Abstract
Background
Despite bisphosphonate treatment, most patients with metastatic breast cancer will have either progressive bone metastases or skeletal related events (SREs). We evaluated the impact of second-line ibandronate on pain control and markers of bone turnover in these patients.
Methods
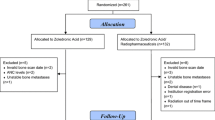
Patients with either an SRE or bony progression while on clodronate or intravenous (IV) pamidronate were switched to oral ibandronate 50 mg daily for 12 weeks. Pain scores and urinary N-telopeptide were evaluated weekly for 4 weeks and at weeks 8 and 12. There was no change in systemic anti-cancer treatment in the month before or after commencing study treatment. Palliative response was defined as a ≥ two-unit reduction in the worst pain score. Patient preferences between IV and oral bisphosphonate therapy were assessed.
Results
Thirty women completed the study. By week 12, patients experienced a significant improvement in pain control (OR = 0.41; P = 0.028) with 12 of 26 (46.2%) evaluable patients achieving a palliative response. Of the 23 patients who had received first-line IV pamidronate, 20 of 23 (87.0%) preferred oral therapy.
Conclusion
Patients with either progressive bone metastases or SREs while on clodronate or pamidronate may experience significant pain palliation with a switch to a more potent bisphosphonate. If confirmed by randomized trials, clinicians can start moving away from the paradigm whereby patients remain on a single bisphosphonate regimen throughout the course of their disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common malignancy in North American women. In 2006 there were an estimated 212,920 new cases and 40,970 deaths [1]. Despite adjuvant treatment, many women will ultimately develop metastatic disease. Affected in 65–75% of women with advanced breast cancer, bone remains the most common site of disease progression. Two-thirds of these women will subsequently develop skeletal-related events (SREs)–that is, pathological vertebral or non-vertebral fractures, spinal cord compression, hypercalcaemia, or surgery or radiation to bone. Even in the absence of SREs, nearly all patients with bone metastases will eventually experience progression [2]. The effective management of bone metastases is therefore essential for improving quality and quantity of life in these patients.
Management has been revolutionized by the use of bisphosphonates. When used in addition to chemotherapy or hormonal therapy, these inhibitors of osteoclast-mediated bone resorption significantly reduce the incidence of and delay the onset of SREs [3]. Indeed, it is now standard practice to prescribe a bisphosphonate for all breast cancer patients with newly diagnosed bone metastases [4]. Even with potent bisphosphonate therapy, however, patients continue to suffer the morbidity and mortality consequences of bone metastases. The management of patients who are on long-term bisphosphonates when bony progression or SREs occur is unclear. While oncologists traditionally switch systemic anti-cancer therapy upon progression, the impact of switching to an alternate second-line bisphosphonate in these patients remains relatively unexplored [5].
In Canada, the most commonly used bisphosphonates in patients with metastatic breast cancer are intravenous (IV) pamidronate and oral clodronate [6]. Our group recently demonstrated in a phase II study that a switch from first-line standard therapy to IV zoledronic acid was associated with improvement in pain control over an 8 week period (P < 0.001) [7]. In addition, that study evaluated the effect of the switch on urinary excretion of type I collagen N-telopeptide (NTX). NTX is a potentially important alternative surrogate endpoint of response to bisphosphonate therapy because it may allow a more rapid assessment of treatment efficacy [8] and is correlated with the severity of bone pain, symptomatic relief, decrease in the incidence of SREs, and survival [8–10]. Switching to zoledronic acid in that study was followed with a significant decline in urinary NTX excretion over the same eight week time period (P = 0.008). Furthermore, an acute drop in urinary NTX (i.e., by week 1) relative to baseline was identified as a significant predictor of the week eight palliative response to zoledronic acid (OR = 9.4; 95% CI: 2.28–79.8) [7]. Thus, that study demonstrated that by switching to a more potent agent such as zoledronic acid, patients may derive additional palliative benefits from other third-generation agents.
However, zoledronic acid has a considerable economic impact on the health care system related to drug acquisition and delivery. In addition, the need for IV drug delivery is an added burden to the patient. The alternative, ibandronate, is an orally administered third-generation aminobisphosphonate with demonstrated activity in bone metastases from breast cancer [11]. Even though an oral agent may offer economic advantages as well as clinical convenience, it was not known whether it would confer the same significant palliative benefit in the second-line bisphosphonate therapy setting. Therefore, in this phase II study, the palliative efficacy of second-line oral ibandronate was evaluated. Biochemical markers of bone metabolism were also assessed in a pre-planned analysis to determine their clinical utility as early predictors of patient benefit.
Patients and methods
The primary objective of this prospective study was to measure the palliative benefit of second-line oral ibandronate in breast cancer patients with either SREs or progressive bone metastases. Palliative benefit was reflected through the Brief Pain Inventory–BPI) [12, 13]. Palliative response was defined as a reduction of at least two units in the worst pain score using the BPI. Secondary objectives included: changes in urinary NTX over time; correlations between pain scores and NTX levels; and assessment of whether a decrease in urinary NTX at week one relative to baseline was a significant predictor of palliative response to ibandronate as measured at weeks eight and twelve.
Patients were included in the study if they had histologically confirmed breast cancer and known bone metastases. Patients also had to have either an SRE–defined as pathological vertebral and non-vertebral fractures, spinal cord compression, hypercalcaemia and surgery or radiation to bone, or radiological progression of bone metastases while on clodronate or pamidronate–and good performance status (Karnofsky performance status–KPS >60) with a life expectancy of at least 3 months. Due to potential effects of new systemic therapy on palliative endpoints, new or additional systemic anti-cancer treatments were suspended for the month before or after commencing study treatment. To avoid ibandronate-induced hypocalcaemia, patients were prescribed oral supplementation of calcium and vitamin D starting a month before treatment. Patients with an acute pathological fracture, spinal cord compression or hypercalcemia, prior hypersensitivity to bisphosphonates or severe renal or hepatic dysfunction were excluded from the study.
The Research Ethics Board of Sunnybrook and Women’s College Health Sciences Center approved the study protocol. After patients provided written informed consent to participate, their current bisphosphonate (pamidronate or clodronate) was discontinued and replaced with oral ibandronate 50 mg daily for 12 weeks. Measures of pain, and analgesic use were conducted at baseline and on a weekly basis during the first month and then again at weeks 8 and 12. For those patients who initially received IV pamidronate in the first-line setting, treatment preferences between IV and oral bisphosphonate therapy were also assessed at week 12. Opiate analgesics administered over the 12-week period were also collected and converted into an oral Morphine Equivalent Dose [14]. This data was then used to adjust the potential effect on pain score assessment over the study period.
At the relevant time points, a second pass morning urine sample was also collected and blood drawn for laboratory tests. Apart from routine clinical monitoring, the urine sample was assayed for creatinine by a standard kinetic Jaffe method, and for NTX with the Osteomark enzyme immunoassay kit (Wampole Laboratories, Princeton NJ).
Statistical considerations
Data are presented descriptively as means, medians or proportions. Ordinal logistic regression analysis using a repeated measures structure was used to compare pain control over the 12-week period relative to baseline [15]. Generalized estimating equations (GEE) were also used in a repeated measures analysis on worst pain score and NTX levels relative to baseline. Spearman’s rho was applied to calculate the correlation between NTX levels and pain scores as well as NTX change at week one and change in worst pain score from at eight and twelve relative to baseline. The Likelihood Ratio test as part of a logistic regression analysis was used to determine if a decrease in urinary NTX at week one relative to baseline was a significant predictor of palliative response to ibandronate when measured at week eight and twelve. An initial assessment of urinary NTX revealed that it was skewed by some extreme values. This is a common occurrence with such markers and the standard practice of normalizing the distribution by taking its natural logarithm was employed. The adequacy of the procedure was verified by inspection of the normal plots and application of the Skew test. All of the statistical analyses were performed using Stata, release 9.0 (Stata Corp., College Station, Texas, USA).
Results
A total of 30 patients completed this study. Patients had a mean age of 57 years, a median Karnofsky performance status of 90, and routine biochemistry parameters as expected at study entry (Table 1). Patients had received a median of 2 and 1 lines of prior endocrine and chemotherapy, respectively, for metastatic disease at study entry. Pamidronate was the most commonly prescribed bisphosphonate, with 23 of 30 (76.6%) patients receiving this as first-line agent; the remaining seven were receiving oral clodronate. Median duration of prior bisphosphonate use was 20 months (range 3–69). With respect to study entry criteria, half the patients (15/30) had experienced an SRE and half had radiological progressive bone disease (Table 1). Potential co-varying contaminants in the evaluation of ibandronate and its impact on pain include new systemic therapies and radiation to bone prior to study entry. Overall, the median time between change in systemic therapy and study entry was 113 days (range 21–289) and only one patient received radiation to bone within 30 days of starting the trial (Table 1).
Oral ibandronate was well tolerated and no patient required drug discontinuation because of side effects. After four weeks, new hormonal or chemotherapy was started in 13 of 30 (43.3%) patients (Table 2). Seven new SREs occurred in our sample of 30 patients over the 12 weeks study period (Table 2). When opiate analgesic consumption was measured and expressed as an oral Morphine Equivalent Dose, the data suggested stability over the study period (Fig. 1). At weeks eight and twelve, 46.4% and 46.2% of evaluable patients experienced a palliative benefit, defined as a minimum two unit drop in the worst pain score using the BPI (Table 2). Of the 23 patients who were initially receiving IV pamidronate at the start of the study, 20 (87.0%) preferred oral therapy.
A more detailed analysis on changes in pain scores and urinary NTX over time was performed using a repeated measures regression analysis. By week twelve, there was a statistically significant reduction in worst pain score, average pain score and the number of pain sites (Figs. 2–4). The application of the GEE statistical methodology for repeated measures offered a more quantitative interpretation of the reduction in worst pain scores. After adjusting for analgesic consumption, the data implied that the most dramatic pain reduction occurred by the eighth week of therapy. At weeks eight and twelve, patients experienced on average, a 1.34 and 1.5 unit drop on the BPI score, respectively (Table 3). Therefore, it appears from these findings that maximum pain reduction with oral ibandronate is achieved after at least eight weeks of treatment. Over the same interval, there was also an immediate and statistically significant decline in urinary NTX levels (Fig. 5). Furthermore, the median percent reduction in urinary NTX was immediate, between 30 to 40% and remained stable at this level over the entire 12 week treatment period (Fig. 6).
The final series of analyses was the evaluation of urinary NTX as a predictor of pain control by correlation analysis (Spearman rho). Significant associations were found between urinary NTX levels and worst pain score (rho = 0.29; P < 0.001), average pain score (rho = 0.19; P = 0.0077) and number of pain sites (rho = 0.21; P = 0.0032). However, in contrast to our earlier second-line zoledronic acid study [7], a drop in NTX at week one was not a significant predictor of palliative response assessed at week eight or week twelve.
Discussion
Bisphosphonates are an accepted standard of practice in the management of breast cancer patients with bone metastases. However, many questions about their use remain unanswered [16, 17]. Even with bisphosphonate therapy from the time of diagnosis of bone metastases, many patients will continue to have SREs and nearly all will have progression of their bone disease [3]. In clinical practice, most patients with bony progression and SREs are maintained on the same agent without any supportive evidence. The findings of the current study, which are consistent with our previous work have shown that second-line therapy with a more potent agent such as oral ibandronate can provide substantial palliative benefit in patients who have had bony progression or an SRE while on a first-line agent. Keeping in mind the caveats associated with cross-trial comparisons, the pain response and urinary NTX drop appear to be of the same magnitude as with second-line zoledronic acid [7].
Urinary NTX was also significantly correlated with the level of pain. However, in contrast to our phase II study with zoledronic acid, a week one drop in urinary NTX was not a significant predictor of future palliative pain response with oral ibandronate. The lack of correlation may be related to drug bioavailability issues secondary to absence of an IV ibandronate loading dose at the start of therapy. Such an IV loading strategy is currently being evaluated in other studies [18].
Although bisphosphonates have clearly revolutionized the treatment of bone metastases, the optimal use of these agents in all types of patients is not known. In addition, there is no evidence supporting their continued use upon bony progression and multiple SREs. As a result, patients often continue to receive the same bisphosphonate until death. One multicenter drug-use evaluation study uncovered the fact that a bisphosphonate was the last IV drug administered prior to death in 90% of patients [6].
The repeat visits to the cancer centre for IV bisphosphonate therapy are costly to the health care system and to the patient in terms of added burden. It is interesting, but hardly surprising, that 20 of 23 (87.0%) patients who initially received first-line IV pamidronate indicated that they preferred oral therapy. A cost-effective strategy may therefore be to initiate therapy with the less expensive pamidronate or clodronate drug, and then to substitute second-line oral ibandronate in those who develop SREs or new bony metastases [19]. This might also help address concerns raised about toxic side-effects associated with prolonged potent bisphosphonate use, such as osteonecrosis of the jaw [20].
There a number of limitations in the current study that should be recognized. This was a small single-centre, open-label, phase II non-randomised trial. Larger confirmatory studies from multiple centres are required to confirm our findings. The current trial protocol limited the treating clinician to a change of systemic anticancer therapy only after week four. Even though this occurred in 13 patients, such new treatments may have contaminated our measurements of pain control. Further research is also needed to identify factors that accurately predict subgroups of patients who are at the highest risk for developing detectable bone metastases and bony complications. The information could then be used to develop a risk stratification model allowing the up-front identification of patients most likely to benefit from the use of more potent agents such as ibandronate or zoledronic acid. What is apparent from the current study is that not all patients may require the front-line use of the more potent bisphosphonates. Markers of bone turnover should be helpful in identifying such patients and may also be useful in monitoring the effectiveness of therapy [8, 9, 21]. More definitive conclusions require a randomised trial of continued therapy with the same agent such a pamidronate, or randomizing to a second-line more potent agent like zoledronic acid or ibandronate. Our group has recently started this much-needed trial in order to confirm the hypothesis that additional patient benefit can be achieved from switching to a more potent agent after either an SRE or bony progression.
In conclusion, patients with either progressive bone metastases or SREs while on clodronate or pamidronate can have relevant palliative benefits with a switch to the more potent bisphosphonate. If confirmed through randomized trials, clinicians can start breaking away from the paradigm whereby patients remain on a single sub-optimal bisphosphonate regimen throughout the course of their disease.
References
Jemal A, Siegel R, Ward E et al (2006) Cancer statistics, 2005. CA Cancer J Clin 56(10):106–130
Plunkett TA, Smith P, Rubens RD (2000) Risk of complications from bone metastases in breast cancer: implications for management. Eur J Cancer 36:476–2
Ross JR, Saunders Y, Edmonds PM et al (2003) Systematic review of role of bisphosphonates on skeletal morbidity in metastatic cancer. BMJ 327:469–475
Hillner B, Ingle JN, Chlebowski RT et al (2003) American Society of Clinical Oncology. American Society Of Clinical Oncology 2003 Update on the role of bisphosphonates and bone health issues in women with breast cancer. J Clin Oncol 21:4042–4057
Jagdev SP, Purohit OP, Heatley S et al (2001) Comparison of the effects of intravenous pamidronate and oral clodronate on symptoms and bone resorption in patients with metastatic bone disease. Ann Oncol 12: 1433–1438
Clemons M, Enright K, Cesta A et al (2004) Do physicians follow systemic treatment and funding policy guidelines? Can J Clin Pharmacol 11:168–178
Clemons M, Dranitsaris G, Ooi WS et al (2006) A phase II trial evaluating the palliative benefit of second-line Zoledronic acid in breast cancer patients with either a skeletal related event or progressive bone metastases despite first line bisphosphonate therapy. J Clin Oncol 24:4895–4900
Brown JE, Ellis SP, Gutcher SA et al (2005) Using bone turnover markers to direct bisphosphonate therapy: is this a feasible approach? Cancer Treat Rev 31:S30
Ali SM, Demers LM, Leitzel K et al (2004) Baseline serum NTx levels are prognostic in metastatic breast cancer patients with bone-only metastases. Ann Oncol 15:455–459
Coleman RE, Major P, Lipton A et al (2005) Predictive value of bone resorption and formation markers in cancer patients with bone metastases receiving the bisphosphonate zoledronic acid. J Clin Oncol 23:4925–4935
Body JJ, Diel IJ, Lichinitzer M et al (2004) Oral ibandronate reduces the risk of skeletal complications in breast cancer patients with metastatic bone disease: results from two randomized, placebo controlled phase III studies. Br J Cancer 90:1133–1137
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the brief pain inventory. Ann Acad Med 23:129–138
Cella DF, Tulsky DS, Gray G et al (1993) The Functional Assessment of Cancer Therapy (FACT) scale: development and validation of the general measure. J Clin Oncol 11:570–579
Repchinky C (ed) (2005) Compendium of pharmaceuticals and specialties. Canadian Pharmacist Association, Ottawa, ON
Allison PD (1999) Logistic regression using the sas system: theory and application; chapter 8. Cary, NC, SAS Institute Inc, p. 179–216
Major P, Cook R (2002) Efficacy of bisphosphonates in the management of skeletal complications of bone metastases and selection of clinical end-points. Am J Clin Oncol 25:s10–s18
Gainford MC, Dranitsaris G, Clemons M (2005) Recent developments in bisphosphonates for patients with metastatic breast cancer. BMJ 330:769–773
Diel IJ (2005) Ibandronate: efficacy in the treatment of metastatic bone disease. Future Oncol 1:593–607
De Cock E, Hutton J, Canney P et al (2005) Cost-effectiveness of oral ibandronate versus IV zoledronic acid or IV pamidronate for bone metastases in patients receiving oral hormonal therapy for breast cancer in the United Kingdom. Clin Ther 27:1295–310
Bamias A, Kastritis E, Bamia E et al (2005) Osteonecrosis of the jaw in cancer after treatment with bisphosphonates: incidence and risk factors. J Clin Oncol 23:8580–8587
Clamp A, Danson S, Nguyen H et al (2004) Assessment of therapeutic response in patients with metastatic bone disease. Lancet Oncol 5:607–16
Acknowledgments
We are grateful to Geetha Yogendran, Tatjana Sukovic, Betty YL Wong for their clinical and laboratory assistance with this project.
Initial findings from the study were presented as a late breaking poster presentation at The 29th Annual San Antonio Breast Cancer Symposium, December 8–11, 2006 in San Antonio, Texas. Abstract number: 3147.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clemons, M., Dranitsaris, G., Ooi, W. et al. A phase II trial evaluating the palliative benefit of second-line oral ibandronate in breast cancer patients with either a skeletal related event (SRE) or progressive bone metastases (BM) despite standard bisphosphonate (BP) therapy. Breast Cancer Res Treat 108, 79–85 (2008). https://doi.org/10.1007/s10549-007-9583-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9583-y