Abstract
Invasive lobular carcinoma (ILC) comprises approximately 5–15% of breast cancers and appears to have a distinct biology. As it is less common than invasive ductal carcinoma, few studies of large size have addressed the value of assessment of histologic grade in ILC. Methods: This study is based on a large and well-characterised consecutive series of breast cancer (4,987 cases), from a single institution, with a long-term follow-up to assess the prognostic value of routine assessment of histologic grade in ILC. Histologic grade and other clinicopathological data were available in 517 pure ILC cases. A panel of biomarkers was also available for 215 cases. Results: The majority of ILC was of classical and mixed lobular variants (89%). Most ILC cases were moderately differentiated (grade 2) tumours (76%), while a small proportion of tumours were either grade 1 or 3 tumours (12% each). There were positive associations between histologic grade and other clinicopathological variables of poor prognosis such as larger size, positive lymph node, vascular invasion, oestrogen receptor and androgen receptor negativity and p53 positivity. Multivariate analyses showed that histologic grade is an independent predictor of shorter breast cancer specific survival and disease free interval. Conclusion: Histologic grade of ILC, as assessed by the Nottingham grading system, provides a strong predictor of outcome in patients with invasive lobular carcinoma of the breast and should be provided routinely in pathology reports.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer represents a heterogeneous group of tumours with varied behaviour, and response to therapy. Current routine clinical management of breast cancer relies on availability of robust clinical and pathologic prognostic and predictive factors to support clinical and patient decision-making where potentially suitable treatment options are increasingly available. The three strongest prognostic determinants in operable breast cancer used in routine clinical practice are lymph node (LN) status, primary tumour size and tumour grade. The most widely used grading system of breast cancer is the Nottingham combined histologic grade (Elston-Ellis modification of Scarff-Bloom-Richardson grading system), also known as the Nottingham Grading System [1, 2], which is based on a microscopic evaluation of morphologic and cytologic features of tumour cells, including degree of tubule formation, nuclear pleomorphism, and mitotic count [2]. The sum of these scores stratifies breast tumours into three grades (grade 1; well-differentiated grade 2; moderately differentiated, and grade 3; poorly differentiated).
Multiple studies have shown an independent prognostic significance of grade in breast cancer [3–5] and improved inter-observer agreement with the Nottingham histologic grade compared with other grading systems [6–8]. Histologic grading is one of the components of the Nottingham Prognostic Index (NPI) that has become widely used for the management of patients with breast cancer in the UK [9] and its validity has been confirmed in other independent studies [10–12] and it is now recognised by the UK RCPath [13], European Commission [14] and WHO [15]. In multivariate analysis, histologic grade has equivalent value to that of LN status and it can be combined with lymph node stage and tumour size in the form of a prognostic index (the Nottingham Prognostic Index [NPI] [16] or Kalmar Prognostic Index [KPI] [5]). In addition, the prognostic value of grade has become more important after the introduction of breast cancer screening with the associated reduction in proportion of LN positive cases at diagnosis and consequent need for tools to assist in management of early small size and LN negative tumours [17]. Histologic grade has been endorsed by the College of American Pathologists and the World Health Organization [18, 19]. However, despite this evidence, the latest Breast Task Force of the American Joint Committee on Cancer did not include histologic tumour grade in its staging criteria [20]. One of the reasons for omitting grade in the staging criteria includes use of different grading systems in different studies, reproducibility and the problems associated with grading of special types of cancers including lobular carcinoma [19].
Invasive lobular carcinoma (ILC) is the commonest special type of breast cancer and the second most common overall type of breast cancer, accounting for 5–15% of cases [21–24]. Although some studies have demonstrated the prognostic value of histologic grading in ILC [4, 25–28], there is a perception that it is of limited value. Several studies found no association between ILC grade and patients’ outcome or any prognostic difference between grade 1 and 2 tumours [25, 29]. Therefore, in this study, we performed a retrospective analysis of a large and well-characterised series of breast cancers with long term follow-up comprising clinicopathologic and outcome information. Cases entered into this single institution tumour series have been routinely graded using the Nottingham grading system and treated in a conventional manner. Our aim was to assess the prognostic value of routine application of the Nottingham grading system in ILC and to evaluate the contribution of each grade component.
Methods
The study population was derived from the Nottingham Tenovus Primary Breast Carcinoma Series of women aged 70 years or less, who presented with primary operable invasive breast carcinomas (with tumours of less than 5 cm diameter on clinical/pre-operative measurement and on operative histology) between 1975 and 1999. This is a well-characterised series of patients treated in a single institution and with a long term follow-up. Women aged over 70 years were not included because of the increased confounding factor of death from other causes and because primary treatment protocols for these patients often differed from those for younger women. Similarly, the majority of women with tumours of greater than 5 cm diameter (locally advanced primary tumours) were managed by different protocols. Patient’s clinical history and tumour characteristics including patients’ age, menopausal status, primary tumour size, histologic tumour type [4, 30, 31], histologic grade [2], degree of tubule formation, nuclear pleomorphism and mitosis, lymph node (LN) status, vascular invasion (VI) [32], and Nottingham Prognostic Index (NPI) and oestrogen receptor (ER) status were obtained from the database. Survival data including survival time, disease free interval, and development of distant metastasis (DM), local and regional recurrence was maintained on a prospective basis. Patients were followed up at 3-month intervals initially, then 6-monthly and annually for a median period of 102 months (range 1–344). Breast cancer specific survival (BCSS) was defined as the interval between the operation and death from breast cancer, death being scored as an event, and patients who died from other causes or were still alive were censored at the time of last follow-up. Disease-free interval (DFI) was also calculated from the date of first operation, with first recurrence, local, regional or distant, being scored as an event, and with censoring of other patients at the time of last follow-up or death. Local recurrence was defined as tumour arising in the treated breast or chest wall. Regional recurrence was defined as tumour arising in the axillary or internal mammary LNs.
Tumour grading was assessed, using the Nottingham grading system [2], in a consistent way using uniform methods of specimen fixation, processing, and the same criteria for scoring the different components of grade. In addition, data on several other prognostic biomarkers with close relevance to breast cancer were available on 215 ILC cases from a consecutive cohort of cases from the series that had been prepared as tissue microarrays [33–37]. These markers included progesterone (PgR) and androgen (AR) receptors, EGFR, c-erbB2 (HER2), c-erbB3, c-erbB4, p53, P-cadherin, FHIT protein, neuroendocrine markers (chromogranin-A and synaptophysin), MUC-1 and luminal cytokeratins (CK7/8 and CK19).
Statistical analysis
Statistical analysis was performed using SPSS 15.0 statistical software (SPSS Inc., Chicago, IL, USA). BCSS and DFI curves were drawn using Kaplan–Meier estimates, and were compared using log rank tests. Survival rates are presented with their 95% confidence intervals. Multivariate analyses of DFI and BCSS, with stepwise variable selection, were conducted using Cox proportional hazard regression models. The clinical and biologic characteristics of ILC were compared using contingency tables and χ2 tests. A p-value < 0.05 was considered significant.
Results
Of the whole series (4,987 cases), 544 (10.9%) ILC cases were identified. Cases of mixed ILC and IDC tumour types were not included in the analysis. Of the 544 ILC, 27 cases were associated with synchronous or meta-synchronous invasive duct carcinoma at the time of diagnosis or during the period of follow-up. These cases were excluded from the analysis; only pure operable ILC were considered in this study (517 cases). Table 1 summarizes the clinicopathologic features of ILC cases. The median size was 2 cm (range 0.2–10 cm). ER status was available in 415 cases; of those, 340 (82%) were ER positive. Hormonal therapy was given to 118 patients (22.8%) and chemotherapy to 22 patients (4.3%).
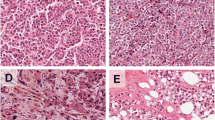
The majority of ILC was of classical subtype (55%) followed by mixed lobular subtypes (34%). Regarding histologic grade, we found that most ILC cases were moderately differentiated (grade 2) tumours (76%), while a small proportion of tumours were either grade 1 or 3 tumours (12% each). Approximately, 10% of cases demonstrated a tubule formation score of two; reflecting the overall percentage of tubulolobular variants of ILC; either pure variant or as a component of lobular mixed subtype. The majority of ILC cases showed a moderate degree of cellular/nuclear pleomorphism (83%) and low mitotic counts (81%).
Association between histologic grade and other clinicopathological variables and patients’ outcome
There was a positive association between histologic grade and larger primary tumour size, LN metastasis, VI, negativity for ER, AR and nuclear BRCA1 and positivity for p53. There was an association between grade and ILC subtypes, development of recurrence, distant metastasis and the number of patients that died from breast cancer (Tables 2 and 3). No association between histologic grade and patients’ age, menopausal status, positive family history or development of regional (LN) recurrences was found.
When the different components of grade were analysed against and the other clinicopathological variables, positive associations were found between high mitotic score and larger tumour size (χ2 = 6.7, P = 0.036), positive VI (χ2 = 17, P = 0.002), ER negativity (χ2 = 8.1, P = 0.018), p53 positivity (χ2 = 21.5, P < 0.001), development of recurrences (χ2 = 20, P < 0.001), and distant metastasis (χ2 = 34, P < 0.001), between lack of tubule formation and larger size (χ2 = 11, P = 0.003) and between marked pleomorphism and larger size (χ2 = 10.7, P = 0.005). There was an association between histologic subtype and mitotic counts (χ2 = 109, P < 0.001, in which mitotic score was higher in solid and mixed variants and low in tubulolobular and classical types), tubule formation (χ2 = 94, P < 0.001) and pleomorphism (χ2 = 40, P < 0.001).
Outcome
Survival analyses showed an association between higher histologic grade and poorer patients’ outcome for both BCSS and DFI (Table 4 and Fig. 1A&B). Multivariate analyses, after adjustment for other prognostic indicators, including LN status (1–3), tumour size, vascular invasion, ER status and adjuvant hormonal treatment were performed to determine whether histologic grade was an independent prognostic factor for BCSS and DFI in patients with ILC. This showed that grade was an independent predictor of survival in ILC (Table 5). In addition, when we analysed the association between NPI, which incorporates grade as one of its three components, an association between NPI and the outcome of patients with ILC (Log Rank (LR) = 85.2, P < 0.001, and LR = 72.1, P < 0.001 for BCSS and DFI respectively) was found.
When individual grade categories were compared, differences in patients’ outcome between grade 1 and 2 and between grade 2 and 3 were found (Table 4). When the three components of histologic grade were analyzed separately, an association between worse outcome and increasing score of each component was found (Table 4). However, the maximum significance was found with mitotic counts where tumours with the highest mitotic counts were associated with the poorest outcome.
Since the majority of ILC lack tubule formation (score 3 for tubule formation), we repeated survival analysis after exclusion of tubule formation from histologic grade (consisting of just pleomorphism (score 1–3) and mitotic counts (score 1–3), to determine whether a simpler scoring system for invasive lobular carcinomas would be as effective. Although we found an association between this grading system and patients’ outcome, multivariate analysis with adjustment of other prognostic variables showed that this new grade was not independent predictor of patients’ outcome. Similar observation was found when we stratified grade 2 tumours into two subgroups (score 6 and 7 of Nottingham histologic grading system).
Discussion
The management of primary breast cancer has changed over the years, and systemic adjuvant therapy is now commonplace. These recent advances in breast cancer treatment have made recognition and characterization of different prognostic and predictive markers mandatory. Histologic grading of breast cancer is a simple, inexpensive and routinely available prognostic factor that has been recognised for a long period of time [2] and validated in multiple independent studies [3, 4, 6–8]. To provide a consistent and uniform way of assessing histologic grade and to improve its reproducibility, consensus criteria have been published [13]. Following these criteria is expected to improve consistency and reproducibility of breast cancer grading among different institutions.
Although the prognostic significance of histologic grade has been thoroughly assessed in ductal carcinoma [2, 38–40], its value in ILC is still controversial and some authorities have been reluctant to grade ILC [41]. This could be explained by several reasons: (i) previous population-based studies that characterised ILC did not analyse grade due to insufficient information on grade as a result of either lack of inclusion of ILC grade or using different grading systems among different institutions [22], (ii) histologically, ILC is characterised by absence of tubule formation, except for the tubulolobular variant, relatively uniform cells and low mitotic counts; all three components of histologic grade [42], (iii) some studies of ILC have reported a limited prognostic value for grading [29].
In the current study, we assessed the prognostic significance of histologic grade in the largest series of ILC to date that has been graded in routine practice using the Nottingham histologic grading system, treated in a single institution and with available long term-term follow-up data. In addition, we investigated the relationship between grade and histologic subtypes and immunophenotype of ILC. Our results demonstrated that histologic grading of ILC is associated with other markers of prognosis and has an independent prognostic value. Differences in outcome were also observed between all three grades of tumour. We also found prognostic significance for all the three components of the grade and in particular for mitotic counts. Our results showed that the prognostic significance of histologic grade is well demonstrated by the Nottingham grading system, which is better than alternative simpler systems such combined pleomorphism and mitosis only (by exclusion of tubule formation) or by splitting grade 2 tumours into two subgroups. Moreover, in this study, we considered that the entity of pleomorphic ILC is a poorly defined entity and a more robust definition needs to be developed and that the results of this study do indicate that high-grade forms of ILC have a more aggressive behaviour.
These results are consistent with previous studies, which showed an independent prognostic significance for histologic grade in breast cancer [2, 4] and in the ILC subtype [25, 43] providing strong evidence for the importance of routine assessment of histologic grade in ILC as well as in invasive ductal carcinoma. We recommend routine assessment of histologic grade of breast cancer using the Nottingham consensus criteria [13–15] to overcome the problems of consistency and reproducibility of histologic grading and to provide the strongest prognostic significance.
References
Bloom HJ, Richardson WW (1957) Histological grading and prognosis in breast cancer; a study of 1409 cases of which 359 have been followed for 15 years. Br J Cancer 11:359–377
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19:403–410
Symmers WC (1998) Assessment of histological grade. systemic pathology. In: Elston CW, Ellis IO (eds) The Breast, vol. 13. Churchill Livingstone, Edinburgh, p 381
Pereira H, Pinder SE, Sibbering DM et al (1995) Pathological prognostic factors in breast cancer. IV: Should you be a typer or a grader? A comparative study of two histological prognostic features in operable breast carcinoma. Histopathology 27:219–226
Sundquist M, Thorstenson S, Brudin L et al (1999) Applying the Nottingham Prognostic Index to a Swedish breast cancer population. South East Swedish Breast Cancer Study Group. Breast Cancer Res Treat 53:1–8
Dalton LW, Page DL, Dupont WD (1994) Histologic grading of breast carcinoma. A reproducibility study. Cancer 73:2765–2770
Frierson HF Jr, Wolber RA, Berean KW et al (1995) Interobserver reproducibility of the Nottingham modification of the Bloom and Richardson histologic grading scheme for infiltrating ductal carcinoma. Am J Clin Pathol 103:195–198
Robbins P, Pinder S, de Klerk N et al (1995) Histological grading of breast carcinomas: a study of interobserver agreement. Hum Pathol 26:873–879
Elston CW, Ellis IO, Pinder SE (1999) Pathological prognostic factors in breast cancer. Crit Rev Oncol Hematol 31:209–223
Balslev I, Axelsson CK, Zedeler K et al (1994) The Nottingham Prognostic Index applied to 9,149 patients from the studies of the Danish Breast Cancer Cooperative Group (DBCG). Breast Cancer Res Treat 32:281–290
D’Eredita G, Giardina C, Martellotta M et al (2001) Prognostic factors in breast cancer: the predictive value of the Nottingham Prognostic Index in patients with a long-term follow-up that were treated in a single institution. Eur J Cancer 37:591–596
Okugawa H, Yamamoto D, Uemura Y et al (2005) Prognostic factors in breast cancer: the value of the Nottingham Prognostic Index for patients treated in a single institution. Surg Today 35:907–911
Third Edition of the NHS Breast Screening Programme’s Guidelines for Pathology Reporting in Breast Cancer Screening and the 2nd edn., of The Royal College of Pathologists’ Minimum Dataset for Breast Cancer Histopathology. Pathology reporting of breast disease. Sheffield, January 2005. NHSBSP Pub. No 58
European Commission (1996) In: de Wolf CJM, Perry NM (eds) European guidelines for quality assurance in mammography screening. Office for Official Publications of the European Communities, Luxembourg
WHO classification of Tumours (2003) In: Tavassoli FA, Devilee P (eds) Pathology and genetics. Tumours of the breast and female genital organs. IARC press, Lyon
Galea MH, Blamey RW, Elston CE et al (1992) The Nottingham Prognostic Index in primary breast cancer. Breast Cancer Res Treat 22:207–219
Hanrahan EO, Valero V, Gonzalez-Angulo AM et al (2006) Prognosis and management of patients with node-negative invasive breast carcinoma that is 1 cm or smaller in size (stage 1; T1a,bN0M0): a review of the literature. J Clin Oncol 24:2113–2122
Tavassoli F, Devilee P (2003) World health organization classification of tumours. In: Kleihues P, Sobin L (eds) Tumours of the breast and female genital organs. IARCPress
Fitzgibbons PL, Page DL, Weaver D et al (2000) Prognostic factors in breast cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 124:966–978
Singletary SE, Allred C, Ashley P et al (2002) Revision of the American Joint Committee on Cancer staging system for breast cancer. J Clin Oncol 20:3628–3636
Sastre-Garau X, Jouve M, Asselain B et al (1996) Infiltrating lobular carcinoma of the breast. Clinicopathologic analysis of 975 cases with reference to data on conservative therapy and metastatic patterns. Cancer 77:113–120
Arpino G, Bardou VJ, Clark GM et al (2004) Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res 6:R149–R156
Martinez V, Azzopardi JG (1979) Invasive lobular carcinoma of the breast: incidence and variants. Histopathology 3:467–488
Borst MJ, Ingold JA (1993) Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery 114:637–641; discussion 641–642
Talman ML, Jensen MB, Rank F (2007) Invasive lobular breast cancer. Prognostic significance of histological malignancy grading. Acta Oncol 46:803–809
Sinn HP, Kellerhoff NM, Kellerhoff R et al (1997) Subtyping and prognostic assessment of invasive lobular breast carcinoma. Pathologe 18:37–44
Moreno-Elola A, Aguilar A, Roman JM et al (1999) Prognostic factors in invasive lobular carcinoma of the breast: a multivariate analysis. A multicentre study after seventeen years of follow-up. Ann Chir Gynaecol 88:252–258
Bane AL, Tjan S, Parkes RK et al (2005) Invasive lobular carcinoma: to grade or not to grade. Mod Pathol 18:621–628
Sinha PS, Bendall S, Bates T (2000) Does routine grading of invasive lobular cancer of the breast have the same prognostic significance as for ductal cancers? Eur J Surg Oncol 26:733–737
Ellis IO, Galea M, Broughton N et al (1992) Pathological prognostic factors in breast cancer. II. Histological type. Relationship with survival in a large study with long-term follow-up. Histopathology 20:479–489
du Toit RS, Locker AP, Ellis IO et al (1989) Invasive lobular carcinomas of the breast—the prognosis of histopathological subtypes. Br J Cancer 60:605–609
Pinder SE, Ellis IO, Galea M et al (1994) Pathological prognostic factors in breast cancer. III. Vascular invasion: relationship with recurrence and survival in a large study with long-term follow-up. Histopathology 24:41–47
Abd El-Rehim DM, Ball G, Pinder SE et al (2005) High-throughput protein expression analysis using tissue microarray technology of a large well-characterised series identifies biologically distinct classes of breast cancer confirming recent cDNA expression analyses. Int J Cancer 116:340–350
Rakha EA, El-Sayed ME, Green AR et al (2007) Prognostic markers in triple-negative breast cancer. Cancer 109:25–32
Rakha EA, Putti TC, Abd El-Rehim DM et al (2006) Morphological and immunophenotypic analysis of breast carcinomas with basal and myoepithelial differentiation. J Pathol 208:495–506
Abd El-Rehim DM, Pinder SE, Paish CE et al (2004) Expression of luminal and basal cytokeratins in human breast carcinoma. J Pathol 203:661–671
Abd El-Rehim DM, Pinder SE, Paish CE et al (2004) Expression and co-expression of the members of the epidermal growth factor receptor (EGFR) family in invasive breast carcinoma. Br J Cancer 91:1532–1542
Schumacher M, Schmoor C, Sauerbrei W et al (1993) The prognostic effect of histological tumor grade in node-negative breast cancer patients. Breast Cancer Res Treat 25:235–245
Davis BW, Gelber RD, Goldhirsch A et al (1986) Prognostic significance of tumor grade in clinical trials of adjuvant therapy for breast cancer with axillary lymph node metastasis. Cancer 58:2662–2670
Page DL (1997) Prognostic indicators in breast cancer and who needs them. Anat Pathol 2:35–52
Roberts MM, Alexander FE, Anderson TJ et al (1990) Edinburgh trial of screening for breast cancer: mortality at 7 years. Lancet 335:241–246
Ladekarl M, Sorensen FB (1993) Prognostic, quantitative histopathologic variables in lobular carcinoma of the breast. Cancer 72:2602–2611
Mokbel K (2001) Grading of infiltrating lobular carcinoma. Eur J Surg Oncol 27:609–610
Conflict of interest statement
None declared. This study was approved by Nottingham Research Ethics Committee 2 under the title of “Development of a molecular genetic classification of breast cancer”.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rakha, E.A., El-Sayed, M.E., Menon, S. et al. Histologic grading is an independent prognostic factor in invasive lobular carcinoma of the breast. Breast Cancer Res Treat 111, 121–127 (2008). https://doi.org/10.1007/s10549-007-9768-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9768-4