Abstract
Background
Radial scar (RS) is a benign breast lesion but a variable percentage of cases are associated with atypical epithelial proliferations and cancer. Previous studies have shown that patient age and the size of RS are correlated to a potential neoplastic transformation.
Method
We collected 117 asymptomatic patients with suspected RS following a mammogram, histologically confirmed. The clinical, pathological and immunophenotypical analysis is reported. The cases are subdivided into three different groups: (1) RS “Pure”, without epithelial atypia; (2) RS associated with epithelial atypical hyperplasia; (3) RS with cancer.
Results
“Pure” RS was detected in 55 patients (47%); the mean age was 48.1 years and the mean size 0.94 cm. RS associated with atypical epithelial hyperplasia was identified in 25 cases (21%) with a mean age of 53.1 years and a mean size of 0.98 cm. Carcinoma in RS was observed in 37 cases (32%); the mean age was 55.5 years and the mean size was 1.16 cm. The mean age was statistically significant (P = 0.004) in separating RS with cancer from the two other RS groups. The size of RS was not sufficiently statistically significant (P = 0.2) to differentiate the risk. Atypical lesions and cancers showed a morphology and marker of low-grade aggressiveness.
Conclusion
RS seems to represent a natural model of carcinogenesis starting from a proliferative lesion in patients of less than 50 years of age and developing into an atypical and later into a carcinomatous lesion. The fact that most carcinomas arising in RS are low grade also favors this hypothesis. All RS should be excised.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radial scar/complex sclerosing lesion (RS) is a benign breast lesion that on radiological imaging and histologycal analysis may mimic invasive carcinoma [1]. RS was initially described as “sclerosing papillary proliferation” by Fenoglio and Lattes [2] and not long after was named “Strahlige Narben” (translated as “radial scar”) by Hamperl et al. in 1975 [3]. Many other terms including “non-encapsulated sclerosing lesion”, “infiltrating epitheliosis”, “indurative mastopathy”, “sclero-elastotic focal lesions” have been used to describe this lesion over the years [4–7], but RS is the currently adopted name. On mammograms RS has a characteristic, well-known, “black star” appearance with long, thin spicules radiating from a radiolucent central area [8]. It is histologically characterized by a sclerotic center with a central core, containing obliterated ducts and infiltrating tubules, surrounded by a corona of contracted ducts and lobules [9]. Before mammographic screening was available, RS was mostly an incidental finding in breast specimens removed for other clinically suspicious lesions [10–12], but nowadays it is increasingly recognized as a primary lesion in asymptomatic patients with atypical mammograms.
In recent years, it has become apparent that RS, albeit benign, is a lesion that carries the risk of a carcinoma developing within its context [13–15] and a subsequent breast carcinoma with an increased relative risk (R.R.1.8) when compared with the normal female population [16]. The size of RS seems to define the risk of associated cancer, the risk being higher when the lesions are large [13, 17–19]. Cancer in RS seems to be infrequent in patients of less than 50 years of age [1, 13].
The aim of the paper is to analyze, in a series of asymptomatic RS, the relationship between RS lesions and breast cancer associated with RS and to highlight the risk factors for developing carcinoma in RS context.
Materials and methods
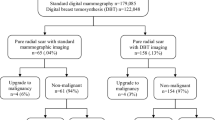
Between January 1989 and December 2004, from the files of the Department of Pathology at “G.B. Rossi” University Hospital in Verona, we collected 117 cases of RS in asymptomatic patients who underwent surgery due to a mammographic stellate lesion. All cases, where RS was an incidental microscopic finding in breast biopsy carried out for other reasons, were excluded.
The Patients’ records were complete in terms of age, clinical and imaging data. Post-surgery follow-up was also examined. The slides of all the cases were reviewed to confirm the diagnosis of RS and the size of the lesion and foci of epithelial atypia or associated carcinoma were recorded. For all those cases, where a carcinoma was detected, the histo-phenotype of the neoplasia and the status of the axillary nodes, if dissected, were specified. The immunohistochemical panel performed consisted of Estrogen Receptor alpha (ER), Progesterone Receptor (PgR), Proliferating index (Ki67) and Her-2/neu status.
For the purpose of this study, radial scar lesions were subdivided into three different groups: “Pure” RS without epithelial atypia (Group 1); RS with associated atypical epithelial hyperplasia (ductal or lobular) (Group 2); RS with cancer, in situ or infiltrating, detected inside the lesion (Group 3).
We used t-test and Analysis of Variance (ANOVA) as statistical analysis to evaluate the significance of the difference in mean age and size of the three different groups of RS. Statistical results were considered significant at a P-value < 0.05. All statistical tests were performed using the SAS software.
Results
The clinical-pathological features are summarized in Table 1.
Of the total series, the mean age of patients was 51.1 years (range 25–84) and none showed clinical symptoms (breast pain, cutaneous changes or palpable mass). All patients underwent a diagnostic excisional biopsy to confirm the radiological suspicion (Fig. 1).
(A) “Black star”. Mammograph showing the typical features of RS: radiolucent central core, elongated radiating spicules and infrequent calcification. (B) Radial scar. A sclerotic center with a central core, containing obliterated ducts and infiltrating tubules, surrounded by a corona of contracted ducts and lobules with a pseudo-cystic appearance
The classic morpho-histological appearance of RS was observed in all cases and consisted of a stellate lesion with a central scleroelastotic core with radiating proliferations of intraductal papillomatosis, sclerosing and florid adenosis, apocrine cysts, duct ectasia and benign epithelial hyperplasia. All RS had a classic stellate shape (Fig. 2) with an ipo-cellular core consisting of a rich elastotic matrix in a pink connective. There were connective fibers with a characteristic cotton-like look in the elastotic matrix (Fig. 3). A pseudo-infiltrative aspect mimicking carcinoma was observed when isolated epithelial ducts were entrapped in the scleroelastotic central core (Fig. 3).
(A) Two radial scars similar in size in the same excisional biopsy (arrows) (20 × , H&E). (B) Dilated ducts in the periphery of radial scar with a pseudo-cystic pattern. Entrapped ducts show a pseudo-infiltrative pattern mimicking carcinoma (20 × , H&E). (C) Ducts showing proliferative hyperplasia without atypia. (100 × , H&E). (D) Elastotic matrix with a cotton-like appearance associated with entrapped duct. (200 × , H&E). (E) Calcification located in benign epithelial hyperplasia at the periphery of the radial scar. Many ducts are enlarged and one of these shows an apocrine metaplasia. (40 × , H&E). (F) Solid and cribiform ductal carcinoma in situ associated with elastosic matrix (100 × , H&E). (G) Lobular carcinoma in situ involving radial scar lesion (40 × , H&E). (H) Tabular carcinoma arising in the core of radial scar. Immunoistochemistry and shape of the ducts can help to distinguish entrapped ducts from carcinoma. (40 × , H&E)
“Pure” RS was detected in 55/117 patients (47%), RS associated with atypical epithelial hyperplasia was identified in 25/117 cases (21%) and carcinoma associated with RS was present in 37/117 cases (32%). The mean diameter of the entire RS series was 1.07 cm (range 0.3– 4).
“Pure” radial scar (55 cases)
“Pure” RS was identified in 55/117 breast specimens (47%). The mean age of patients was 48.1 years (range 25–66) (Table 1) (Fig. 4). Two of the patients had had a previous contralateral breast carcinoma.
The mean size of RS was 0.94 cm (range 0.3–4). Calcifications were identified in 34/55 cases (62%), and mostly limited to the periphery of the lesion within the lumen of dilated ductules (Fig. 3).
Follow-up was available in 27 cases (49%). The mean follow-up period was 100 months (range 17–216). None of the patients underwent any further treatment related to RS. One patient later underwent breast surgery due to a mucocele-like lesion and another for multiple papillomatosis. Two other patients developed gynecological neoplasia, 1 endometrial carcinoma and 1 carcinoma of the ovary. All patients are still alive.
Radial scar with associated atypical epithelial hyperplasia (25 cases)
In 25/117 cases (21%), RS was associated with atypical epithelial hyperplasia. The mean age of patients was 53.1 years (range 31–71) (Table 1) ( Fig. 4). Two of them had previously been submitted to surgery for carcinoma in the contralateral breast.
The mean size of RS was 0.98 cm (range 0.4–3). In five cases (20%) atypical hyperplasia only involved ducts and in eight cases (32%) it was confined to lobular units. In 12 cases (48%) atypical hyperplasia was mixed, involving both ductal and lobular structures. Atypical duct hyperplasia was frequently present at the periphery of RS, while lobular atypical hyperplasia was usually observed in the core.
Small calcifications were present in 14/25 cases (56%) with the same pattern as the “pure” RS group, but very rarely associated with atypical cells.
Follow-up was available in 13/25 cases (52%). The mean follow-up period was 86 months (range 37–204). None of these patients underwent any further surgery or medical treatment. All patients with follow-up are alive and well.
RS with associated breast carcinoma (37 cases)
About of 37/117 RS (32%) were associated with breast carcinoma. The mean age of patients was 55.5 years (range 38–84) (Table 1) ( Fig. 4) and the mean lesion size was 1.16 cm (range 0.4–2.5). Small calcifications were present in 18/37 cases (47%) with the same pattern as “pure” RS. Calcifications were rarely observed in neoplastic foci. The follow-up was available for 32 of the 37 cases (86.5%).
In situ carcinoma was identified in 22/37 cases (59%). The mean age of patients was 56.17 years (range 43–84). The mean RS size was 1.07 cm (range 0.4–2.5) and the associated carcinoma had a mean diameter of 0.58 cm (range 0.1–1.5). The histotype was intraductal (DCIS) in 14 cases (Fig. 3), intralobular neoplasia in six cases (Fig. 3) and mixed, intraductal and intralobular in two cases. DCIS had a cribriform pattern in four cases, solid-cribriform in three cases, solid-comedo in one case, apocrine in one case, cribriform-clinging in two cases and in three cases DCIS was non-specified (NAS). Intraductal neoplasia was well-differentiated (G1) in 14 cases, moderately differentiated in one case (G2) and poorly-differentiated in one case (G3). Calcifications were identified in 12/22 cases.
Invasive carcinoma was present in 15 cases (41%). 2/15 patients had previously had a breast carcinoma and 1/15 had a contralateral breast carcinoma simultaneously to RS associated with carcinoma. The mean age of patients was 55 years (range 38–68). The mean RS size was 1.31 cm (range 0.5–2.5) and the associated carcinoma had a mean diameter of 1.05 cm (range 0.1–1.6). The histotype was tubular in eight cases (53.3%), ductal (IDC) in two cases (13.3%) and lobular (ILC) in five cases (33.3%). Tubular carcinomas were G1, IDC were 1 G1 and 1 G2. All ILC (5/5) were of the classic-type. In no case was vascular invasion observed.
Carcinomas involved the surgical margins of the biopsies in 7/37 cases (18.9%); these cancers were invasive in three cases and in situ in four cases. Of the patients where the surgical margins were involved by in situ carcinoma, only one case was submitted to conservative surgical re-excision. On the other hand, all of the patients with invasive carcinoma in the surgical margin underwent further surgery (one radical mastectomy and two wide re-excision). Node axillary dissection was performed in four cases of tubular carcinoma and in two cases of ILC; metastases were identified in one case of tubular carcinoma (1/5 nodes was involved) and one case of ILC (34/35 nodes were involved).
Immunophenotypical data were available in 11/22 in situ carcinoma and in 9/15 invasive carcinoma. All carcinomas were ER and PgR positive with a rate of neoplastic positive cells ranging from 30 to 90% and from 5 to 90%, respectively. Proliferating index was low (range in neoplastic cells: 1–8%) [20]. No amplification or over-expression of Her-2/neu was detected in 7/37 cancers of the series analyzed.
Surgery was the only treatment for most cases except for 7/22 patients with in situ carcinoma and 5/15 patients with invasive carcinoma who underwent adjuvant hormonal therapy. In two cases with invasive carcinoma chemotherapy was associated with hormonal therapy. In five cases of RS with invasive carcinoma data on treatment were unavailable.
Follow-up data for the patients with RS and in situ carcinoma (mean time 75 months; range 23–170) show that they are all alive and well, except for one elderly patient who died for other unrelated causes. For those patients affected by RS with associated invasive carcinoma, the mean follow-up time was 83.71 months (range 59–212). Four years later, one patient developed an intraductal carcinoma in RS in the contralateral breast.
Statistical analysis
Statistical evaluation showed a close relationship between carcinoma in RS and patient age. Our data show that age has a statistical significance for cancer risk when “pure” RS are compared with RS with epithelial atypia and RS with carcinoma (P = 0.004) (Fig. 5). There is no statistical age-difference between RS associated with atypical hyperplasia and RS associated with carcinoma.
A size difference between the various groups of RS was present but not statistically significant (P = 0.2) (Fig. 6). The mean diameter of RS associated with carcinoma was >1 cm while the mean diameter of the other two groups was < 1 cm. Nevertheless, this size could not be used as a potential preoperative cut-off value to distinguish RS with or without carcinoma because of the lack of real statistical support.
Discussion
Radial scar is increasingly observed in asymptomatic patients due to mammographic imaging particularly in a screening program. The radiological aspect of a stellate lesion mimicking infiltrative carcinoma has been the cause of surgical over-treatment in the past and, for many years, it has been quite difficult to establish strict criteria to avoid the misdiagnosis of cancer. On the other hand, it has become apparent that RS should be considered a lesion that carries the risk of a carcinoma developing within its context. According to various study series, the rate for carcinomas arising in RS ranges from 3 to 41% [8, 10, 13, 14, 17, 18, 21, 22]. In this study, from the analysis of 117 cases of RS, the incidence of associated carcinoma and atypical hyperplasia was 32% and 21% respectively. The rate of carcinoma occurrence is higher than in most reported studies. A possible explanation of this high rate seems to lie in the selection of our cases. We only considered asymptomatic, mammographically suspicious cases and not RS observed as an incidental finding in surgical biopsy performed for other lesions, thus reducing the number of microscopic benign RS. In fact, studies with the same patient selection criteria have a carcinoma rate similar to our data [8, 14, 17].
Patient age seems to influence the risk of cancer in RS. Many Authors have concluded that carcinoma in RS is very rare when the patient is under 50 years of age [1, 13, 23]. Our data support this finding and show that age has a statistical significance for cancer risk when cases of “pure” RS are compared with RS with epithelial atypia and RS with carcinoma (P = 0.004) (Fig. 5). This evidence states that pre-malignant and malignant proliferations arising in RS are infrequent under 50 years of age and that patients with carcinoma and atypical hyperplasia in RS are older than those with “pure” RS [13, 23]. The mean age distribution of the three different RS groups graphically results in a continuous crescent-shaped line that shows risk progression (Fig. 5). This could suggest that pure RS may represent an early stage related to neoplastic transformation [13, 16]. However, age alone cannot exclude the presence of atypia in RS. In fact, in our series 32% of atypical epithelial proliferation and 24% of cancers in RS were found in patients of less than 50.
The size of RS has been considered as a way to differentiate the risk of cancer in these lesions. Sloane et al. have reported that 0.6 cm was a cut-off value below which carcinoma was very rare and above which cancer was relatively common [13]. In previous communications we reported that RS larger than 1 cm was consistently associated with pre-malignant or overtly malignant lesions [15]. In our current series, the mean diameter of RS associated with carcinoma is >1 cm while the mean diameter for the other two kinds of RS is <1 cm (Table 1), but a potential size difference has no statistical significance (P = 0.2) (Fig. 6).
Invasive cancers in RS are low-grade and the staging of patients is prognostically favorable [17, 19, 24]. We found that the most frequent histotype of invasive cancer was tubular (53%) and classic-type lobular (33%). Low clinical staging and good biological profile of the cancers (positivity for estrogen and progesterone receptors, low proliferative index) explain the favourable prognosis of patients with either invasive or in situ neoplasia in our series and in Literature [17, 19, 24]. In our study, follow-up was available for 61.5% of cases, no local recurrence or death due to related breast disease has been observed since RS with atypical hyperplasia or carcinoma was diagnosed.
In one exceptional case (Lobular carcinoma) however, we observed 34 metastases in 35 nodes. This unusual case has been followed up for 5 years without recurrence but the prognosis is gloomy.
In conclusion, RS seems to represent a natural model of carcinogenesis starting from a proliferative lesion in patients of less than 50 years of age and developing into an atypical and then carcinomatous lesion in later years. The fact that most carcinomas arising in RS are low grade also favors this hypothesis. All cases of RS should be excised because of the intrinsic risk of neoplastic transformation.
Reference
Tavassoli FA, Devilee P (2003) WHO pathology and genetics of tumors of the breast and female genital organs. WHO, Lyon
Fenoglio C, Lattes R (1974) Sclerosing papillary proliferations in the female breast. A benign proliferation often mistaken for carcinoma. Cancer 33(3):691–700
Hamperl H (1975) Radial scars (scarring) and obliterating mastopathy (author’s transl). Virchows Arch A Pathol Anat Histol 29 369(1):55–68
Eusebi V, Grassigli A, Grosso F (1976) Breast sclero-elastotic focal lesions simulating infiltrating carcinoma. Pathologica 68(985–986):507–518
Fisher ER, Palekar AS, Kotwal N et al (1979) A nonencapsulated sclerosing lesion of the breast. Am J Clin Pathol 71(3):240–246
Azzopardi JG (1979) Infiltrating epitheliosis. In: Problems in breast pathology, 1st edn. Saunders, London
Rickert RR, Kalisher L, Hutter RV (1981) Indurative mastopathy: a benign sclerosing lesion of breast with elastosis which may simulate carcinoma. Cancer 47(3):561–571
Alleva DQ, Smetherman DH, Farr GH Jr et al (1999) Radial scar of the breast: radiologic-pathologic correlation in 22 cases. Radiographics 19 Spec No:S27–S35
Rosen PP (2001) Rosen’s breast pathology, 2nd edn. Lippincott Williams & Wilkins Publishers, Philadelphia
Patterson JA, Scott M, Anderson N et al (2004) Radial scar, complex sclerosing lesion and risk of breast cancer. Analysis of 175 cases in Northern Ireland. Eur J Surg Oncol 30(10):1065–1068
Cohen MA, Sferlazza SJ (2000) Role of sonography in evaluation of radial scars of the breast. Am J Roentgenol 174(4):1075–1078
Azavedo E, Svane G (1992) Radial scar detected mammographically in a breast cancer screening programme. Eur J Radiol 15(1):18–21
Sloane JP, Mayers MM (1993) Carcinoma and atypical hyperplasia in radial scars and complex sclerosing lesions: importance of lesion size and patient age. Histopathology 23(3):225–231
Caneva A, Bonetti F, Manfrin E et al (1997) Is radial scar of the breast a premalignant lesion? Paper presented at the 86th USCAP Annual Meeting, Orlando, Florida, 1–7 March 1997
Manfrin E, Reghellin D, Remo A et al (2003) Radial scar and carcinoma of the breast. Paper presented at the 92nd USCAP Annual Meeting, Washington DC, 22–28 March 2003
Jacobs TW, Byrne C, Colditz G et al (1999) Radial scars in benign breast-biopsy specimens and the risk of breast cancer. N Engl J Med 11 340(6):430–436
Mokbel K, Price RK, Carpenter R (1999) Radial scars and breast cancer. N Engl J Med 15; 341(3):210
King TA, Scharfenberg JC, Smetherman DH et al (2000) A better understanding of the term radial scar. Am J Surg 180(6):432–433
Alvarado-Cabrero I, Tavassoli FA (2000) Neoplastic and malignant lesion involving or arising in a radial scar: a clinicopathologic analysis of 17 cases. Breast Journal 6(2):96–102
Molino A, Micciolo R, Turazza M et al (1997) Ki-67 immunostaining in 322 primary breast cancers: associations with clinical and pathological variables and prognosis. Int J Cancer 22; 74(4):433–437
Fasih T, Jain M, Shrimankar J (2005) All radial scar/complex sclerosing lesions seen on breast screening mammograms ` be excised. Eur J Surg Oncol 31(10):1125–1128
Patel A, Steel Y, McKenzie J et al (1997) Radial scars: a review of 30 cases. Eur J Surg Oncol 23(3):202–205
Douglas-Jones AG, Pace DP (1997) Pathology of R4 spiculated lesions in the breast screening programme. Histopathology 30(3):214–20
Frouge C, Tristant H, Guinebretiere JM et al (1995) Mammographic lesions suggestive of radial scars: microscopic findings in 40 cases. Radiology 195(3):623–5
Acknowledgements
This work was supported by: Fondazione Cassa di Risparmio di Verona Vicenza Belluno e Ancona. “Carcinoma della mammella: marcatori fenotipici e molecolari indicatori di prognosi e risposta terapeutica”. Bando di ricerca scientifica 2004, indirizzo biomedico. Resp Scientifico: Prof Franco Bonetti
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Manfrin, E., Remo, A., Falsirollo, F. et al. Risk of neoplastic transformation in asymptomatic radial scar. Analysis of 117 cases. Breast Cancer Res Treat 107, 371–377 (2008). https://doi.org/10.1007/s10549-007-9569-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9569-9