Abstract
Objective
To estimate the incidence, prevalence, and economic burden of secondary breast cancer brain metastases (BCBM) among a US-based population of patients with primary breast cancer.
Methods
Female patients diagnosed with secondary BCBM between 1/2002 and 12/2004 and with a brain or head diagnostic test within 30 days of the BCBM diagnosis were identified in a US commercial insurance claims database. A 12-month look-back period was used to identify patients with a breast cancer diagnosis and those with and without a history of BCBM. Patients were required to be continuously enrolled in their health plan for the duration of the study. Incident BCBM patients were matched to a control group of breast cancer patients with no evidence of BCBM. Patient characteristics at baseline, incidence and prevalence rates, and resource utilization and health care costs were determined.
Results
From 2002 to 2004, 779 incident and 995 prevalent BCBM patients and 8,518 primary breast cancer patients were identified. The incidence of BCBM during this time period was 9.1% (95% CI = 8.5%, 9.8%); the prevalence of BCBM was 11.7% (95% CI = 11.0%, 12.4%), with rates increasing from 2002 to 2004. About 22% of incident patients died (based on a proxy measure) during the follow-up period, an average of 158 days (95% CI = 131.1, 183.9) from the index BCBM diagnosis. A 1:1 match of incident BCBM patients to controls resulted in 775 patients in each group. At 6 months follow-up (N = 398), incident BCBM patients had significantly more hospital stays (mean 1.1 vs. 0.5, P < 0.001) and remained hospitalized for a longer period (mean 8.0 days vs. 2.5 days, P < 0.001) compared to controls. Incident BCBM patients also averaged more physician office visits (32.8 vs. 24.3, P < 0.001) as well as pharmacy claims (56.0 vs. 39.1, P < 0.001). Similar differences were found at 12 months (N = 230). Average total costs for incident BCBM patients at 6 months were $60,045 compared to $28,193 for controls (P < 0.001); this difference was driven by higher mean inpatient ($17,462 vs. $5,362, P < 0.001) and outpatient ($26,209 vs. $11,652, P < 0.001) costs among incident BCBM patients. At 12 months, higher mean total costs persisted in incident BCBM patients ($99,899 vs. $47,719, P < 0.001). After adjusting for key variables, mean costs for these patients were 123% higher than those for control group patients.
Conclusions
Secondary BCBM is a common occurrence among breast cancer patients, with rates increasing over time. Breast cancer patients with secondary BCBM incurred significantly more health care resources following diagnosis compared to those with breast cancer but no BCBM. Mean total costs for BCBM patients were more than double those of patients without BCBM at 6 and 12 months. The increasing prevalence and economic burden associated with BCBM suggests an unmet need that could be filled with newer treatments that improve breast cancer outcomes, including the prevention or delay of BCBM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization estimates that breast cancer is newly diagnosed in more than 1.1 million women annually, which represents approximately 10% of all new cancer cases [1]. Among women in the United States (US), breast cancer is the most commonly diagnosed non-cutaneous cancer, with an estimated 213,000 new cases in 2006 [2]. It is also the second most fatal oncologic disorder after lung cancer. The National Cancer Institute (NCI) estimates that in the US, almost 41,000 women will die from breast cancer in 2006 [2].
According to the SEER program registry, about 6% of newly diagnosed breast cancer between 1996 and 2003 were metastatic or in advanced stage, and the 5-year relative survival rate was approximately 26% [2]. Median survival for patients with metastatic breast cancer (MBC) has been reported to be between 18 and 24 months. Often times, the cancer cells cannot be detected clinically or radiologically in their earliest stages; about 50% of patients who receive surgery, radiation, or systemic therapy for localized disease develop signs and symptoms of advanced breast cancer 3–5 years following treatment, and these signs and symptoms depend on the site of metastasis. Bone soreness and pain (bone metastases), persistent cough and shortness of breath (lung metastases), weight loss (liver metastases), and severe headache and seizures (brain metastases) are typical symptoms; however, some patients may present as asymptomatic [2].
Breast cancer brain metastasis (BCBM) is the most common intracranial tumor in adults, and is 10 times more common than primary brain tumors [3]. The exact incidence and prevalence of brain metastasis are unknown, but reports suggest an increasing yearly incidence, with estimates of 170,000 cancer patients developing brain metastasis in the US each year [4]. Although brain metastasis most commonly arises from primary tumors of the lung (50–60%), the second most common primary tumor site is the breast (15–20%) [5]. The incidence of clinically apparent BCBM in patients with breast cancer is 10–20% [6]. Barnholtz-Sloan et al. [7] estimated a 5.1% incidence proportion of BCBM among patients with primary breast cancer using a population based cancer surveillance system. The increasing frequency and rising incidence of brain metastasis may be due to several factors, including advances in neuroimaging, routine staging tests, and possibly the sanctuary effect provided by the blood-brain barrier, which may isolate the brain tissue from the antitumor effects of systemic chemotherapy [8]. The most frequent symptoms associated with brain metastasis include headaches, cognitive changes, focal weakness, and seizures; less common symptoms include gait difficulty, visual loss, speech abnormalities, and sensory loss [5]. The often disabling effects of these symptoms are likely to extract a significant personal (quality of life) and societal toll.
Although research continues to be conducted to expand treatment choices and improve outcomes for MBC patients with BCBM, an appreciation of the unmet health care need related to this disease is warranted. This study was conducted to evaluate the epidemiology and assess the economic burden associated with BCBM among women with primary breast cancer.
Materials and methods
Data source
Data were obtained from the PharMetrics Patient-Centric Database, which is comprised of fully adjudicated health care and pharmaceutical claims for over 50 million unique patients in 88 health plans across the US. The database includes inpatient and outpatient diagnoses (in ICD-9-CM format) and procedures (in CPT-4 and HCPCS formats), as well as both retail and mail order prescription records. Additional data elements include demographic variables, product and payer type, provider specialty, paid and charged amounts, and start and stop dates for plan enrollment.
Study population
For the incident and prevalent cohorts, patients with BCBM between 1/2002 and 12/2004 were identified, defined as those with a diagnostic encounter code for any secondary BCBM (ICD-9 code 198.3) and at least one of eight procedure codes for a brain or head diagnostic test (70450–70470, 70551–70553, 78607–78608) within 30 days before or after the BCBM diagnosis. The date of the first diagnosis of BCBM during the 3-year identification period served as the index date. A 12-month look-back period from the index date was used to identify patients with at least one diagnosis of primary breast cancer (ICD-9 codes 174.x, 233.0); for incident BCBM patients, this 12-month look-back period also was used to identify only those patients with no diagnostic history of BCBM.
The incident and prevalent cohort populations were stratified by patients with BCBM only versus those with additional metastasis to other body systems (ICD-9 codes 196.x, 197.x, 198.x [except 198.3]) at any point during the entire study time period. In addition, the incident cohort was stratified by incident versus prevalent breast cancer; incident breast cancer was defined as those patients having a period of at least 12 months prior to a primary breast cancer diagnosis with no evidence of additional breast cancer diagnoses.
A control population was created for statistical comparisons related to resource utilization and direct health care costs and included patients with a primary diagnosis of breast cancer identified during the same time period between 1/2002 and 12/2004. Patients in the control population could not have any diagnosis of BCBM during the 12-month look-back period or at any time during the follow-up period. The control group population was stratified by patients with incident versus prevalent breast cancer.
Patients were excluded from the study if they were male; less than 18 years of age, or 65 years of age or older and not in a Medicare Advantage plan; or continuously enrolled in their health plan for less than 12 months prior to or 1 month following the index diagnosis.
For the purposes of assessing resource utilization and direct health care costs, incident BCBM cases and control patients initially were matched based on the length of follow-up eligibility (6, 12, 18, 24 months). Next, incident cohort and control patients within each of the four time periods were matched randomly (1:1 ratio) by propensity score methodology on the basis of 5-year age groups, geographic region, comorbidity index scores (Dartmouth-Manitoba adaptation of the Charlson comorbidity index), and other metastatic cancer diagnoses (yes versus no). Incident BCBM patients were matched only at the aggregate level; therefore, analyses of incident BCBM patients and control patients by any of the stratifications were performed at an unmatched level.
Study measures and data analysis
Measures of interest included the incidence rate and prevalence rate of BCBM in a commercially-insured population, demographic and clinical characteristics of the study samples, time-to-event analyses for the incident BCBM and incident breast cancer cohorts, as well as health resource utilization and direct health care costs following the incident diagnosis for BCBM.
Patient characteristics for the incident and prevalent cohorts included age (mean age, 10-year age groups), health plan type, payer type, geographic region, comorbidity burden, prior breast cancer treatments during the 12-month pre-index period, total incident breast cancer patients, and death during follow-up. Prior breast cancer treatments were defined as any claim with a primary diagnosis of breast cancer and CPT-4 codes for chemotherapy (96400–96425), radiation therapy (77401–77417, 77520–77525), or surgical treatment (19160, 19162, 19180–19240, 19296–19298, 19340–19342, 38530) on the same claim; NDC and HCPCS codes also were utilized to identify chemotherapy regimens. Patients were assumed to have died, and assigned a mortality flag, if they had evidence of any of the following during the last month in which health care and pharmacy claims were available prior to disenrollment: (1) a cardiac event including resuscitation (CPT-4 92950); (2) defibrillation (CPT-4 92960, 92961); (3) cerebral death (CPT-4 95824); (4) cardiac arrest/failure (ICD-9-CM 427.5x); (5) evidence of injection given to stimulate the heart (J0170, J2000); (6) hospitalization (revenue center codes 100–219); (7) emergency room visit (place of service code 23, CPT-4 99281–99288, revenue center codes 450–459, 981); or (8) ambulance service (CPT-4 99289–99290, revenue center codes 540–549). This methodology has been employed successfully in a 2004 analysis of diabetics and non-diabetics with end-stage renal disease [9]. Univariate statistics on all patient characteristics were reported for each patient cohort.
For incidence and prevalence rate calculations, a cohort of prevalent MBC patients was identified, which included female patients who met all study inclusion and exclusion criteria and who had at least one diagnosis of metastatic disease at any time during the study period under investigation. These patients were used for the denominator in both the incidence and prevalence rate analyses. The diagnosed incidence of BCBM was defined as the total number of breast cancer patients newly diagnosed with BCBM in the 3-year index window divided by the total number of prevalent MBC patients in the 3-year index window. Incident rates were calculated for the aggregate incident cohort over the 3-year index window only. The diagnosed prevalence of BCBM was calculated on a yearly basis (2002, 2003, 2004) and for aggregate time periods of 2 years (2002–2003) and 3 years (2002–2004). For each period of time, the BCBM cases (numerator) included the subset of the eligible population who had a diagnosis of BCBM during the year(s) of interest; the denominator, similar to the incidence rate calculation, included all prevalent MBC patients.
Resource utilization and cost of care were reported for the incident cohort population and the control group population only. Resource utilization and cost were calculated for a minimum of 1 month to a maximum of 24 months following the date of the index event and were reported at time intervals of 6, 12, 18, and 24 months post-index date. Patients were required to be eligible through the time period of interest to be included in the analysis.
Components of resource utilization and health care costs included medications, outpatient care (e.g., emergency-room visits, physician office visits, laboratory diagnostic tests, all other outpatient care), and inpatient care (e.g., hospitalizations). Paid claims were used as a proxy for costs. Costs were expressed in 2006 US dollars and adjusted as necessary using the health care component of the US Consumer Price Index. Data were presented as univariate descriptive statistics and comparisons between the matched incident BCBM cohort and the control group populations were provided using both parametric and non-parametric analyses, where appropriate. A P-value <0.05 was considered statistically significant. A similar cost analysis was executed for patients with incident BCBM only versus those with additional metastases to other body systems at any point during the entire study time period.
A multivariate analysis using a generalized linear model (GLM) also was performed to evaluate total costs for the incident cohort and the corresponding control group after adjusting for pre-index date demographic characteristics (age, geographic region, health plan type, payer type) and clinical characteristics (comorbidity burden and prior breast cancer treatments). Regression analyses were used to take into consideration potential correlations between covariates. Type I and type III P-values were provided; the type I P-values differ from the type III P-values only when evaluating categorical variables, with the type I P-values evaluating each category individually and the type III P-values producing values based on the group as a whole.
A subset of the incident BCBM cohort was created that included all incident breast cancer patients; a second subset consisted of all incident BCBM patients who died. Within the incident breast cancer subset, a Kaplan–Meier model with 95% confidence intervals (CI) was used to estimate the time from the incident breast cancer diagnosis to the first BCBM diagnosis. A second Kaplan–Meier model using the subset of incident BCBM patients who died evaluated the time from the first BCBM diagnosis to death.
All analyses were conducted using Statistical Analysis Software (SAS®), versions 8.2 and 9.1.
Results
Patient population
A total of 13,845 patients with BCBM initially were identified in the PharMetrics Patient-Centric Database from 1/2002 through 12/2004. After applying study entry criteria, 779 incident and 995 prevalent BCBM patients remained in the study sample (Table 1). During the same time period, 164,550 breast cancer patients were identified; 44,043 patients remained in the sample after applying exclusion criteria and were used as the control population. After matching, 755 incident BCBM patients (96.9%) from the original incident cohort were included in this analysis.
Because the propensity matching program uses scores rather than exact values to match cases to controls, there was some variation among patients in the incident BCBM cohort and control population for a number of the demographic and clinical characteristics used in the matching process, including age group, region, and comorbidity index score (P < 0.001) (Table 2). Additionally, several characteristics not used in matching (plan and payer type, death, and all pre-index breast cancer treatments except lymph node dissection) were statistically significantly different between the incident BCBM cohort and the matched control group population.
When the overall incident BCBM cohort was stratified by those patients with BCBM only (N = 75) versus those with multiple metastatic sites (N = 704), BCBM only patients (59.1 years of age) appeared to be slightly older than those patients with multiple metastatic sites (52.8 years of age) (data not shown). The BCBM only cohort also had a greater percentage of patients defined as incident breast cancer (50.0% vs. 36.2%). Conversely, patients with multiple metastatic sites had more comorbid conditions during the pre-index period (mean 6.1 vs. 3.5) and were more likely to die during the follow-up period (23.4% vs. 8.0%) compared to the BCBM only patients.
The average age of the prevalent BCBM study sample was 53.4 years, with about 50% in a health maintenance organization (HMO) plan and two-thirds (78.2%) with a commercial payer. The average Charlson comorbidity index was 6.0, similar to that seen in the incident cohort.
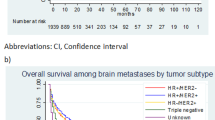
Epidemiology of brain metastases
Using the entire 3-year index window of 1/2002 through 12/2004, the total number of incident BCBM patients identified was 779, and the total prevalent MBC patients was 8,518 (Table 3). This resulted in an incidence rate of 0.09145, or 9.15% (95% CI = 8.53%, 9.76%). Examining prevalence over 1-year timeframes, the rate increased approximately 66% between 2002 and 2004, from a low of 6.61% (95% CI = 5.90%, 7.33%) in 2002 to 10.92% (95% CI = 10.07%, 11.78%) by year 2004. The 3-year (2002–2004) prevalence rate was 11.68% (95% CI = 11.00%, 12.36%), which was approximately 28% higher than the incidence rate. Among a subset of newly diagnosed breast cancer patients (N = 170), the average time from the first breast cancer diagnosis to the first BCBM diagnosis was approximately 4 months (123 days; 95% CI = 106.9, 139.3). The time from the first BCBM diagnosis to death in a subset of incident BCBM patients who died (N = 171) also was calculated. In this population, the average time from diagnosis to death was almost 5 months (158 days; 95% CI = 131.1, 183.9), with a median of 96 days.
Economic burden of brain metastases
Resource utilization and health care costs were reported for incident BCBM patients and matched control patients by 6-month post-index date increments. Because patients had to be eligible for the entire timeframe of interest to be included in the analysis, the patient sample decreased over the 24-month follow-up period, from 398 patients (52.7%) at 6 months to 230 patients (30.5%), 107 patients (14.2%), and 59 patients (7.8%) at 12, 18, and 24 months, respectively. Due to the relatively small sample sizes at 18 and 24 months, our economic analysis focused on 6- and 12-month data.
At 6 months, patients in the incident cohort had a significantly greater number of prescription claims (mean 56.0) compared to the control group (mean 39.1, P < 0.001) (Table 4). Similarly, incident BCBM patients had significantly more physician office visits (mean 32.8 vs. 24.3, P < 0.001), lab diagnostic tests (mean 37.0 vs. 30.2, P = 0.003), and other outpatient services (mean 75.2 vs. 44.3, P < 0.001). Patients in the incident cohort also were more likely to be hospitalized at 6 months (P < 0.001) and to stay longer in the hospital (mean 8.0 days compared to 2.5 days, P < 0.001).
At 12 months, significant differences between incident BCBM and control patients continued to be observed for all services, including emergency room visits (mean 0.5 vs. 0.4, P = 0.023), which was not significant at 6 months. Use of pharmacy services from 6 to 12 months increased by almost 80% among incident BCBM patients; similar increases of more than 75% were seen among these patients for physician office visits and lab diagnostic tests. The increase in services between 6 and 12 months among control patients was smaller, approximately 63% for pharmacy services, and 70% and 58% for physician office visits and lab diagnostic tests, respectively. Conversely, use of other outpatient services grew faster among control patients (82% increase) compared to incident patients (61% increase), although it continued to be significantly higher among BCBM patients (mean 121.2 vs. 80.7, P < 0.001).
At both 6 and 12 months, total mean pharmacy costs, outpatient costs, and inpatient costs were significantly higher for patients in the incident BCBM cohort as compared to the control population (Table 5). At 6 months, overall mean total costs for the incident cohort were $60,045 (median $52,325) as compared to $28,193 (median $18,390) for the control group (P < 0.001). This significant difference in overall costs was driven primarily by the much higher cost among the incident BCBM cohort for inpatient hospitalizations ($17,462 [median $5,763] vs. $5,362 [median $0], P < 0.001) and outpatient services ($26,209 [median $20,593] vs. $11,652 [median $6,875], P < 0.001). Mean prescription costs also were higher for the incident cohort, averaging $16,374 (median $10,205) vs. $11,179 (median $3,266) for the control group (P < 0.001). Within outpatient services, higher costs for other outpatient services ($21,644 [median $14,949] vs. $8,671 [$4,481], P < 0.001) and to a lesser degree, physician office visits ($3,449 [median $2,452] vs. $2,057 [median $1,217], P < 0.001) contributed to the significantly higher costs for total outpatient services among the incident BCBM cohort.
Similar to costs at 6 months, overall total costs were significantly higher among the incident BCBM cohort at 12 months, with mean costs of $99,899 (median $86,098) for BCBM patients compared to $47,719 (median $36,551) for control patients (P < 0.001). Inpatient hospitalizations and outpatient services continued to be the main drivers behind the significant difference in overall costs. Within outpatient services, other outpatient services again was the biggest contributor to the higher overall outpatient costs among the incident BCBM cohort, while costs associated with emergency room visits had a greater impact on overall outpatient costs at 12 months than at 6 months.
The costs of healthcare services over a 12-month time period for the matched subset of incident patients with BCBM only versus those with multiple metastatic sites also were evaluated (data not shown). As expected, patients with multiple metastatic sites had higher overall total mean costs than those patients with BCBM only at 6 months, ($62,937 [median $54,810] vs. $37,354 [median $26,927]) and 12 months ($105,788 [median $90,887] vs. $51,609 [median $30,127]), with the percentage difference in these costs increasing from 68.5% at 6 months to over 104% at 12 months. Mean pharmacy costs and mean inpatient hospitalization costs were higher among patients with multiple metastatic sites at both time periods, as were mean costs for physician office visits, lab diagnostic tests, and other outpatient services.
The results of the GLM evaluating 12-month total healthcare costs for incident BCBM patients and corresponding control patients (N = 230) showed that for every $1.00 increment in cost associated with control patients, incident BCBM patients, on average, were $0.80 more expensive (e.g., $1.80) adjusting for all other factors in the model (P < 0.001) (Table 6). Not surprisingly, those patients with more comorbid conditions during the pre-index period also were slightly more costly (P = 0.017). Conversely, patients aged 45–54 years and 55–64 years were $0.32 and $0.44 less expensive per $1.00 incremental cost, respectively, compared to patients 35–44 years of age (P < 0.05). The factor with the greatest impact on total 12-month costs was Medicare Advantage. Controlling for all of the other factors in the model, patients in Medicare Advantage cost $1.72 less for every $1.00 cost associated with patients in a Commercial plan, which, along with the age group results, suggests more aggressive treatment, and therefore higher costs, in the younger cohort of patients. Overall, after adjusting for all variables in the GLM model, the mean total costs were $99,201 for the incident BCBM patients compared to $44,405 for the corresponding control patients (P < 0.001), a difference of 123% (Table 7). Although these values are lower than the costs in the matched analysis ($99,899 and $47,719), the difference in overall mean total costs between incident BCBM patients and control patients is greater (123% vs. 109%).
Discussion
This study was conducted using a US claims database to examine the characteristics and outcomes associated with metastatic brain disease in a cohort of breast cancer patients. Outcomes of interest included the incidence and prevalence of BCBM as well as demographic and clinical characteristics at baseline, time to first BCBM diagnosis and to death, and resource utilization and health care costs among an incident BCBM cohort.
The incidence of BCBM within the breast cancer population over the 3-year period from 2002 to 2004 was in the range of rates reported in previously published studies. Barnholtz-Sloan et al. [7], in a 2004 study evaluating the incidence proportions of BCBM in patients diagnosed in the Metropolitan Detroit Cancer Surveillance System from 1973 to 2001 found an overall incidence rate from all primary sites of 9.6%; the rate for primary breast cancer was 5.1%. A review by Nathoo et al. [5] estimated that the incidence of metastases to the brain from primary breast cancer was 15–20%. The prevalence rates in our study increased from years 2002 to 2004. This could be attributed to an increase in the median survival of patients with cancer because of modern therapies, increased availability of advanced imaging techniques for early detection, and vigilant surveillance protocols for monitoring recurrence.
The results of the analyses suggest that costs associated with breast cancer patients with incident BCBM are dramatically higher than those for patients with breast cancer and no evidence of BCBM over a 24-month period; this difference in costs was associated with higher utilization of inpatient and pharmacy services as well as non-emergency room outpatient services. Not surprisingly, patients with multiple sites of metastases had much higher costs than patients with BCBM only.
The limitations commonly associated with retrospective analyses of claims databases would apply to this study. The method for selecting patients relied on the use of ICD-9-CM codes for diagnosing breast cancer and BCBM. Because of the absence of health care record reviews, the study may have included some patients without breast cancer or excluded some patients with breast cancer. Additionally, clinicians may not accurately record a comorbid diagnosis at the time of treatment due to the lack of a reimbursement incentive, and therefore, the rates of patients with comorbid conditions may be under or overestimated. This study did not consider indirect costs of lost wages, decrease in work productivity, caregiver time, or emotional or quality of life domains. Additionally, we used managed care reimbursement rates as our measure of cost. While other measures of health care costs might have been considered, our measure has the advantage of representing the total costs to providers covered by one key decision-maker—managed care payers. The database also does not provide information on systemic factors that could affect care, including plan limits on chemotherapy use or complex health care procedures. With the large and diverse nature of the health plans contained in the general database, however, it is likely that these factors were represented in our analysis. Finally, the database does not contain a flag to indicate patient mortality; to determine death in our study, we relied on an algorithm which takes into account serious events that when paired with patient disenrollment, imply a patient has died. However, misrepresentation of patient mortality may have occurred if we mistakenly identified patients as having died or conversely, failed to capture patients who may have died but did not have one of our events of interest prior to disenrollment.
Conclusions
The incidence and prevalence of BCBM among primary breast cancer patients are high and appear to be increasing with time. Breast cancer patients with secondary BCBM also incurred significantly more health care resources following diagnosis compared to those with breast cancer but no BCBM. Mean total costs for BCBM patients were more than double those of patients without BCBM at 6 and 12 months. All these findings suggest that there is an unmet need for newer treatments that improve breast cancer outcomes, including the prevention or delay of metastatic diseases such as BCBM.
References
Anderson BO, Shyyan R, Eniu A et al (2006) Breast cancer in limited-resource countries: an overview of the breast health global initiative 2005 guidelines. Breast J 12(S1):S3–S15
Ries LAG, Harkins D, Krapcho M et al (2006) SEER cancer statistics review, 1975–2003. National Cancer Institute, Bethesda. http://seer.cancer.gov/csr/1975_2003/
Patchell RA (2003) The management of brain metastases. Cancer Treat Rev 29(6):533–540
Posner JB (1992) Management of brain metastases. Rev Neurol (Paris) 148(6–7):477–487
Nathoo N, Toms SA, Barnett GH (2004) Metastases to the brain: current management perspectives. Expert Rev Neurother 4(4):633–640
Yau T, Swanton C, Chua S et al (2006) Incidence, pattern and timing of brain metastases among patients with advanced breast cancer treated with trastuzumab. Acta Oncol 45(2):196–201
Barnholtz-Sloan JS, Sloan AE, Davis FG et al (2004) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the metropolitan detroit cancer surveillance system. J Clin Oncol 22(14):2865–2872
Klos KJ, O’Neill BP (2004) Brain metastases. Neurologist 10(1):31–46
Joyce AT, Iacoviello JI, Nag S et al (2004) End-stage renal disease-associated managed care costs among patients with and without diabetes. Diabetes Care 27(12):2829–2835
Acknowledgments
The authors wish to thank Paula J. Smith, MS for her assistance with the analysis of this study. Funding for this study was provided by GlaxoSmithKline.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pelletier, E.M., Shim, B., Goodman, S. et al. Epidemiology and economic burden of brain metastases among patients with primary breast cancer: results from a US claims data analysis. Breast Cancer Res Treat 108, 297–305 (2008). https://doi.org/10.1007/s10549-007-9601-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9601-0