/CTCAEv3.pdf. Cited November 12, 2007
Cancer Therapy Evaluation Program (1999) Common toxicity criteria, version 2.0. Available via. http://www.ctep.cancer.gov/forms/ctcv2nom-4-30-99-final3.pdf. Cited November 13, 2007
Di Leo A, Gomez H, Aziz Z et al (2007) Lapatinib with paclitaxel compared to paclitaxel as first-line treatment for patients with metastatic breast cancer: a phase III randomized, double-blind study of 580 patients [abstract]. J Clin Oncol 25(suppl):34s. Abstract 1011
Crown JP, Burris HA, Jones S et al (2007) Safety and tolerability of lapatinib in combination with taxanes (T) in patients with breast cancer (BC) [abstract]. J Clin Oncol 25(suppl):38s. Abstract 1027
Jones SF, Burris HA, III, Yardley DA et al (2004) Lapatinib (an oral dual kinase inhibitor) plus weekly or every 3 weeks paclitaxel. Poster presented at the 27th annual San Antonio breast cancer symposium, San Antonio, Texas, 8–11 December 2004. Abstract 1069
Baskerville A, Batter-Hatton D (1977) Intestinal lesions induced experimentally by methotrexate. Br J Exp Pathol 58:663–669
de Roy van Zuidewijn DB, Schillings PH, Wobbes T et al (1992) Morphometric analysis of the effects of antineoplastic drugs on mucosa of normal ileum and ileal anastomoses in rats. Exp Mol Pathol 56:96–107
Wadler S, Haynes H, Wiernik PH (1995) Phase I trial of the somatostatin analog octreotide acetate in the treatment of fluoropyrimidine-induced diarrhea. J Clin Oncol 13:222–226
Forsythe B, Faulkner K (2004) Overview of the tolerability of gefitinib (IRESSA) monotherapy: clinical experience in non-small-cell lung cancer. Drug Saf 27:1081–1092
Iressa [package insert] (2005) AstraZeneca Pharmaceuticals LP, Wilmington, DE
Tarceva [package insert] (2007) OSI Pharmaceuticals, Inc, Melville, NY
Erbitux [package insert] (2007) ImClone Systems Incorporated, Branchburg, NJ
Herceptin [package insert] (2006) Genentech, San Francisco, CA
Tazotere [package insert] (2006) Sanofi-Aventis, Bridgewater, NJ
Xeloda [package insert] (2006) Roche Pharmaceuticals, Nutley, NJ
Nexavar [package insert] (2007) Bayer Pharmaceuticals Corporation, West Haven, CT
Sutent [package insert] (2007) Pfizer Labs, New York
Acknowledgments
The studies described in this analysis were supported by GlaxoSmithKline, Philadelphia, PA. The authors would like to acknowledge all of the patients who participated in this analysis, the teams and investigators who contributed to this analysis, and Shradha Sainju from GlaxoSmithKline. We would also like to thank Jeff Riegel, PhD, and Ann Marie Fitzmaurice, PhD, ProEd Communications, Inc,® for their editorial assistance in preparing this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s10549-008-9971-y
Rights and permissions
About this article
Cite this article
Crown, J.P., Burris, H.A., Boyle, F. et al. Pooled analysis of diarrhea events in patients with cancer treated with lapatinib. Breast Cancer Res Treat 112, 317–325 (2008). https://doi.org/10.1007/s10549-007-9860-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9860-9