Abstract
This multicenter phase II trial evaluated the efficacy and tolerability of 4 months of neoadjuvant exemestane in 44 postmenopausal patients with estrogen receptor (ER)-positive and/or progesterone receptor-positive, stage II to IIIB breast cancer measuring ≥3 cm. Pathological response was assessed by a central review board using response criteria proposed by the Japanese Breast Cancer Society. Clinical response [complete or partial response (PR)] was assessed by caliper, mammography, or ultrasound. Rates of breast-conserving surgery (BCS) and adverse events were also evaluated. A pathological response was observed in 13 (43%) of 30 patients who underwent surgery at 4 months. Fourteen patients were excluded from the pathological analysis: eight continued exemestane because of PR or stable disease (SD) at 4 months, three underwent chemotherapy because of progressive disease, and three underwent surgery within 2 months because of adverse events. A clinical response was seen in 27 (66%) of 41 evaluable patients. BCS was performed in 27 (90%) of 30 patients who underwent surgery at 4 months. Of the ten patients eligible for mastectomy at baseline, six chose to continue exemestane treatment without surgery because of a PR or SD at 4 months. Adverse events, most of which were grade 1, occurred in ≤10% of patients. These results suggest that neoadjuvant exemestane treatment is effective and well tolerated in postmenopausal women with ER-positive breast cancer. Further studies are required to determine the optimal duration of neoadjuvant treatment and to identify response criteria that can more accurately predict long-term outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aim of neoadjuvant treatment is to decrease tumor volume through the delivery of drugs before surgery, thereby facilitating a more complete surgical removal of the tumor and improved patient survival. In locally advanced breast cancer, neoadjuvant treatment can downstage the disease and increase the rate of breast-conserving surgery (BCS), but survival benefits over standard adjuvant treatment have not yet been demonstrated [1, 2]. With recent advances in hormone therapy and the routine assessment of hormone receptor status in core needle biopsy samples, neoadjuvant endocrine therapy has come to the forefront of research investigations into chemotherapy alternatives for the treatment of hormone receptor-positive, large, operable, or locally advanced breast cancer [2].
Two categories of third-generation aromatase inhibitors are currently available for use in neoadjuvant therapy: type I steroidal inhibitors, such as exemestane, and type II nonsteroidal inhibitors, such as anastrozole and letrozole [2, 3]. The efficacy of all three of these aromatase inhibitors is superior to tamoxifen as first-line therapy for patients with locally advanced or metastatic breast cancer [4–6]. Anastrozole and letrozole have also demonstrated superior efficacy compared with tamoxifen when used as early adjuvant therapy after surgery in postmenopausal breast cancer [7–9], and switching to anastrozole and exemestane after 2–3 years of tamoxifen use is superior to remaining on tamoxifen after surgery [10–12]. Furthermore, letrozole produced disease-free survival benefits compared with placebo after 5 years of adjuvant tamoxifen use in early postmenopausal breast cancer [13]. In neoadjuvant settings, aromatase inhibitors have been shown to be effective in reducing tumor volume and enabling BCS, rather than a mastectomy, to be performed [14–21]. The findings from clinical trials to date indicate that aromatase inhibitors have a favorable toxicity profile with good treatment compliance.
Tamoxifen has been reported to be less effective in preventing relapse in patients with progesterone receptor (PgR)-negative and/or human epidermal growth factor receptor 2 (HER2)-positive tumors [22]. Therefore, PgR and HER2 can be used as surrogate markers for predicting the efficacy of adjuvant tamoxifen. On the other hand, letrozole has been reported to be more effective than tamoxifen as neoadjuvant therapy for epidermal growth factor receptor-positive and/or HER2-positive tumors [17]. In addition, adjuvant anastrozole treatment has been shown to provide longer relapse-free survival periods than tamoxifen for patients with PgR-negative tumors [23].
In Japan, anastrozole was the first aromatase inhibitor to be approved (in 2000) for use in women with breast cancer. Exemestane approval in advanced breast cancer followed in 2002, with subsequent approval for use in early breast cancer in 2005. Finally, letrozole was approved in 2006. Fewer studies have been conducted with exemestane than anastrozole, and the efficacy of neoadjuvant therapy with exemestane has not yet been evaluated in Japan. Exemestane is a steroidal aromatase inhibitor and may have less detrimental effects on bone formation and lipid metabolism than the nonsteroidal aromatase inhibitors [24, 25]. Consequently, we designed a multicenter phase II trial [Saitama Breast Cancer Clinical Study Group (SBCCSG)-03] to evaluate the efficacy and safety of exemestane as neoadjuvant therapy for 4 months in postmenopausal women with estrogen receptor (ER)-positive and/or PgR-positive breast cancer. Study end points included pathological and clinical response rate, conversion rate from anticipated mastectomy to BCS, and toxicity.
Patients and methods
Study design
In this phase II multicenter trial, patients with histologically confirmed ER-positive and/or PgR-positive invasive breast cancer were assigned to receive exemestane 25 mg/day for 16 weeks before surgery. Patients underwent baseline caliper, ultrasound, and/or mammography measurements, along with a core needle biopsy and blood sampling. Body weight and height at baseline were also recorded. Clinical measurements and blood sampling were repeated every 4 weeks after the start of treatment. Final caliper, ultrasound, and/or mammogram measurements, as well as body weight measurements and blood sampling, were performed at 16 weeks, before surgical excision.
Patients
Eligible patients were postmenopausal women with untreated, core needle biopsy-proven, invasive, ER-positive and/or PgR-positive breast cancer lesions that were 3 cm or larger and measurable using caliper, ultrasound, or mammography. All patients were operable or potentially operable and showed no evidence of metastases. Women were defined as being postmenopausal if they had a uterus and had been amenorrheic for at least 12 months or if they did not have a uterus and had circulating levels of follicle-stimulating hormone and estradiol that were compatible with a postmenopausal status.
Exclusion criteria included inoperable disease considered to be irreversible with neoadjuvant endocrine therapy, inflammatory breast cancer, concurrent severe medical disease, concurrent use of hormone replacement therapy, any previous malignancy, and any medical or psychiatric condition making informed consent impossible.
Study end points
The primary study end point was the pathological response rate after 16 weeks of treatment. Pathological response was assessed by a central review board according to the “histopathological criteria for assessment of therapeutic response in breast cancer” proposed by the Japanese Breast Cancer Society [26]. These response criteria are classified as grade 0, 1a, 1b, 2, or 3 and represent no change and mild, moderate, marked, and complete responses (CR), respectively: grade 0 includes almost no change in cancer cells; grade 1a includes slight changes in cancer cells, not suggestive of the death of cancer cells regardless of the area, or marked changes in cancer cells suggesting the cancer cells could barely survive, which is seen in less than one third of the area; grade 1b includes marked changes in cancer cells in one third or more but less than two thirds of the area; grade 2 includes marked changes in cancer cells in two thirds or more of the area; and grade 3 includes necrosis or disappearance of all tumor cells.
The secondary study end points were clinical response rate, conversion rate to BCS in patients deemed by their surgeons to require a mastectomy at baseline before starting treatment, and the occurrence of adverse events. Clinical response was defined as a CR or partial response (PR) and was assessed by caliper, ultrasound, or mammography. CR was defined as the clinical disappearance of the tumor at 4 months of treatment, and PR was defined according to the Response Evaluation Criteria in Solid Tumors (2000) [27] as a 30% or more decrease from baseline in the product of one maximum diameter. Stable disease (SD) was defined as a decrease of less than 30% (minor response) or an increase of less than 20% in the area of the tumor from baseline. Progressive disease (PD) was defined as an increase of 20% or more in the area of the tumor from baseline.
Statistical analysis
Because the clinical response rate for neoadjuvant tamoxifen use was expected to be 35% based on previous study results [14–17], we calculated that 37 patients would be needed to detect an increase in response to exemestane of 55% with 80% power and a two-sided 5% significance level. To allow for missing data, 40 patients were recruited. All end points, with the exception of safety outcomes, were analyzed on an intent-to-treat basis. All data were recorded on case report forms designed for the study, and the study database was compiled by the Saitama Cancer Center (Saitama, Japan). Data validation was carried out by the clinical study coordinator (K.I.).
ER, PgR, and HER2 analysis
Estrogen receptor and PgR status were initially determined locally for entry into the trial and were then confirmed at a central laboratory (Saitama Cancer Center, Saitama, Japan) using immunohistochemistry. Monoclonal anti-ERα antibody 1D5 (M7047, DakoCytomation, Glostrup, Denmark) was used to detect ER, and monoclonal anti-PgR antibody PgR 636 (M3569, DakoCytomation) was used to detect PgR. Tumors with more than 10% staining nuclei were described as ER positive or PgR positive. HER2 positivity was also assessed at the central laboratory (Saitama Cancer Center) using the Hercep Test™ (DakoCytomation); results were scored as 0, 1+, 2+, and 3+, according to the manufacturer’s instructions. Specimens scored as 2+ or 3+ were considered HER2 positive, and those 0 or 1+ were considered HER2 negative.
Tolerability assessment
Adverse events (defined as the development of a new medical condition or the deterioration of a pre-existing medical condition) were recorded every 4 weeks, and they were graded according to the National Cancer Institute, Common Toxicity Criteria, version 2 [28]. No pre-specified checklists were used. Serious adverse events (defined as fatal or life threatening, requiring hospitalization, causing disability or incapacity, or requiring medical intervention to prevent incapacity) were recorded as they occurred.
Ethical considerations
The trial was conducted in accordance with the principles of Good Clinical Practice as specified in the Declaration of Helsinki (1996 revision). The study protocol was approved by the Institutional Review Boards of the institutions where the patients were recruited and treated, and all patients gave written informed consent before study enrollment.
Results
Patients
Forty-four patients were enrolled from five institutes between July 2003 and November 2004, all of whom met the eligibility criteria. Baseline characteristics for this population, including disease stage, tumor size, and receptor status, are presented in Table 1. The median age of patients was 60 years (range, 48–88 years). Twenty-six patients (59%) had stage IIA disease, eight (18%) had stage IIB disease, four (9%) had stage IIIA disease, and six (14%) had stage IIIB disease. All patients had ER-positive tumors, of which 32 (73%) were also PgR positive. HER2 testing was performed in 41 patients; only 6 of these patients were HER2 positive. Most HER2-positive tumors were also PgR positive.
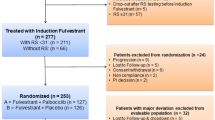
Pathological response
A pathological response was obtained in 13 (43%) of the 30 patients who underwent surgery after 4 months of neoadjuvant exemestane treatment. Grade 3 lesions were not seen, but grade 1b and grade 2 lesions were observed in nine and four patients, respectively (Table 2). A pathological response was more frequently obtained in invasive lesions than in situ lesions (Table 2). Fourteen patients were excluded from the pathological analysis; three of these patients underwent surgery within 2 months because of adverse events. The remaining 11 patients did not undergo surgery; 3 were treated with chemotherapy because of PD within 4 months, and 8 continued exemestane therapy because of a PR or SD at 4 months. The microscopic appearances of the invasive and in situ lesions before and after exemestane treatment are shown in Fig. 1.
Microscopic appearance of invasive ductal carcinoma (hematoxylin and eosin staining). Core needle biopsy specimen of an invasive lesion before 4 months of exemestane treatment (a) and grade 2 pathological response obtained in surgically removed specimen after treatment (b). Core needle biopsy specimen of an in situ lesion before 4 months of exemestane treatment (c) and grade 1b pathological response obtained in surgically removed specimen after treatment (d)
Clinical response
A clinical response was seen in 27 (66%) of the 41 patients who were assessed either by caliper, ultrasound, or mammography. SD and PD were observed in nine (22%) and five (12%) patients, respectively (Table 3). Among the five patients diagnosed as having PD, three were treated with chemotherapy without surgery and two underwent surgery at 4 months.
Adverse events
Of the 44 patients who participated in the trial, 3 (7%) discontinued exemestane treatment because of adverse events: hematologic disorder (grade 3, 1 patient), dizziness (grade 2, 1 patient), and genital bleeding (grade 1, 1 patient) (Table 4). All three of these patients underwent surgery within 2 months of starting exemestane treatment. Other adverse events, most of which were grade 1, occurred in ≤10% of the patients (Table 4).
Conversion from anticipated mastectomy to breast-conserving surgery
At baseline, 10 patients were deemed to require a mastectomy, and the other 34 were eligible for BCS. Of the ten patients eligible for mastectomy, two underwent a mastectomy despite having a PR at 4 months and one underwent a mastectomy within 1 month of the start of exemestane treatment because of a hematologic disorder. Six patients chose to continue exemestane therapy without surgery because of a PR or SD at 4 months, and one underwent chemotherapy because of PD. Of the 34 patients eligible for BCS, 30 underwent BCS, 2 underwent chemotherapy without surgery because of PD, and 2 chose to continue exemestane use because of a PR. As a result, the BCS rate was 90% among the 30 patients who underwent surgery at 4 months.
Tumor response and PgR or HER2 expression
Partial response was seen in 22 of 31 (71%) patients with PgR-positive tumors; 17 of these tumors were also HER2 negative (Table 5). In PgR-negative tumors, five of ten (50%) patients had a PR. Three HER2-positive patients had a PR or SD. No significant correlation between pathological response and PgR or HER2 expression was observed, although the small numbers of PgR-negative and HER2-positive patients makes it difficult to draw conclusions from these data.
Discussion
In this study, a pathological response rate of 43% was achieved following 16 weeks of neoadjuvant exemestane in postmenopausal women with stage II to IIIB breast cancer measuring more than 3 cm in diameter. However, this rate may not reflect the true pathological response rate associated with neoadjuvant exemestane because only 30 patients underwent surgery and 8 patients were maintained on treatment with exemestane because of continued clinical benefit (PR or SD). Histopathologic evaluations of the response to neoadjuvant therapy have not yet been standardized [29]; however, the Japanese Breast Cancer Society has proposed histopathological criteria for assessing therapeutic response and has classified the responses into grades 0 to 3 [26]. A pathological CR after neoadjuvant chemotherapy is important because it improves prognosis; however, the predictive values of response criteria other than pathological CR, such as grade 1 and 2 responses according to the Japanese response criteria, remain to be evaluated. Because a pathological CR is rare for neoadjuvant hormone therapy, pathological responses other than a pathological CR are likely to be important. Whether such responses are capable of predicting survival needs to be evaluated in long-term follow-up studies.
The clinical response rate in this study was 66%, which is comparable with previously reported response rates ranging from 37 to 89% in trials of neoadjuvant exemestane use (Table 6) [18–21]. This clinical response rate was considered to be satisfactory because more than 60% of the patients whose tumors were clinically defined as being sensitive to exemestane were able to receive further exemestane treatment after surgery. Furthermore, clinical response rate may be affected by duration of treatment. In a neoadjuvant trial with letrozole, the median time to achieve a maximum response was 4.2 months [30]. In the current study, seven patients chose to continue exemestane administration because of a PR or SD at 4 months, suggesting that the optimal duration of neoadjuvant treatment with aromatase inhibitors is probably longer than 4 months. Further clinical trials are required to resolve this question.
In previous neoadjuvant trials with exemestane, no fatal adverse events have been reported. In this study, adverse events occurred in ≤10% of the patients, most of whom experienced grade 1 events with the exception of one patient who experienced grade 3 liver dysfunction and leukocytopenia. In a trial of adjuvant exemestane in which patients were switched to exemestane after 2–3 years of tamoxifen treatment, adverse events such as thromboembolic disease and gynecological symptoms were more frequent among patients who continued to receive tamoxifen, whereas visual disturbances, osteoporosis, arthralgia, and diarrhea were more frequent among those switched to exemestane [10]. The adverse event profile of exemestane is similar to the nonsteroidal aromatase inhibitors.
Studies have shown that the conversion rate from an anticipated mastectomy to BCS is higher after neoadjuvant therapy with aromatase inhibitors than with tamoxifen [15–17, 21]. In this study, none of the ten patients who were deemed to need a mastectomy at baseline underwent BCS at 4 months; however, six patients chose to continue exemestane use without surgery. Thus, the conversion rate from anticipated mastectomy to BCS after 4 months of exemestane use could not be determined. This finding suggests that once tumors begin to shrink, patients prefer to continue exemestane treatment rather than undergo surgery. The eight patients in this study who continued exemestane use without surgery will require careful follow-up, and such monitoring should help to determine the appropriate duration of neoadjuvant exemestane treatment.
Recent reports have suggested that ER-positive/PgR-negative tumors are more likely to be HER2 positive than tumors that are ER positive/PgR positive, and that HER2 signaling decreases the transcription of ER and PgR genes [31, 32]; PgR loss may therefore be a surrogate marker for HER2 activity. Although aromatase inhibitors are no less effective than tamoxifen, regardless of their PgR or HER2 status, they are likely to be more effective than tamoxifen in PgR-positive or HER2-negative tumors. In fact, letrozole administered after 5 years of tamoxifen use was no more effective than placebo for patients with PgR-negative tumors [33]. In this study, however, no correlation was observed between PgR and HER2 expression or in clinical or pathological response by PgR or HER2 status. This may be due, in part, to the small study size and the small number of HER2-positive breast cancers (6 of 44; 14%).
The potential survival advantage of neoadjuvant therapy with aromatase inhibitors in postmenopausal breast cancer remains unknown. However, clinical response and pathological response may be surrogate markers for predicting prognosis because the same aromatase inhibitor that is effective in neoadjuvant therapy can also be used for adjuvant therapy in the same patient. In contrast, for patients who require chemotherapy or surgery for PD after neoadjuvant aromatase inhibitor therapy, an aromatase inhibitor may not be the adjuvant treatment of choice. Therefore, the neoadjuvant use of aromatase inhibitors provides important information for selecting further optimal treatments based on tumor response.
The results of this study indicate that neoadjuvant exemestane treatment is effective and well tolerated in postmenopausal women with ER-positive breast cancer. Further studies are required to determine the optimal duration of neoadjuvant treatment with aromatase inhibitors in this setting and to identify study end points that can more accurately predict long-term clinical outcomes.
References
Wolff AC, Davidson NE (2000) Primary systemic therapy in operable breast cancer. J Clin Oncol 18:1558–1569
Freedman OC, Verma S, Clemons MJ (2005) Using aromatase inhibitors in the neoadjuvant setting: evolution or revolution? Cancer Treat Rev 31:1–17
Strasser-Weippl K, Goss PE (2005) Advances in adjuvant hormonal therapy for postmenopausal women. J Clin Oncol 23:1751–1759
Nabholtz JM, Buzdar A, Pollak M et al (2000) Anastrozole is superior to tamoxifen as first-line therapy for advanced breast cancer in postmenopausal women: results of a North American multicenter randomized trial. J Clin Oncol 18:3758–3767
Mouridsen H, Gershanovich M, Sun Y et al (2001) Superior efficacy of letrozole versus tamoxifen as first-line therapy for postmenopausal women with advanced breast cancer: results of a phase II study of the International Letrozole Breast Cancer Study Group. J Clin Oncol 19:2596–2606
Paridaens R, Therasse P, Dirix L et al (2004) First line hormonal treatment (HT) for metastatic breast cancer (MBC) with exemestane (E) or tamoxifen (T) in postmenopausal patients—a randomized phase III trial of the EORTC Breast Group [abstract 515]. Proc Am Soc Clin Oncol 23:6
Baum M, Budzar AU, Cuzick J et al (2002) Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomized trial. Lancet 359:2131–2139
Baum M, Budzar AU, Cuzick J et al (2003) Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: results of the ATAC (Arimidex, Tamoxifen Alone or in Combination) trial efficacy and safety update analyses. Cancer 98:1802–1810
The Breast International Group (BIG) 1-98 Collaborative Group (2005) A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 353:2747–2757
Coombes RC, Hall E, Gibson LJ et al (2004) A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 350:1081–1092
Jakesz R, Jonat W, Gnant M et al (2005) Switching of postmenopausal women with endocrine responsive early breast cancer to anastrozole after 2 years’ adjuvant tamoxifen: combined results of the ABCSG trial 8 and ARNO 95 trial. Lancet 366:455–462
Boccardo F, Rubagotti A, Puntoni M et al (2005) Switching to anastrozole versus continued tamoxifen treatment of early breast cancer: preliminary results of the Italian Tamoxifen Anastrozole Trial. J Clin Oncol 23:5138–5147
Goss PE, Ingle JN, Martino S et al (2005) Randomized trial of letrozole following tamoxifen as extended adjuvant therapy in receptor-positive breast cancer: updated findings from NCIC CTG MA.17. J Natl Cancer Inst 97:1262–1271
Dixon JM, Renshaw L, Bellamy C et al (2000) The effects of neoadjuvant anastrozole (Arimidex) on tumor volume in postmenopausal women with breast cancer: a randomized, double-blind, single-center trial. Clin Cancer Res 6:2229–2235
Smith IE, Dowsett M, Ebbs SR et al (2005) Neoadjuvant treatment of postmenopausal breast cancer with anastrozole, tamoxifen, or both in combination: the immediate preoperative anastrozole, tamoxifen, or combined with tamoxifen (IMPACT) multicenter double-blind randomized trial. J Clin Oncol 23:5108–5116
Eiermann W, Paepke S, Appfelstaedt J et al (2001) Preoperative treatment of postmenopausal breast cancer patients with letrozole: a randomized double-blind multicenter study. Ann Oncol 12:1527–1532
Ellis MJ, Coop A, Singh B et al (2001) Letrozole is more effective neoadjuvant endocrine therapy than tamoxifen for ErbB-1- and/or ErbB-2-positive, estrogen receptor-positive primary breast cancer: evidence from a phase III randomized trial. J Clin Oncol 19:3808–3816
Gil MJ, Barnadas A, Cirera L et al (2004) Primary hormonal therapy with exemestane in patients with breast tumors >3 cm in diameter; results of a Spanish multicenter phase II trial [abstract 603]. Proc Am Soc Clin Oncol 23:27
Tubiana-Hulin M, Spyratos F, Becette V et al (2003) Phase II study of neo-adjuvant exemestane in postmenopausal patients with operable breast cancer [abstract 443]. Breast Cancer Res Treat 82:S106
Krainick U, Astner A, Jonat W, Wallwiener D (2003) Phase II study to define safety and efficacy of exemestane as preoperative therapy for postmenopausal patients with primary breast cancer-final results of the German Neoadjuvant Aromasin Initiative (GENARI) [abstract 239]. Breast Cancer Res Treat 82:S55
Semiglazov VF, Semiglazov VV, Ivanov VG et al (2003) Neoadjuvant endocrine therapy: exemestane (E) vs tamoxifen (T) in postmenopausal ER+ breast cancer patients (T1-4N1-2M0) [abstract 111]. Breast Cancer Res Treat 82:S22
Tovey S, Dunne B, Witton CJ et al (2005) Can molecular markers predict when to implement treatment with aromatase inhibitors in invasive breast cancer? Clin Cancer Res 11:4835–4842
Dowsett M, Cuzick J, Wale C et al (2005) Retrospective analysis of time to recurrence in the ATAC trial according to hormone receptor status: an hypothesis-generating study. J Clin Oncol 23:7512–7517
Bundred NJ (2005) The effects of aromatase inhibitors on lipids and thrombosis. Br J Cancer 93:S23–S27
Goss PE, Qi S, Cheung AM et al (2004) Effects of the steroidal aromatase inhibitor exemestane and the nonsteroidal aromatase inhibitor letrozole on bone and lipid metabolism in ovariectomized rats. Clin Cancer Res 10:5717–5723
Kurosumi M, Akiyama F, Iwase T et al (2001) Histopathological criteria for assessment of therapeutic response in breast cancer. Breast Cancer 8:1–2
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Cancer Therapy Evaluation Program. Common Toxicity Criteria version 2.0 (1999) National Cancer Institute. http://www.fda.gov/cder/cancer/toxicityframe.htm. Cited 30 November 2006
Kuroi K, Toi M, Tsuda H et al (2006) Issues in the assessment of the pathologic effect of primary systemic therapy for breast cancer. Breast Cancer 13:38–48
Llombart A, Galán A, Fuster C et al (2006) Phase II trial with letrozole (2.5 mg) to maximal response as neoadjuvant endocrine therapy in postmenopausal patients with ER/PR[+] operable breast cancer [abstract 362]. Eur J Cancer 4:154
Arpino G, Weiss H, Lee AV et al (2005) Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst 97:1254–1261
Cui X, Schiff R, Arpino G et al (2005) Biology of progesterone receptor loss in breast cancer and its implications for endocrine therapy. J Clin Oncol 23:7721–7735
Goss P, Ingle J, Tu D (2006) NCIC CTG MA17: updated analysis on disease free survival (DFS) according to the estrogen receptor and progesterone receptor status of the primary tumor [abstract 350]. Eur J Cancer 4:149–150
Acknowledgments
This study was supported by a grant from Pharmacia, Inc. We thank Janet E. Stead, MBBS, who provided editorial assistance on behalf of Pfizer Inc. This paper was presented at the 5th European Breast Cancer Conference, Nice, France, March 23, 2006.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takei, H., Suemasu, K., Inoue, K. et al. Multicenter phase II trial of neoadjuvant exemestane for postmenopausal patients with hormone receptor-positive, operable breast cancer: Saitama Breast Cancer Clinical Study Group (SBCCSG-03). Breast Cancer Res Treat 107, 87–94 (2008). https://doi.org/10.1007/s10549-007-9529-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9529-4