Abstract
The randomized multicenter study on rapidly proliferating breast cancer, assessed according to thymidine labelling index (TLI), was activated at the end of the 1980s. The present work investigated whether and to what degree the short-term advantages observed from adjuvant CMF (cyclophosphamide, methotrexate, 5-fluorouracil) were maintained at a longer follow-up. Two hundred and eighty-one patients with node-negative and high TLI tumors were randomized to receive six cycles of CMF or no further treatment. At a median follow-up of 12 years, CMF produced a 25% and 20% relative reduction in relapse and death cumulative incidence, respectively. A breakdown analysis identified a subgroup of patients with intermediate proliferating tumors for whom a 70% and 73% reduction in relapse and death was observed in the intention-to-treat population. An even higher reduction of 80% and 84% in relapse and death was seen for the patients who had received the full CMF dose. We identified a subgroup of patients with intermediate proliferating tumors in whom the high benefit obtained from adjuvant CMF was maintained at a long-term follow up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The randomized multicenter study in question was initiated at the end of the 1980s and the novelty was its biological rationale based on patient stratification according to cell proliferation of the primary tumor, evaluated by thymidine labelling index (TLI).
We chose TLI, which has consistently shown to be an indicator of biological and clinical aggressiveness [1–5] and is therefore capable of identifying patients at risk.
It is also a predictor of response to chemotherapy in early and previously untreated tumors [1, 6–8]. We used the regimen cyclophosphamide, methotrexate, 5-fluorouracil (CMF), which was, at that time, considered the most effective drug combination, as adjuvant chemotherapy. Five-year results highlighted a significant improvement in disease-free survival for the CMF group with respect to the control group [6].
In the present study we aimed to investigate whether and to what degree the advantages produced by adjuvant chemotherapy at 5 years were maintained at a longer follow-up in terms of both disease-free and overall survival.
Materials and methods
The multicentre study design, case series, treatment, compliance and statistical methods have previously been reported in detail [6].
Case series
Patients were eligible if they met the following criteria: female ≤70 years of age who underwent radical resection (mastectomy or quadrantectomy plus radiotherapy) for operable invasive breast cancer, with histological and clinical confirmation of no axillary lymph node involvement (at least 10 lymph nodes examined) or distant metastases, and with rapidly proliferating tumors, defined on the basis of thymidine labelling index (TLI).
Patients who had a previous malignancy, bilateral breast cancer, or prior systemic therapy for cancer were excluded from the study.
The protocol was approved by the institutional review boards of each participating centre and informed consent was obtained from each patient.
A total of 281 patients consecutive for available TLI information were entered onto the trial: 138 were allocated to receive post-surgical adjuvant CMF, and 143 locoregional therapy alone. Three patients (1.1%) were found to be ineligible after randomization, two in the control group (one had liver metastases and one bilateral breast carcinoma), and the third patient in the CMF arm (due to abnormal γ-glutamyltransferase value).
Overall, the two arms were well balanced for patient age, menopausal status and type of locoregional treatment. Two-thirds of tumors were <2 cm and about 65% were estrogen receptor-positive.
Biological determinations
TLI was expressed as the ratio between thymidine-labeled cells and total number of tumor cells [9], and was determined independently by two observers scoring 2,000–5,000 cells in multiple fragments of the same tumor. Patients were candidates for the study when the TLI value of the primary tumor was >3% [6].
Estrogen (ER) receptor was assayed by the dextran-coated charcoal method according to the European Organisation for Research and Treatment of Cancer [10]. HER-2 overexpression was evaluated using the CB11 monoclonal antibody (Biogenex, San Ramon, CA), as previously reported [5].
Intra- and interlaboratory quality controls were periodically repeated within the context of a National Quality Control Programme, activated for TLI in the late 1980s [11], and maintained as part of the National Oncology Project promoted by the National Research Council (CNR) and the Ministry of Education, University and Research (MIUR) [12].
Treatment
Within 6 weeks of surgery, patients eligible for the randomized study were allocated to receive either no systemic treatment or six courses of CMF every 4 weeks: cyclophosphamide 100 mg/m2 orally days 1–14, methotrexate 40 mg/m2 intravenously on days 1 and 8, and 5-fluorouracil 600 mg/m2 intravenously on days 1 and 8. Dose modification procedures for hematological and non hematological toxicity were outlined in the trial protocol and described in the previous paper [6]. Permuted block randomization was stratified by center and ER content.
Of the 137 patients randomized to the CMF arm, 30 did not receive the planned full dose because of toxicity or refusal to continue treatment, not because of disease relapse.
Clinical, hematological, and biochemical assessment for each patient was performed as stated in the protocol [6]. Routine follow-up evaluation was carried out, when possible, by an oncologist or by the patient’s general practitioner if the patient no longer attended the participating oncology centre. In the event of disease relapse, treatment was at the discretion of the investigating physician of the participating centers.
Statistical analysis
The cumulative incidences of relapse and death were estimated by Kaplan–Meier curves. Events were defined as the first documented evidence of recurrence in locoregional or distant sites, occurrence of a contralateral tumor, or death. Hazard ratio and 95% confidence intervals (95% CI) unadjusted and adjusted for menopausal status, tumor size and type of surgery were calculated using the Cox proportional-hazard model, stratified according to centre and ER content.
Data were analyzed in the intent-to-treat population, (i.e., all eligible patients evaluated on the basis of their assigned therapy), and in the per-protocol population (i.e., for the control arm, all randomized patients, and for the CMF arm, only patients who had received at least 85% of the planned drug dosage, defined as full CMF dose). Moreover, in accordance with the previous study [6], a breakdown analysis was performed in cell kinetic subgroups identified on the basis of tertile criteria.
All P values were two-sided. No correction for multiple testing was performed in prospectively planned subgroup analysis. Statistical analyses were carried out with SAS Statistical software (SAS/STAT User’s Guide).
Results
No further life-threatening adverse events or deaths from toxicity were registered at 12 years with respect to those observed at 5 years [6], as expected for non anthracycline-containing treatment.
Overall, at a median follow-up of 12 years, 99 relapses have been observed, 55 in the control arm and 44 in the CMF arm. In particular, locoregional relapses and distant metastases decreased by 40% (10 vs.6) and 31% (32 vs. 22), respectively, following adjuvant CMF treatment. The maximum reduction was observed for bone lesions (11 vs. 6) and lung metastases (8 vs. 5).
The incidence of contralateral tumors was similar in the two arms (10 vs. 11), and death without evidence of disease occurred in only five patients in the CMF arm and in three patients in the control arm.
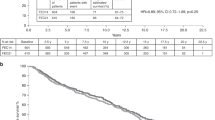
Overall, CMF produced a 25% relative reduction in relapse cumulative incidence with an absolute benefit of 10% at 5 years and 6% at 12 years. Similarly, the cumulative incidence of death was reduced by 20%, with an absolute benefit of only 2% and 4% at 5 and 12 years, respectively (Fig. 1). None of the differences in relapse or death between control and treatment arms reached statistical significance. Similar results were observed when treatment effect was adjusted for menopausal status, tumor size and type of locoregional treatment (HR = 0.72, 95% CI 0.48–1.08, P = 0.11 for relapse cumulative incidence; HR = 0.77, 95% CI 0.45–1.30, P = 0.32 for death cumulative incidence). Conversely, clinical outcome in the per-protocol population showed an important decrease in both relapse (HR = 0.59, 95% CI 0.36–0.95, P = 0.03) and death (HR = 0.57, 95% CI 0.31–1.07, P = 0.08) cumulative incidence in patients who had received the full CMF dose with respect to the control group (Table 1). Such a benefit was attributable to the dosage of the two antimetabolites, 5-FU and methotrexate, whereas it was not influenced by that of cyclophosphamide (data not shown).
A more in-depth analysis was performed as a function of primary tumor TLI (Table 1). No significant differences in either relapse or death cumulative incidence were observed for the lowest and highest TLI tertile subgroups in patients given adjuvant treatment with respect to corresponding control groups. However, in the latter tertile subgroup, 25% of relapses occurred within 20 months in the control arm and within 93 months in the CMF group. In the intermediate TLI tertile subgroup, relapse and death risk were reduced by 70% and 73%, respectively, in the intention-to-treat population and by 80% and 84% in the per-protocol population.
Although the study was not designed to have the power for subgroup comparison, breakdown analysis showed a risk reduction for relapse cumulative incidence of 36% in patients with tumors ≤2 cm and of 51% in pre-menopausal women (Fig. 2). Moreover, a reduction of 31% and 17% was observed in patients with ER-negative and ER-positive tumors, respectively. A risk reduction of 67% in relapse cumulative incidence was seen in patients with tumors overexpressing HER-2. However, confidence intervals were very wide due to the very low number of patients. The benefit in terms of death was somewhat lower than that of relapse in pre-menopausal patients and in those with smaller tumors, whereas it was fully maintained in the subset characterized by ER-negative tumors.
Discussion
Over the past fifty years, breast cancer management has vastly improved thanks to the use of locoregional conservative treatments and ever more effective systemic chemotherapy. The introduction of anthracyclines and taxanes has further contributed to increasing the efficacy of chemotherapy [13–15].
One of the first biological markers investigated was the proliferative activity of the primary tumor, expressed as TLI, which consistently proved to be both a prognostic and predictive indicator of response to the chemotherapy regimens used before the introduction of novel agents [1–8, 16–18].
In the present study, the analysis performed on the clinical outcome of control-arm patients confirmed that the prognostic relevance of the cell kinetic marker, observed for this case series at the 5-year follow-up [6], was still present at 12 years, thereby reinforcing and validating the criterion used for patient selection in the randomized study.
With regard to the rationale of our study, based on experimental and clinical evidence of the direct relationship between cell proliferation and response to anti-tumor drugs, we must conclude that the benefit from adjuvant treatment observed at the 5-year follow-up [6] in the overall series weakens over time. In particular, within the population of patients with rapidly proliferating tumors considered in the present study, a detailed analysis showed no benefit from adjuvant CMF for patients with slower proliferating cancers, a delay in relapse and death for those with more rapidly proliferating cancers, and a significant benefit in terms of both relapse-free and overall survival for patients with intermediate proliferating lesions. Therefore, in the fastest proliferating tumors, drug concentrations reaching the target cells are probably insufficient to control tumor progression. Consequently, these tumors possibly require more intensive treatment.
In line with the increasing tendency to personalise treatment, the present study highlighted a subgroup of patients with intermediate proliferating tumors that are highly sensitive to adjuvant CMF, a relatively inexpensive regimen with an acceptable toxicity profile, especially when the full dose of antimetabolites is administered. This finding further confirms the importance of drug dose [19].
The similar decrease in relapse and death in the subgroup of patients with intermediate proliferating tumors strongly suggests that we have identified a subgroup of patients, which represents 15–20% of the overall population, the majority of whom can be cured by adjuvant CMF. The benefit is far greater than that obtained by adding anthracyclines and/or taxanes to chemotherapy regimens.
Since the inception of the present trial, many other approaches ranging from morpho-pathological parameters, such as grade and tumor size, to last generation molecular markers and microarray studies have been used to define subgroups of patients with node negative disease who are candidates for adjuvant chemotherapy. Notwithstanding interesting results, it should be remembered that very few studies assessing the predictive role of biomarkers have reached level 1 evidence [8]. Consequently, Consensus Conferences on adjuvant therapy for breast cancer take into consideration as risk factors only estrogen receptor status and HER-2 amplification/overexpression, which have entered into routine clinical practice.
We believe that, although TLI determination requires fresh tumor material and is a somewhat complex and time-consuming methodology to define the proliferative rate of tumor cells, its proven importance indicates that it should not have been abandoned.
The results of the present paper can be considered as hypothesis-generating data that now need to be verified and validated in further larger randomized studies investigating the role of a combination of general and specific markers in an adjuvant setting to improve the clinical outcome of breast cancer patients.
References
Silvestrini R, Luisi A, Daidone MG et al (1998) Effect of menstrual phase on cell proliferative rate of breast cancer. Breast Cancer Res Treat 48:93–94
Tubiana M, Pejovic MH, Koscielny S et al (1989) Growth rate, kinetics of tumor cell proliferation and long-term outcome in human breast cancer. Int J Cancer 44:17–22
Meyer JS, Province M (1988) Proliferative index of breast carcinoma by thymidine labeling: prognostic power independent of stage, estrogen and progesterone receptors. Breast Cancer Res Treat 12:191–204
Volpi A, De Paola F, Nanni O et al (2000) Prognostic significance of biologic markers in node-negative breast cancer patients: a prospective study. Breast Cancer Res Treat 63:181–192
Volpi A, Nanni O, De Paola F et al (2003) HER-2 expression and cell proliferation: prognostic markers in patients with node-negative breast cancer. J Clin Oncol 21:2708–2712
Amadori D, Nanni O, Marangolo M et al (2000) Disease-free survival advantage of adjuvant cyclophosphamide, methotrexate, and fluorouracil in patients with node-negative, rapidly proliferating breast cancer: a randomized multicenter study. J Clin Oncol 18:3125–3134
Paradiso A, Schittulli F, Cellamare G et al (2001) Randomized clinical trial of adjuvant fluorouracil, epirubicin, and cyclophosphamide chemotherapy for patients with fast-proliferating, node-negative breast cancer. J Clin Oncol 19:3929–3937
Colozza M, Azambuja E, Cardoso F et al (2005) Proliferative markers as prognostic and predictive tools in early breast cancer: where are we now? Ann Oncol 16:1723–1739
Silvestrini R, Benini E, Daidone MG et al (1993) p53 as an independent prognostic marker in lymph node-negative breast cancer patients. J Natl Cancer Inst 85:965–970
Piffanelli A, Pelizzola D, Giovannini G et al (1989) Characterization of laboratory working standard for quality control of immunometric and radiometric estrogen receptor assays. Clinical evaluation on breast cancer biopsies. Italian Committee for Hormone Receptor Assays Standardization. Tumori 75:550–556
Silvestrini R (1991) Feasibility and reproducibility of the [3H]-thymidine labelling index in breast cancer. The SICCAB Group for Quality Control of Cell Kinetic Determination. Cell Prolif 24:437–445
Paradiso A, Volpe S, Iacobacci A et al (2002) Quality control for biomarker determination in oncology: the experience of the Italian Network for Quality Assessment of Tumor Biomarkers (INQAT). Int J Biol Markers 17:201–214
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trials. Lancet 365:1687–1717
Henderson IC, Berry DA, Demetri GD et al (2003) Improved outcomes from adding sequential Paclitaxel but not from escalating Doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol 21:976–983
Martin M, Pienkowski T, Mackey J et al (2005) Adjuvant docetaxel for node-positive breast cancer. N Engl J Med 352:2302–2313
Amadori D, Volpi A, Maltoni R et al (1997) Cell proliferation as a predictor of response to chemotherapy in metastatic breast cancer: a prospective study. Breast Cancer Res Treat 43:7–14
Gardin G, Alama A, Rosso R et al (1994) Relationship of variations in tumor cell kinetics induced by primary chemotherapy to tumor regression and prognosis in locally advanced breast cancer. Breast Cancer Res Treat 32:311–318
Silvestrini R, Luisi A, Zambetti M et al (2000) Cell proliferation and outcome following doxorubicin plus CMF regimens in node-positive breast cancer. Int J Cancer 87:405–411
Bonadonna G, Valagussa P (1981) Dose-response effect of adjuvant chemotherapy in breast cancer. N Engl J Med 304:10–15
Acknowledgements
The authors thank Gráinne Tierney for editing the manuscript. The following participating investigators and institutions are acknowledged: L. Amaducci, Oncology Unit, Degli Infermi Hospital, Faenza; A. Piancastelli, B. Venturini, and F. Zumaglini, Isitituto Oncologico Romagnolo, Forlì; M. Balzi, Department of Clinical Physiopathology, Careggi University Hospital, Florence, Italy.
Supported by Consiglio Nazionale delle Ricerche (CNR) and Istituto Oncologico Romagnolo (IOR).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amadori, D., Nanni, O., Volpi, A. et al. Phase III randomized multicenter study on the effects of adjuvant CMF in patients with node-negative, rapidly proliferating breast cancer: twelve-year results and retrospective subgroup analysis. Breast Cancer Res Treat 108, 259–264 (2008). https://doi.org/10.1007/s10549-007-9593-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9593-9