Abstract
Background
The two-gene expression ratio HOXB13:IL17BR has been proposed to predict the outcome of tamoxifen-treated breast cancer patients. We intended to examine whether this ratio can predict the benefit of 5 years vs. 2 years of tamoxifen treatment of postmenopausal patients. A further objective was to investigate any prognostic effects of the ratio in systematically untreated premenopausal patients. Based on the current knowledge of HOXB13 and IL17BR, we hypothesized that these genes may have individual prognostic or predictive power.
Patients and methods
Expression of HOXB13 and IL17BR were quantified by real-time PCR in tumors from 264 randomized postmenopausal patients and 93 systemically untreated premenopausal patients.
Results
A high HOXB13:IL17BR ratio was associated with aggressive tumor characteristics, as were low levels of IL17BR alone. The ratio and HOXB13 alone predicted recurrence-free survival after endocrine treatment, with a benefit of prolonged treatment in estrogen receptor-positive patients correlated to a low ratio (recurrence rate ratio: RR = 0.39; P = 0.030), or low expression of HOXB13 (RR = 0.37; P = 0.015). No difference in recurrence-free survival was seen for the high ratio or high HOXB13 subgroups. The predictive value of HOXB13 and HOXB13:IL17BR was significant in multivariate analysis. In the systemically untreated cohort, only IL17BR showed independent prognostic significance.
Conclusion
We conclude that the ratio or HOXB13 alone can predict the benefit of endocrine therapy, with a high ratio or a high expression rendering patients less likely to respond. We have also shown that IL17BR might be an independent prognostic factor in breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Optimal development of endocrine treatment for women with breast cancer requires evaluation of potential biomarkers so that additional prognostic and predictive markers can be implemented in the clinic. The presence of estrogen (ER) and progesterone receptors (PgR) in breast cancer cells is the most important determinant for predicting the response to adjuvant endocrine treatment with tamoxifen in primary breast cancer. Five years of tamoxifen treatment of ER-positive patients reduce the annual breast cancer death rate by about one third, but still almost 25% of the women participating in trials of adjuvant endocrine therapy with tamoxifen fail to respond and relapse within 10 years [1]. These patients represent a group where alternative therapies could be beneficial.
Sorlie et al. [2] showed that clinical outcome of breast cancer could be predicted by using gene expression profiles, and since then, several studies have been performed in order to develop predictive models. Some studies have shown that gene expression profiles are linked to ER status [3, 4] and to clinical outcome [2, 5–7]. In metastatic breast cancer, a 44-gene expression signature was found to be associated with an objective response to tamoxifen [8]. Paik and co-workers developed a recurrence score, based on 21 genes, which correlated with the likelihood of distant recurrence in node-negative patients after adjuvant tamoxifen [9]. Ma et al. performed a genome-wide microarray analysis of tumors from ER-positive patients treated with adjuvant tamoxifen, in which they were able to reduce an expression signature to a two-gene expression ratio predictive of disease-free survival [10]. Homeobox B13 (HOXB13) over interleukin 17B receptor (IL17BR) was found to be strongly correlated with treatment outcome, with higher ratios associated with decreased disease-free survival. In another study, these results could not be verified [11]. However, the cohort of 58 patients in this study, mainly comprised lymph node-positive patients, and subsequent studies on the two gene expression ratio have suggested that the principal prognostic value may be found among lymph node-negative patients [12, 13]. As the importance of HOXB13:IL17BR has not been evaluated in a randomized study comparing adjuvant tamoxifen vs. no adjuvant tamoxifen, the importance of the ratio for predicting the response to adjuvant tamoxifen is still a matter of debate.
The aim of the present study was to investigate the significance of the HOXB13 to IL17BR ratio in a large cohort of postmenopausal breast cancer patients. The patients in our study were participants in a previous randomized trial investigating the benefit of 5 versus 2 years of adjuvant tamoxifen treatment. This enabled us to investigate whether the two-gene expression ratio, or either of the genes alone, can predict the benefit of prolonged treatment in postmenopausal women. A further objective was to analyze the expression ratio in a cohort of systematically untreated premenopausal patients, in order to investigate any prognostic effects of the genes. Based on the current knowledge of HOXB13 and IL17BR, and the fact that they do not seem to have a functional interconnection, we hypothesized that the genes could have individual prognostic or predictive power.
Materials & methods
Patients
This study was performed as a collaborative study including two centers in the Southeast (Center 1) and South (Center 2) Health Care Regions in Sweden. The study was approved by the local ethical committee in Lund. We analyzed tissue from excised primary tumors of a total of 373 women, treated in these regions between 1982 and 1995. The postmenopausal patients were participants in a randomized clinical trial, comparing 2 and 5 years of adjuvant tamoxifen treatment [14]. The premenopausal patients were enrolled in a trial aimed at comparing the effect of tamoxifen treatment versus no treatment [15]. From this trial, only patients from the untreated cohort were chosen. The patients underwent modified radical mastectomy or breast conserving surgery with axillary lymph node dissection. After breast conserving surgery, radiotherapy (50 Gy/25 fractions) was delivered locoregionally to patients with lymph node-positive breast cancer. In the present study, subsets of patients from the two trials were included, based on availability of frozen tumor material and RNA quality. After surgery, the tumor samples were stored at −70°C.
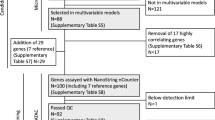
ER and PgR content, HER2 status, DNA ploidy, proportion of cells in S-phase, and Nottingham histologic grade (NHG) were assessed as in clinical routine practice and as previously described [15–17]. Of 373 tumor samples analyzed, RNA expression data were obtained from 357 tumors, 264 were postmenopausal and 93 were premenopausal patients. The selected groups of patients did not significantly differ from the original cohorts in terms of clinical and tumor characteristics, except for tumor size and the duration of tamoxifen treatment, with a higher proportion of large tumors and patients treated for two years with tamoxifen in the selected cohorts (Table 1).
Total RNA extraction and cDNA synthesis
Fresh-frozen tumor tissue (30–100 mg) was homogenized with a microdismembrator (B Braun Melsungen AG, Melsungen, Germany) and total RNA was isolated with the SV Total RNA Isolation System (Promega Corporation, Madison, WI; Center 1) or Trizol reagent (Invitrogen Carlsbad, CA) followed by RNeasy Midi kit (Qiagen, Chatsworth, CA; Center 2). RNA quality was tested using RNA 6000 Nano LabChip Kit with Agilent 2100 BioAnalyzer (Agilent Technologies, Palo Alto, CA; Center 2). Concentration was determined using NanoDrop Spectrophotometer (NanoDrop Technologies, Wilmington, DE).
Reverse transcription of RNA was performed with the 1st Strand cDNA Synthesis Kit for RT-PCR (Roche Diagnostics, Indianapolis, IN) with random primers (Center 1), or SuperScript™ II Reverse Transcriptase (Invitrogen) with Anchored Oligo(dT)20 Primer (Invitrogen) (Center 2), according to the manufacturers’ instructions.
Real-time PCR
The relative abundances of HOXB13 and IL17BR mRNA were determined with real-time quantitative PCR with triplicates of each sample. Primer and probe sequences used in the reactions for amplification of the two target genes were as follows: HOXB13: TTCATCCTGACAGTGGCAATAATC (forward) CTAGATAGAAAATATGAGGCTAACGATCAT (reverse), VIC-CGATAACCAGTACTAGCTG (MGB-probe); IL17BR: GCATTAACTAACGATTGGAAACTACATT (forward), GGAAGATGCTTTATTGTTGCATTATC (reverse), VIC-ACAACTTCAAAGCTGTTTTA (MGB-probe) [10]. For amplification of the endogenous reference gene human ACTB (β-actin) the primers and probe used in Center 2 were TCACCCACACTGTGCCCATCTACGA (forward), CAGCGGAACCGCTCATTGCCAATGG (reverse), VIC-ATGCCCTCCCCCATGCCATCCTGCGT (MGB-probe) whereas Center 1 used TaqMan® Endogenous Control (VIC/TAMRA probe). Primers and probes were purchased from Applied Biosystems (Foster City, CA).
Center 1 performed the real-time PCR reactions using ABI Prism 7700 Sequence Detection System (Applied Biosystems) with TaqMan PCR core Reagent Kit (PE Applied Biosystems). Center 2 used Rotor-Gene 3000 (Corbett Research, Sydney, Australia) and TaqMan Universal PCR Master Mix (Applied Biosystems). All reactions were performed according to the manufacturers’ instructions.
A relative kinetic method was applied using four point standard curves in each run, constructed of serial dilutions of cDNA from the breast cancer cell line BT−474. The quantity of the target genes in each sample was determined from the corresponding standard curve, and the amount of HOXB13 and IL17BR was normalized to β-actin quantity. Samples with a β-actin quantity lower than the most diluted sample in the standard curve were excluded from the study. Expression analysis performed for a reproducibility study of both participating centers demonstrated highly concordant results, calculated with Pearson’s correlation (n = 10; HOXB13:β-actin: r = 0.96, P < 0.001, IL17BR:β-actin: r = 0.87, P = 0.002; HOXB13:IL17BR: r = 0.99, P < 0.001). The median values in the two complete subsets, analyzed at the two centers, were similar for HOXB13:β-actin (0.086 vs. 0.081), IL17BR:β-actin (1.4 vs. 1.3), and HOXB13:IL17BR (0.074 vs. 0.055).
Statistical analysis
The relationships between grouped variables were analyzed with the χ2 test, or χ2 test for trend when required. Spearman’s rank order correlation was used when comparing HOXB13 and IL17BR levels. Recurrence-free survival was defined as the time from diagnosis to the first of the following events: local, regional, or distant recurrence or death due to breast cancer. Breast cancer survival was the time elapsed from diagnosis to the date of death due to breast cancer. The median periods of follow-up for recurrence free patients were 9.7 and 11.2 years for premenopausal and postmenopausal patients, respectively. Prior to the statistical analyses, the median values of HOXB13, IL17BR, and their ratio were chosen for cut-off points when patients were divided into categories with low or high expression. Survival curves were calculated using the Kaplan-Meier method and analyzed with the log rank test. Multivariate analysis of recurrence and mortality rates was performed with Cox proportional hazard model. A Cox model was also used to test for the interaction between the two-gene ratio and the benefit from prolonged duration of tamoxifen treatment. Only patients who remained recurrence-free at 2 years were included in the survival analyses, thus, 3 additional years with tamoxifen was compared with no further therapy. The following variables were included: HOXB13:IL17BR ( > median vs. ≤ median), treatment (5 vs. 2 years), lymph node status (N+ vs. N−), tumor size ( > 20 mm vs. ≤ 20 mm), PgR status (PgR+ vs. PgR−), and an interaction variable (HOXB13:IL17BR x treatment). Similar models were used for HOXB13 and IL17BR alone. All statistical analyses were carried out with the Statistica 6.0 software (Statsoft Scandinavia AB, Sweden).
Results
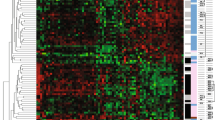
Expression data from 357 tumors were obtained, 264 from postmenopausal patients and 93 from premenopausal. Within these cohorts, 97 (37%) of the postmenopausal and 40 (43%) of the premenopausal women developed recurrence within the follow-up period. The level of the HOXB13:IL17BR ratio was well correlated with both HOXB13 and IL17BR, but HOXB13 had the main impact on the ratio (r s= 0.68 and r s = −0.26, respectively). No significant correlation was found between HOXB13 and IL17BR (r s = 0.06).
Comparisons between the HOXB13:IL17BR ratio and clinicopathological variables revealed a correlation between a high ratio and larger tumors, high histological grade, lack of ER and PgR, positive HER2 status, DNA non-diploidy, and a high proportion of cells in S-phase (Table 2). IL17BR itself, but not HOXB13, was also correlated to a number of factors related to poor prognosis, with lower expression of IL17BR associated with markers of worse outcome. HOXB13 expression, on the other hand, was higher in larger and non-diploid tumors only.
The survival curves for ER-negative postmenopausal patients did not reveal any significant differences for the expression ratio or the genes separately (ratio: P = 0.92, HOXB13: P = 0.30, IL17BR: P = 0.21). Therefore, all further analyses on the postmenopausal cohort were performed in the ER-positive group of patients only.
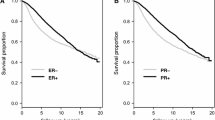
HOXB13, IL17BR, and the benefit of five vs. two years of tamoxifen
Among postmenopausal ER-positive patients, whose tumor displayed a lower ratio of HOXB13:IL17BR, a benefit from a prolonged duration of tamoxifen treatment was evident (P = 0.021; Fig. 1A). This advantage could not be seen among patients with a higher ratio (P = 0.90). Consistent with the predictive power of the lower ratio and the main impact of HOXB13 on the ratio, a low expression of HOXB13 combined with 5 years of tamoxifen was beneficial for the patients (P = 0.010, Fig. 1B). Prolonged treatment was not advantageous in the group with high IL17BR expression (P = 0.44, Fig. 1C), but the beneficial effects of longer endocrine treatment reached borderline significance among patients with low expression of this gene (P = 0.061). The predictive significance of both the two-gene ratio and HOXB13 alone remained true in multivariate analysis using Cox proportional hazard modeling adjusting for tumor size, PgR status, and lymph node status (Table 3). The interaction between IL17BR and the result of prolonged tamoxifen treatment was not significant (Table 3). In order to further validate the finding of the significance of the two-gene ratio in node-positive patients, we performed similar univariate and multivariate analysis as described above, in which we excluded node-negative patients (Table 4). Both the HOXB13:IL17BR ratio and HOXB13 remained significant in this cohort of patients.
HOXB13 and IL17BR as prognostic factors
For systemically untreated premenopausal patients, there was a slight trend that patients with high IL17BR expression had better recurrence-free survival compared to those with low IL17BR expression (P = 0.12; Fig. 2). A similar difference was found for the HOXB13:IL17BR ratio (P = 0.12). However, when HOXB13 and IL17BR were used as continuous variables in univariate analyses according to Cox proportional hazard regression, IL17BR was significantly associated with recurrence (Table 5). With borderline significance, this remained true in multivariate analysis. An independent prognostic significance of the HOXB13:IL17BR ratio was not evident. Similar results were found when breast cancer mortality was analyzed (data not shown). HOXB13 on its own did not influence the outcome, regardless of the endpoint used.
Discussion
By studying 264 postmenopausal patients treated with adjuvant tamoxifen and 93 premenopausal patients, not treated with any systemic adjuvant therapy, we have found that the HOXB13:IL17BR gene expression ratio, and the expression of HOXB13 alone, predict the effect of prolonged treatment with tamoxifen, whereas high IL17BR was associated with low risk of recurrence in the subgroup of systemically untreated patients.
According to previous studies, the clinical importance of the two-gene ratio is largely confined to lymph node-negative patients [10–13]. The patients in the present study, on the other hand, were mainly lymph node-positive (72%). Earlier studies have included patients uniformly treated with tamoxifen and thus can not for certain prove if the ratio is treatment predictive, prognostic, or both, although the recent study by Ma and colleagues indicated a prognostic value in a cohort of untreated patients [13]. The randomization of treatment duration in our group of patients enabled us to investigate whether the two-gene ratio could predict the benefit of prolonged treatment with tamoxifen. In fact, in the present study we have shown that the ratio may have a predictive value also for lymph node-positive patients. In order to validate this finding, we excluded node-negative patients from the analysis and then found the interaction between the two-gene ratio and the treatment effect to remain statistically significant. Our results suggest a possible involvement for at least one of the genes in the development of resistance to tamoxifen. Based on these results, we, unlike previous studies, suggest that the two-gene ratio is valuable also in node-positive patients.
During the analysis of a possible correlation between the ratio (and the genes alone) and a variety of clinicopathological factors, we found that IL17BR, rather than HOXB13, was correlated to a number of factors that are all related to a poor prognosis. This made us hypothesize that IL17BR is more of a prognostic nature, whereas HOXB13 is more implicated in the development of resistance to tamoxifen. In fact, in the subsequent analyses of the individual genes, a high expression of HOXB13 predicted that the patients were unresponsive to prolonged endocrine adjuvant treatment. The gene expression of IL17BR was not of significant treatment predictive value even though tumors expressing a low level of IL17BR seemed to respond better to tamoxifen than tumors with high levels. In the cohort with systematically untreated patients we found that only IL17BR, and not HOXB13, alone had prognostic importance and this remained true, albeit with borderline significance when adjusting for other variables. Taken together, patients with tumors expressing IL17BR at a low level, with a shorter recurrence free survival than those with high IL17BR, may still be candidates for tamoxifen treatment. The HOXB13:IL17BR ratio has previously been shown to be an independent prognostic factor in ER-positive and node-negative patients [13]. The ratio and HOXB13 gene expression could be of importance for identification of which ER-positive breast cancer patients will respond to tamoxifen and those who are resistant and thus need different adjuvant treatment.
HOX genes are known to control morphogenesis and to maintain tissue and organ specificity in the adult body. The implication of the HOXB13 gene product in different types of cancer is beginning to be elucidated. It has been proposed as a marker for prostate cancer [18], and is also believed to be involved in endometrial cancer [19], cervical cancer [20], as well as renal cell carcinoma [21], and colorectal cancer [22]. In human cutaneous malignant melanoma with distant metastasis, the expression level of certain HOX genes, including HOXB13, was higher than in those melanoma patients without metastases [23], and in endometrial cancer cells, antisense-transfection of the HOXB13 gene reduced the invasive ability of the cells [19]. In contrast, overexpression of HOXB13 in prostate cancer cells resulted in inhibition of cell growth and suppression of hormone-activated androgen receptor transcriptional activity, presumably via physical interaction with the receptor [24, 25]. In the same study it was seen that estradiol-stimulated ER activity in breast cancer cells was not suppressed by HOXB13; in fact, if there was any influence on the activity it appears as though HOXB13 enhanced this activity [25]. Recent studies on ER signaling suggests HOXB13 to be an ER target gene since its expression in breast cancer cells is suppressed after estrogen stimulation [26]. A survey of the HOX gene network expression in normal human breast and breast cancer tissue revealed that HOXB13 is upregulated in tumor tissue compared to its normal counterpart [27]. The chromosomal localization of HOXB13 also gives an indication of its importance in breast tumorigenesis [28], since 17q21 is an area harboring a number of genes involved in breast carcinogenesis. Deregulation of HOXB13 may have different consequences in different cancer types but it seems to have oncogenetic properties in some hormone dependent malignancies through interactions with hormone receptors and thus might interact with ER. Overexpression of HOXB13 may therefore contribute to tamoxifen resistance. Further studies are required in order to shed light on the molecular network and interconnections between HOXB13, ER and tamoxifen resistance.
The role of IL17BR in breast cancer is not well explored. The protein is a cytokine receptor that specifically binds to IL17B and IL17E in the IL17 family [29, 30]. One may speculate that IL17BR could act in a protective way by taking part in the immune response against cancer cells, but this remains to be shown. The IL17BR gene is located at 3p21 and this chromosomal region is frequently lost in cancer, including breast cancer. Thus, low expression of IL17BR may correlate with the loss of putative tumor suppressor genes at 3p21, which could be an alternative explanation for the correlation between IL17BR and prognosis.
We have demonstrated that the gene expression of HOXB13 and the HOXB13:IL17BR ratio were able to predict the benefit of prolonged tamoxifen treatment in ER-positive breast cancer patients and may be useful as treatment predictive markers. We have also demonstrated that the expression of IL17BR seems to be an independent prognostic marker, but further studies are needed in a larger cohort of untreated breast cancer patients for confirmation of these findings.
References
Early Breast Cancer Trialists’ Collaborative Group (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365(9472):1687–1717
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98(19):10869–10874
Gruvberger S, Ringner M, Chen Y et al (2001) Estrogen receptor status in breast cancer is associated with remarkably distinct gene expression patterns. Cancer Res 61(16):5979–5984
Sotiriou C, Neo SY, McShane LM et al (2003) Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc Natl Acad Sci USA 100(18):10393–10398
van ‘t Veer LJ, Dai H, van de Vijver MJ et al (2002) Gene expression profiling predicts clinical outcome of breast cancer. Nature 415(6871):530–536
Wang Y, Klijn JG, Zhang Y et al (2005) Gene-expression profiles to predict distant metastasis of lymph-node-negative primary breast cancer. Lancet 365(9460):671–679
van de Vijver MJ, He YD, van ‘t Veer LJ et al (2002) A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med 347(25):1999–2009
Jansen MP, Foekens JA, van Staveren IL et al (2005) Molecular classification of tamoxifen-resistant breast carcinomas by gene expression profiling. J Clin Oncol 23(4):732–740
Paik S, Shak S, Tang G et al (2004) A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351(27):2817–2826
Ma XJ, Wang Z, Ryan PD et al (2004) A two-gene expression ratio predicts clinical outcome in breast cancer patients treated with tamoxifen. Cancer Cell 5(6):607–616
Reid JF, Lusa L, De Cecco L et al (2005) Limits of predictive models using microarray data for breast cancer clinical treatment outcome. J Natl Cancer Inst 97(12):927–930
Goetz MP, Suman VJ, Ingle JN et al (2006) A two-gene expression ratio of homeobox 13 and interleukin−17B receptor for prediction of recurrence and survival in women receiving adjuvant tamoxifen. Clin Cancer Res 12(7 Pt 1):2080–2087
Ma XJ, Hilsenbeck SG, Wang W et al (2006) The HOXB13:IL17BR expression index is a prognostic factor in early-stage breast cancer. J Clin Oncol 24(28):4611–4619
Swedish Breast Cancer Cooperative Group (1996) Randomized trial of two versus five years of adjuvant tamoxifen for postmenopausal early stage breast cancer. J Natl Cancer Inst 88(21):1543–1549
Ryden L, Jonsson PE, Chebil G, et al (2005) Two years of adjuvant tamoxifen in premenopausal patients with breast cancer: a randomised, controlled trial with long-term follow-up. Eur J Cancer 41(2):256–264
Fernö M, Stål O, Baldetorp B et al (2000) Results of two or five years of adjuvant tamoxifen correlated to steroid receptor and S-phase levels. South Sweden Breast Cancer Group, and South–East Sweden Breast Cancer Group. Breast Cancer Res Treat 59(1):69–76
Stål O, Borg Å, Fernö M et al (2000) ErbB2 status and the benefit from two or five years of adjuvant tamoxifen in postmenopausal early stage breast cancer. Ann Oncol 11(12):1545–1550
Edwards S, Campbell C, Flohr P, et al (2005) Expression analysis onto microarrays of randomly selected cDNA clones highlights HOXB13 as a marker of human prostate cancer. Br J Cancer 92(2):376–381
Zhao Y, Yamashita T, Ishikawa M (2005) Regulation of tumor invasion by HOXB13 gene overexpressed in human endometrial cancer. Oncol Rep 13(4):721–726
Lopez R, Garrido E, Pina P et al (2006) HOXB homeobox gene expression in cervical carcinoma. Int J Gynecol Cancer 16(1):329–335
Okuda H, Toyota M, Ishida W, et al (2006) Epigenetic inactivation of the candidate tumor suppressor gene HOXB13 in human renal cell carcinoma. Oncogene 25(12):1733–1742
Jung C, Kim RS, Zhang H et al (2005) HOXB13 is downregulated in colorectal cancer to confer TCF4-mediated transactivation. Br J Cancer 92(12):2233–2239
Maeda K, Hamada J, Takahashi Y, et al (2005) Altered expressions of HOX genes in human cutaneous malignant melanoma. Int J Cancer 114(3):436–441
Jung C, Kim RS, Lee SJ et al (2004) HOXB13 homeodomain protein suppresses the growth of prostate cancer cells by the negative regulation of T-cell factor 4. Cancer Res 64(9):3046–3051
Jung C, Kim RS, Zhang HJ et al (2004) HOXB13 induces growth suppression of prostate cancer cells as a repressor of hormone-activated androgen receptor signaling. Cancer Res 64(24):9185–9192
Rodriguez BAT, Jin VX, Cheng AS, et al (2006) HOXB13 is an estrogen receptor responsive gene preferentially methylated in ER-positive breast cancer. In: Proceedings of the 97th annual meeting, AACR, Washington, USA, 1–5 April 2006
Cantile M, Pettinato G, Procino A, et al (2003) In vivo expression of the whole HOX gene network in human breast cancer. Eur J Cancer 39(2):257–264
Apiou F, Flagiello D, Cillo C, et al (1996) Fine mapping of human HOX gene clusters. Cytogenet Cell Genet 73(1–2):114–115
Shi Y, Ullrich SJ, Zhang J, et al (2000) A novel cytokine receptor–ligand pair. Identification, molecular characterization, and in vivo immunomodulatory activity. J Biol Chem 275(25):19167–19176
Lee J, Ho WH, Maruoka M, et al (2001) IL−17E, a novel proinflammatory ligand for the IL−17 receptor homolog IL−17Rh1. J Biol Chem 276(2):1660–1664
Acknowledgements
We are indebted to participating members of the South and Southeast Sweden Breast Cancer Groups for providing us with breast cancer samples and to Gunilla Chebil and Sten Thorstenson for re-evaluation of histological grade. This study was supported by funds from the Swedish Cancer Society, the Gunnar Arvid and Elisabeth Nilsson Foundation, the Mrs Berta Kamprad Foundation, the Swedish Research Council and the University Hospital of Lund Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Piiha-Lotta Jerevall, Sara Brommesson contributed equally.
Mårten Fernö, Olle Stål—Equally shared senior authorship
Rights and permissions
About this article
Cite this article
Jerevall, PL., Brommesson, S., Strand, C. et al. Exploring the two-gene ratio in breast cancer—independent roles for HOXB13 and IL17BR in prediction of clinical outcome. Breast Cancer Res Treat 107, 225–234 (2008). https://doi.org/10.1007/s10549-007-9541-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9541-8